Published online Jan 26, 2024. doi: 10.12998/wjcc.v12.i3.601
Peer-review started: October 11, 2023
First decision: December 5, 2023
Revised: December 16, 2023
Accepted: January 4, 2024
Article in press: January 4, 2024
Published online: January 26, 2024
Processing time: 98 Days and 21.1 Hours
Polyneuropathy, organomegaly, endocrinopathy, M-protein, skin changes (POEMS) syndrome is a rare paraneoplastic syndrome that encompass multiple systems. The most common clinical symptoms of POEMS syndrome are pro
Herein, we report the case of a 59-year-old woman with POEMS syndrome that involved dilated cardiomyopathy. The patient presented to the hospital with complaints of shortness of breath and discomfort in the chest. The patient reported previous experiences of limb numbness. During hospitalization, the brain natriuretic peptide levels were 3504.0 pg/mL. Color doppler echocardiography showed an enlarged left side of the heart, along with ventricular wall hypokinesis and compromised functioning of the same side of the heart. Ab
When patients with cardiomyopathy have systemic manifestations such as numb limbs and darkening skin, the POEMS syndrome is the most possible diagnosis.
Core Tip: Polyneuropathy, organomegaly, endocrinopathy, M-protein, skin changes (POEMS) syndrome is a rare paraneoplastic syndrome that encompass multiple systems. Diagnoses are often delayed because the unusual and atypical nature of the syndrome, exposing patients to possibly severe disability. Our report presents the first case of a 59-year-old Chinese female with newly diagnosed dilated cardiomyopathy and POEMS syndrome. Although POEMS syndrome with dilated cardiomyopathy is rare, physicians should consider it when patients with cardiomyopathy have systemic manifestations.
- Citation: Li JR, Feng LY, Li JW, Liao Y, Liu FQ. Polyneuropathy, organomegaly, endocrinopathy, M-protein, skin changes syndrome with dilated cardiomyopathy: A case report. World J Clin Cases 2024; 12(3): 601-606
- URL: https://www.wjgnet.com/2307-8960/full/v12/i3/601.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i3.601
Polyneuropathy, organomegaly, endocrinopathy, M-protein, skin changes (POEMS) syndrome is a rare condition that is characterized by monoclonal plasma cell disorder, peripheral neuropathy, and other systemic symptoms[1]. In 2003, a national survey that was conducted in Japan revealed a prevalence of approximately 0.3 per 100000[2]. However, more cases have been reported from China and India[3,4].
Currently, the mechanism that leads to the initiation and progression of POEMS is unclear. However, it is suggested that the vascular endothelial growth factor (VEGF), together with pro-inflammatory cytokines such as tumor necrosis factor-alfa, interleukin-6 (IL-6) and IL-12, might be involved in the pathogenesis of POEMS syndrome[5].
In China, the median age for the onset of POEMS syndrome is 46 years, with a male to female ratio of 2.23:1[6]. The most common symptoms of the POEMS syndrome include peripheral neuropathy, endocrine abnormalities, skin changes, organomegaly, and extravascular volume overload. Typically, the diagnosis is delayed by 12-16 mo due to a range of systemic manifestations that are often overlooked as trivial comorbidities[7]. The median survival time was only 5-7 yr in China in cases where treatment is unsuccessful[3]. The most common causes of death among patients with POEMS syndrome are cardiorespiratory failure, progressive inanition, infection, capillary leak-like syndrome, and renal failure[6]. Case reports about POEMS syndrome with dilated cardiomyopathy are relatively rare. Therefore, identifying atypical symptoms can improve the prognosis and quality of life among POEMS syndrome patients.
In this study, we report a case of POEMS syndrome with dilated cardiomyopathy in a 59-year-old woman. The clinical features and treatment methods for POEMS syndrome were summarized based on information that was obtained from literature. Some manifestations that may be overlooked during the diagnosis process were also highlighted.
A 59-year-old Chinese woman was admitted to the hospital with symptoms of shortness of breath and discomfort in the chest, which had been experienced for 1 mo.
There were no apparent triggers that were associated with the symptoms prior to presentation at our hospital. During the course of illness, the patient had abdominal distension, nausea, edema, and paroxysmal nocturnal dyspnea. However, the patient did not experience chest pain, abdominal pain, fever, cough, expectoration, and walking difficulties.
The patient experienced limb numbness for three years, but without systematic diagnosis and treatment. She denied the existence of underlying conditions like hypertension, diabetes, cardiomyopathy, and coronary heart disease.
The patient had no significant history of smoking, drinking alcohol, and medication or food allergies. According to the information provided by the patient, there were no cases of cardiomyopathy in the family history. Moreover, the patient’s children are healthy.
Physical examination of the patient showed the following results: body temperature was 36.8 °C; blood pressure was 159/99 mmHg; heart rate was 78 beats/min; and respiratory rate was 20 breath/min. Furthermore, the patient developed symptoms of cardiac enlargement, depressed edema of both lower limbs, and limb pigmentation.
Upon admission, the laboratory data showed that brain natriuretic peptide levels were 3504.0 pg/mL. Blood routine tests revealed a platelet count of 492 × 109/L. The C-response protein levels were 33.78 mg/L while the urinary microalbumin concentration was 104 mg/L. There were no abnormal findings from the routine tests for the feces, urine, blood coagulation parameters, thyroid function, serum complement, rheumatoid factor, antinuclear antibody spectrum, cortisol, and adrenocorticotropic hormone rhythm. Immunoelectrophoresis of the serum showed the presence of a monoclonal IGA λ M protein. The VEGF levels were 622.56 pg/mL. Electromyography was described as a symmetric sensorimotor demyelinating polyneuropathy.
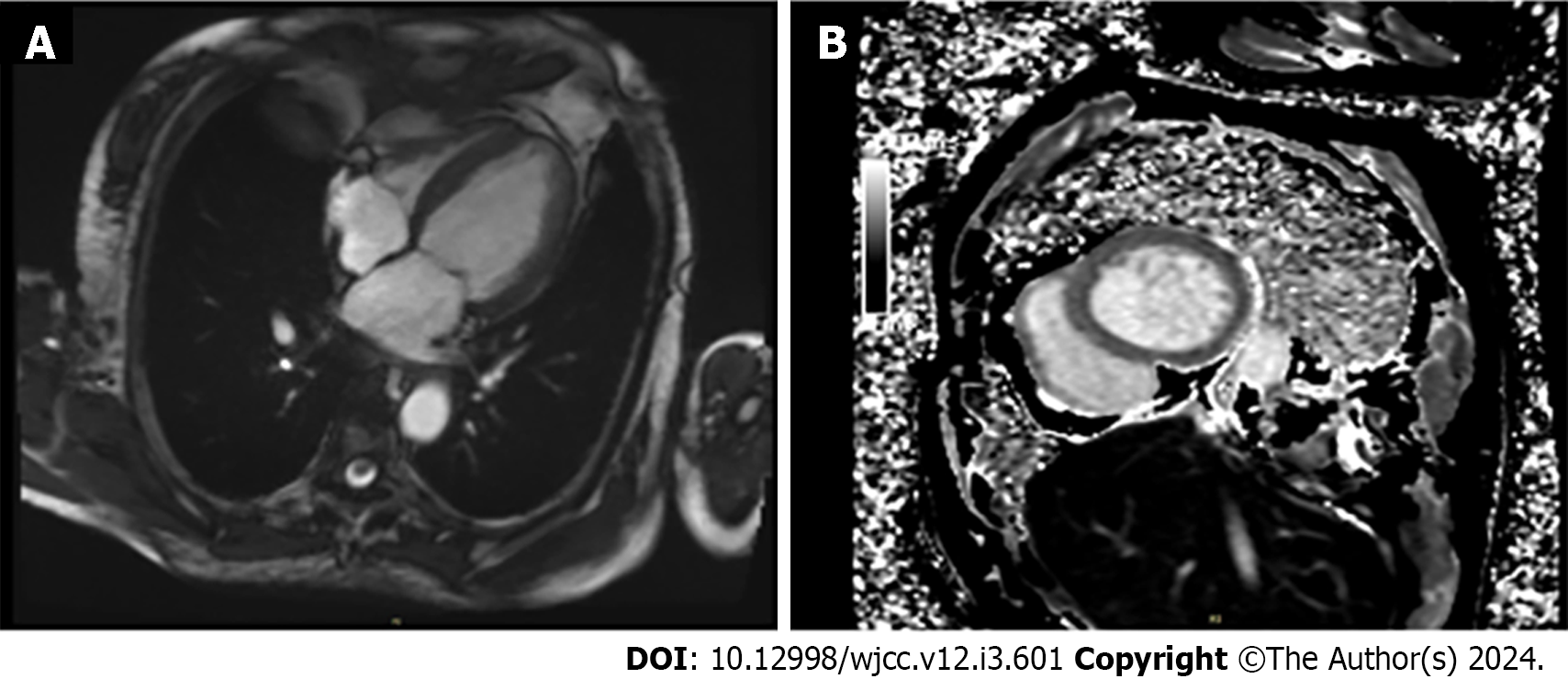
Color doppler echocardiography showed that the patient had an enlarged left atrium (inner diameter of 43.0 mm) and left ventricle (inner diameter of 62.0 mm). Ventricular wall hypokinesis and decreased functioning of the left side of the heart (ejection fraction 50%) were also observed. Cardiac magnetic resonance imaging also showed an enlarged left side of the heart, along with slight myocardical fibrosis (Figure 1). According to the results from abdominal color ultrasonography, the spleen had increased in size.
Bone marrow biopsy was performed when the patient was hospitalized. The findings showed megakaryocyte hyperplasia, a constant number of immature cells, and plasma cells that were scattered in a few or individual small foci (approximately 2%-20%). Flow cytometry for the bone marrow showed that normal plasma cells accounted for 0.2% of nuclear cells. Antigens such as CD38, CD138, CD27, CD19, kappa, and lamda were expressed by these plasma cells. However, antigens like CD56 and CD117 were not expressed. No monoclonal plasma cells were detected through immunohistochemical staining of the bone marrow.
Based on the patient's medical history, laboratory and imaging examination results, and bone marrow biopsy, the final diagnosis was POEMS syndrome with dilated cardiomyopathy.
While waiting for the bone marrow biopsy report, the patient received treatment to reduce cardiac preload, diuresis, control the ventricular rate, and maintain the electrolyte balance. On the 15th of February, the bone marrow biopsy confirmed that the patient had POEMS syndrome with dilated cardiomyopathy. The prognosis of POEMS was stratified into high-risk groups. After communicating with the patient about the risks and costs of various treatments, she chose treatment with lenalidomide-dexamethasone.
After four months of follow-up, the shortness of breath and discomfort in the chest disappeared, while numbness significantly improved. Laboratory indicators (Table 1) such as brain natriuretic peptide also remarkably improved.
| Base-line | First follow-up visit | Second follow-up visit | Laboratory reference range | |
| WBC (109/L) | 6.55 | 5.75 | 7.45 | 3.69-9.16 |
| NE (109/L) | 4.40 | 3.91 | 3.73 | 2.00-7.00 |
| PLT (109/L) | 492 | 454 | 385 | 101-320 |
| HB (g/L) | 111 | 105 | 104 | 110-150 |
| CRP (mg/L) | 33.78 | 44.88 | 5.13 | 0.00-3.00 |
| BNP (pg/mL) | 3504 | 1469 | - | 0-900 |
POEMS syndrome is a rare paraneoplastic syndrome caused by a plasma cell proliferative disorder. The mechanism of POEMS syndrome is complex and currently unclear. The pathogenesis of POEMS is thought to arise from a cytokine imbalance that is characterized by excessive production of multiple proinflammatory and angiogenic cytokines (IL-1β, IL-6, fibroblast growth factor, and IL-12) as well as the suppression of anti-inflammatory cytokines (transforming growth factor β1)[8]. Kourelis et al[9] reported an increase in programmed cell death protein 1-positive CD4+ T-cells and a decrease in naive CD4+ T-cells in patients with POEMS syndrome. This indicated a chronic antigenic stimulation of CD4+ T-cells and their consequent exhaustion. In addition, the serum levels of the VEGF are elevated in most patients with POEMS syndrome.
It is hypothesized that some of the manifestations of POEMS syndrome are associated with VEGF-induced endothelial dysfunction, vascular wall hypertrophy, and tissue edema[10]. Recently, treatments that target the plasma cells that produce the M-protein have shown excellent clinical responses. This suggests that the M-protein might be one of the driving factors of the disease[11]. Additionally, patients with an M-protein restricted to clonal immunoglobulin λ light variable chain -1-40 experienced severe clinical symptoms[12]. However, the mechanism underlying the pathogenesis of POEMS syndrome still needs to be explored.
The most common symptoms of POEMS syndrome are peripheral neuropathy, endocrine abnormalities, skin changes, organomegaly, and extravascular volume overload. The rate at which POEMS syndrome is misdiagnosed is extremely high due to its diverse atypical symptoms. The diagnosis of POEMS syndrome is confirmed when both of the mandatory major criteria, one of the three other major criteria, and one of the six minor criteria are positive[13]. The mandatory major criteria consists of polyneuropathy and monoclonal plasma cell-proliferative disorder (almost always λ). The other major criteria include Castleman disease, sclerotic bone lesions, and VEGF. The minor criteria is made up of organomegaly, extravascular volume overload, endocrinopathy, skin changes, papilledema, and thrombocytosis. Therefore, the diag
Risk stratification is limited to clinical phenotypes rather than specific molecular markers. Some of the common risk factors are age, low serum albumin, pleural effusion, pulmonary hypertension, and reduced estimated glomerular filtration rate[13]. It is also important to note that the VEGF levels in the plasma and serum correlate with the activity of POEMS syndrome[13].
We report the case of a middle-aged woman with POEMS syndrome. Initially, the patient experienced shortness of breath and discomfort in the chest. The patient confirmed heart failure after the laboratory examinations. Furthermore, color doppler echocardiography showed that the left side of the heart had increased in size. Ventricular wall hypokinesis was also observed, although no previous cardiovascular risk factors and associated genetic history had been reported. Moreover, the patient experienced limb numbness and pigmentation. Therefore, we considered the possibility that there could be other causes of myocardial enlargement in the patient. Further examinations were completed to aid diagnosis. Electromyography was described as a symmetric sensorimotor demyelinating polyneuropathy. Immunoelectrophoresis of the serum showed the presence of a monoclonal IGA λ M protein. The other results were as follows: the VEGF levels were 622.56 pg/mL; cardiac magnetic resonance imaging showed an enlarged left side of the heart as well as slight myocardical fibrosis; flow cytometric and immunohistochemical staining of bone marrow detected no monoclonal plasma cells. The clinical characteristics of this patient were as follows: Demyelinating polyneuropathy, positive M protein, VEGF elevation, splenomegaly, enlarged left heart and slight myocardical fibrosis, skin changes, and edema. After all the tests, the patient was diagnosed with POEMS syndrome associated with dilated cardiomyopathy.
Cardiac involvements in POEMS syndrome are rare and heterogenous. The most common type of cardiac involvement is pulmonary hypertension with resultant right ventricular dysfunction. However, there are few reports of cardiomyopathy, arrhythmia, and pericarditis[13-17]. Shimizu et al[15] reported the first case of POEMS syndrome that was accompanied by hypertrophic cardiomyopathy. Tanus and Miller[16] presented a case of POEMS syndrome that had cardiomegaly and cardiomyopathy. Abdelahad et al[17] presented a 28-year-old African American with a history of POEMS syndrome, in addition to an unfortunate newly diagnosed dilated, non-ischemic cardiomyopathy. Therefore, our report presents the first case of a 59-year-old Chinese female with newly diagnosed dilated cardiomyopathy and POEMS syndrome.
The evidence regarding the treatment in POEMS syndrome is largely limited to retrospective cohort studies[18,19]. However, POEMS syndrome can be treated using radiotherapy, autologous stem cell transplant, bortezomib, therapies targeting VEGF, alkylating chemotherapy, dexamethasone, thalidomide, and lenalidomide. The treatment of POEMS syndrome depends on the presence of marrow plasma cell infiltration and the number of bone lesions[8]. POEMS syndrome patients who have one to three bone lesions and no clonal plasma cells should receive radiation therapy. Once a disseminated disease is identified, systemic therapy is recommended with the caveat that large bony lesions with a significant lytic component may require adjuvant radiation therapy[13]. This indicates that autologous stem cell transplantation have significant clinical improvement in surviving patients with POEMS syndrome[13].
After treatment with melphalan-dexamethasone, hematologic response was reported inn 81% of the patients with POEMS syndrome while 100% showed neurologic improvement[13]. After treatment with lenalidomied-dexamethasone, 75%-95% patients showed significant clinical and VEGF improvement[13]. Thalidomide and bortezomib are not recommended as first line treatments because they may exacerbate the risk of peripheral neuropathy[13]. On the other hand, bevacizumab does not offer consistent benefits to patients with POEMS syndrome[13].
Our report presents the first case of a 59-year-old Chinese female with newly diagnosed dilated cardiomyopathy and POEMS syndrome. Although POEMS syndrome with dilated cardiomyopathy is rare, physicians should consider it when patients with cardiomyopathy have systemic manifestations. Early diagnosis and therapy can improve the prognosis of POEMS syndrome in patients, thereby enhancing their quality of life.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shamseldeen AM, Egypt; Yildiz K, Turkey S-Editor: Gao CC L-Editor: A P-Editor: Chen YX
| 1. | Ali T, Qazilbash MH. POEMS syndrome: A multisystem clonal disorder. Eur J Haematol. 2021;106:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Dispenzieri A, Kyle RA, Lacy MQ, Rajkumar SV, Therneau TM, Larson DR, Greipp PR, Witzig TE, Basu R, Suarez GA, Fonseca R, Lust JA, Gertz MA. POEMS syndrome: definitions and long-term outcome. Blood. 2003;101:2496-2506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 562] [Cited by in RCA: 492] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 3. | Li J, Zhou DB, Huang Z, Jiao L, Duan MH, Zhang W, Zhao YQ, Shen T. Clinical characteristics and long-term outcome of patients with POEMS syndrome in China. Ann Hematol. 2011;90:819-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 4. | Kulkarni GB, Mahadevan A, Taly AB, Yasha TC, Seshagiri KS, Nalini A, Satishchandra P, Veerendrakumar M, Shankar SK. Clinicopathological profile of polyneuropathy, organomegaly, endocrinopathy, M protein and skin changes (POEMS) syndrome. J Clin Neurosci. 2011;18:356-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Cerri F, Falzone YM, Riva N, Quattrini A. An update on the diagnosis and management of the polyneuropathy of POEMS syndrome. J Neurol. 2019;266:258-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Wang Y, Huang LB, Shi YH, Fu H, Xu Z, Zheng GQ, Wang Y. Characteristics of 1946 Cases of POEMS Syndrome in Chinese Subjects: A Literature-Based Study. Front Immunol. 2019;10:1428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | D'Sa S, Khwaja J, Keddie S, Keh RY, Smyth D, Ronneberger R, Dubash S, Sivabalasingham S, Wan S, Hoskote C, Baldeweg S, Sive J, Lunn MP. Comprehensive Diagnosis and Management of POEMS Syndrome. Hemasphere. 2022;6:e796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Khouri J, Nakashima M, Wong S. Update on the Diagnosis and Treatment of POEMS (Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal Gammopathy, and Skin Changes) Syndrome: A Review. JAMA Oncol. 2021;7:1383-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Kourelis TV, Jevremovic D, Jessen E, Dasari S, Villasboas JC, Dispenzieri A, Kumar S. Mass cytometry identifies expansion of double positive and exhausted T cell subsets in the tumour microenvironment of patients with POEMS syndrome. Br J Haematol. 2020;190:79-83. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Watanabe O, Maruyama I, Arimura K, Kitajima I, Arimura H, Hanatani M, Matsuo K, Arisato T, Osame M. Overproduction of vascular endothelial growth factor/vascular permeability factor is causative in Crow-Fukase (POEMS) syndrome. Muscle Nerve. 1998;21:1390-1397. [PubMed] [DOI] [Full Text] |
| 11. | Bou Zerdan M, George TI, Bunting ST, Chaulagain CP. Recent Advances in the Treatment and Supportive Care of POEMS Syndrome. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 12. | Li J, Huang Z, Duan MH, Zhang W, Chen M, Cao XX, Guan HZ, Tian Z, Zhou DB. Characterization of immunoglobulin λ light chain variable region (IGLV) gene and its relationship with clinical features in patients with POEMS syndrome. Ann Hematol. 2012;91:1251-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Dispenzieri A. POEMS Syndrome: 2019 Update on diagnosis, risk-stratification, and management. Am J Hematol. 2019;94:812-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 126] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 14. | Levene J, Murray N, Desai S, Simpson TF, Karam C, Silbermann R, Masri A. Pericardial Tamponade and Other Cardiac Complications in POEMS Syndrome. JACC Case Rep. 2021;3:286-290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Shimizu N, Goya M, Akimoto H, Koike A, Nogami A, Ito H, Marumo F, Hiroe M. Cardiomyopathy in a case of Crow-Fukase syndrome. Jpn Heart J. 1997;38:877-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Tanus T, Miller HJ. POEMS syndrome presenting with cardiomegaly and cardiomyopathy. J Intern Med. 1992;231:445-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Abdelahad M, Pearson R, Mauri B, Fenton K, Savu C. Heart Failure With Cardiogenic Shock as a Manifestation of Untreated POEMS (Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal Protein, Skin Changes) Syndrome. Cureus. 2021;13:e18046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Inoue D, Kato A, Tabata S, Kitai T, Takiuchi Y, Kimura T, Shimoji S, Mori M, Nagai Y, Togami K, Matsushita A, Nagai K, Maruoka H, Imai Y, Beppu M, Kawamoto M, Takahashi T. Successful treatment of POEMS syndrome complicated by severe congestive heart failure with thalidomide. Intern Med. 2010;49:461-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Brown R, Ginsberg L. POEMS syndrome: clinical update. J Neurol. 2019;266:268-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |