Published online Dec 6, 2024. doi: 10.12998/wjcc.v12.i34.6705
Revised: September 1, 2024
Accepted: September 25, 2024
Published online: December 6, 2024
Processing time: 250 Days and 1.2 Hours
Pneumoparotid is a rare disease associated with retrograde airflow into the ductal system. There is no established treatment for this disease, which has no known complications. Mouth puffing and playing wind instruments are known to be the causes of this disease.
We managed a case, in which pneumoparotid suddenly recurred 4 months after surgery for purulent parotiditis. The patient did not report any obvious etiological factors, such as mouth puffing or playing a wind instrument. We reviewed 128 articles (from 1941 to 2023) that reported on a total of 166 patients with pneumoparotid, including the patient from the present case report, with imaging findings. This is the first reported case of pneumoparotid following surgery for purulent parotitis. The etiology in our case was classified as idiopathic.
Imaging findings could be sufficient for accurate pneumoparotid diagnoses and the exclusion of complications; computed tomography could be useful.
Core Tip: Pneumoparotid is a rare disease linked to retrograde airflow into the parotid ductal system, often caused by mouth puffing or playing wind instruments. No established treatment exists, and it typically has no complications. We present a unique case of pneumoparotid recurrence 4 months after surgery for purulent parotitis without typical etiological factors. Our review of 128 articles (1941-2023), involving 166 patients, identified this as the first reported case post-parotitis surgery, classified as idiopathic. Imaging, especially computed tomography, proves crucial for accurate diagnosis and excluding complications.
- Citation: Kubota W, Kyan-Onodera M, Fujimoto Y, Sakuma A, Katada R, Sugiura C. Pneumoparotid with imaging findings: A case report and review of literature. World J Clin Cases 2024; 12(34): 6705-6714
- URL: https://www.wjgnet.com/2307-8960/full/v12/i34/6705.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i34.6705
Edema or discomfort in the parotid region or facial area is a common patient presentation in the daily practice of otolaryngology, oral and maxillofacial surgery, pediatrics, and dentistry. Parotid gland swelling can stem from several underlying factors, such as inflammation, viral infection, sialoliths, benign or malignant tumors, autoimmune disorders, and endocrine abnormalities. Pneumoparotid is a rare cause of swelling and discomfort in the parotid gland area. The term pneumoparotid was first used by Hyrtl and Mundhöhlein 1865 to describe this condition in individuals engaged in playing wind instruments[1]. Until the mid-20th century, pneumoparotid was primarily associated with playing wind instruments and glassmaking. However, in 1915, Hemphill reported a case of a patient who developed self-induced pneumoparotitis in the French Legion of North Africa, which was initially misdiagnosed as mumps[2]. Another case of a patient who developed self-induced pneumoparotid was reported in 1918[3]. Subsequently, several cases of pneumoparotid have been reported worldwide[1-131]. Recently, the incidence of pneumoparotid with an iatrogenic cause (such as dental treatment or continuous positive airway pressure) has been increasing[6,8,11,12,33,51,93,95,98,116,127]. Herein, we report the case of an 83-year-old man who developed pneumoparotid approximately 4 months after undergoing surgery for purulent parotiditis. Although surgical treatments for purulent parotiditis have been performed in numerous patients in the fields of otolaryngology and oral surgery, to the best of our knowledge, no study has reported on the postoperative complications associated with pneumoparotid. As the complications occurred 4 months after surgery in our patient, it can be inferred that the etiology of pneumoparotid was not solely attributable to the surgical procedure but may have involved other contributing factors as well. Herein, we aimed to review previous case reports of this disease and show that objective evaluation using imaging studies and timely and accurate identification of identifying disease etiology are important for its treatment. Computed tomography (CT) may help identify this disease with a high rate of accuracy, highlighting the relevance of this method in this context.
An 83-year-old male patient presented to our hospital with concerns of swelling and crepitus in the left cheek.
The patient’s medical history included hypertension and pacemaker placement due to a complete atrioventricular block.
The patient had undergone surgical intervention in the Dentistry and Oral Surgery department of the Sapporo Tokushukai hospital for the management of Stensen’s duct orifice stenosis resulting from recurrent purulent parotiditis. The patient’s medical history included left suppurative parotitis and abdominal aortic aneurysm surgery. The patient experienced satisfactory postoperative recovery; however, approximately 4 months later, he presented to our hospital with concerns of swelling and crepitus in the left cheek.
The patient denied any occupational or habitual exposure to increased intraoral pressure, such as playing wind instruments or inflating balloons.
The patient’s cheeks were swollen but were neither red nor warm. Palpation of the left cheek revealed the presence of frothy salivary flow (Figure 1).
The patient’s blood test results were normal, lacking any evidence of an inflammatory reaction. Saliva culture results did not show the presence of gas-producing bacteria.
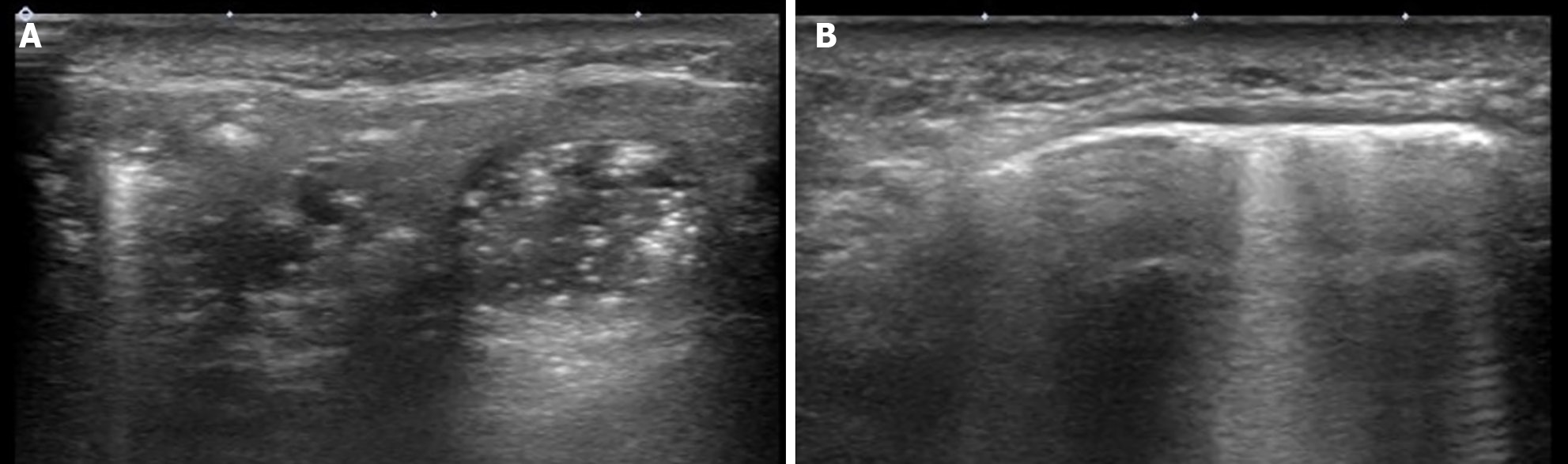
Ultrasound (US) evaluation revealed areas of heightened echogenicity in the left parotid gland and Stensen’s duct, suggesting the presence of air (Figure 2). CT using a 320-row multidetector CT scanner (Aquilion one, Canon, Tokyo, Japan) was performed.
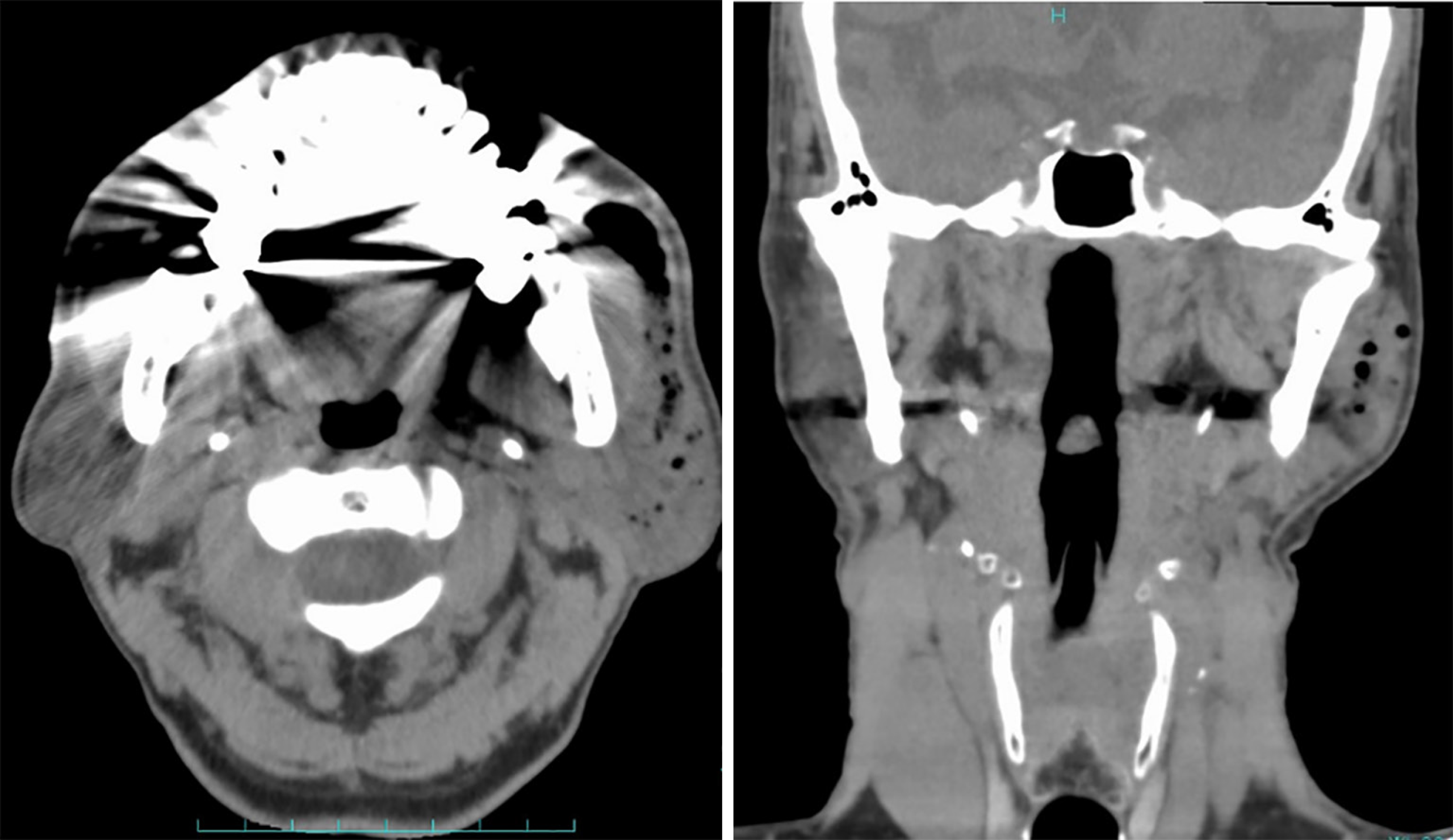
CT (Figure 3) confirmed the presence of swelling accompanied by air accumulation in the left parotid gland and Stensen’s duct, with no evidence of subcutaneous emphysema or pneumomediastinum.
As the patient’s left pneumoparotid was not complicated by infection, conservative treatment was employed, which involved expelling air from the parotid gland through massage.
The patient’s left pneumoparotid persisted after 6 months of follow-up, but with no worsening of swelling, pain, or warmth in the left cheek. Currently, patients with pneumoparotid are required to consult an oral surgeon when symptoms worsen.
Parotid gland swelling is a commonly encountered manifestation in daily clinical practice[4-131]. Considering its various etiologies, including autoimmune diseases, recurrent mumps, sarcoidosis, and parotid tumors, pneumoparotid is a rare and challenging-to-diagnose condition[4,5]. Pneumoparotid occurs when air refluxes through the Stensen’s duct due to increased intraoral pressure, leading to emphysema within the gland and duct[35]. Typically, the mucosal opening of the Stensen’s duct is narrower than that of the parotid duct and has a slit-like structure, which functions to regulate airflow[20]. If pneumoparotid extends beyond the capsule, it can result in subcutaneous emphysema, pneumomediastinum, and rarely, pneumothorax. The diagnosis relies on clinical findings, such as crepitus in the swollen area and the presence of frothy saliva upon parotid gland massage. Moreover, imaging examinations, such as CT and US scanning, are used to confirm the presence of pneumoparotid.
When this condition is suspected, a comprehensive medical interview is necessary to identify the potential factors contributing to the elevated oral pressure. Although glass craftsmen and wind instrument players are commonly affected by this condition, occupation-related cases are rarely reported in Japan. Many cases are associated with abnormal habits, psychogenic factors, balloon inflation, and breath holding. In addition, iatrogenic cases related to dental treatments, respiratory disease management, and medical examinations have been reported recently[6,8,11,12,33,51,93,95,98,116,127]. Moreover, some patients develop pneumoparotid with no evident cause[4,5]. In our case, we speculated that the pneumoparotid was associated with the patient’s medical history because the patient developed pneumoparotid on the same side as the previous surgery. However, it was unlikely to be iatrogenic, given the delayed onset several months postoperatively.
To our knowledge, this is the first study to report on the imaging findings of pneumoparotid. We evaluated the diagnostic contribution of CT scans, US images, and radiographic images, including their ability to detect complications. CT scans were required to adequately assess the complications associated with pneumoparotid in our case. Globally, there have been fewer than 200 reported cases of pneumoparotid, and further large studies are required to determine the standard diagnostic and treatment protocols for this disease.
Given the rarity of this disease and the challenges associated with designing a large study on the diagnosis, treatment of this disease, and pathogenesis, we conducted a literature comprehensive review. The PubMed, Scopus, Web of Science, Business Source Complete, Ovid, Google Scholar, SciElo, LILACS, Japan Centra Revuo Medical database, CiNii, and J-Stage databases were searched using the following keywords "pneumoparotid", "pneumoparotitis", and "pneumoparotide". The total number of records from the databases was 867 (Google Scholar: 267; Business Source Complete: 223; PubMed: 103; Scopus: 85; Web of Science: 66; CiNii: 38; Ovid: 36; Japan Centra Revuo Medical database: 32; J-Stage: 9; SciElo: 4; and LILIACS: 4), and an additional 5 records were obtained from manual searches of relevant papers and books. Duplicate reports and double publications from the same cases and cases without imaging findings were excluded. Supplementary Table 1 summarizes the results of the 128 articles on pneumoparotid.
The authors of some articles did not provide details of the course of treatment and were contacted by electronic mail for supplemental information[75,92,102]. Meanwhile, some of the authors reported detailed progress of the examined patients. We analyzed data from 166 patients diagnosed with pneumoparotid worldwide (1941-2023), including the present case, with studies using sialography, US, radiography, CT, and magnetic resonance imaging (MRI) (Table 1). Data on a total of 166 patients (mean age: 28.6 years) from 128 studies were reviewed. The patient in our case report was the oldest. This disease was approximately three times more common in men than in women[4,5]. The chief complaints often included swelling (92.9%) and pain (36.9%). Our patient was a man presenting with swelling of the left parotid gland. Symptoms of crepitus in the parotid region (75.8%) and frothy saliva from the orifice (72.2%) are characteristic of this disease. Our patient also had these symptoms. The disease equally affected the left, right, and both parotid glands. Patients with this condition frequently visited otolaryngologists, ear-nose-throat doctors, and head and neck surgeons (53.0%), followed by dentists, oral and maxillofacial surgeons, oral surgeons (13.3%), emergency room doctors (10.8%), pediatricians (9.0%), and internal medicine doctors (2.4%). The most frequent etiology of pneumoparotid was self-induction by mouth puffing (29.5%). Self-induced pneumoparotid was more prevalent in children aged < 18 years (55.1%), i.e., pediatric patients with self-induced pneumoparotid, which was often associated with school or home stress. Idiopathy (21.7%) was also frequently reported as an etiology. Pneumoparotid due to mouth puffing (13.9%) or another self-induced behavior presented in a similar manner; however, abnormal habits that made patients unconsciously puff their mouths made the treatment challenging. The rate of iatrogenic disease was approximately 11.4%, with increased reporting in recent years[6,8,11,12,33,51,93,95,98,116,127], especially for cases associated with dental treatment. Most patients underwent medical treatment, such as antibiotic, analgesic, and steroid administration (46.4%). Many patients who did not respond to antibiotics (15.6%) had pneumoparotid caused by self-induction or abnormal habits. A significant proportion of patients positively responded to behavior modification therapy (26.5%) and psychotherapy (8.7%), highlighting the need for detailed patient history in disease management. Some patients required surgery (9.6%)[17,21,22,29,30,41,42,59-61,63,72,75,91,111,130]. Subcutaneous emphysema (33.7%), pneumomediastinum (10.2%), and pneumothorax (0.6%)[68] were reported as complications. Patients with complications were approximately three times more likely to require surgery. Considering the risk of airway obstruction due to subcutaneous emphysema and mediastinitis due to pneumomediastinum, a detailed examination using CT scanning is important. Before the 1980s, sialography was the primary imaging modality for evaluating parotid emphysema; however, CT, US, and radiography have been commonly used in recent years. CT scans have an accuracy of 99.1%. Only one of the 109 patients could not be accurately evaluated by CT scans owing to the presence of artifacts associated with dentures[12]. Of the seven patients who underwent MRI scanning, three had no abnormal findings[12,45,50,60,79,81,90]. There were no abnormal findings in any of the five patients who underwent panoramic dental radiographs[12,44,79,116]. Therefore, MRI and panoramic dental radiograph were not useful in this context. Both CT and US evaluations were performed, and the US did not detect parotid emphysema or any other complications in six of 23 patients[67,96,102,104,113,131]. Air appears as a bright spot on a US image. Nonetheless, it must be distinguished from calcification and salivary stones. CT makes distinguishing between calcification and air straight forward and offers a more objective assessment compared to US. However, a history of X-ray exposure must be considered when performing a CT scan. Radiation exposure to the thyroid should be avoided, especially in children. As approximately 10% of patients with complications require surgery[17,21,22,29,30,41,42,59-61,63,72,75,91,111,130], CT is considered an important evaluation tool.
| Characteristics | |
| Age (years) | 5-83 |
| Mean | 28.6 |
| Percentage of children (%) | 55.1 |
| Percentage of men (%) | 72.9 |
| Chief symptom (%) | |
| Swelling | 92.9 |
| Pain | 36.9 |
| Signs (%) | |
| Crepitus | 75.8 |
| Frothy saliva | 72.2 |
| First consultation specialist (%) | |
| Otolaryngologist | 53.0 |
| Dentists and oral and maxillofacial surgeons | 13.3 |
| ER doctors | 10.8 |
| Pediatricians | 9.0 |
| Etiology (%) | |
| Self-induced | 29.5 |
| Idiopathic | 21.7 |
| Abnormal habit | 13.9 |
| Iatrogenic | 11.4 |
| Playing wind instruments | 11.4 |
| Blowing balloons | 4.2 |
Most patients with pneumoparotid respond to conservative treatment; however, 10% of patients develop severe disease requiring surgery. Complications, such as subcutaneous emphysema, pneumomediastinum, and pneumothorax, may arise; consequently, local evaluation using US or radiography, along with comprehensive evaluations utilizing CT, is essential.
| 1. | Hyrtl Joseph. Handbuch der Topographischen Anatomie und Ihrer Praktisch Medicinisch-Chirurgischen Anwendungen, 5th ed. Wilhelm Braumüller: Wien, Austria, 1865: 390. |
| 2. | Saunders HF. Wind parotitis. N Engl J Med. 1973;289:698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Trémollieres F, Caussade L. Simulation des oreillons. Presse Méd. 1918;192:334 Available from: https://scholar.google.com/scholar_lookup?title=Simulation+des+oreillons&author=Tr%C3%A9mollieres,+F.&author=Caussade,+L.&publication_year=1918&journal=Presse+M%C3%A9d.&volume=192&pages=334. |
| 4. | Gazia F, Freni F, Galletti C, Galletti B, Bruno R, Galletti C, Meduri A, Galletti F. Pneumoparotid and Pneumoparotitis: A Literary Review. Int J Environ Res Public Health. 2020;17:3936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Yoshida K. Etiology of Pneumoparotid: A Systematic Review. J Clin Med. 2022;12:144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 6. | Takenoshita Y, Kawano Y, Oka M. Pneumoparotis, an unusual occurrence of parotid gland swelling during dental treatment. Report of a case with a review of the literature. J Craniomaxillofac Surg. 1991;19:362-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Moënne KB, Cordero JT, Poli CH. [Pneumoparotitis or pneumoparotid: a differential diagnosis to consider]. Rev Chilena Infectol. 2009;26:555-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Abdullayev R, Saral FC, Kucukebe OB, Sayiner HS, Bayraktar C, Akgun S. [Bilateral parotitis in a patient under continuous positive airway pressure treatment]. Rev Bras Anestesiol. 2016;66:661-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Almario Hernández AF, Trenchs Sainz de la Maza V, Sangorrin Iranzo A, Luaces Cubells C. [Pneumoparotid: presentation of a case]. An Pediatr (Barc). 2014;81:e42-e43. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Sinha D, Brown J, Fan K. Bubbling parotitis. Clin Surg. 2020;5:2812 Available from: https://www.clinicsinsurgery.com/openaccess/bubbling. |
| 11. | Goncalves M, Sievert M, Mantsopoulos K, Schapher ML, Mueller SK, Iro H, Koch M. Pneumoparotid: Practical impact of Surgeon performed Ultrasound in an effective Diagnostic Approach. Oral Dis. 2023;29:3278-3288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 12. | Goates AJ, Lee DJ, Maley JE, Lee PC, Hoffman HT. Pneumoparotitis as a complication of long-term oronasal positive airway pressure for sleep apnea. Head Neck. 2018;40:E5-E8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Greisen O. Pneumatocele glandulae parotis. J Laryngol Otol. 1968;82:477-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Gaus W. Seltene Spätfolge nach Parotis epidemica. Zeitschr. F. Hals-: Nasen Ohrenheilkd. 1941;47:97-102 Available from: https://cir.nii.ac.jp/crid/1370861287039741214. |
| 15. | Rysenaer L, van Deinse J, Stuyt L. Pneumo-parotidite récidivante. ORL. 1963;25:128-131. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Rupp RN. Pneumoparotid. Arch Otolaryngol. 1963;77:111. [DOI] [Full Text] |
| 17. | Kozlova EV, Pivovarenko TV, Malinovskaia IV, Aminov RI, Kovalenko NK, Voronin AM. [Antibiotic resistance of Lactobacillus strains]. Antibiot Khimioter. 1992;37:12-15. [PubMed] |
| 18. | Yoel J, Alberti CD, Cignetti JM. [Pneumoparotiditis]. Prensa Med Argent. 1970;57:423-428. [PubMed] |
| 19. | Rosefsky JB. Parotid swelling and school phobia. Arch Otolaryngol. 1970;92:396-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Calcaterra TC, Lowe J. Pneumoparotiditis. An unusual case of parotid gland swelling. Arch Otolaryngol. 1973;97:468-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | O'hara AE, Keohane RB. Sialography in an unusual case of subcutaneous emphysema of the neck. Arch Otolaryngol. 1973;98:354-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Watt J. Benign parotid swellings: a review. Proc R Soc Med. 1977;70:483-486. [PubMed] |
| 23. | Sánchez Sánchez ML, Millán Núñez-Cortés J, Calvo Manuel E, Espinos Pérez D, Rubio Pérez P. [Crisis of recurrent parotid swelling in factitious cervico-facial subcutaneous emphysema]. Rev Clin Esp. 1980;157:197-199. [PubMed] |
| 24. | Hadas E, Leventon G, Lerner K, Zimin RJ. [Pneumoparotitis: psychosomatic aspects]. Harefuah. 1982;102:104-105. [PubMed] |
| 25. | Rozas Aristy F. [Case of parotid swelling with cervicofacial emphysema]. Rev Med Panama. 1982;7:49-52. [PubMed] |
| 26. | Markowitz-Spence L, Brodsky L, Seidell G, Stanievich JF. Self-induced pneumoparotitis in an adolescent. Report of a case and review of the literature. Int J Pediatr Otorhinolaryngol. 1987;14:113-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Komori T, Sato O, Mori Y, Ishii M, Enomoto S. Emphysema of the parotid gland induced by abnormal habit: Rreport of a case. J Jpn Stomatol Soc. 1988;37:696-701 Available from: https://cir.nii.ac.jp/crid/1390001206435280128. |
| 28. | David ML, Kanga JF. Pneumoparotid. In cystic fibrosis. Clin Pediatr (Phila). 1988;27:506-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Brodie HA, Chole RA. Recurrent pneumosialadenitis: a case presentation and new surgical intervention. Otolaryngol Head Neck Surg. 1988;98:350-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Telfer MR, Irvine GH. Pneumoparotitis. Br J Surg. 1989;76:978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Yamashita K, Oishi K, Sawaki S, Furukawa M. A case of pneumoparotid. Stomato-Pharyngology. 1990;3:58. [DOI] [Full Text] |
| 32. | Mandel L, Kaynar A, Wazen J. Pneumoparotid: a case report. Oral Surg Oral Med Oral Pathol. 1991;72:22-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Piette E, Walker RT. Pneumoparotid during dental treatment. Oral Surg Oral Med Oral Pathol. 1991;72:415-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Krief O, Gomori JM, Gay I. CT of pneumoparotitis. Comput Med Imaging Graph. 1992;16:39-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 35. | Curtin JJ, Ridley NT, Cumberworth VL, Glover GW. Pneumoparotitis. J Laryngol Otol. 1992;106:178-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 36. | Ferlito A, Andretta M, Baldan M, Candiani F. Non-occupational recurrent bilateral pneumoparotitis in an adolescent. J Laryngol Otol. 1992;106:558-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Terahara E, Jitosho T, Ninomiya M, Umemoto M, Minamishima I, Take H, Kiyota R. A case of self-induced pneumoparotitis. J Pediatr Pract. 1992;145:1705-1708 Available from: https://cir.nii.ac.jp/crid/1574231875301786880. |
| 38. | Yonetsu K, Miwa K, Kanda S, Oobu K, Shiratsuchi Y. Pneumoparotid. Oral Radiol. 1993;9:41-42. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 39. | Birzgalis AR, Curley JW, Camphor I. Pneumoparotitis, subcutaneous emphysema and pleomorphic adenoma. J Laryngol Otol. 1993;107:349-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 40. | Cook JN, Layton SA. Bilateral parotid swelling associated with chronic obstructive pulmonary disease. A case of pneumoparotid. Oral Surg Oral Med Oral Pathol. 1993;76:157-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Nassimbeni G, Ventura A, Boehm P, Guastalla P, Zocconi E. Self-induced pneumoparotitis. Clin Pediatr (Phila). 1995;34:160-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 42. | Goguen LA, April MM, Karmody CS, Carter BL. Self-induced pneumoparotitis. Arch Otolaryngol Head Neck Surg. 1995;121:1426-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Nakamura Y, Ino Y, Morita T. Recurrent parotid swelling due to psychologic stress – Rreport of a case. Otolaryngol Head Neck Surg. 1996;68:166-170. [DOI] [Full Text] |
| 44. | Eligi C, Scasso CA, Bruschini P, Neri E, Dotti S. [Pseudomonas aeruginosa pneumoparotitis. Report of a case]. Radiol Med. 1997;94:108-110. [PubMed] |
| 45. | Barthold U. [Air collection in the parotid region and the soft tissues of the neck bilaterally caused by self-insufflation]. HNO. 1998;46:64-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 46. | Gudlaugsson O, Geirsson AJ, Benediktsdóttir K. Pneumoparotitis: a new diagnostic technique and a case report. Ann Otol Rhinol Laryngol. 1998;107:356-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 47. | Alcalde RE, Ueyama Y, Lim DJ, Matsumura T. Pneumoparotid: report of a case. J Oral Maxillofac Surg. 1998;56:676-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | Leuwer A, Greess H. [Painless recurrent cheek swelling. Parotid emphysema (pneumoparotis)]. HNO. 1998;46:766-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 49. | Golz A, Joachims HZ, Netzer A, Westerman ST, Gilbert LM. Pneumoparotitis: diagnosis by computed tomography. Am J Otolaryngol. 1999;20:68-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 50. | Sittel C, Jungehülsing M, Fischbach R. High-resolution magnetic resonance imaging of recurrent pneumoparotitis. Ann Otol Rhinol Laryngol. 1999;108:816-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 51. | Kirsch CM, Shinn J, Porzio R, Trefelner E, Kagawa FT, Wehner JH, Jensen WA. Pneumoparotid due to spirometry. Chest. 1999;116:1475-1478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 52. | Martín-Granizo R, Herrera M, García-González D, Mas A. Pneumoparotid in childhood: report of two cases. J Oral Maxillofac Surg. 1999;57:1468-1471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 53. | Huang PC, Schuster D, Misko G. Pneumoparotid: a case report and review of its pathogenesis, diagnosis, and management. Ear Nose Throat J. 2000;79:316-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 54. | Yokoyama T, Nonaka S, Takahara M, Harabuchi Y. A Case of Pneumoparotitis. Practica Otologica. 2001;94:33-37. [DOI] [Full Text] |
| 55. | Cho YS, Seo IS, Na DG, Chu KC. A case of recurrent pneumoparotitis in a wind instrumentalist. Korean J Otolaryngol. 2001;44:330-332 Available from: https://pesquisa.bvsalud.org/portal/resource/pt/wpr-644940. |
| 56. | Franco V, Houliat T, Devars F, Traissac L. [Pneumoparotid: a case report and review of the literature]. Rev Laryngol Otol Rhinol (Bord). 2002;123:149-151. [PubMed] |
| 57. | Brasseur P, Peché R, Sukkarieh F, Van Meerhaeghe A. [Subcutaneous emphysema in a borderline patient]. Rev Pneumol Clin. 2003;59:149-153. [PubMed] |
| 58. | Orabi AA, Nigam A. Bilateral longstanding self-induced pneumoparotitis. Aust J Otolaryngol. 2004;7:43-46 Available from: https://www.proquest.com/openview/37c2380a2224b94b4b5c4266c8c98678/1?pq-origsite=gscholar&cbl=33823. |
| 59. | Han S, Isaacson G. Recurrent pneumoparotid: cause and treatment. Otolaryngol Head Neck Surg. 2004;131:758-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 60. | Apaydin M, Sarsilmaz A, Calli C, Erdogan N, Varer M, Uluc E. Giant pneumoparotitis. European Journal of Radiology Extra. 2004;52:17-20. [DOI] [Full Text] |
| 61. | Maehara M, Ikeda K, Ohmura N, Sugimoto T, Harima K, Ino C, Sawada S. Multislice computed tomography of pneumoparotid: a case report. Radiat Med. 2005;23:147-150. [PubMed] |
| 63. | Grainger J, Saravanappa N, Courteney-Harris RG. Bilateral pneumoparotid. Otolaryngol Head Neck Surg. 2006;134:531-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 64. | Paksoy G, Oğuz H, Arslan N, Demirci M, Şafak MA. Idiopathic recurrent pneumoparotitis: Ccase report. KBB-Forum. 2006;5:161-163 Available from: https://kbb-forum.net/journal/abstract.php?lang=en&id=159. |
| 65. | Scherr MK, Schmitz S, Wirth S. [Pneumoparotis and cervical emphysema as a rare complication of medical protests]. Rofo. 2006;178:816-818. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 66. | Adachi Masao. A Case of parotid emphysema in a severely intellectually retarded patient with repeated mouth blowing habits. J Sev Mot Intellect Disabil. 2006;31:299-303 Available from: https://cir.nii.ac.jp/crid/1572543025746954752. |
| 67. | Yang SM, Park CH, Hong SJ, Kim HC. Case of bilateral pneumoparotitis in the children. Korean J Otolaryngol. 2007;50:366-368 Available from: https://pesquisa.bvsalud.org/portal/resource/pt/wpr-644359. |
| 68. | Chun JH, Kim HY, Kwon SJ, Nam SY. A case of self-induced pneumoparotitis. Korean J Otorhinolaryngol-Head Neck Surg. 2007;50:726-728 Available from: https://pesquisa.bvsalud.org/portal/resource/pt/wpr-645633. |
| 69. | Balasubramanian S, Srinivas S, Aparna KR. Pneumoparotitis with subcutaneous emphysema. Indian Pediatr. 2008;45:58-60. [PubMed] |
| 70. | Hervás Núñez MJ, Benito Navarro JR, Rodríguez Fernández-Freire A, Rodríguez Pérez MA. [Parotid pneumocele in Down's syndrome]. Acta Otorrinolaringol Esp. 2008;59:41-42. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 71. | Luaces R, Ferreras J, Patiño B, Garcia-Rozado A, Vázquez I, López-Cedrún JL. Pneumoparotid: a case report and review of the literature. J Oral Maxillofac Surg. 2008;66:362-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 72. | Joo YH, Shin JH, Park SN, Sun DI. A case of pneumoparotid treated by ligation of Stensen’s duct. Korean J Otorhinolaryngol-Head Neck Surg. 2008;51:643-645 Available from: https://pesquisa.bvsalud.org/portal/resource/pt/wpr-643866. |
| 73. | Prabhu SP, Tran B. Pneumoparotitis. Pediatr Radiol. 2008;38:1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 74. | Faure F, Plouin Gaudon I, Tavernier L, Ayari Khalfallah S, Folia M. A rare presentation of recurrent parotid swelling: Self-induced parotitis. International Journal of Pediatric Otorhinolaryngology Extra. 2009;4:29-31. [DOI] [Full Text] |
| 75. | Mukundan D, Jenkins O. Images in clinical medicine. A tuba player with air in the parotid gland. N Engl J Med. 2009;360: 710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 76. | Lee HI, Jung HW, Joo J, Cho JE. A Case of Self-Induced Pneumoparotid. J Clin Otolaryngol Head Neck Surg. 2009;20:272-276. [DOI] [Full Text] |
| 77. | Kyung SK, Heurtebise F, Godon A, Rivière MF, Coatrieux A. Head-neck and mediastinal emphysema caused by playing a wind instrument. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127:221-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 78. | Aghaei Lasboo A, Nemeth AJ, Russell EJ, Siegel GJ, Karagianis A. The use of the "puffed-cheek" computed tomography technique to confirm the diagnosis of pneumoparotitis. Laryngoscope. 2010;120:967-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 79. | Fukuta Y, Fukuta K, Takeda Y. Pneumoparotitis induced by an abnormal habit: Rreport of an adult case. Jpn J Oral Diagn. 2011;24:26-29 Available from: https://cir.nii.ac.jp/crid/1573387450615624576. |
| 80. | van Ardenne N, Kurotova A, Boudewyns A. Pneumoparotid: a rare cause of parotid swelling in a 7-year-old child. B-ENT. 2011;7:297-300. [PubMed] |
| 81. | Iwaki H, Suzuki S, Shinogami M. A case of pneumoparotid due to habit of blowing the cheeks. Pract Otol. 2011;160:131 Available from: https://cir.nii.ac.jp/crid/1570572701182505600. |
| 82. | Vasi AZ, Hoskins WP. Radiology quiz case 3. Bilateral self-induced pneumoparotitis. Arch Otolaryngol Head Neck Surg. 2011;137:1041-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 83. | Zuchi DF, Silveira PC, Cardoso Cde O, Almeida WM, Feldman CJ. Pneumoparotitis. Braz J Otorhinolaryngol. 2011;77:806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 84. | Ghanem M, Brown J, McGurk M. Pneumoparotitis: a diagnostic challenge. Int J Oral Maxillofac Surg. 2012;41:774-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 85. | Tachibana T, Ogawara Y, Matsuyama Y, Abe I, Hase S. A Case of Pediatric Pneumoparotitis. Jibi inkoka rinsho. 2012;105:567-570. [DOI] [Full Text] |
| 86. | Kitahara H. Pneumoparotid /Pneumoparotitis. Jpn J Clin Radiol. 2012;57:1371-1373 Available from: https://cir.nii.ac.jp/crid/1520291855838129920. |
| 87. | Li F, Ji YX, Zhu SR. A case report of pneumoparotid and review of the literature. China J Oral Maxillofac Surg. 2012;10:347-349 Available from: https://openurl.ebsco.com/results?bquery=A+case+report+of+pneumoparotid+and+review+of+the+literature.&page=1. |
| 89. | McCormick ME, Bawa G, Shah RK. Idiopathic recurrent pneumoparotitis. Am J Otolaryngol. 2013;34:180-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 90. | Potet J, Arnaud FX, Valbousquet L, Ukkola-Pons E, Donat-Weber G, Thome A, Peroux E, Teriitehau C, Baccialone J. Pneumoparotid, a rare diagnosis to consider when faced with unexplained parotid swelling. Diagn Interv Imaging. 2013;94:95-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 91. | McGreevy AE, O'Kane AM, McCaul D, Basha SI. Pneumoparotitis: a case report. Head Neck. 2013;35:E55-E59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 92. | Nicot R, Myon L, Konopnicki S, Ferri J, Raoul G. [Pneumoparotid: a rare cause of recurrent parotid swelling]. Rev Stomatol Chir Maxillofac Chir Orale. 2014;115:111-113. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 93. | Watanabe S, Hata S, Nakajima J, Yokoe H, Sato Y. A case of pneumoparotid caused by strong pressure with an air syringe. J Jpn Stomatol Soc. 2014;63:106-107 Available from: https://mol.medicalonline.jp/library/journal/download?GoodsID=cp8stoma/2014/s06301/210&name=0106-0107j. |
| 94. | Konstantinidis I, Chatziavramidis A, Constantinidis J. Conservative management of bilateral pneumoparotitis with sialendoscopy and steroid irrigation. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 95. | Ino C, Tada N, Minami T, Ino M, Tanabe M. Pneumoparotid. Pract Otol. 2015;61:155-169. [DOI] [Full Text] |
| 96. | Dietrich U, Holtmann L, Weller P, Ringelstein A. [Sudden swelling of cheek after valsalva maneuver]. Laryngorhinootologie. 2015;94:105-106. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 97. | Bowden BK, Bowden SA. Cervicofacial subcutaneous emphysema in a 4-year-old boy. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 98. | Cabello M, Macías E, Fernández-Flórez A, Martínez-Martínez M, Cobo J, de Carlos F. Pneumoparotid associated with a mandibular advancement device for obstructive sleep apnea. Sleep Med. 2015;16:1011-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 99. | Osawa Y, Kaneko M, Takano Y, Maeda S. Recurrent pneumoparotitis with pneumomediastinum. J Jpn Pediatr Soc. 2015;119:1386-1390 Available from: https://cir.nii.ac.jp/crid/1520290882879066752. |
| 100. | Shibata D, Harada T. Two cases of pneumoparotis. Kawasaki Med J. 2016;41:25-31. [DOI] [Full Text] |
| 101. | Lagunas JG, Fuertes AF. Self-induced parapharyngeal and parotid emphysema: A case of pneumoparotitis. Oral and Maxillofacial Surgery Cases. 2017;3:81-85. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 102. | Alnæs M, Furevik LL. Pneumoparotitis. Tidsskr Nor Laegeforen. 2017;137:544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 103. | Oh Y, Kim J.M., Jung H.J., Shim W.S.. A Case of Bilateral Pneumoparotid Improved with Conservative Treatment. Korean J. Head Neck Surg. 2017;33:43-45. [DOI] [Full Text] |
| 104. | Lee KP, James V, Ong GY. Emergency Department Diagnosis of Idiopathic Pneumoparotitis with Cervicofacial Subcutaneous Emphysema in a Pediatric Patient. Clin Pract Cases Emerg Med. 2017;1:399-402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 105. | Kwon H, Kim DJ, Chon K, Lee B. A Case of Recurrent Self-Induced Pneumoparotid. J Clin Otolaryngol Head Neck Surg. 2017;28:307-310. [DOI] [Full Text] |
| 106. | Takeuchi J, Akashi M. A case of pneumoparotitis induced by an abnormal habit. Hospital Dentistry & Oral-Maxillofacial Surgery. 2017;29:123-126 Available from: https://www.hospital-dentistry.org/pdf/index/vol29-2.pdf. |
| 107. | Yamazaki H, Kojima R, Nakanishi Y, Kaneko A. A Case of Early Pneumoparotid Presenting With Oral Noises. J Oral Maxillofac Surg. 2018;76:67-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 109. | Paterson T, Maini N, Ganesh V, Newman L. Pneumoparotid: An unusual case of intermittent unilateral cheek swelling. Int J Surg. 2018;55:S27. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 110. | House LK, Lewis AF. Pneumoparotitis. Clin Exp Emerg Med. 2018;5:282-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 111. | Miłoński J, Kolary K, Spencer S, Olszewski J. A rare case of a pneumoparotid. J Hear Sci. 2019;9:46-50. [DOI] [Full Text] |
| 112. | Ambrosino R, Lan R, Romanet I, Le Roux MK, Gallucci A, Graillon N. Severe idiopathic pneumoparotitis: Case report and study review. Int J Pediatr Otorhinolaryngol. 2019;125:196-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 113. | Basha MS. A rare case of unilateral pneumoparotid. Sci Arch J Dent Sci. 2019;2:13-15 Available from: https://saods.net/wp-content/uploads/SAODS/PDF-Data/2019/Volume-2-Issue-11/SAODS-02-0086.pdf. |
| 114. | Raczkowska-łabuda K, Jabłońska-jesionowska M, Jadczyszyn J, Frąckiewicz M, Pilch M, Zawadzka-głos L. Self-induced pneumoparotitis – a rare case report. New Med. 2019;23. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 115. | Kim HY, Park KS, Jung SH, Lee DH. Incidentally Diagnosed Asymptomatic Pneumoparotid. Korean J Head Neck Oncol. 2019;35:81-83. [DOI] [Full Text] |
| 116. | Enami S, Sato A, Myers M, Maruoka Y. A Case of Emphysema of the Parotid Gland Caused by Dental Treatment. Jpn J Oral Diag / Oral Med. 2020;33:39-42. [DOI] [Full Text] |
| 117. | Yang Z, Bundrick PE. Subcutaneous Emphysema of the Neck With Pneumomediastinum. JAMA Otolaryngol Head Neck Surg. 2020;146:306-307. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 118. | Gray SC, Pienaar JA, Sofianos Z, Varghese J. Complicated spontaneous pneumoparotid mimicking a neck mass in a child with Down's syndrome. SA J Radiol. 2020;24:1883. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 119. | Aljeaid D, Mubarak A, Imarli Y, Alotaibi O. Pneumoparotid: a rare but well-documented cause of parotid gland swelling. Egypt J Otolaryngol. 2020;36:46. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 120. | Al Ohali S, Al‐qahtani M, Al Shahrani M, Islam T, Al‐qahtani K. Self‐induced pneumoparotid: Case report of a rare cause. Oral Science International. 2020;17:179-182. [DOI] [Full Text] |
| 121. | Fernandez S, Garaycochea O, Prieto-matos C, Álvarez de Linera M, Alcalde J. Inflating parotids with air: A case of pneumoparotid and review of the literature. A case of pneumoparotid. Otolaryngology Case Reports. 2020;17:100227. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 122. | Yoshida K. Pneumoparotid related to obstructive sleep apnea syndrome treated by oral appliance with anterior opening to reduce intraoral pressure. Clin Case Rep. 2022;10:e05816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 123. | Kim J, Kim G. A Case of Self-induced Pneumoparotid Improved with Conservative Treatment. Korean J Head Neck Oncol. 2022;38:19-21. [DOI] [Full Text] |
| 124. | Galletti C, Bruno G, Ciodaro F, Freni F. Pneumoparotid and Subcutaneous Emphysema in a Man with Psychiatric Disorders. An International Journal of Otorhinolaryngology Clinics. 2023;14:110-113. [DOI] [Full Text] |
| 125. | Barros M, Rodrigues I, Silva M, Cascais M, Sá A. Pneumoparotid: A diagnosis to consider. J Paediatr Child Health. 2022;58:2099-2100. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 126. | Youner ER, Cox R, Zapanta P. Inadvertent, Self-Induced Pneumoparotitis Provoking Pneumomediastinum. Cureus. 2023;15:e34016. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 127. | Caudo D, Santalco A, Cammaroto S, Anfuso C, Zullo Y, Cacopardi D, Lo Monte V, Benedetto C, Benedetto C, Militi A, Smorto C, Italiano F, Barbaro U, Salamone I. “Endo-Oral Contrast-Puffing CT” in Pneumoparotitis: A Case Report. Asp Biomed Clin Case Rep. 2023;6:50-53. [DOI] [Full Text] |
| 128. | Yanagizono K, Adachi M, Akizuki H. A Case of Pediatric Pneumoparotitis with Extensive Mediastinal Emphysema. Jibi inkoka rinsho. 2023;116:339-343. [DOI] [Full Text] |
| 129. | Ramsey S, Ely R. Pediatric Idiopathic Bilateral Pneumoparotid. Cureus. 2023;15:e33621. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 130. | Liangyu GE, JI li JI, Lin C, Zhiping LI, Qianping GU, Jian M, Jing Z. Refractory pneumoparotid in children: A case report and literature review. J Prev Treat Stomatol Dis. 2023;12:192-196 Available from: https://pesquisa.bvsalud.org/portal/resource/pt/wpr-960887. |
| 131. | Van Gool H, Vermeulen F, Toelen J. Facial swelling caused by pneumoparotid: A case report and review of the literature. Belg J Paediatr.. 2023;25:122-126 Available from: https://www.belgjpaediatrics.com/index.php/bjp/article/view/76. |