Published online Jan 26, 2024. doi: 10.12998/wjcc.v12.i3.665
Peer-review started: November 22, 2023
First decision: December 15, 2023
Revised: December 24, 2023
Accepted: January 4, 2024
Article in press: January 4, 2024
Published online: January 26, 2024
Processing time: 57 Days and 1.2 Hours
Porocarcinoma is a rare type of skin cancer that originates from sweat gland tumors. It is an aggressive malignant skin cancer that is difficult to diagnose clinically owing to its rarity and similarity to squamous cell carcinoma (SCC).
This case involved a 92-year-old woman, a farmer by profession, presented with an exophytic and verrucous mass on her left palm that had formed 2 years prior and caused chronic pain and frequent bleeding. Initially, the patient was diagnosed with SCC using a punch biopsy; however, a repeat biopsy with addi
Porocarcinoma is commonly misdiagnosed as SCC; therefore, clinicians should consider porocarcinomas when evaluating mass-like lesions on the hands.
Core Tip: Porocarcinoma is rare malignant skin tumor, which accounts for approximately 0.005% to 0.01% of cutaneous carcinomas. Among these cases, the occurrence of porocarcinoma in the hands is even rarer. Herein, we report a rare case of porocarcinoma in the palm, including the clinicopathological characteristics, treatment, and prognosis.
- Citation: Lim SB, Kwon KY, Kim H, Lim SY, Koh IC. Porocarcinoma in a palm reconstructed with a full thickness skin graft: A case report. World J Clin Cases 2024; 12(3): 665-670
- URL: https://www.wjgnet.com/2307-8960/full/v12/i3/665.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i3.665
In 1963, Pinku et al[1] first described porocarcinoma as a rare malignant skin tumor originating from the intraepidermal ductal portion of the sweat glands. Porocarcinoma accounts for approximately 0.005%-0.01% of cutaneous carcinomas; however, its pathophysiology has not been completely elucidated. Porocarcinomas can develop de novo or from benign poromas[2]. The risk factors for porocarcinoma include exposure to sunlight, immunosuppression, chronic exposure to benzene, and acquired immunodeficiency syndrome[3]. Nevertheless, the diagnosis and appropriate treatment of porocarcinoma remain challenging owing to the lack of data[4].
Porocarcinoma occurs more frequently with age, predominantly during the seventh and eighth decades of life[5]. The distribution of sites of presentation suggests that the head and neck (39.9%) are the most frequent primary sites, followed by the lower (33.9%) and upper (8.8%) extremities[5].
In this report, we describe a rare case of porocarcinoma in the left palm, where it is rarely located, in a 92-year-old woman. The patient underwent successful reconstruction with a full-thickness skin graft after wide excision.
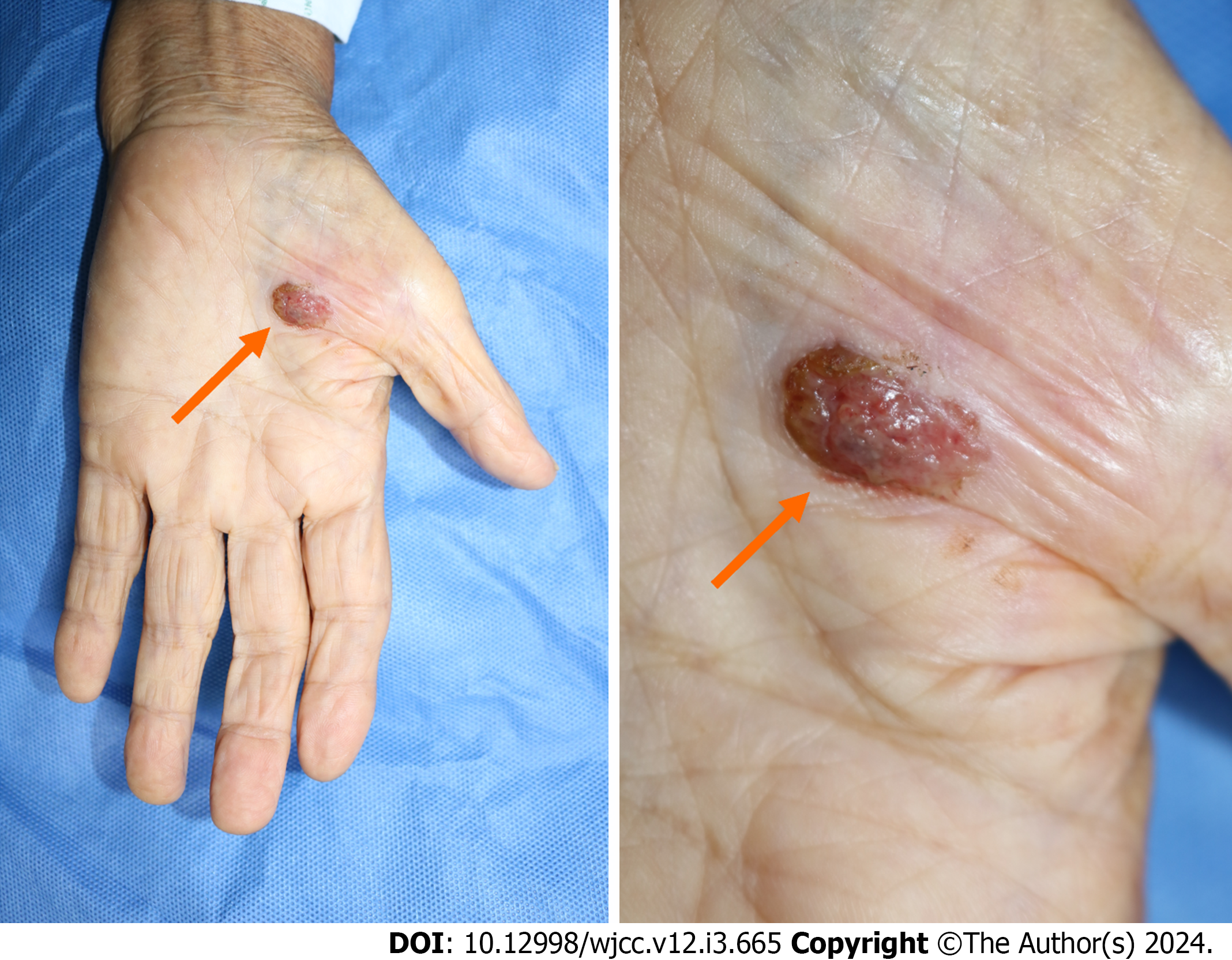
A 92-year-old woman presented with a painful mass in her left palm (Figure 1).
The mass developed 2-3 years prior, causing chronic pain and bleeding.
The patient had a history of heart failure, hypertension, gout, and chronic kidney disease.
The patient worked as a farmer, which exposed her to considerable sunlight from her 20s to her mid-80s.
The lesion was an exophytic, verrucous, and easily bleeding nodule measuring 1.2 cm × 1.0 cm in size, suggestive of a viral wart. Squamous cell carcinoma (SCC) was diagnosed in the initial pathological study; however, a re-biopsy with additional immunohistochemical tests was performed, considering porocarcinoma.
No special laboratory tests were performed.
Positron emission tomography-computed tomography (PET-CT) was subsequently performed to evaluate metastasis. We observed 18-fluoro-deoxyglucose (FDG)-avid malignancy in the left palm with no evidence of FDG-avid metastasis on PET-CT (Figure 2).
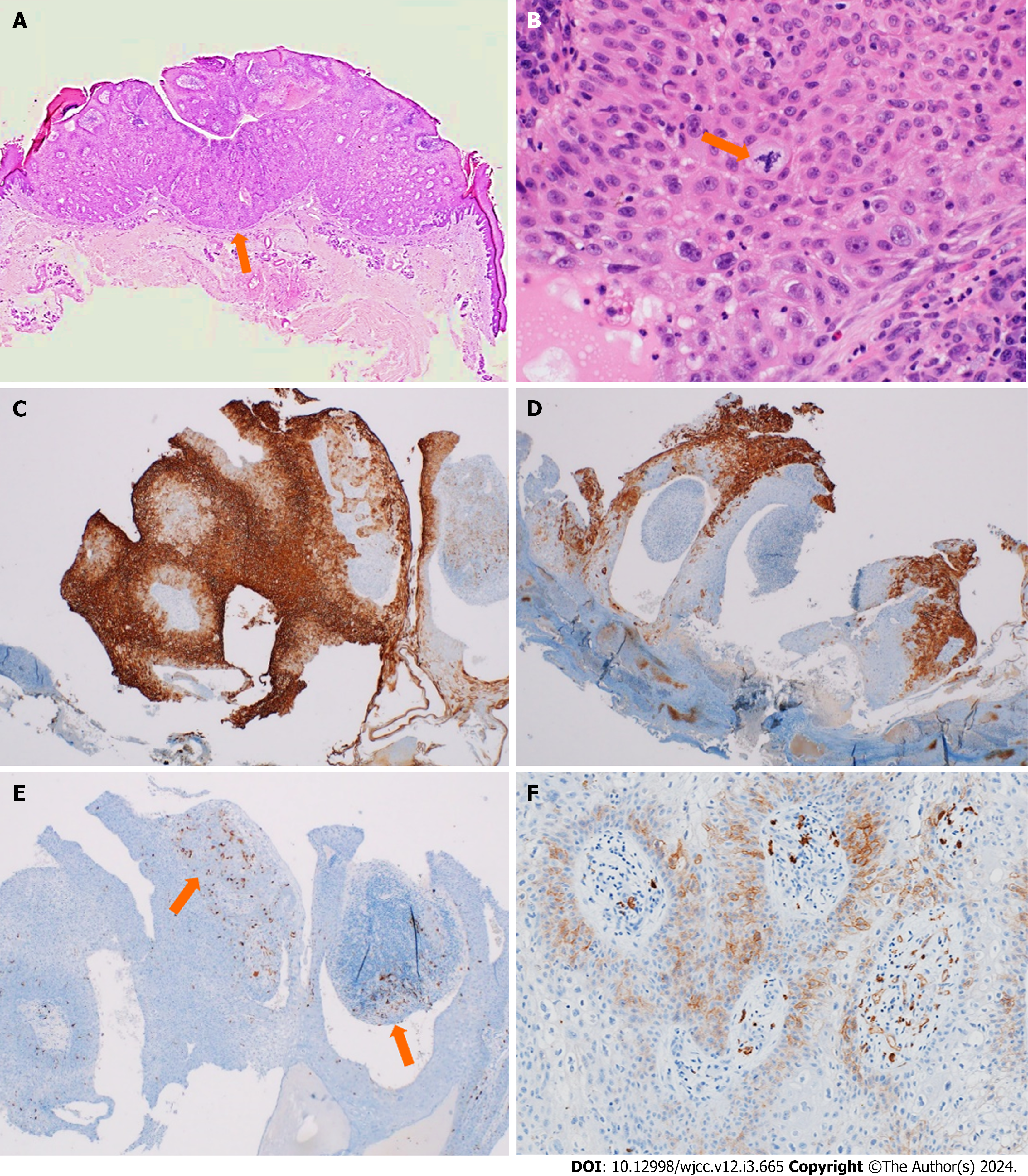
Pathological studies revealed epidermal tumor clusters arising from the intraepidermal portion of the sweat gland ducts and extending to the dermal portion. The tumor cells exhibited atypical mitoses. Upon immunohistochemical analysis, the patient was positive for epithelial membrane antigen (EMA), periodic acid–Schiff (PAS), cytokeratin 19, and C-kit (CD117); focally positive for S-100 and GATA3; partially positive for cytokeratin 7; and negative for carcinoembryonic antigen (Figure 3).
The patient was ultimately diagnosed with porocarcinoma.
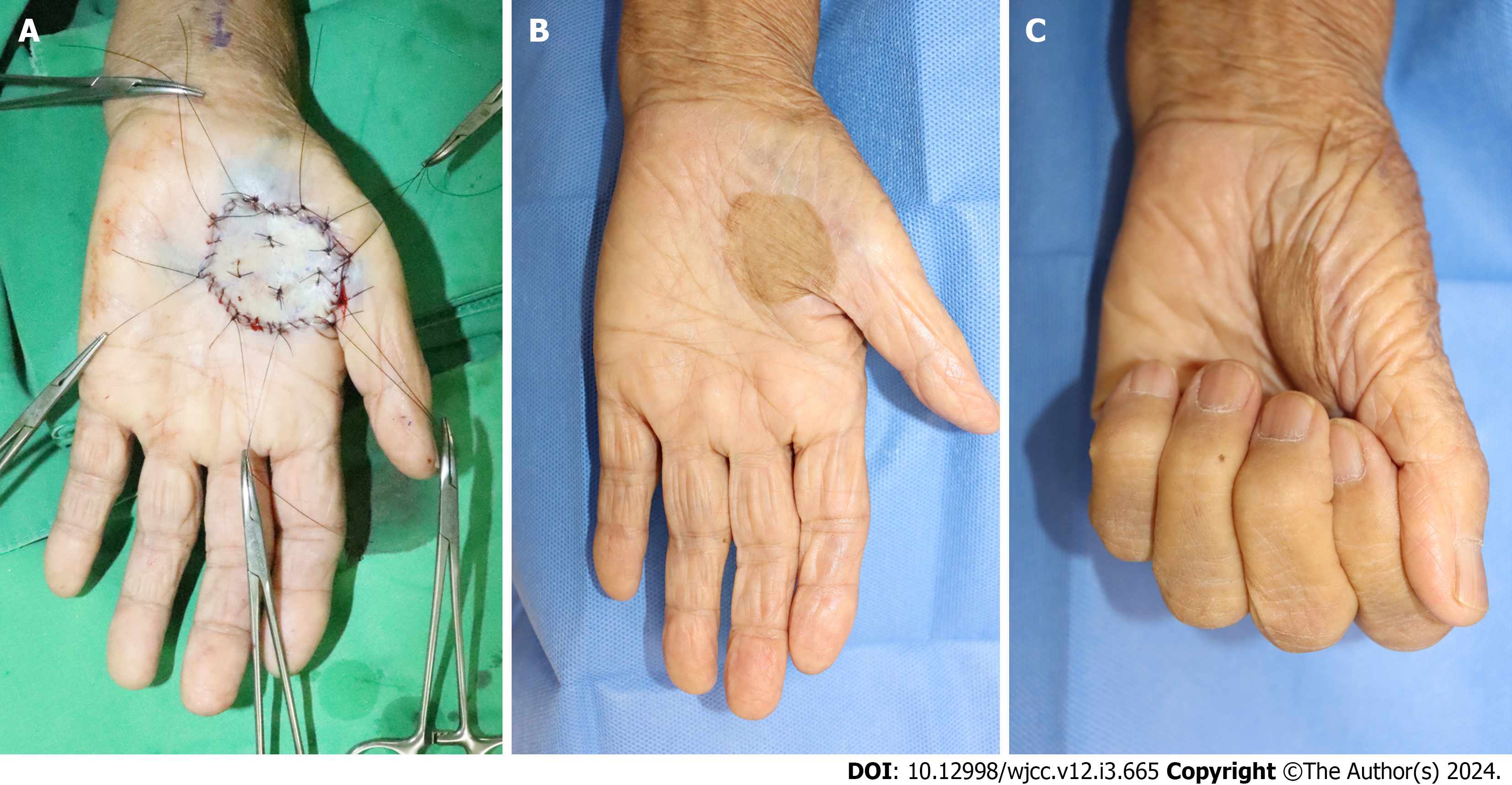
Because no evidence of metastasis was observed, surgical excision was planned. We performed a wide excision with a 1.3 cm lateral margin and subcutaneous fat layer depth. After excision, the defect size was 4.2 cm × 4.0 cm, and a clear resection margin was confirmed. Although several methods have been proposed to cover the affected areas, local flap coverage was excluded because of the lack of skin laxity of the palm. The patient was an older adult with poor general condition for free tissue transfer; therefore, we performed a full-thickness skin graft coverage, with the left inguinal area as the donor site, to preserve the range of motion of the hand and derive better aesthetic outcomes (Figure 4).
Wound recovery occurred without functional complications, such as limitations in movement and contracture. Moreover, we recorded satisfactory aesthetic outcomes, achieving a shape similar to that of the original without a hypertrophic scar. At the 6-mo follow-up, adjuvant chemotherapy and radiotherapy were not required, and the patient was satisfied with the results, with no cancer recurrence.
Porocarcinoma is a rare tumor that originates from the intraepidermal eccrine duct epithelium or acrosyringium, has an aggressive course, and does not exhibit any specific sex preferences[5]. The primary sites most commonly affected by porocarcinomas are the head and neck (32%), lower limbs (33%), trunk (14.1%), and genitalia and buttocks (11.2%). Moreover, upper limb involvement was observed in only 9.7% of the patients. In contrast, porocarcinoma has been reported in the palm area in only one of 206 reported cases[6]. Among these cases, Chow et al[6] described a case of porocarcinoma in the right palm that developed from a puncture wound exposed to an unknown chemical. They utilized anterolateral thigh fascia perforator flap coverage after wide excision. Moreover, Singh et al[7] presented a case of porocarinoma in the right palm, suspected to be associated with an infected ganglion developed due to repeated trauma in the patient’s job of pushing trolleys at a factory. They also utilized split-thickness skin graft coverage after wide excision.
Porocarcinoma usually presents as a plaque, nodular mass, or chronic ulcerative lesion. Therefore, it is often misdiagnosed as SCC, pyogenic granuloma, or a wart[6]. Due to its diverse histological characteristics, the diagnosis of porocarcinoma requires histological examination[2,8]. A histological study of the porocarcinoma using hematoxylin and eosin staining demonstrated nuclear atypia, necrosis, and increased mitotic activity. Notably, infiltrative porocarcinomas exhibit poorly defined lower margins with malignant cell clusters infiltrating the dermis[8]. Moreover, to avoid misdiagnosis due to histological variations, immunohistochemical studies are typically performed using EMA, PAS, CKs (AE1/AE3), p63, and Ki67, all of which are positive in most porocarcinoma cases[6,8]. However, porocarcinomas can mimic SCC when they exhibit pagetoid intraepidermal spread, adnexal structure colonization, acantholysis, and pseudogland formation[9]. In such cases, ductal differentiation, intracytoplasmic lumina, and CD117 positivity can facilitate the differential diagnosis of SCC[2,3,9].
The treatment options for primary tumors without metastasis include wide local excision or Mohs micrographic surgery; the excision margin varies, with 1-2 cm being the most commonly used margin[8,10]. Reconstruction options for defects include primary closure, dermal regeneration templates, skin grafts, flaps, and free tissue transfer[6]. However, owing to its rarity, there is no standard protocol for treating metastatic porocarcinoma. While clinicians may recommend chemotherapy or radiotherapy for the treatment of metastatic porocarcinoma, there is limited evidence to support its clinical efficacy[10,11].
Delayed diagnosis of porocarcinoma may postpone optimal treatment. The metastatic rate of porocarcinoma is approximately 20%-30%[5,8,11], and the mortality rate of metastatic porocarcinoma is approximately 80% or 65%-67% when it involves the lymph nodes[10]. PET-CT and CT are primarily performed for evaluating metastasis[8]. In this case, we achieved the detection of porocarcinoma during the early stages, allowing surgical excision of the lesion before metastasis. Notably, no recurrence was observed 6 months after surgery. After excision, the defect was reconstructed using a full-thickness skin graft harvested from the ipsilateral inguinal area, which healed without motion limitations or aesthetic flaws.
As porocarcinoma occurs sparsely and its clinical features are nonspecific, it can mimic other lesions such as SCC, pyogenic granuloma, and warts. Porocarcinomas rarely occur on the hand, whereas SCC is the most common skin cancer of the hand. Thus, porocarcinomas are often misdiagnosed as SCC. Porocarcinoma has high malignant potential and requires a relatively wide excision margin. Thus, delayed treatment due to late diagnosis can lead to increased mortality due to metastasis, aesthetic deficits, and functional disabilities, such as movement limitations or hand amputation. Therefore, clinicians should not overlook porocarcinomas when evaluating mass-like lesions on the hands.
Porocarcinoma has a poor prognosis and high rates of metastasis and recurrence. Thus, clinicians should evaluate this rare tumor based on histological features and immunohistochemical studies. Through appropriate evaluation, proper treatment should be provided without misdiagnosis and delay.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lamichane SR, Nepal S-Editor: Zhang H L-Editor: A P-Editor: Cai YX
| 1. | Pinkus H, Mehregan AH. Epidermotropic eccrine carcinoma. A case combining features of eccrine poroma and paget's dermatosis. Arch Dermatol. 1963;88:597-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 192] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Joshy J, Mistry K, Levell NJ, van Bodegraven B, Vernon S, Rajan N, Craig P, Venables ZC. Porocarcinoma: a review. Clin Exp Dermatol. 2022;47:1030-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Miyamoto K, Yanagi T, Maeda T, Ujiie H. Diagnosis and Management of Porocarcinoma. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 4. | Kurashige Y, Minemura T, Nagatani T. Eccrine porocarcinoma: clinical and pathological report of eight cases. Case Rep Dermatol. 2013;5:259-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Salih AM, Kakamad FH, Baba HO, Salih RQ, Hawbash MR, Mohammed SH, Othman S, Saeed YA, Habibullah IJ, Muhialdeen AS, Nawroly RO, Hammood ZD, Abdulkarim NH. Porocarcinoma; presentation and management, a meta-analysis of 453 cases. Ann Med Surg (Lond). 2017;20:74-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 6. | Chow KL, Peters X, Mashbari H, Shokouh-Amiri M, Benjamin M, Warso M. A Case Report of Malignant Eccrine Porocarcinoma Involving the Palm Requiring Surgical Excision and Free Flap Reconstruction. Am J Case Rep. 2020;21:e925231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Singh R, Majumder S. Eccrine porocarcinoma of the hand: a case report. Internet J Hand Surg. 2008;2:2. [DOI] [Full Text] |
| 8. | Nazemi A, Higgins S, Swift R, In G, Miller K, Wysong A. Eccrine Porocarcinoma: New Insights and a Systematic Review of the Literature. Dermatol Surg. 2018;44:1247-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 9. | Tomar SS, Supekar BB, Bhushan R, Mukh, J, Singh R, Bhat D, Jaiswal A. Eccrine porocarcinoma at unusual location. J Dermatol and Dermatologic Surg. 2022;26:S15-S18. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Signorelli C, Zanella-Cavallero L, Ranucci V, Pellicciotti A, Ruggeri EM. Porocarcinoma of the left arm: A report of a rare skin cancer case and literature review. Clin Case Rep. 2022;10:e05721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Salih AM, Kakamad FH, Essa RA, Rauf GM, S A M, H M S, Q S R, A H H, A H D, Othman S. Porocarcinoma: A systematic review of literature with a single case report. Int J Surg Case Rep. 2017;30:13-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |