Published online Feb 6, 2024. doi: 10.12998/wjcc.v12.i4.766
Peer-review started: November 30, 2023
First decision: December 18, 2023
Revised: December 25, 2023
Accepted: January 15, 2024
Article in press: January 15, 2024
Published online: February 6, 2024
Processing time: 55 Days and 22.8 Hours
Heart failure (HF), a common cardiovascular condition, is characterized by significant morbidity and mortality. While traditional Chinese medicine (TCM) is often used as a complementary approach in HF management, systematic evalua
To systematically analyze the effects of TCM on the clinical comprehensive outcomes, TCM syndrome scores, and BNP levels in patients with HF and evaluated the quality of evidence for these trials.
RCTs on TCM for HF treatment published since the establishment of the database were searched in four Chinese and English databases, including China National Knowledge Infrastructure, Wanfang, VIP Information Chinese Science and Technology Journal, and PubMed. Methodological quality was assessed for the included studies with the Cochrane risk-of-bias assessment tool, and the meta-analysis and publication bias assessment was performed with the RevMan5.3 software. Finally, the quality of evidence was rated according to the GRADE criteria.
A total of 1098 RCTs were initially retrieved. After screening, 16 RCTs were finally included in our study, which were published between 2020 and 2023. These RCTs involved 1660 HF patients, including 832 in the TCM group [TCM combined with conventional Western medicine (CMW) treatment] and 828 in the CWM group (CWM treatment). The course of treatments varied from 1 wk to 3 months. TCM syndrome differentiation was analyzed in 11 of the included RCTs. In all included RCTs, outcome indicators included comprehensive clinical outcomes, TCM syndrome scores, and BNP levels. The meta-analysis results showed significant differences between the TCM and CWM groups in terms of comprehensive clinical outcomes [risk ratio = -0.54; 95% confidence interval (CI) = -0.61, -0.47; P < 0.00001], TCM syndrome scores [weighted mean difference (WMD) = -142.07; 95%CI = -147.56, -136.57; P < 0.00001], and BNP levels (WMD = -142.07; 95%CI = -147.56, -136.57; P < 0.00001). According to the GRADE criteria, RCTs where "TCM improves clinical comprehensive outcomes" were rated as low-quality evidence, and RCTs where "TCM reduces TCM syndrome scores" or "TCM decreases BNP levels" were rated as medium-quality evidence.
TCM combined with CWM treatment effectively improves comprehensive clinical outcomes and diminishes TCM syndrome scores and BNP levels in HF patients. Given the low and medium quality of the included RCTs, the application of these results should be cautious.
Core Tip: This study evaluated the effects of traditional Chinese medicine (TCM) on heart failure (HF) patients by analyzing randomized controlled trials (RCTs). The meta-analysis results showed that TCM combined with conventional Western medicine treatment improved comprehensive clinical outcomes, reduced TCM syndrome scores, and decreased B-type natriuretic peptide levels. However, caution should be exercised due to the low and medium quality of the included RCTs. TCM shows promise as a complementary therapy for HF, but further high-quality research is needed to confirm its effectivenes.
- Citation: Xia LL, Yang SY, Xu JY, Chen HQ, Fang ZY. Comprehensive effects of traditional Chinese medicine treatment on heart failure and changes in B-type natriuretic peptide levels: A meta-analysis. World J Clin Cases 2024; 12(4): 766-776
- URL: https://www.wjgnet.com/2307-8960/full/v12/i4/766.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i4.766
Heart failure (HF) is a clinical syndrome primarily characterized by dyspnea, stemming from various factors that impair heart function[1]. The incidence and mortality rates of HF have been increasing annually, influenced by the growing prevalence of chronic diseases and an aging population. Despite advancements, current HF treatments often fall short of achieving satisfactory patient outcomes[2]. In modern medicine, there is a significant need to explore therapies that enhance the comprehensive clinical outcomes for HF patients[3]. Recently, Traditional Chinese Medicine (TCM), known for its multifaceted components, has shown promising advantages in HF treatment[4]. For instance, Liang et al[5] observed that compared with conventional Western medicine (CWM) alone, a combination of TCM, acupuncture, and CWM effectively improved HF indexes and clinical outcomes in patients with Qi-deficiency-blood-stasis syndrome of HF (heart functional class II). As growing studies have appeared in recent years, multiple studies have also demonstrated that TCM can improve comprehensive clinical outcomes and also is effective in improving TCM syndrome scores and lowering B-type natriuretic peptide (BNP) levels in HF patients[6,7]. Nevertheless, the low quality of single studies limits the current application of these results. Accordingly, we conducted a meta-analysis of randomized controlled trials (RCTs) on TCM for HF treatment and assessed the quality of evidence for these RCTs based on GRADE criteria to evaluate the effect of TCM on comprehensive clinical outcomes, TCM syndrome scores, and BNP levels in HF patients, thus aiding in making evidence-based clinical decisions.
Study type: This study included RCTs of TCM for HF treatment which were published in Chinese or English only.
Participants: Included patients must meet the diagnostic criteria in one of the recognized guidelines or expert consensuses, such as Chinese expert consensus on the diagnosis and treatment of chronic heart failure in elderly patients (2021)[8], Chinese Expert Consensus on Biomarkers for Heart Failure[9], and Age, functional capacity, and health-related quality of life in patients with heart failure[10]. There was no restriction on sex, age, and disease duration.
Interventions: TCM combined with CWM was used in the TCM group, and CWM was utilized in the CWM group, with unlimited dosage and treatment duration in both groups.
Outcome indicators: Outcome indicators included comprehensive clinical outcomes, TCM syndrome scores, and BNP levels.
Exclusion criteria: Exclusion criteria for trials were as follows: (1) Trials involving two or more TCM interventions; (2) Trials with non-comparable general data between groups; (3) Trials with incomplete or erroneous data; (4) Trials with repeated publications; and (5) Animal experiments, case studies, meta-analyses, and reviews.
Relevant RCTs published since the establishment of the database were searched in four Chinese and English databases, including China National Knowledge Infrastructure, Wanfang, VIP Information Chinese Science and Technology Journal, and PubMed. Keywords for searching Chinese articles were as follows: (1) “Traditional Chinese medicine”; and (2) “Heart failure” and its synonyms. Keywords for searching English articles were as follows: (1) “Traditional Chinese medicine”; and (2) “Heart failure” and its synonyms. Additionally, the reference list of the searched articles was tracked.
Two researchers read the title and abstract independently, screened the searched articles according to the inclusion and exclusion criteria, and then cross-checked the screened articles. In case of disagreement, the researchers negotiated and a third researcher was involved.
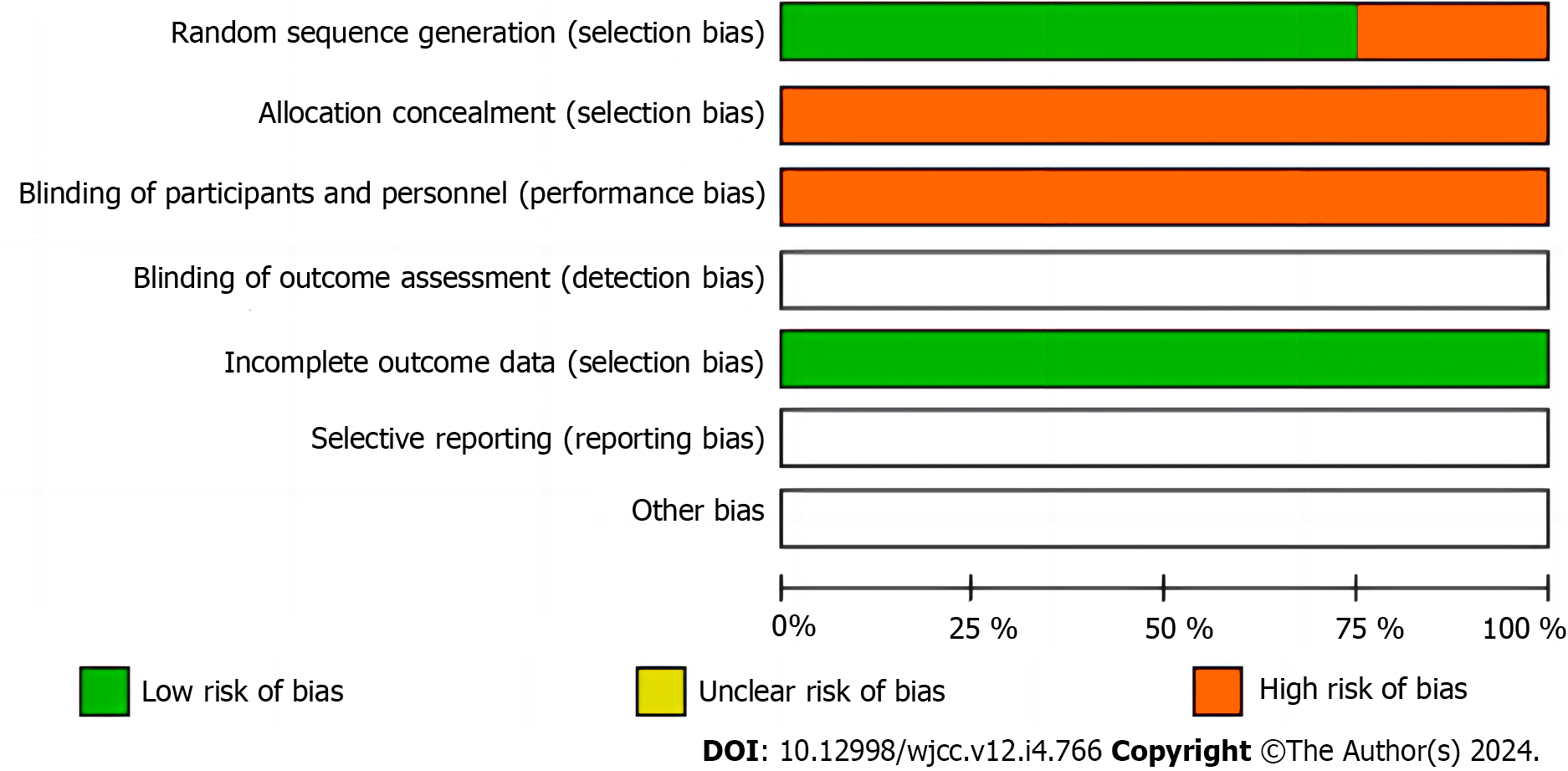
The Cochrane Handbook[11] was used to evaluate the quality of methodologies, including randomized sequence generation, allocation concealment, blinding of participants and implementers, blinding of study outcome assessors, incomplete outcome data, selective outcome reporting, and other biases. The included trials were assessed as “low risk”, “high risk”, or “unclear risk”.
The quality of evidence was assessed based on GRADE criteria, which was categorized into four levels: high, medium, low, and very low.
Revman 5.3 was applied for data analysis. Effect sizes were presented using risk ratio (RR) and its 95% confidence interval (95%CI) for dichotomous variables and using weighted mean difference (WMD) and its 95%CI for continuous variables. Heterogeneity was tested with I2. When P > 0.1 and I2 < 50%, heterogeneity was considered small and the fixed-effects model was selected. when P ≤ 0.1 and I2 ≥ 50%, heterogeneity was considered large and sensitivity analysis was conducted. P < 0.05 indicated a statistically significant difference. If ≥ 10 studies were included, a funnel plot was drawn.
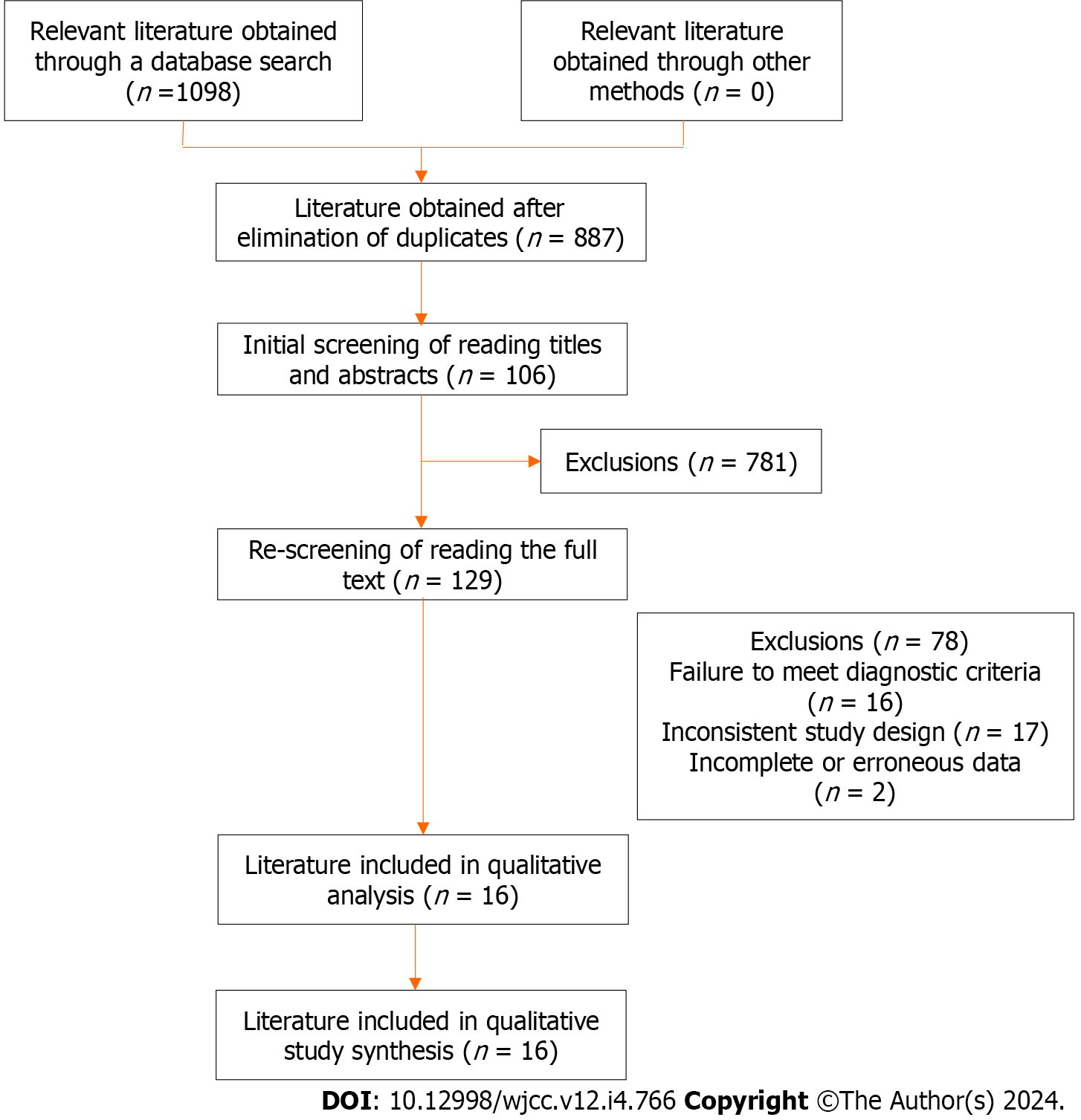
A total of 1098 relevant articles were searched, among which 16 were included in the study after screening. The screening process is shown in Figure 1.
Relevant literature obtained through a database search (n = 1098); Relevant literature obtained through other methods (n = 0); Literature obtained after elimination of duplicates (n = 887); Initial screening of reading titles and abstracts (n = 106); Exclusions (n = 781); Re-screening of reading the full text (n = 129); Exclusions (n = 78); Failure to meet diagnostic criteria (n = 16); Inconsistent study design (n = 17); Incomplete or erroneous data (n = 2); Literature included in qualitative analysis (n = 16); Literature included in qualitative study synthesis (n = 16).
Eventually, 16 RCTs, published between 2020 and 2023, were included in our study, which involved 1660 HF patients, including 832 patients in the TCM group (TCM combined with CMW treatment) and 828 patients in the CWM group (CWM treatment). The course of treatments ranged from 1 wk to 3 months. Among the included RCTs, 11 trials analyzed TCM syndrome differentiation. Outcome indicators in these trials included comprehensive clinical outcomes, TCM syndrome scores, and BNP levels. The basic characteristics of the included studies are detailed in Table 1.
| Ref. | Syndrome differ classification | n (T/C) | Interventions | Course of treatment | Outcome indicators | |
| T | C | |||||
| Wang et al[13] | Not mentioned | 45/45 | TCM + CWM | CWM | 3 wk | 1,2,3 |
| Leung et al[14] | Qi-Yin deficiency syndrome, Qi-deficiency-blood-stasis syndrome, syndrome of heart-lung Qi deficiency | 63/63 | TCM + CWM | CWM | 3 months | 1,3 |
| Syndrome of water overflowing due to Yang deficiency, syndrome of Yang deficiency of both heart and kidney | ||||||
| Tang et al[15] | Syndrome of paroxysmal stridor with sputum, syndrome of wheezes when sitting, syndrome of pathogenic water attacking heart | 33/33 | TCM + CWM | CWM | 2 wk | 1,2 |
| Wang et al[16] | Syndrome of water overflowing due to Yang deficiency | 30/32 | TCM + CWM | CWM | 8 wk | 1,2,3 |
| Vorovich et al[17] | Syndrome of heart-lung deficiency | 30/30 | TCM + CWM | CWM | 12 wk | 1,2,3 |
| Elkammash et al[18] | Qi-deficiency-blood-stasis syndrome | 98/98 | TCM + CWM | CWM | 2 wk | 1,2,3 |
| Zou et al[19] | Not mentioned | 74/74 | TCM + CWM | CWM | 8 wk | 1,3 |
| Li et al[20] | Yang-deficiency-water-stasis syndrome | 40/40 | TCM + CWM | CWM | 12 wk | 1,3 |
| Guan et al[21] | Not mentioned | 55/55 | TCM + CWM | CWM | 4 wk | 1,3 |
| Li et al[22] | Syndrome of blood stasis and water retention | 46/46 | TCM + CWM | CWM | 1 wk | 1,2,3 |
| Nie et al[23] | Not mentioned | 30/30 | TCM + CWM | CWM | 2 wk | 1 |
| Zhang et al[24] | Qi-deficiency-blood-stasis syndrome | 42/42 | TCM + CWM | CWM | 2 wk | 1 |
| Li et al[25] | Not mentioned | 100/100 | TCM + CWM | CWM | 2 wk | 1 |
| Greene et al[26] | Qi-Yin deficiency syndrome | 45/45 | TCM + CWM | CWM | 2 wk | 1 |
| Wilcox et al[27] | Heart failure with Qi-Yin deficiency syndrome | 53/53 | TCM + CWM | CWM | 4 wk | 1 |
| Chen et al[28] | Syndrome of qi deficiency of heart and kidney, syndrome of blood stasis and water retention | 45/45 | TCM + CWM | CWM | 8 wk | 1,3 |
The results of the assessment are depicted in Figure 2. In terms of randomized sequence generation, 12 RCTs were low risk, whilst the remaining 4 RCTs[12-14], where participants were grouped based on "different treatment regimens", were classified as high risk. Regarding allocation concealment, none of the 16 RCTs mentioned the implementation of allocation concealment. As for blinding of participants and implementers, all of the 16 RCTs did not report the implementation of blinding, which were classified as high risk since the measurement of the outcome indicators could be affected by their subjective nature. With respect to blinding of outcome assessors, all of the 16 RCTs did not report the implementation of blinding and were assessed as unclear risk. For incomplete outcome data, all trials were classified as low risk because of the absence of incomplete outcome data. With regard to selective outcome reporting, all trials were assessed as unclear risk because of the absence of selective outcome reporting. Concerning other biases, all trials were classified as unclear risk because of no report of other biases.
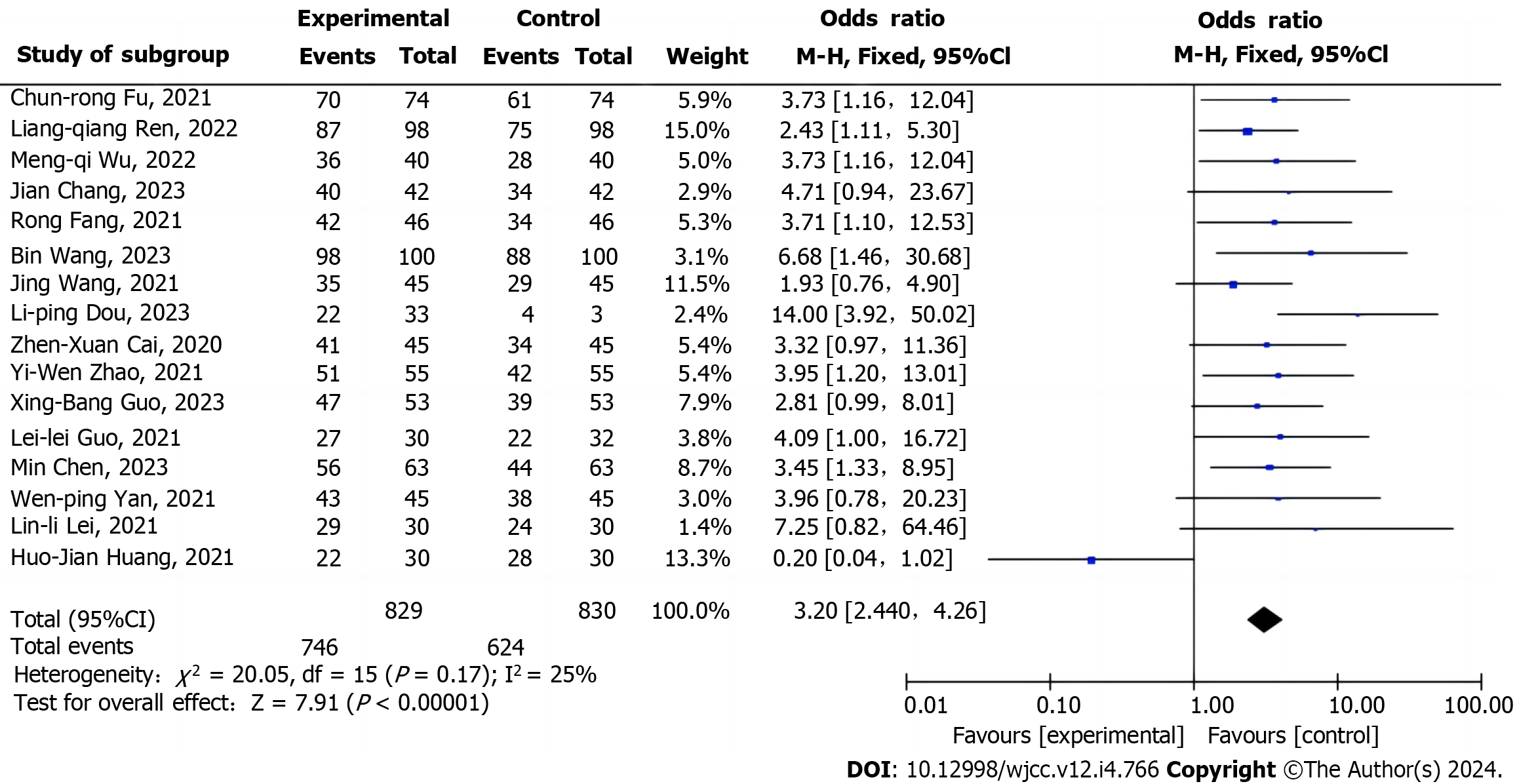
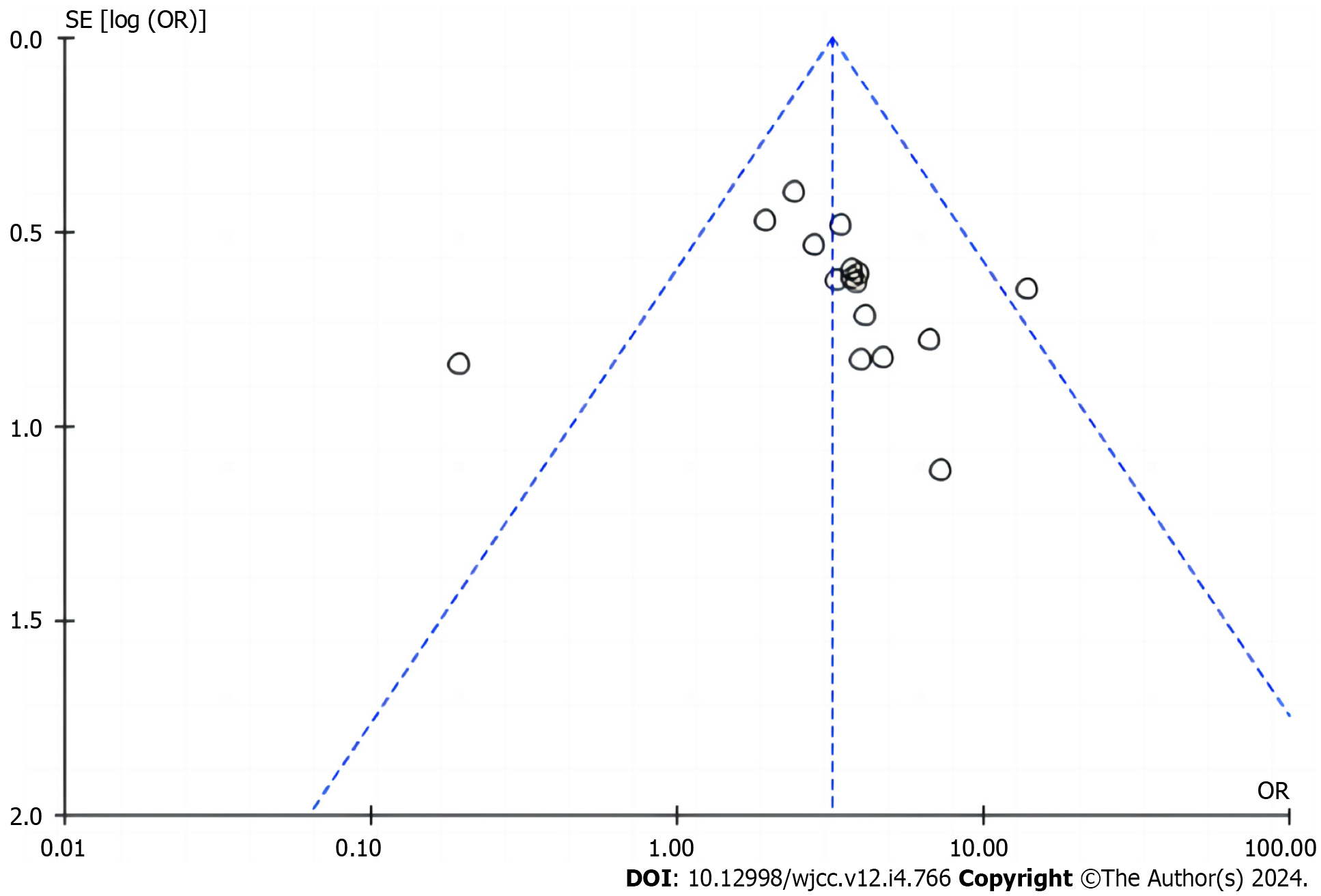
Comprehensive clinical outcomes: Comprehensive clinical outcomes were analyzed in all 16 trials[15-17], and the heterogeneity test showed no significant heterogeneity among trials (P = 0.17, I2 = 25%). Therefore, the fixed-effects model was chosen for analysis[18]. The results unveiled a marked difference between the two groups (RR = 3.20; 95%CI = 2.40, 4.26; P < 0.00001), indicating that TCM combined with CWM treatment could improve the comprehensive clinical outcomes of patients (Figure 3). The funnel plot was asymmetric, highlighting the presence of publication biases (Figure 4).
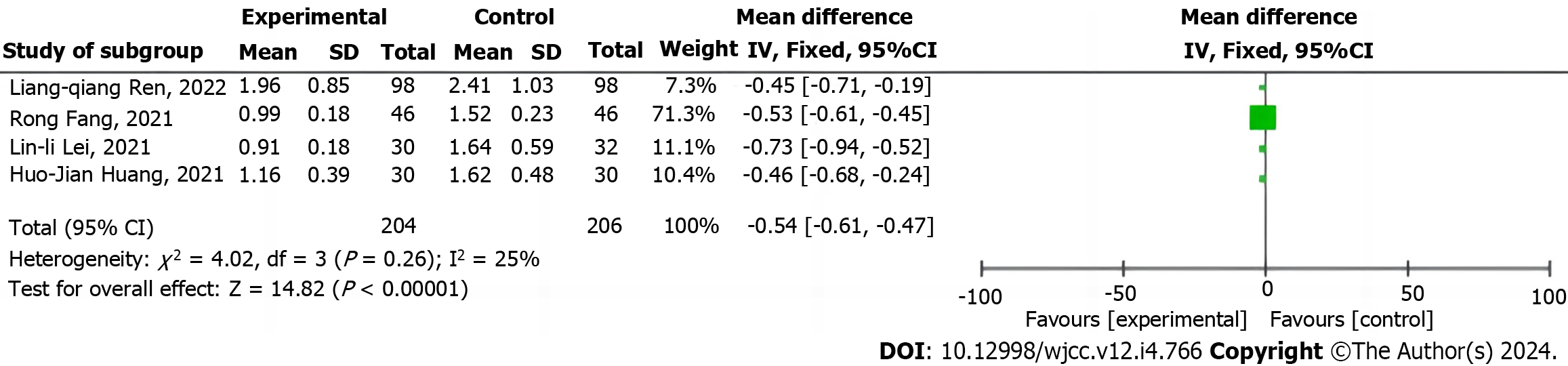
TCM syndrome scores: Six studies[12,14-17,19] reported TCM syndrome scores. Because of obvious heterogeneity among studies (P < 0.00001, I2 = 98%), sensitivity analysis was carried out to clarify the source of heterogeneity, which displayed that the heterogeneity was reduced after two RCTs[13,15] were discarded (P = 0.26, I2 = 25%). After the article was read, it was found that this result might be due to differences in the sub-item of statistics. Therefore, the remaining 4 items were subjected to analysis with the fixed-effects model. The results demonstrated a substantial difference between the two groups (WMD = -0.54; 95%CI = -0.61, -0.47; P < 0.00001), illustrating that the combination of TCM and CWM treatment could reduce the TCM syndrome score of HF patients (Figure 5).
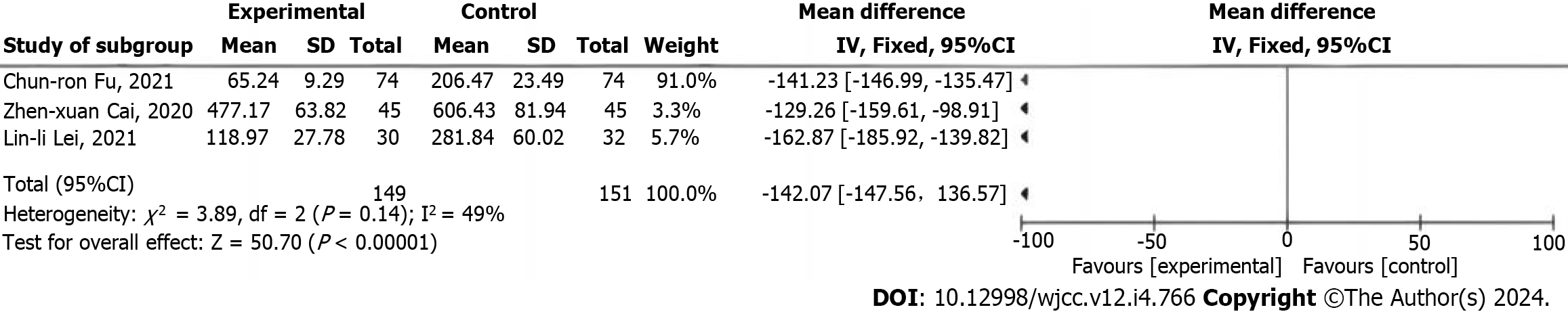
BNP levels: Trials[20-25] analyzed BNP levels. Since the heterogeneity test unraveled that the heterogeneity among studies was obvious (P < 0.00001, I2 = 99%), sensitivity analysis was performed. The results presented that exclusion of seven trials[12,13,15-17] triggered a decline in the heterogeneity (P = 0.14, I2 = 49%). After reading the article, we found that this result might be attributed to differences in treatment course. Hence, a fixed-effects model was selected for analyzing the remaining three trials. The findings exhibited a prominent difference between the two groups (WMD =
Rating of quality of evidence: The GRADE criteria were utilized for rating the quality of the evidence. In detail, trials reporting that "TCM improves comprehensive clinical outcomes" were rated as low-quality evidence, and those revealing that "TCM lowers TCM syndrome scores" or that "TCM reduces BNP levels" were rated as medium-quality evidence (Table 2).
| Outcome indicators | Number of trials (practice/sample size) | Analysis results | Limitation | Inconsistency | Indirectness | Inaccuracy | Publication biases | Quality of evidence |
| Improving comprehensive clinical outcomes | 16 (1294/1659) | RR = 3.20; 95%CI = 2.40, 4.26; P < 0.00001 | Downgrade by one level1 | No | No | No | Downgrade by one level3 | Low |
| Lowering TCM syndrome scores | 4 (400) | WMD = -0.54; 95%CI = -0.61, -0.47, P < 0.00001 | Downgrade by one level1 | No | No | Downgrade by half a level2 | Not found | Medium |
| Reducing BNP levels | 3 (300) | WMD = -142.07, 95%CI = -147.56, -136.57, P < 0.00001 | Downgrade by one level1 | No | No | Downgrade by half a level2 | Not found | Medium |
HF is the inability of the heart to pump a blood supply required for venous return and tissue metabolism at a time. Specifically, the reduced contractility of the myocardium triggered by multiple diseases generally diminishes blood output and fails to satisfy the needs of the body, resulting in a range of symptoms[26]. HF does not occur independently and, contrarily, is a relatively severe condition with numerous causes, which has similar incidence and mortality rates to cancers. HF is initially caused by myocardial damage and stress effects. Furthermore, many causes can increase the burden on the diseased heart, thus inducing HF[27]. Currently, this disease is still treated by targeting symptoms, comorbidities, and risk factors, and the improvement and rational evaluation of therapies are the focus of current research. According to TCM, HF is a syndrome of deficiency Ben and excessive Biao, with the deficiency of the heart Qi and heart Yang as Ben and blood stasis and pattern of phlegm-rheum collecting internally as Biao. Therefore, this disease should be treated by targeting both Biao and Ben through flexible use of tonifying deficiency, warming Yang, invigorating blood circulation, and relieving diuresis according to deficiency and excess[28]. Although several studies systematically evaluated the efficacy of TCM in the treatment of HF, there are few comprehensive analyses of outcome indicators in HF patients treated with TCM. Intriguingly, the present study comprehensively analyzed comprehensive clinical outcomes, TCM syndrome scores, and BNP levels to evaluate the efficacy of TCM, complementing the existing evaluations.
Our results revealed that TCM combined with CWM treatment was effective in improving the comprehensive clinical outcomes, TCM syndrome scores, and BNP level of HF patients, and the sensitivity analysis exhibited that the above conclusions were stable. Based on the GRADE criteria, the quality of evidence was low to medium, indicating that the above conclusions should be applied with caution. Accordingly, high-quality clinical trials are still warranted for verification.
Of course, this meta-analysis has several limitations. First, most of the included trials had small sample sizes, and most of them had the problems of the lack of allocation concealment and blinding, which must have affected the reliability of the results. Second, although it was found that TCM improved TCM syndrome scores, only 4 of the 16 included trials analyzed TCM syndrome scores, which resulted in a certain bias, and may have an effect on the evaluation of the efficacy of TCM. Third, although 10 of the 16 included trials analyzed BNP levels, 3 trials were discarded after sensitivity analysis, which led to a certain bias in the included trials.
To optimize the reliability of the evidence, trials should be designed strictly according to the RCT format. During the trial, it should focus on the feasibility of the outcome indicators and the development of a reasonable follow-up program. In the future, outcome indicators that better reflect the characteristics of TCM should be evaluated to provide high-quality evidence for TCM interventions.
In conclusion, our study reveals that the integration of TCM with CWM significantly improves comprehensive clinical outcomes, TCM syndrome scores, and BNP levels in HF patients. Nevertheless, the inherent biases due to design flaws in the original studies underscore the need for more rigorously designed RCTs. Such studies are essential to provide a robust, evidence-based foundation for clinical decision-making in this area.
Heart failure (HF) is a cardiovascular condition with significant morbidity and mortality. While traditional Chinese medicine (TCM) is often used as a complementary approach for HF management, there is a lack of systematic evaluations on its impact. This study aims to fill this gap by analyzing randomized controlled trials (RCTs) focusing on TCM for HF treatment. The study assesses methodological quality, performs a meta-analysis, and evaluates evidence quality based on established standards. The results provide valuable insights into the potential advantages and limitations of TCM in managing HF. However, caution is advised due to the low and medium quality of the included RCTs, necessitating further high-quality research for confirming effectiveness.
The main motivation behind this research is the need for systematic evaluations of the impact of TCM on HF management. Despite its common use as a complementary approach, there is a lack of comprehensive studies analyzing the effects of TCM on clinical outcomes, TCM syndrome scores, and B-type natriuretic peptide (BNP) levels in HF patients. By conducting a meta-analysis of RCTs, this study aims to bridge this gap and provide valuable insights into the potential advantages and limitations of TCM in HF management. The findings will guide future research and contribute to the understanding of TCM's role in HF treatment.
The main objectives of this study were to systematically analyze the effects of TCM on clinical comprehensive outcomes, TCM syndrome scores, and BNP levels in HF patients. The study aimed to evaluate the quality of evidence for these trials by conducting a meta-analysis of RCTs. The objectives were realized through the retrieval and inclusion of relevant RCTs, assessment of methodological quality, meta-analysis using appropriate software, and rating of evidence quality based on established criteria. Realizing these objectives provided valuable insights into the effectiveness of TCM as a complementary therapy for HF and highlighted the need for further high-quality research in this field.
This study utilized a systematic search across Chinese and English databases to identify relevant RCTs on TCM for heart failure treatment. Methodological quality assessment employed the Cochrane risk-of-bias tool, while meta-analysis and publication bias evaluation were conducted using RevMan 5.3 software. The quality of evidence was appraised using GRADE criteria. A total of 16 RCTs involving 1660 HF patients were included, with a comprehensive analysis of clinical outcomes, TCM syndrome scores, and BNP levels. Novelty lies in the comprehensive nature of the analysis, providing crucial insights into the potential benefits and limitations of TCM in managing HF.
The meta-analysis of 16 RCTs revealed that the combination of TCM with conventional Western medicine (CWM) effectively improved comprehensive clinical outcomes, decreased TCM syndrome scores, and reduced BNP levels in patients with HF. The differences between the TCM and CWM groups were statistically significant for all three outcome measures. However, the overall quality of evidence was rated as low to medium due to the limitations of the included RCTs. These findings contribute valuable insights into the potential benefits of TCM in HF management, highlighting the need for further high-quality research in this field.
This study concludes that the combination of TCM with CWM treatment effectively improves comprehensive clinical outcomes, reduces TCM syndrome scores, and decreases BNP levels in HF patients. However, it is important to exercise caution when applying these results due to the low and medium quality of the included RCTs. This study fills the gap in systematic evaluations of TCM's impact on HF management by providing crucial insights into the potential advantages and constraints of TCM. Further research utilizing high-quality RCTs is needed to validate these findings.
Future research should focus on conducting high-quality RCTs with larger sample sizes and longer follow-up periods to establish the efficacy and safety of TCM in HF management. Additionally, investigations into the mechanisms underlying TCM's effects on comprehensive clinical outcomes, TCM syndrome scores, and BNP levels are crucial. It is essential to explore TCM's potential role as a standalone or complementary therapy and to address the limitations identified in this study to provide more robust evidence for TCM's application in HF treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zelano J, Sweden S-Editor: Gong ZM L-Editor: A P-Editor: Zhao S
| 1. | Arrigo M, Jessup M, Mullens W, Reza N, Shah AM, Sliwa K, Mebazaa A. Acute heart failure. Nat Rev Dis Primers. 2020;6:16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 309] [Article Influence: 61.8] [Reference Citation Analysis (0)] |
| 2. | Castiglione V, Aimo A, Vergaro G, Saccaro L, Passino C, Emdin M. Biomarkers for the diagnosis and management of heart failure. Heart Fail Rev. 2022;27:625-643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 220] [Article Influence: 55.0] [Reference Citation Analysis (0)] |
| 3. | Savarese G, Stolfo D, Sinagra G, Lund LH. Heart failure with mid-range or mildly reduced ejection fraction. Nat Rev Cardiol. 2022;19:100-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 226] [Article Influence: 75.3] [Reference Citation Analysis (0)] |
| 4. | Zhou Q, Qin WZ, Liu SB, Kwong JS, Zhou J, Chen J. Shengmai (a traditional Chinese herbal medicine) for heart failure. Cochrane Database Syst Rev. 2014;CD005052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Liang B, Yan C, Zhang L, Yang Z, Wang L, Xian S, Lu L. The Effect of Acupuncture and Moxibustion on Heart Function in Heart Failure Patients: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2019;2019:6074967. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Wu YJ, Wang ZB, Li Y, Wang DP, Miao L, Ren JG, Pan YH, Liu JX. [Chronic heart failure due to Qi deficiency and blood stasis and intervention mechanism of Compound Renshen Buqi Granules:a proteomics-based study]. Zhongguo Zhong Yao Za Zhi. 2021;46:5052-5063. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Ramani GV, Uber PA, Mehra MR. Chronic heart failure: contemporary diagnosis and management. Mayo Clin Proc. 2010;85:180-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 154] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 8. | Wang X, Zhang C; Cardiovascular Group, Geriatrics Branch, Chinese Medical Association; Editing Group of the Chinese Expert Consensus on the Diagnosis and Treatment of Chronic Heart Failure in Elderly Patients. Chinese expert consensus on the diagnosis and treatment of chronic heart failure in elderly patients (2021). Aging Med (Milton). 2022;5:78-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Evidence Based Medicine Committee Affiliated to China International Exchange and Promotion Association for Medical and Healthcare; Committee Geriatric Medicine Affiliated to Cross-straits Medicine Exchange Association. Chinese expert consensus on biomarkers for heart failure. Zhonghua Jianyan Yixue Zazhi. 2020;43:130-141. [DOI] [Full Text] |
| 10. | Masoudi FA, Rumsfeld JS, Havranek EP, House JA, Peterson ED, Krumholz HM, Spertus JA; Cardiovascular Outcomes Research Consortium. Age, functional capacity, and health-related quality of life in patients with heart failure. J Card Fail. 2004;10:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 167] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 11. | Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews for Interventions, Version5.1.0, 2011; 12: 12-13. |
| 12. | Hu Y, Jiang J, Xu L, Wang C, Wang P, Yang B, Tao M. Symptom clusters and quality of life among patients with chronic heart failure: A cross-sectional study. Jpn J Nurs Sci. 2021;18:e12366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Wang Y, Wang Q, Li C, Lu L, Zhang Q, Zhu R, Wang W. A Review of Chinese Herbal Medicine for the Treatment of Chronic Heart Failure. Curr Pharm Des. 2017;23:5115-5124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 14. | Leung AYL, Chen H, Jia Z, Li X, Shen J. Study protocol: Traditional Chinese Medicine (TCM) syndrome differentiation for heart failure patients and its implication for long-term therapeutic outcomes of the Qiliqiangxin capsules. Chin Med. 2021;16:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Tang Q, Wang Y, Li K. Zhenwu decoction for chronic heart failure: Protocol for a systematic review and meta-analysis. Medicine (Baltimore). 2018;97:e11559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Wang C, Zhang Y, Gong LH. [Treatment of chronic heart failure by shencao tongmai granule: a multi-centered, double-blinded, randomized, parallel controlled trial]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2012;32:612-615. [PubMed] |
| 17. | Vorovich EE, Chuai S, Li M, Averna J, Marwin V, Wolfe D, Reilly MP, Cappola TP. Comparison of matrix metalloproteinase 9 and brain natriuretic peptide as clinical biomarkers in chronic heart failure. Am Heart J. 2008;155:992-997. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Elkammash A, Tam SSC, Yogarajah G, You J. Management of Heart Failure With Preserved Ejection Fraction in Elderly Patients: Effectiveness and Safety. Cureus. 2023;15:e35030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Zou X, Pan GM, Sheng XG, Yao GZ, Zhu MJ, Wu Y, Chen XH, Wang YX, Cui J, Chen JD. [Effect of clinical pathways based on integrative medicine for patients with chronic heart failure: a multi-center research]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2013;33:741-746. [PubMed] |
| 20. | Li Y, Wu H, Zhang B, Xu X, Wang Y, Song Q. Efficacy and safety of Linggui Zhugan decoction in the treatment of chronic heart failure with Yang deficiency: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e26012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Guan H, Dai G, Ren L, Gao W, Fu H, Zhao Z, Liu X, Li J. Efficacy and safety of Qishen Yiqi dripping pills as a complementary treatment for Heart Failure: A protocol of updated systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e24285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Li Z, Liu M, Chen M, Luo G, Wu J, Mazhar M, Yang F, Zheng Y, Wu H, Wu Q, Yang S. Clinical effect of Danshen decoction in patients with heart failure: A systematic review and meta-analysis of randomized controlled trials. PLoS One. 2023;18:e0284877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 23. | Nie H, Li S, Liu M, Zhu W, Zhou X, Yan D. Yiqi Fumai Injection as an Adjuvant Therapy in Treating Chronic Heart Failure: A Meta-Analysis of 33 Randomized Controlled Trials. Evid Based Complement Alternat Med. 2020;2020:1876080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Zhang X, Kang J, Zhang J, Chen Y, Dai H, Hu M, Liu Y, Shang H. Effectiveness of Yiqi Fumai lyophilized injection for acute heart failure: Rationale and design of the AUGUST-AHF cohort study. Front Cardiovasc Med. 2022;9:1074406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 25. | Li Z, Zhang Y, Yuan T. Clinical efficacy and safety of nuanxin capsule for chronic heart failure: A systematic review and meta-analysis. Medicine (Baltimore). 2018;97:e11339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Greene SJ, Bauersachs J, Brugts JJ, Ezekowitz JA, Lam CSP, Lund LH, Ponikowski P, Voors AA, Zannad F, Zieroth S, Butler J. Worsening Heart Failure: Nomenclature, Epidemiology, and Future Directions: JACC Review Topic of the Week. J Am Coll Cardiol. 2023;81:413-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 120] [Reference Citation Analysis (0)] |
| 27. | Wilcox JE, Fang JC, Margulies KB, Mann DL. Heart Failure With Recovered Left Ventricular Ejection Fraction: JACC Scientific Expert Panel. J Am Coll Cardiol. 2020;76:719-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 197] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 28. | Chen J, Wei X, Zhang Q, Wu Y, Xia G, Xia H, Wang L, Shang H, Lin S. The traditional Chinese medicines treat chronic heart failure and their main bioactive constituents and mechanisms. Acta Pharm Sin B. 2023;13:1919-1955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 49] [Reference Citation Analysis (0)] |