Published online Jan 26, 2024. doi: 10.12998/wjcc.v12.i3.650
Peer-review started: November 15, 2023
First decision: December 15, 2023
Revised: December 22, 2023
Accepted: January 2, 2024
Article in press: January 2, 2024
Published online: January 26, 2024
Processing time: 63 Days and 21.9 Hours
Cerebral syphilitic gumma is a relatively rare clinical disease. Its clinical manifestations are non-specific, and the imaging manifestations are similar to other in
We report the case to explore the diagnostic essentials of cerebral syphilitic gumma and attempt to mitigate the rates of misdiagnosis and missed diagnosis by equipping physicians with knowledge of neurosyphilis characteristics. The cli
Cerebral syphilitic gumma is rare in clinical practice, and it is often misdiagnosed and missed. Clinical diagnosis should be considered in combination with multiple examinations.
Core Tip: Cerebral syphilitic gumma is a relatively rare clinical disease. Its clinical manifestations are non-specific, and the imaging manifestations are similar to other intracranial occupying lesions, often misdiagnosed as tumors or abscesses. There are few reports on this disease in the relevant literature. To our knowledge, we have reported the first case of cerebral syphilitic gumma misdiagnosed as a brain abscess. We report this case and provide useful information for clinical doctors on neurosyphilis diseases.
- Citation: Mu LK, Cheng LF, Ye J, Zhao MY, Wang JL. Cerebral syphilitic gumma misdiagnosed as brain abscess: A case report. World J Clin Cases 2024; 12(3): 650-656
- URL: https://www.wjgnet.com/2307-8960/full/v12/i3/650.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i3.650
Cerebral syphilitic gumma is a late form of syphilis caused by Treponema pallidum (T. pallidum), which invades the central nervous system and often develops 3-20 years after syphilis infection. Cerebral syphilis gummata is a rare type of neurosyphilis with an incidence of only 2%, and the affected population is mainly middle-aged and elderly men who are mostly newly diagnosed with intracranial masses[1]. With an insidious onset, nonspecific clinical manifestations, and the imaging findings resembling other intracranial space-occupying ring enhancements, the condition poses challenges in differential diagnosis, making it susceptible to misdiagnosis and mistreatment. Surgical treatment, often mistaken for a tumor or abscess, necessitates pathological examination for accurate confirmation of the diagnosis[2]. The clinical data of a patient with cerebral syphilis gummata admitted to the Department of Neurosurgery at Shengli Oilfield Central Hospital are reported below to further deepen our understanding of this disease.
A 55-year-old female patient was admitted to the hospital with “intermittent fever with weakness of right limbs for half a month” on June 28, 2019.
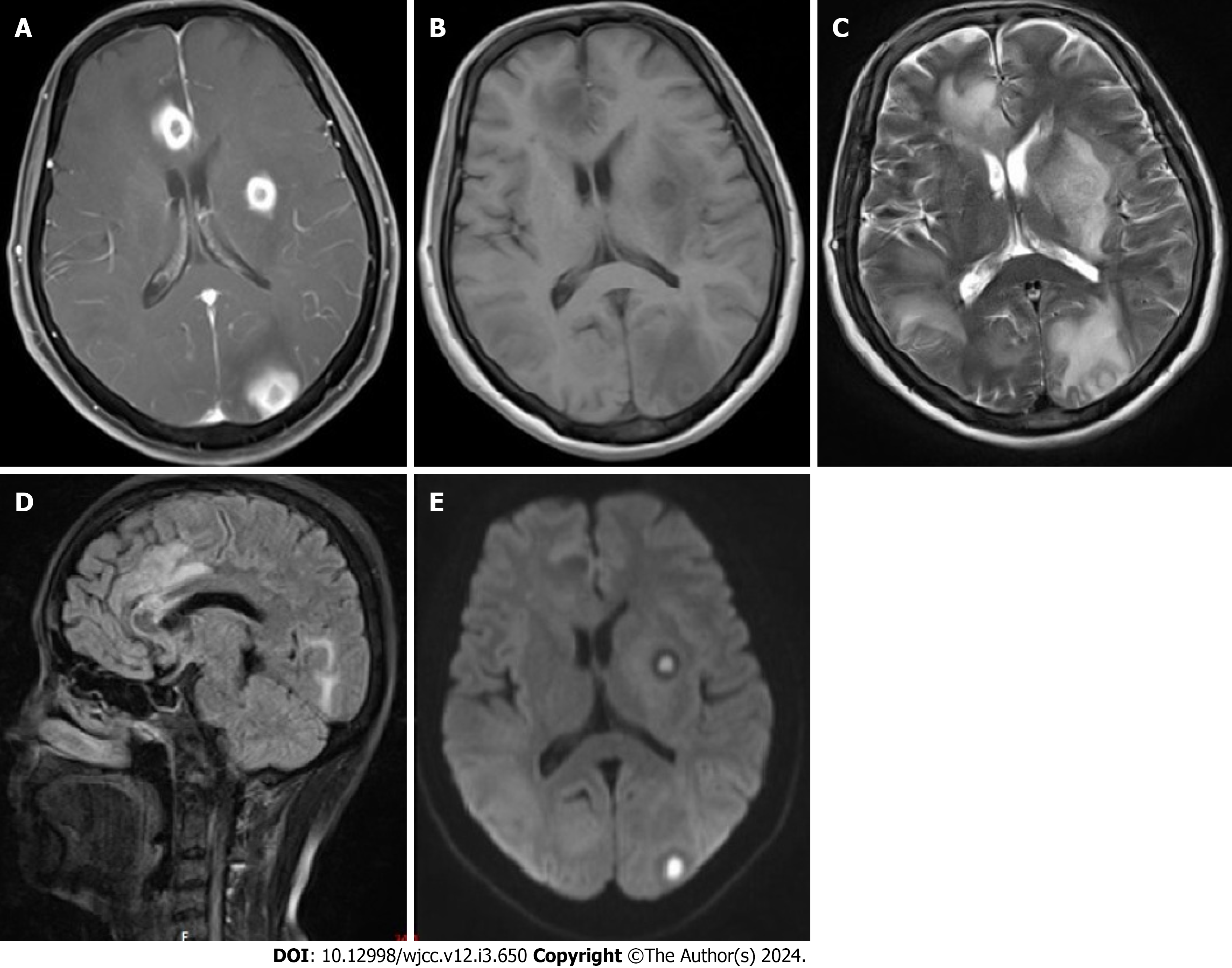
Half a month ago, the patient experienced right limb weakness without obvious cause, coinciding with two episodes of low-grade fever with diarrhea. After oral administration of cephalosporins at a local clinic (details unknown), the patient exhibited marked improvement in diarrhea and return to normal body temperature. However, the right-sided weakness persisted, and there the patient tended to lean towards the right rear while standing. Subsequently, she was referred to our neurology clinic, and brain magnetic resonance imaging (MRI) showed multiple intracranial space-occupying lesions with surrounding edema. Considering the possibility of a brain abscess, metastases were not excluded (Figure 1). On the same day, the patient was admitted to our department with a diagnosis of brain abscess from the neurology clinic. Since the onset of disease, the patient had paroxysmal headache, dizziness, and blurred vision, without limb twitching or numbness.
The patient had a history of “liver abscess” for half a year and underwent puncture drainage of liver abscess and anti-infection treatment in the Department of Hepatobiliary Surgery of our hospital.
The pus culture from the puncture revealed Klebsiella pneumoniae, and the remaining medical history was unre
Physical examination on admission revealed a temperature of 36.9 °C; heart rate, 86 beats/min; respiration, 18 breaths/min; and blood pressure, 131/75 mmHg, and physical examination of the heart, lungs, and abdomen showed no signi
Laboratory tests indicated a white blood cell (WBC) count of 10.9 × 109/L (3.5-9.5 × 109/L), neutrophil percentage of 82.4% (40%-75%), and direct neutrophil count or 9 × 109/L (1.8-6.3 × 109/L). Other blood biochemical parameters showed no significant abnormalities.
Neurological examination revealed clear consciousness, clear and fluent speech, normal orientation, intact calculation, and memory functions. Pupils were equal and round bilaterally, responding well to light sensitivity. Fundus examination identified bilateral papilledema. Eye movements were well-coordinated, and there were no abnormalities in the exami
Preliminary diagnosis included brain abscess and post-puncture drainage of the liver abscess. Abdominal ultrasound after admission showed a 14 mm × 9 mm heterogeneous echogenic area in the right liver; however, positron emission tomography and computed tomography revealed no evidence of malignancy. Considering the patient’s medical history, a hematogenous brain abscess was suspected. The initial approach involved dehydration to reduce intracranial pressure, administration of meropenem for anti-infection, and fluid replacement. Lumbar puncture (July 1, 2019) revealed a cere
The patient did not support the diagnosis of brain abscess during treatment; subsequently, a thorough inquiry into the medical history was conducted again. The patient reported a history of unprotected sexual activity following a divorce. A physical examination conducted 1 year prior had revealed a positive T. pallidum antibody in the blood, with no subse
On July 12, a dermatology consultation was requested, and the recommended treatment plan included: (1) Conducting serological examinations for syphilis in sexual partners and close contacts; and (2) administering intravenous penicillin at 4 million U ivdrip every 6 h × 14 d, subsequently switched to intramuscular benzathine penicillin at 2.4 million U every week × 3 times.
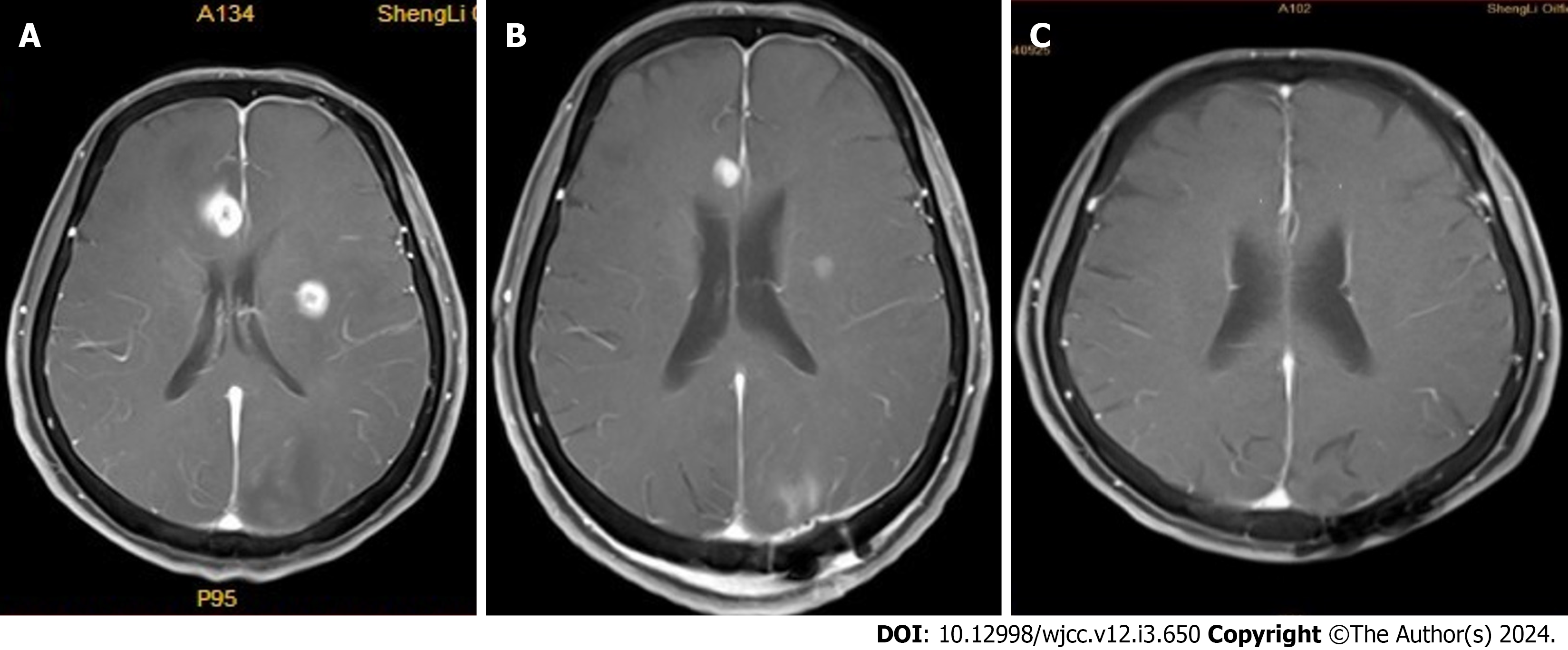
The patient’s symptoms resolved after treatment. Repeated brain MRI (July 25, 2019) showed that the multiple in
Cerebral syphilitic gumma occurs when T. pallidum, originating from a primary infection, spreads throughout the whole body, penetrates the blood-brain barrier, and induces chronic infectious diseases in the central nervous system. Its incidence has increased in recent years[3,4]. Cerebral syphilitic gumma is divided into: (1) Asymptomatic; (2) interstitial syphilis (meningovascular syphilis); (3) parenchymal syphilis (paralytic dementia, spinal phthisis); and (4) gummatous syphilis. Gumma is a late-onset neurosyphilis with a long incubation period that occurs 8-12 years after syphilis infection[5]. Gummatous lesions may appear anywhere in the brain tissue, such as the posterior fossa, pons, midbrain, cerebellopontine angle, corpus callosum, or cerebral convexity[6]. Imaging examinations showed lesions that were either single or multiple. Computed tomography scans exhibited low or isodense areas, with possible ring enhancement. On MR T1WI, the lesions appeared as low or isointensity, while on T2WI, they showed high signal intensity. Post-enhancement, nodular or ring enhancement was observed. However, these imaging findings were similar to other intracranial space-occupying lesions, such as malignant meningioma, glioma, metastases, tuberculoma, cryptococcal tumor, sarcoma, and brain ab
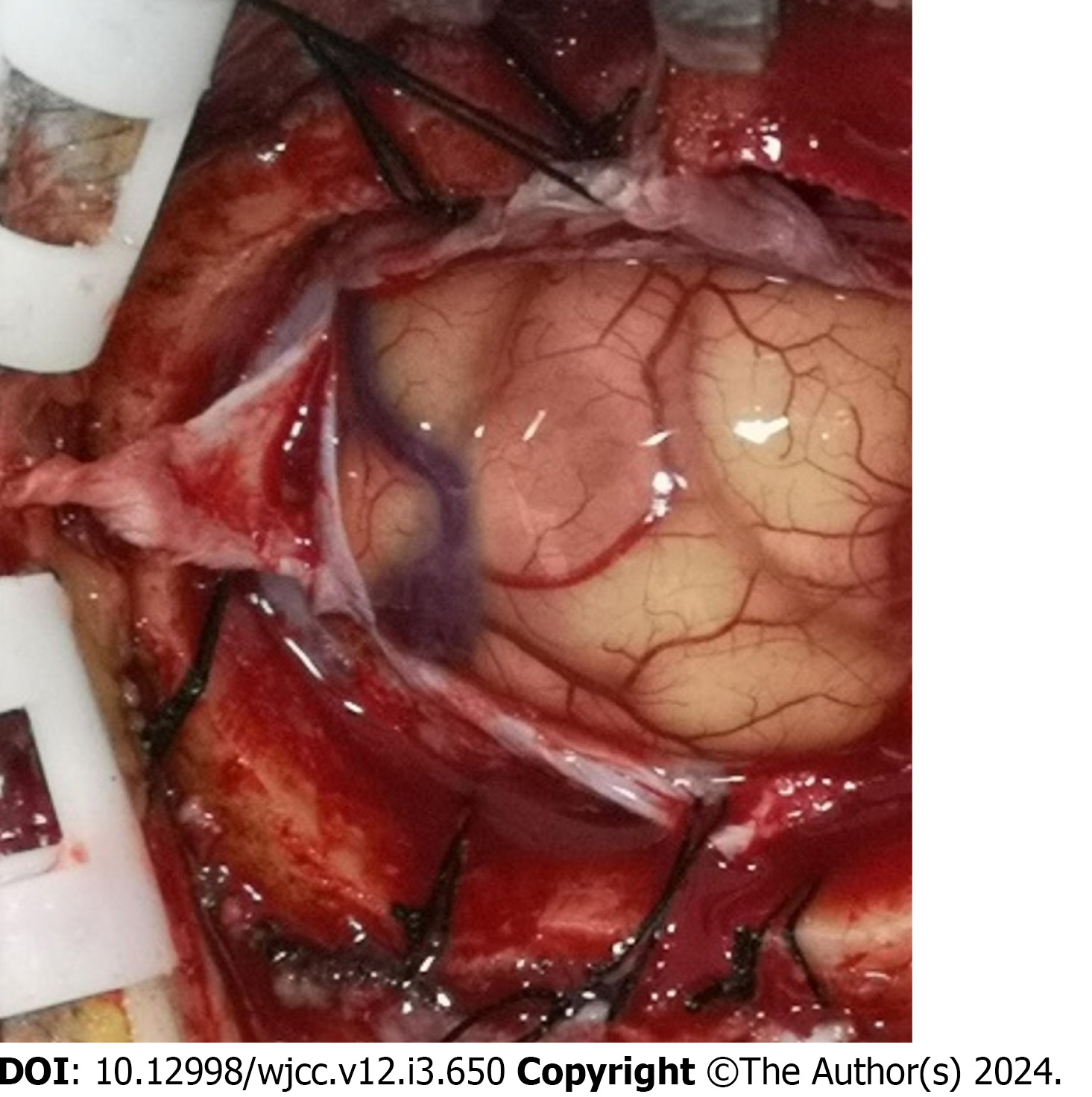
Upon entering the central nervous system, T. pallidum adheres to hyaluronidase on the cell membrane of the vessel’s inner wall, using its own mucopolysaccharide as a receptor. This interaction leads to the decomposition of the mucopolysaccharide of the vessel, resulting in vascular collapse and the development of obliterative arteritis or periarteritis. Because the body’s inflammatory cells infiltrate and develop edema, granulomatous changes occur locally in the damaged area, with caseous necrosis in the center, mostly surrounded by a large area of the edema zone, and the adjacent meninges are often thickened owing to inflammatory reactions. Patients often present with symptoms of increased in
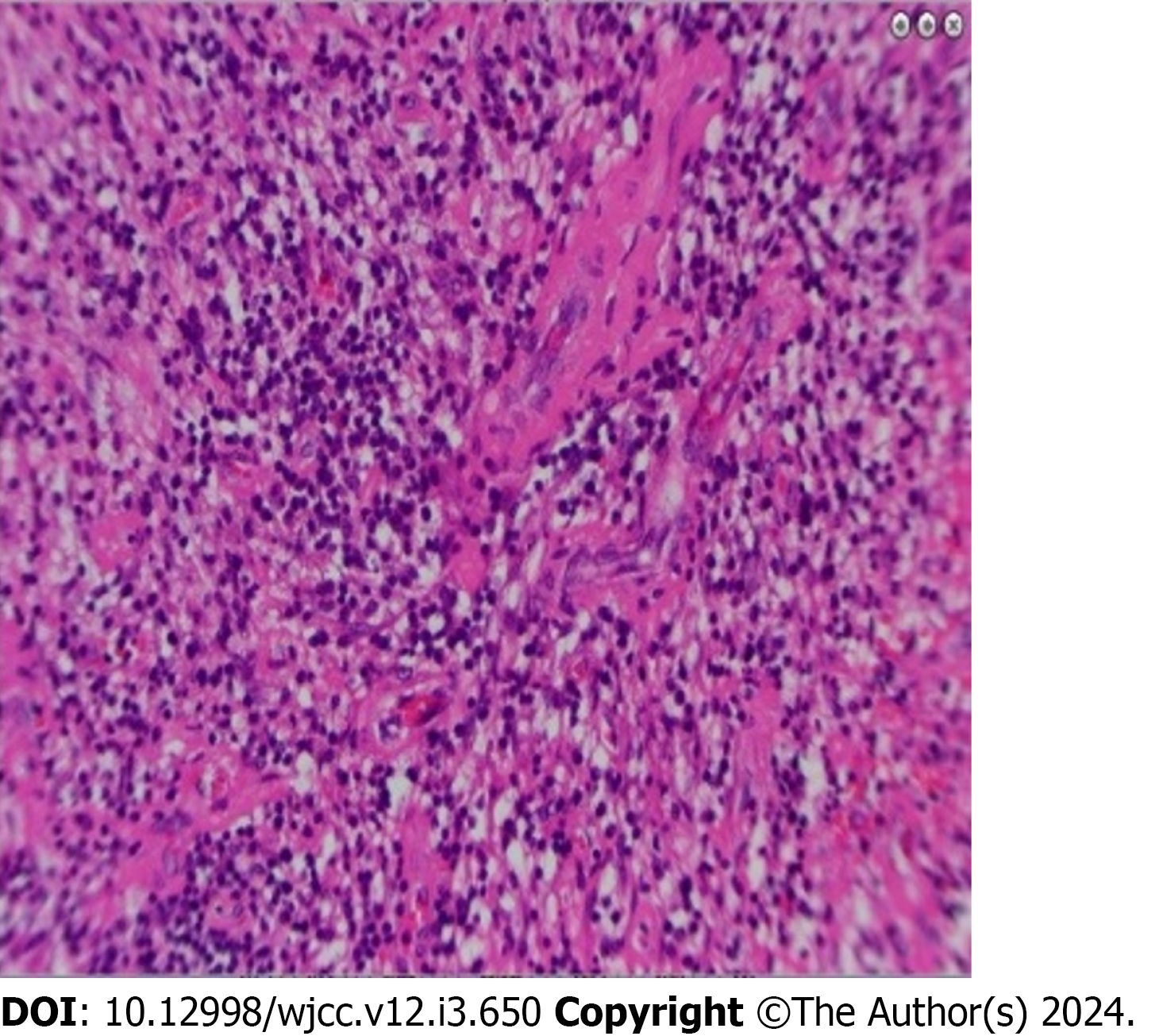
The specimens examined included serum and cerebrospinal fluid, and T. pallidum nonspecific antibody tests rapid plasma reagin test (RPR) and toluidine red unheated serum test are commonly used for screening. Specific antibody tests such as the T. pallidum particle agglutination assay (TPPA), T. pallidum hemagglutination assay, and T. pallidum antibody absorption test can be used to confirm the diagnosis of T. pallidum infection. Positive specific antibodies indicate syphilis infection but cannot distinguish whether the infection is short-term or long-term, whereas nonspecific antibodies can reflect the activity of syphilis infection, and the combination of the two can further confirm the diagnosis. Patients often exhibit abnormal changes in WBC counts and protein levels in the cerebrospinal fluid. Laboratory tests are crucial for the diagnosis and treatment of this disease; however, these results may be false-positive or false-negative. Therefore, based on a full understanding of the clinical history, a comprehensive analysis of imaging examinations and laboratory findings can facilitate a preoperative diagnosis of this disease. Nonetheless, postoperative pathological biopsy remains the gold standard for confirming the diagnosis.
After the diagnosis is confirmed, the patient must be actively treated with antibiotics against syphilis. Remission is often associated with the normalization of cerebrospinal fluid cell counts and reduction of protein levels, such as the reduction and conversion of cerebrospinal fluid RPR and TPPA, indicating good treatment results[8]. Postoperative follow-up showed that the main clinical symptoms of this patient significantly improved and disappeared, and re-examination of the brain MRI showed that the number of lesions was significantly reduced, indicating that the the
Causes of misdiagnosis may include: (1) The patient’s admission with symptoms resembling “intermittent fever”, and a history of “liver abscess”, often leading to misdiagnosis as bacterial infectious diseases; (2) cerebral syphilitic gumma’s rarity in clinical practice, where patients often present to dermatology departments, and neurosurgeons may lack sufficient awareness of this disease; (3) inadequate attention to the patient’s sexual history by medical staff and oversight of the syphilis serological examination results upon admission, contributing to misdiagnosis; and (4) the lack of clear specificity in imaging findings for cerebral syphilitic gumma, further complicating the diagnostic process.
The clinical manifestations of neurosyphilis are complex and similar to those of many neurological and other systemic diseases. Because patients themselves and doctors often misdiagnose and miss the diagnosis owing to the abovementioned reasons, clinicians should enhance their understanding of neurosyphilis, heighten disease awareness during clinical processes, and consider neurosyphilis when facing unexplained central nervous system infections, cerebro
The authors would like to thank the patient for permitting us to use her clinical information in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kaur M, United States S-Editor: Chen YL L-Editor: Filipodia P-Editor: Xu ZH
| 1. | Li JC, Mahta A, Kim RY, Saria M, Kesari S. Cerebral syphilitic gumma: a case report and review of the literature. Neurol Sci. 2012;33:1179-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Liu LL, Zheng WH, Tong ML, Liu GL, Zhang HL, Fu ZG, Lin LR, Yang TC. Ischemic stroke as a primary symptom of neurosyphilis among HIV-negative emergency patients. J Neurol Sci. 2012;317:35-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Karsan N, Barker R, O'Dwyer JP. Clinical reasoning: the "great imitator". Neurology. 2014;83:e188-e196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Timmermans M, Carr J. Neurosyphilis in the modern era. J Neurol Neurosurg Psychiatry. 2004;75:1727-1730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 122] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Singh AE, Romanowski B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features. Clin Microbiol Rev. 1999;12:187-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 336] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 6. | Darwish BS, Fowler A, Ong M, Swaminothan A, Abraszko R. Intracranial syphilitic gumma resembling malignant brain tumour. J Clin Neurosci. 2008;15:308-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Agrons GA, Han SS, Husson MA, Simeone F. MR imaging of cerebral gumma. AJNR Am J Neuroradiol. 1991;12:80-81. [PubMed] |
| 8. | Casolla B, Ristori G, Romano A, Bozzao A, Orzi F. Subacute multicranial neuropathy revealing an early case of meningeal syphilis. Neurol Sci. 2015;36:1033-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |