Published online Dec 16, 2024. doi: 10.12998/wjcc.v12.i35.6834
Revised: August 21, 2024
Accepted: September 13, 2024
Published online: December 16, 2024
Processing time: 125 Days and 7.8 Hours
Gastrointestinal lymphoma typically arises in the stomach, small bowel, or colorectum and is usually a B-cell lymphoma. However, primary T-cell lymp
We report a 63-year-old male presenting with epigastric pain. Esophagogastro
This case highlights the necessity of considering PTCL-NOS in differential diag
Core Tip: Gastrointestinal lymphoma is an extranodal malignancy primarily arising in the stomach, small intestine, or colorectum, most commonly presenting as B-cell lymphoma. In contrast, primary T-cell lymphomas of the stomach are exceedingly rare, particularly within the spectrum of T-cell lymphoma subtypes. Among these, gastric peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS) is extremely rare. In this report, we present a rare case of a 63-year-old male diagnosed with gastric PTCL-NOS, along with a detailed examination of the clinicopathological features.
- Citation: Jang HR, Lee K, Lim KH. Rare primary gastric peripheral T-cell lymphoma not otherwise specified: A case report. World J Clin Cases 2024; 12(35): 6834-6839
- URL: https://www.wjgnet.com/2307-8960/full/v12/i35/6834.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i35.6834
Gastrointestinal (GI) lymphoma is the most common extranodular lymphoma, accounting for 30%-40% of all extranodular lymphoma, and has distinct clinical and pathological characteristics[1,2]. More than 80% of the GI lymphomas are B-cell lymphomas. The stomach is the most commonly affected site for GI lymphoma, followed by the small bowel, colorectum, and esophagus[3,4]. The majority of primary gastric lymphoma cases are B-cell lymphomas, while T-cell lymphomas are known to be rare. The incidence of primary gastric T-cell lymphoma (PG-TCL) is estimated to be excep
To the best of our knowledge, primary gastric PTCL-NOS have been rarely reported. Therefore, we present a gastric PTCL-NOS case and describe its clinic-pathological and endoscopic features.
A 63-year-old male was admitted to Kangwon National University Hospital with a 3-week history of epigastric pain.
The patient denied weight loss and febrile sense. Physical examination revealed that his abdomen was soft without tenderness or rebound tenderness.
The patient denied any significant past medical history.
The patient's personal and family history had no notable findings.
The physical examination revealed that the patient’s abdomen was soft. It was not tender. Rebound tenderness was not observed.
Blood test results revealed that white blood cell count, hemoglobin, and platelet count were within normal ranges. However, lactate dehydrogenase level was slightly elevated at 244 U/L (reference range: 119-229 U/L).
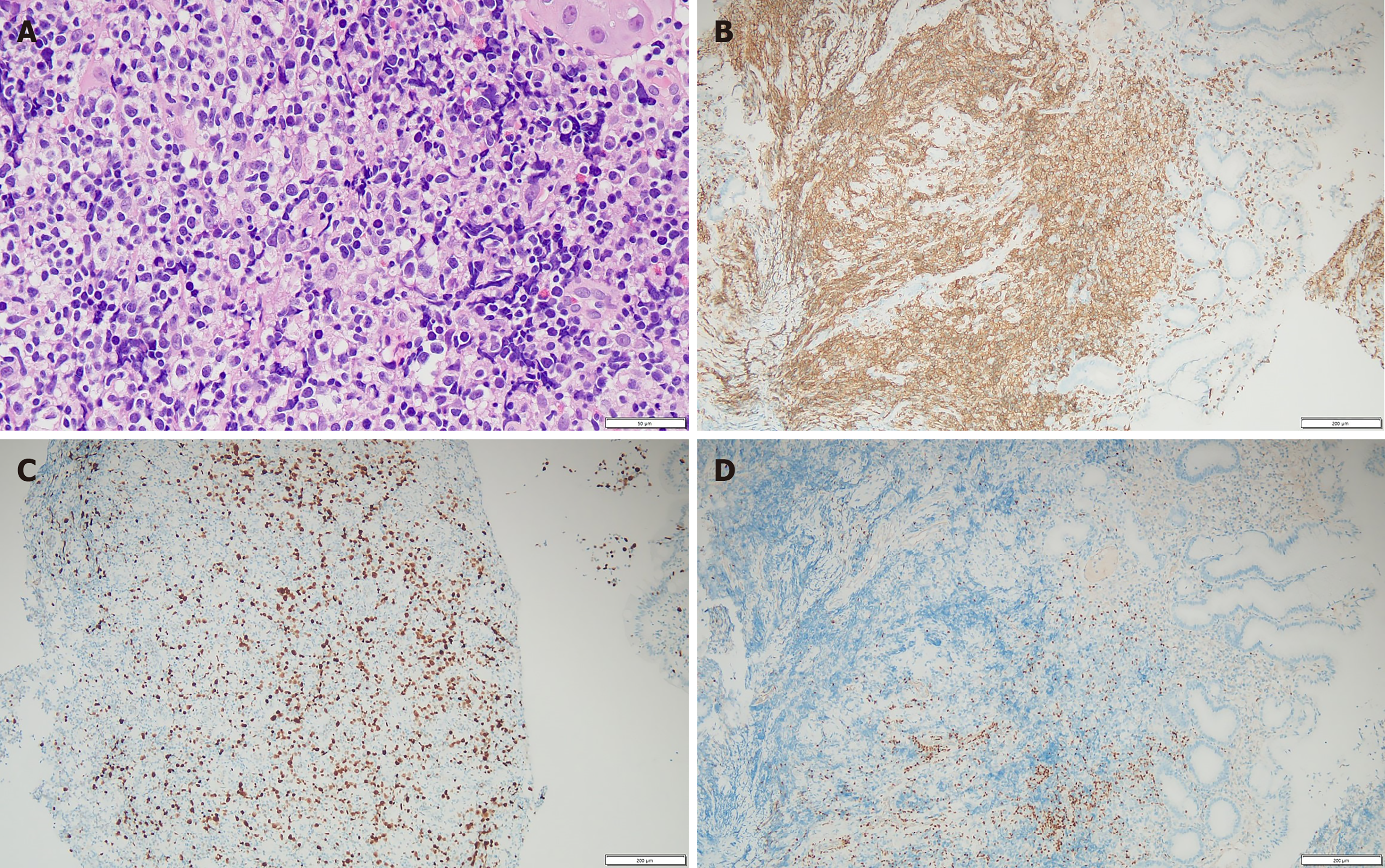
In hematoxylin and eosin staining of the stomach tissue, majority of malignant cells were intermediate to large-sized abnormal lymphoid cells. Characteristics commonly found in gastric carcinomas, such as intestinal dysplasia, cylindrical epithelial cells, and prominent intracytoplasmic mucin vacuoles, were not detected in this case. A pan-cytokeratin immunohistochemistry (IHC) test yielded a negative result, ruling out gastric carcinoma. Tests for CD20, PAX5, CD10, and Bcl-6 also returned negative results, excluding the possibility of B-cell lineage lymphoma. CD3, CD5, CD7, and CD4 were expressed positively (Figure 1). These cells also exhibited a relatively elevated Ki-67 proliferation index (30%). The T-cell receptor gamma gene rearrangement test demonstrated a positive result. Pathological findings were indicative of high-grade T-cell lymphoma. Further IHC tests were conducted to differentiate between various subtypes of T-cell lymphoma, including NK/T-cell lymphoma, EATL, monomorphic epitheliotropic intestinal T-cell lymphoma, angioimmunoblastic T-cell lymphoma, ALCL, and PTCL-NOS. However, CD30, ALK (D5F3), CD56, granzyme B, and Epstein-Barr virus all showed negative results.
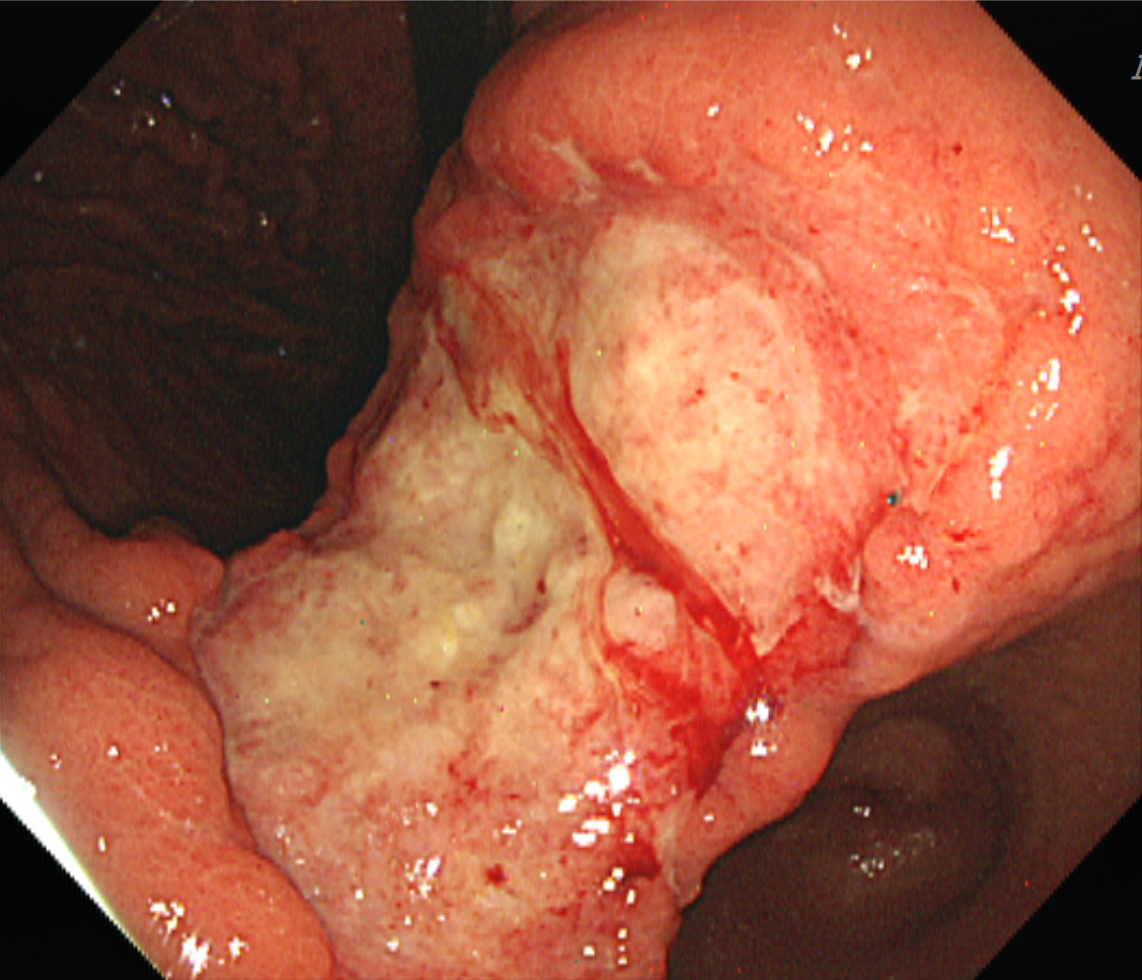
To investigate the cause of the patient's primary symptom, an esophagogastroduodenoscopy was first performed, re
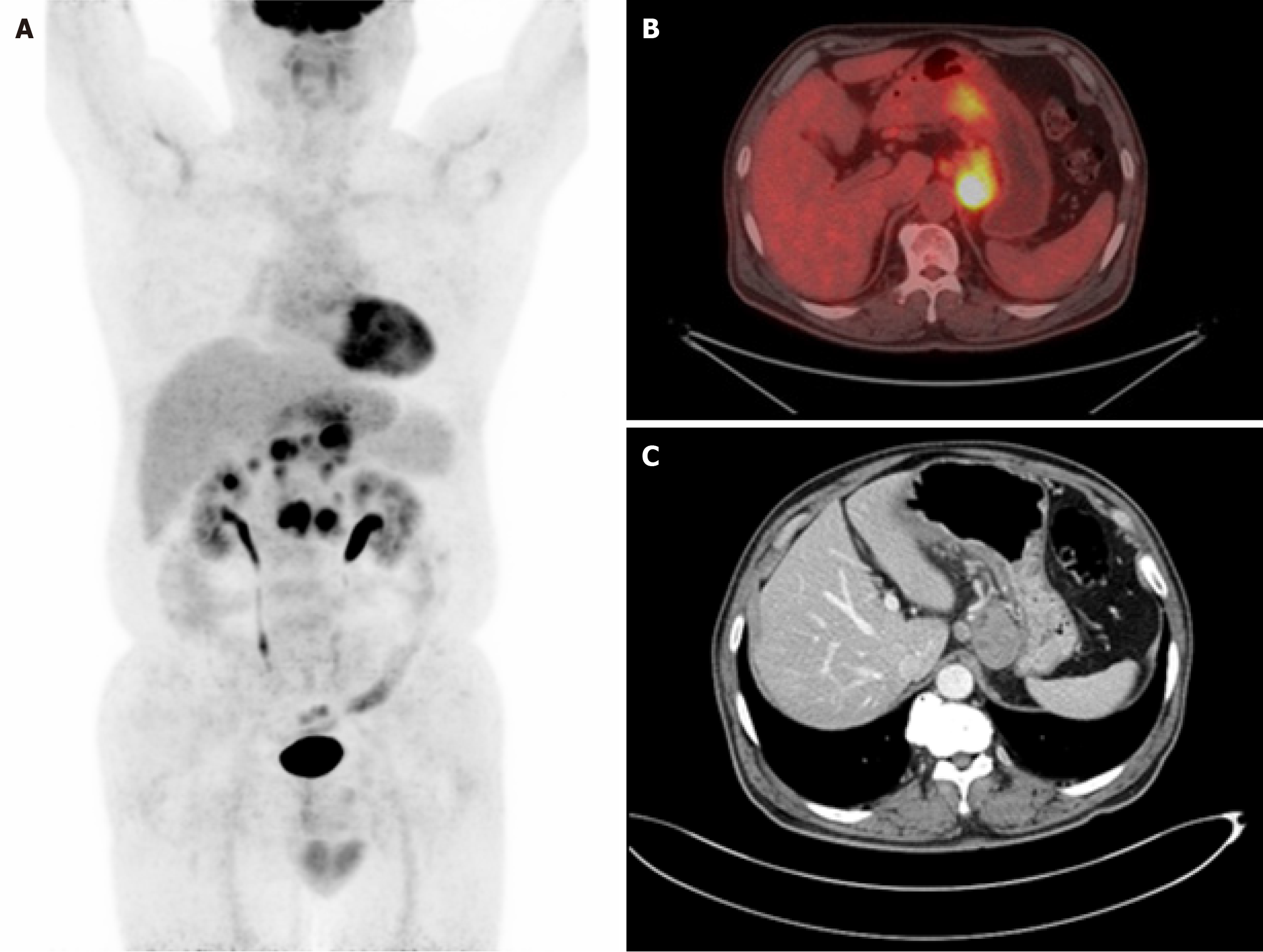
After confirmation of the biopsy result, to determine the stage of the lymphoma, the patient underwent imaging tests, including abdominal and pelvic computed tomography (CT) scans and 18F-fluorodeoxyglucose-positron emission tomography/CT scans (Figure 3). These imaging studies showed the involvement of stomach and intra-abdominal lymph nodes.
Based on these findings, the patient received a diagnosis of PTCL-NOS, meeting the diagnostic criteria for intestinal T-cell lymphoma, not otherwise specified based on the revised World Health Organization 2018 classification.
The patient underwent a bone marrow examination, which confirmed that there was no lymphoma involvement in the bone marrow. The final staging was determined to be stage II. The patient received a total of six cycles of chemotherapy with cyclophosphamide, doxorubicin, vincristine, prednisone, and etoposide.
The patient did not experience any significant complications or treatment-related adverse events throughout the chemo
Primary gastric PTCL-NOS is a rare subtype of lymphoma. As a result, report about its prevalence is limited. Among several subtypes of T-cell lymphoma, EATL appears to be the most common subtype of gastric T-cell lymphoma according to several studies. It has been reported that EATL accounts for 12%-40% of all gastric T-cell lymphomas[6,7].
In a study on primary GI lymphoma conducted in China, 415 patients with primary GI lymphoma were identified between 1998 and 2013. Among these cases, T-cell lymphoma was reported in approximately 60 cases. Specifically, PG-TCL was reported in about 7 cases[6]. The study from China provided limited information regarding specific subtypes of T-cell lymphoma. According to SEER data analysis, from 1965 to 2016, a total of 164 patients with PG-TCL were analyzed. The age-adjusted occurrence rate of PG-TCL stood at 0.0091 per 100000 person-years and demonstrated an increase in frequency as age advanced. This incidence rate is about 1/20000 of the incidence rate of B-cell lymphoma. The present report also showed that its occurrence varied depending on ethnicity and geographic location. Patients with primary gastric PTCL-NOS showed distinctive clinical characteristics such as younger age at disease onset, higher incidence among males, less prevalence among white race, advanced disease stage, and frequent presence of symptom B. Fur
The optimal management for primary gastric PTCL-NOS has not been established yet. Although there was no specific research exclusively focusing on PTCL-NOS, retrospective studies related to the treatment of T-cell lineage gastric ly
| Ref. | Study period (year) | Study type | Sample size | Patients with gastric peripheral T-cell lymphoma-not otherwise specified | Patient demographics | Treatment | Outcomes |
| Park et al[9] | 1990-2004 | Primary gastric lymphoma of T-cell origin | 17 | 7 (41.1) | Median age 49 years, male (14 : 3) | CHOP, cyclophosphamide, doxorubicin, vincristine, prednisone, and etoposide, Vanderbilt regimen, surgical resection | Median progression-free survival 10 months, median OS 12 months |
| Kim et al[8] | 1995-2008 | Endoscopic and clinical analysis of primary T-cell lymphoma of the GI tract | 36 | 5 (13.9) | Median age 50 years, male to female ratio 2.6:1 | Of the 36 patients, primary surgical resection with chemotherapy (55%), primary chemotherapy without surgery (45%) | Median OS 7.8 months, 3-year survival rate 19.4% |
| Kohri et al[10] | 2007-2018 | Peripheral T-cell lymphoma with GI involvement | 11 | 2 (2.4) | Median age 75 years, 10 males and 1 female | CHOP | OS 7 months and 83 months (2 patients) |
| Zhang et al[5] | 1975-2016 | Gastric T-cell lymphoma in the SEER program | 164 | 104 (63.4) | Median age 65 years, mostly White and male | Chemotherapy, surgery, radiotherapy | Median OS 8 months, 5-year OS 23.5% |
Primary gastric PTCL-NOS is rare, as it is typically found in other organs such as the small bowel rather than the stomach. B-cell lymphomas are more commonly associated with gastric involvement. However, in cases where gastric lymphoma is suspected, despite its low incidence, it is crucial to conduct appropriate testing for the diagnosis of T-cell lymphoma, known to have a poor prognosis. This approach can provide valuable insights and guide appropriate treat
We present a case of gastric PTCL-NOS, a condition that is seldom discussed in relation to it endoscopic findings and the process of pathological differential diagnosis. This case is notable due to the rarity of gastric PTCL-NOS.
| 1. | Bautista-Quach MA, Ake CD, Chen M, Wang J. Gastrointestinal lymphomas: Morphology, immunophenotype and molecular features. J Gastrointest Oncol. 2012;3:209-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 62] [Reference Citation Analysis (0)] |
| 2. | Groves FD, Linet MS, Travis LB, Devesa SS. Cancer surveillance series: non-Hodgkin's lymphoma incidence by histologic subtype in the United States from 1978 through 1995. J Natl Cancer Inst. 2000;92:1240-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 371] [Cited by in RCA: 351] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 3. | Peng JC, Zhong L, Ran ZH. Primary lymphomas in the gastrointestinal tract. J Dig Dis. 2015;16:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Morton JE, Leyland MJ, Vaughan Hudson G, Vaughan Hudson B, Anderson L, Bennett MH, MacLennan KA. Primary gastrointestinal non-Hodgkin's lymphoma: a review of 175 British National Lymphoma Investigation cases. Br J Cancer. 1993;67:776-782. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 95] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Zhang M, Xiao F, Lin M, Chen M, Hou J, Huang H. The epidemiology and prognosis of patients with primary gastric T-cell lymphoma in the SEER program. Cancer Med. 2023;12:84-98. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Chen Y, Chen Y, Chen S, Wu L, Xu L, Lian G, Yang K, Li Y, Zeng L, Huang K. Primary Gastrointestinal Lymphoma: A Retrospective Multicenter Clinical Study of 415 Cases in Chinese Province of Guangdong and a Systematic Review Containing 5075 Chinese Patients. Medicine (Baltimore). 2015;94:e2119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Tse E, Gill H, Loong F, Kim SJ, Ng SB, Tang T, Ko YH, Chng WJ, Lim ST, Kim WS, Kwong YL. Type II enteropathy-associated T-cell lymphoma: a multicenter analysis from the Asia Lymphoma Study Group. Am J Hematol. 2012;87:663-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 8. | Kim DH, Lee D, Kim JW, Huh J, Park SH, Ha HK, Suh C, Yoon SM, Kim KJ, Choi KD, Ye BD, Byeon JS, Song HJ, Jung HY, Yang SK, Kim JH, Myung SJ. Endoscopic and clinical analysis of primary T-cell lymphoma of the gastrointestinal tract according to pathological subtype. J Gastroenterol Hepatol. 2014;29:934-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Park YH, Kim WS, Bang SM, Lee SI, Kang HJ, Na II, Yang SH, Lee SS, Uhm JE, Kwon JM, Kim K, Jung CW, Park K, Ko YH, Ryoo BY. Primary gastric lymphoma of T-cell origin: clinicopathologic features and treatment outcome. Leuk Res. 2006;30:1253-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Kohri M, Tsukasaki K, Akuzawa Y, Tanae K, Takahashi N, Saeki T, Okamura D, Ishikawa M, Maeda T, Kawai N, Matsuda A, Arai E, Arai S, Asou N. Peripheral T-cell lymphoma with gastrointestinal involvement and indolent T-lymphoproliferative disorders of the gastrointestinal tract. Leuk Res. 2020;91:106336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |