Published online Feb 6, 2024. doi: 10.12998/wjcc.v12.i4.777
Peer-review started: August 22, 2023
First decision: October 9, 2023
Revised: November 5, 2023
Accepted: January 8, 2024
Article in press: January 8, 2024
Published online: February 6, 2024
Processing time: 156 Days and 0.8 Hours
Bezoars usually compile human fibers and debris. A special form of bezoar in case of psychologically altered individuals is the trichobezoar. It consists of voluntarily swallowed hair bulks and is normally removed via gastroscopy. Trichobezoars leading to ileus have rarely been reported.
A 24-year-old female patient presented to the emergency room with abdominal pain, nausea, and vomiting for 3 d. Her previous medical and psychiatric history was unremarkable. Laboratory analysis showed iron deficiency anemia, leukocytosis, and elevated liver enzymes. An abdominal CT scan revealed a dense structure in the patients’ stomach which turned out to be a huge trichobezoar completely obstructing the pylorus. The trichobezoar had to be removed surgi
A mechanical bowel obstruction is a potentially life-threatening event for every patient. In our case a young female was suffering from severe symptoms of an obstruction which might have resulted in serious harm without successful surgical management.
Core Tip: A 24-year-old female patient presented to the emergency room with symptoms of a mechanical bowel obstruction. An abdominal CT scan confirmed the obstruction by a dense structure in the patients’ stomach which turned out to be a huge trichobezoar completely obstructing the pylorus. Endoscopic removal failed and therefore the trichobezoar had to be removed surgically. The patient recovered, underwent psychiatric treatment, and is well in her 24-mo follow-up since the operation.
- Citation: Scherrer M, Kornprat P, Sucher R, Muehlsteiner J, Wagner D. Mechanical upper bowel obstruction caused by a large trichobezoar in a young woman: A very unusual case report. World J Clin Cases 2024; 12(4): 777-781
- URL: https://www.wjgnet.com/2307-8960/full/v12/i4/777.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i4.777
Bezoars usually represent amounts of human or vegetable fibers that accumulate in the gastrointestinal tract. The word “bezoar” comes from the Arabic word “bedzehr” or the Persian word “padzhar,” meaning “protecting against a poison.” In ancient times animal guts were used as antidot to poisons and are still used in traditional Chinese medicine[1]. In the medical literature they were first referenced in the late 1770s in an autopsy report of a patient who died from ingestion causing gastric perforation and peritonitis[2,3]. Bezoars usually comprise phytobezoars consisting of plant fibers, lactobezoars out of milk fibers, pharmacobezoars which consist of pills and pharmacological capsules, and trichobezoars[4].
Trichobezoars are common in patients with underlying psychiatric disorders who chew and swallow their own hair. Trichobezoar describes the pulling out and swallowing of one's own hair and is usually associated with other psychodynamic illnesses[5]. These hairs accumulate in the patients’ stomach and form a mass since they are retained in the folds of the gastric mucosa because their surface prevents propulsion and peristalsis. This causes amassing of more hair leading to larger formations. These formations cause gastric atony preventing further emptying. The hair becomes matted together and usually assimilates the stomachs form, making further intestinal passages impossible[2,6]. The swallowed hair accumulates in the stomach and, after reaching a certain size, leads to various gastrointestinal symptoms, wasting, and cachexia[7].
Rapunzel syndrome is a rare disease with a long trichobezoar reaching the small intestine and sometimes beyond leading to an intestinal obstruction[5].
Usually, the hair can be extracted using gastroscopy as most patients cannot live with a mass that large in their stomach. We herein report a young female adult patient who swallowed so much hair that it accumulated to the size of her stomach leading to a complete obstruction with a size too huge to extract endoscopically.
A 24-year-old young woman without signs of cachexia (height 175, weight 85 kg – body mass index 27.8 kg/m2) presented to the emergency department with abdominal pain, nausea, and vomiting for 3 d.
The patient had no fever, her pulse rate was 69/min, and her blood pressure was 135/69 mmHg. There was no evidence of cardiorespiratory or hemodynamic instability.
The patient had no past illnesses, and this was her first presentation to the hospital.
The patient’s family history was unremarkable.
On abdominal clinical examination, the abdominal wall was soft, without defensive tension and with regular bowel sounds.
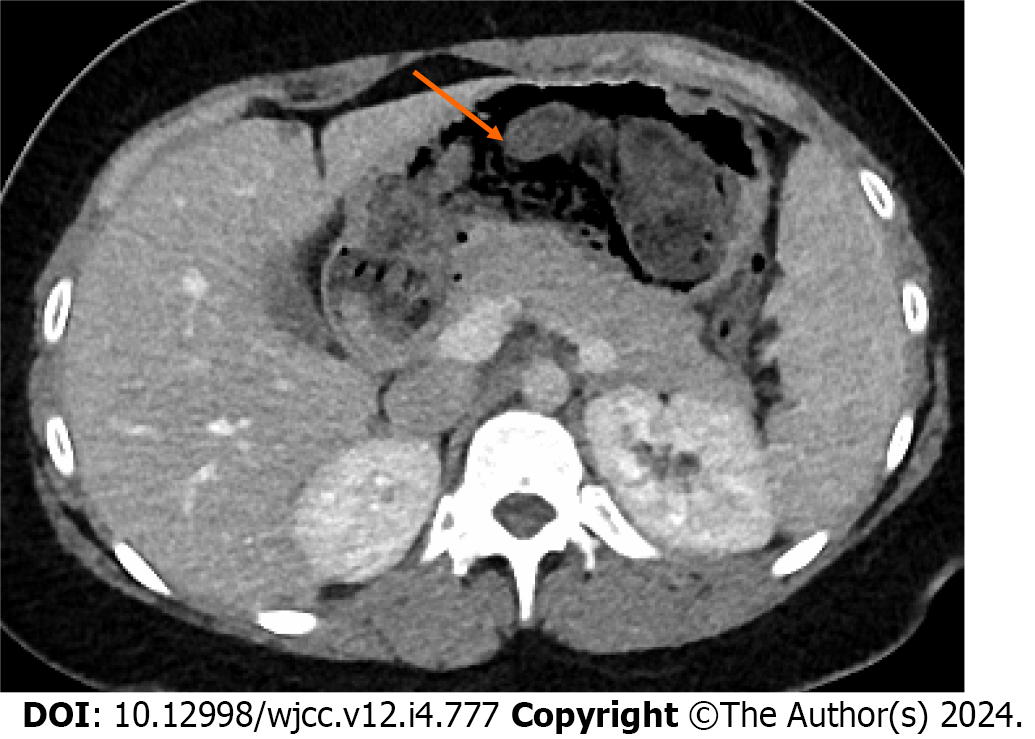
The dense structure in the patients’ stomach extended throughout to the duodenum and distended it to take its course into the proximal jejunum loops. With suspicion of trichobezoar, a gastroscopy was performed immediately, which showed a huge trichobezoar mixed with undigested food material that completely obstructed the pylorus (Figure 1).
Laboratory examination revealed iron deficiency anemia, leukocytosis, and elevated liver enzymes correlating with CT findings of focal steatosis in segment IVa. Additionally, the stomach of the patient looked filled with a fibrous mass on abdominal CT. Upon questioning, the patient admitted on pulling out her own hair and eating it habitually. The previous psychiatric history of the patient was insignificant without prior medication.
Removal via gastroscopy was attempted. Due to the size of the trichobezoar and its dense nature, fractured removal was not possible. As the trichobezoar extended into the patient’s duodenum, endoscopic removal was not feasible.
The final diagnosis of an unremovable trichobezoar due to existing Rapunzel syndrome causing a complete upper intestinal obstruction was made.
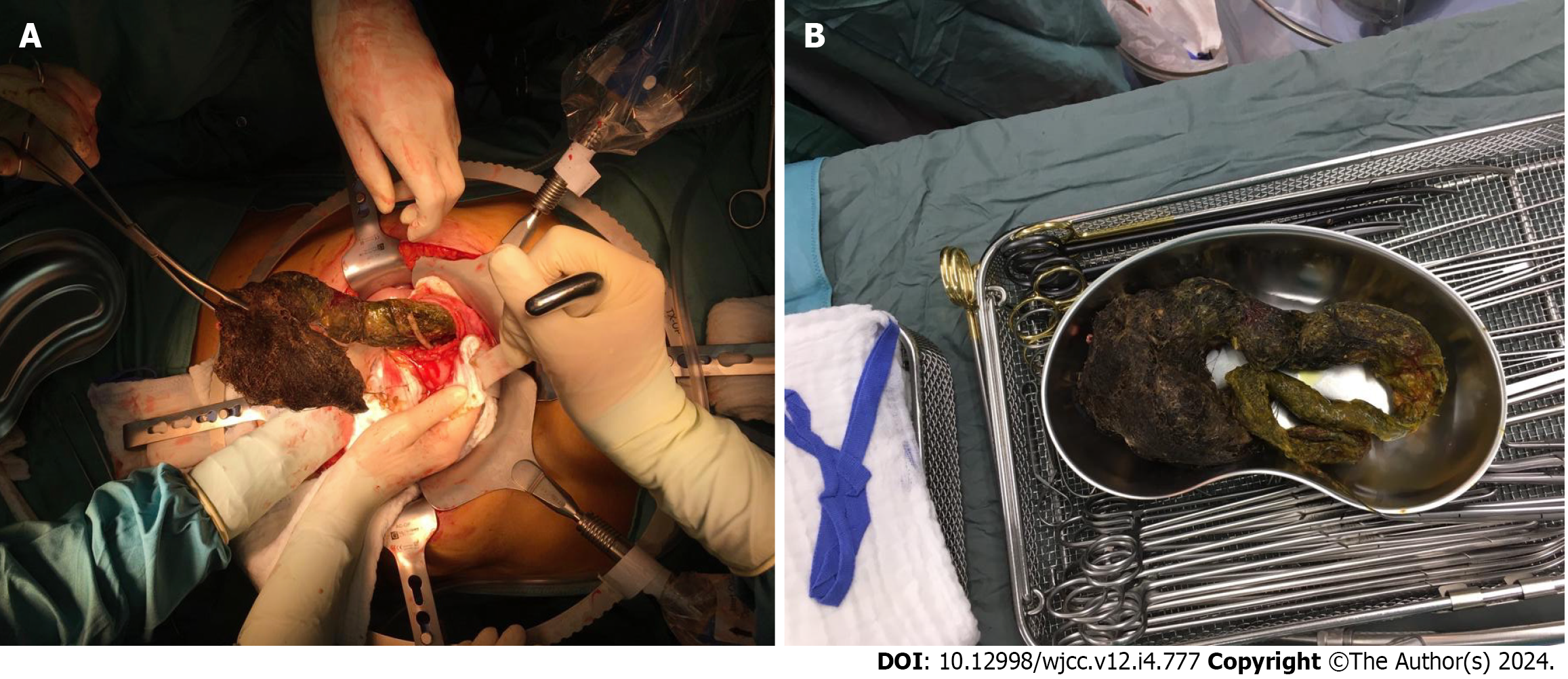
After unsuccessful endoscopic removal, a surgical laparotomy was indicated. Midline minilaparotomy was performed, revealing an enlarged stomach. Gastrotomy was done and the trichobezoar was extracted completely (Figure 2A). Even after extraction, the trichobezoar retained the patients’ stomach form. Surgery was well tolerated, and the bezoar could be extracted completely (Figure 2B). Immediate postoperative course was unremarkable. After 11 d, the patient developed a subcutaneous seroma which was managed via puncturing.
Further psychological and psychiatric support was introduced to the patient. In our patient, no real stressor for the obvious psychiatric alteration could be found, even as she was examined recurrently by our psychiatrists. She described boredom and family distress without further explanation for her psychiatric condition. After medication with serotonin reuptake inhibitors, no further hair swallowing was observed.
Trichobezoars are formed by hair follicles and usually collected in the mucosal folds. Over time, these masses grow increasingly longer and amass more hair. Usually, one of the first symptoms is an unpleasant odor from the patient’s mouth that is derived from denaturizing hair follicles. Usually, trichobezoars that size like described in our patient are observed in pediatric or geriatric patients but not in adults. In childhood, these diseases are associated with emotional stress and eating disorders, and in adults, also emotional or psychiatric trouble is usually present[8]. In our patient, no real stressor for the obvious psychiatric alteration could be found, even as she was examined recurrently by our psychiatrists. She described boredom and family distress without further explanation for her psychiatric condition. After medication with serotonin reuptake inhibitors, no further hair swallowing was observed. In our case, the trichotillomania also did not result in alopecia areata nor any physical remarks. Generally, trichobezoars are only present in 0.6%-1.6% of patients with trichotillomania, and only under 1% of these patients need surgery[8]. Therefore, this case is clearly unique with regard to age and the magnitude of the bezoar present.
Rapunzel syndrome is even rarer than normal trichobezoars, and usually not all of the following criteria are required to diagnose the syndrome: (1) Trichobezoar with a tail; (2) tail extending into the duodenum; and (3) intestinal obstruction is present[3]. Our patient even met all these criteria (Figure 2B).
Usual complications exerted from Rapunzel syndrome are hemorrhage, enteropathy, steatorrhea, pancreatitis, or intussusception. The syndrome has even been described as a cause of jaundice or appendicitis. A complete obstruction of the stomach is rare due to its flexible nature[9,10]. However, this was the case in our patient – another unique point about this case. Without intervention, this case might even have resulted in a fatal outcome, which could only be prevented via surgical removal. However, our patient had not suffered from weight loss or appetite change prior to hospital admission and presented with the sole symptom of nausea and vomiting. Also, no petechial bleeding or nutritional deficiencies were observed in the patient. The diagnosis made in this case on the CT scan is a chance diagnosis that prevented a fatal outcome. Even the CT scan was only performed as the patient presented to the emergency department with nausea and vomiting as acute symptoms. If the patient would have presented at family medicine with these symptoms, the diagnoses would have been delayed and the symptoms might have worsened, leading to a worse outcome.
Until now, there is no medical treatment for trichobezoars of the stomach. Despite approaches with enzymatic degradation have been made in pediatric medicine, endoscopic removal remains the mainstay of cure[8,11]. Due to the large and rigid trichobezoar, this was not feasible in our patient. In our case, the patient presented with a complete intestinal obstruction which might have led to a fatal outcome without recognition and immediate intervention.
Endoscopic removal of trichobezoars is not always possible for every patient. Due to the flexible nature of trichobezoars, these formations can stick to the stomach wall and careful removal is not possible. Our patient suffered from a complete upper intestinal obstruction, so only surgical removal was possible to reach the desired recovery. Without removal, the outcome might have become fatal. This case is clearly unique due to the patient’s age and the unremarkable medical history prior presentation. So the complete obstruction was more a chance finding due to gastrointestinal symptoms than what we would have expected.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Austrian Society of Gastroenterology & Hepatology.
Specialty type: Surgery
Country/Territory of origin: Austria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ghannam WM, Egypt; Shiryajev YN, Russia S-Editor: Lin C L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Wang C, Zhao X, Mao S, Wang Y, Cui X, Pu Y. Management of SAH with traditional Chinese medicine in China. Neurol Res. 2006;28:436-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Naik S, Gupta V, Naik S, Rangole A, Chaudhary AK, Jain P, Sharma AK. Rapunzel syndrome reviewed and redefined. Dig Surg. 2007;24:157-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 111] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Vaughan ED Jr, Sawyers JL, Scott HW Jr. The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery. 1968;63:339-343. [PubMed] |
| 4. | Gonuguntla V, Joshi DD. Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res. 2009;7:99-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 107] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 5. | Del Val Ruiz P, Carrasco Aguilera B, Turienzo Santos EO, Sanz Álvarez LM. Intragastric foreign body: Giant trichobezoar. Cir Esp (Engl Ed). 2022;100:787. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Deslypere JP, Praet M, Verdonk G. An unusual case of the trichobezoar: the Rapunzel syndrome. Am J Gastroenterol. 1982;77:467-470. [PubMed] |
| 7. | Kyin C, Pushpak P, Casas-Melley A, Abdalla WM. Westmoreland T Acute case of trichobezoar diagnosed from computed tomography and 3D images: Rapunzel Syndrome re examined. Cureus. 28:e35597. |
| 8. | Chintamani, Durkhure R, Singh JP, Singhal V. Cotton Bezoar--a rare cause of intestinal obstruction: case report. BMC Surg. 2003;3:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Ventura DE, Herbella FA, Schettini ST, Delmonte C. Rapunzel syndrome with a fatal outcome in a neglected child. J Pediatr Surg. 2005;40:1665-1667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Wolfson PJ, Fabius RJ, Leibowitz AN. The Rapunzel syndrome: an unusual trichobezoar. Am J Gastroenterol. 1987;82:365-367. [PubMed] |
| 11. | Dalshaug GB, Wainer S, Hollaar GL. The Rapunzel syndrome (trichobezoar) causing atypical intussusception in a child: a case report. J Pediatr Surg. 1999;34:479-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |