Published online Oct 6, 2024. doi: 10.12998/wjcc.v12.i28.6204
Revised: July 27, 2024
Accepted: July 31, 2024
Published online: October 6, 2024
Processing time: 66 Days and 18.6 Hours
Traditional paper-based preoperative patient education is a struggle for new nurses and requires extensive training. In this situation, virtual reality technology can help the new nurses. Despite its potential benefits, there are studies on patient satisfaction but there is limited information on the usability of virtual reality (VR) technology for new nurses in giving preoperative education to patients.
To investigate the impact on satisfaction, usability, and burnout of a system using VR technology in preoperative patient education.
The study involved 20 nurses from the plastic surgery ward and 80 patients admitted between April and May 2019. Each nurse taught four patients: Two using traditional verbal education and two using virtual reality. The System Usability Scale, After-Scenario Questionnaire, and Maslach Burnout Inventory (MBI) were employed to evaluate the impact of these education methods.
The VR education groups showed a statistically higher satisfaction than the traditional verbal education groups. Among the three subscales of the MBI, emotional exhaustion and personal accomplishment improved statistically significantly. VR was also better in terms of usability.
This study suggests VR enhances usability and reduces burnout in nurses, but further research is needed to assess its impact on depersonalization and objective measures like stress and heart rate.
Core Tip: Virtual reality technology proved to be significantly more satisfactory and usable than traditional paper based methods for healthcare providers (especially for nurses) working in plastic surgeries wards.
- Citation: Kim J, Kim D, Oh SH, Kwon H. Virtual reality for preoperative patient education: Impact on satisfaction, usability, and burnout from the perspective of new nurses. World J Clin Cases 2024; 12(28): 6204-6216
- URL: https://www.wjgnet.com/2307-8960/full/v12/i28/6204.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i28.6204
In recent years, virtual reality (VR) technology has evolved rapidly, opening new possibilities for many industries, including healthcare[1]. With the aid of VR technology, users can engage in immersive and realistic experiences in computer-generated environments and simulations. It has been applied to a variety of patient care, including psychotherapy[2], medical education[3], pain management[4], and rehabilitation[5]. VR can provide patients with a simpler approach for understanding complicated medical procedures in preoperative situations[6,7]. More dynamically and interestingly, it enables patients to experience the procedure and understand the possible risks and complications[8].
In addition, traditional paper-based preoperative patient education is stressful for new nurses, requires extensive training[9], and the patients receive varying levels of instruction as a result of nurses' various understandings and practices[10].
Receiving varying degrees of care from various nurses is a concern in terms of quality of nursing. Furthermore, the learning curve that new nurses must go through to overcome this can deplete their energy and produce excessive stress, leading to work dissatisfaction and maladjustment, poor mental and physical impacts, and burnout[11].
Burnout is a phenomenon characterized by emotional exhaustion, depersonalization, and a sense of poor accom
According to one study, 43% of nurses who reported high levels of burnout showed plans to quit compared to just 11% of non-burned-out nurses, indicating that managing burnout can help keep experienced nurses in the field for a longer period[18]. Another study showed that healthcare employees had a 32% greater risk of suicide than non-healthcare workers. Medical support staff had the highest annual suicide rate per 100000 among healthcare workers, followed by nurses at 16.0[19].
In this situation, virtual reality technology can help both the patient and the new nurse. Despite its potential benefits, there are studies on patient satisfaction[6,20,21] but there are limited studies on the satisfaction and usability of VR technology for preoperative education of new nurses and its impact on burnout of new nurses. We hypothesized that using VR technology would result in higher satisfaction and usability for new nurses compared to traditional paper-based methods, and that it would reduce burnout and promote wellness. Thus, this study aims to compare the satisfaction and usability, impact on burnout of new nurses of a system using VR technology with traditional paper-based methods in preoperative patient education from the perspective of new nurses.
This study was approved by the Research Ethics Board of Chungnam National University Hospital (approval no. CNUH 2019-06-008-002) and informed consent was obtained from all participants. From April to December 2019, this study involved 20 nurses from the plastic surgery ward of Chungnam National University Hospital in Daejeon, South Korea. All nurses who participated in the study had been working at the advanced beginner level with less than two years of experience[22] (Table 1).
| Characteristics of participating nurses | |||
| Sex | Male | 0 | (0/20) |
| Female | 20 | (20/20) | |
| Mean age, years | 24.4 | ||
| Mean years of experience | 2.3 | ||
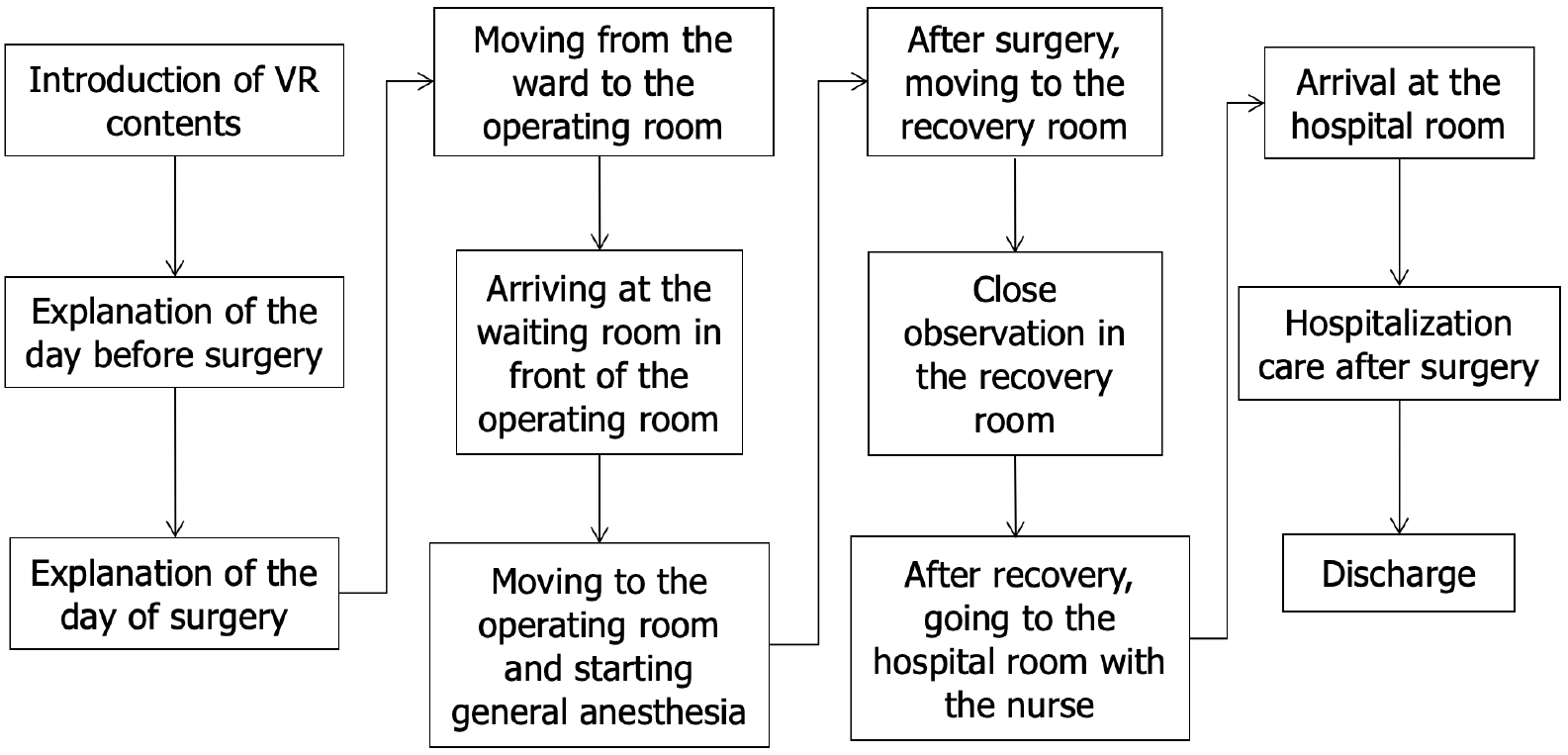
The Department of Anesthesiology and Pain Medicine and the Department of Plastic Surgery collaborated to create a scenario of educational content using VR before and after surgery. Subsequently, VR contents for the full hospitalization process, pre-surgery education, procedures on the day of surgery, and discharge were produced based on the completed scenario. In particular, general education the day before and at the time for surgery, shifting from the ward bed to the stretcher car, arrival in front of the operating room via the elevator, wait and entry into the waiting room, entry into the operating room, laying on the operating bed for general anesthesia, shifting of the patient to the recovery room and hospital room after surgery, and discharge from the hospital after recovery was implemented using VR (Figure 1). An Insta360 ONE X (Insta 360, Seoul, South Korea) was used to record the video. Multiple persons can watch the presentation at once using a PICO G2 head mount device (PICO Interactive Korea Co., Ltd., Seoul, South Korea). The full video can be viewed on YouTube at https://www.youtube.com/watch?v=thq3GikfPL4&t=11s.
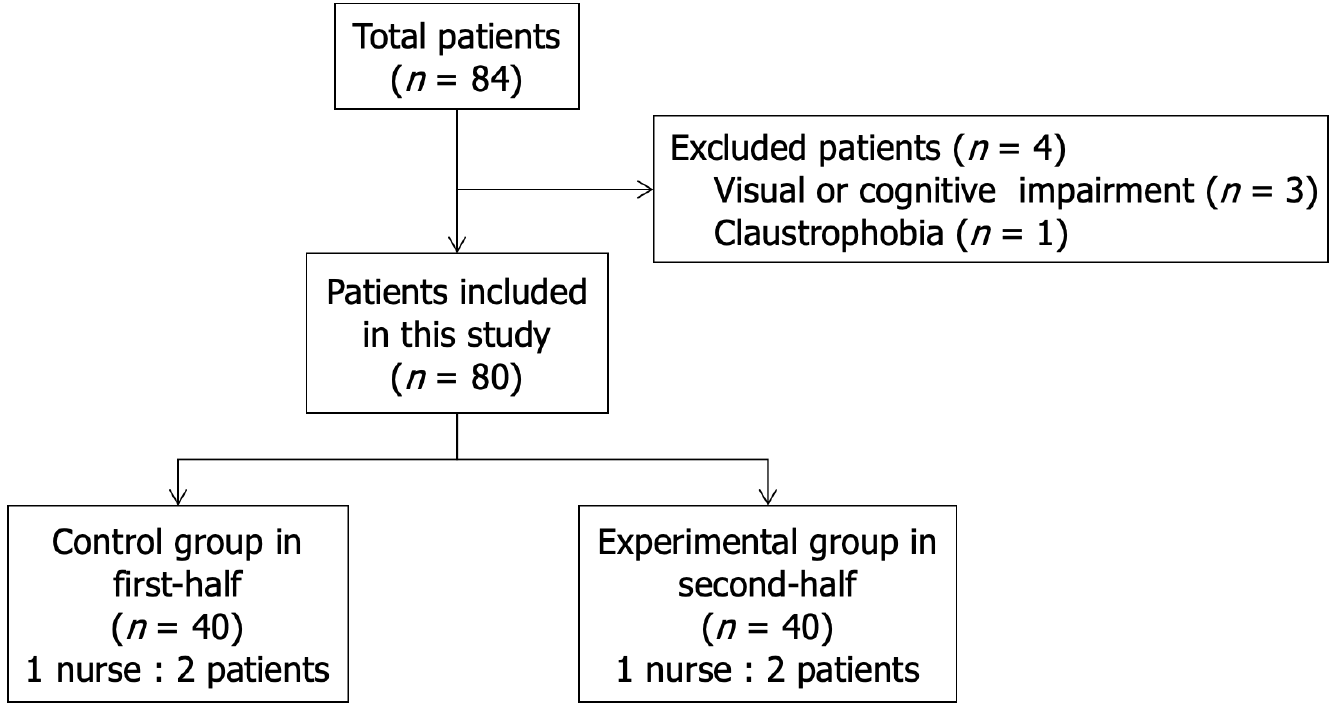
Patients who were admitted to our plastic surgery department between April 21, 2019, and May 31, 2019, and underwent their first operation under general anesthesia served as the study participants. Patients who could not benefit from VR education because of cognitive disability, visual impairment, claustrophobia, or those who refused to participate in the questionnaire were excluded. After excluding unsuitable patients, we used randomization software (Random Allocation Software, version 1.0; Isfahan Medical Sciences) to randomly assign the 40 patients in the control group to 20 ward nurses in groups of two (Figure 2).
Each patient was hospitalized the day before surgery, and the nurses who participated in the study (n = 20) provided traditional paper-based education to the two control group patients assigned to each participating nurse and completed satisfaction, usability, burnout surveys the following day. After the preoperative patient education of the control group and the satisfaction, usability, burnout surveys of the nurses who participated in the study, the preoperative education using VR and satisfaction, usability, burnout surveys were conducted in the same manner as for the control group (n = 40) (Figure 3). Patient characteristics are listed in Table 2. Age was tested for homogeneity between the two groups using an independent t-test, sex was tested using a χ2 test, and the type of surgery was tested using Fisher’s exact test. After patient education, and satisfaction, usability, burnout surveys were conducted.
| Characteristics of the patients | Control group (n = 40), n of mean ± SD | VR Group(n = 40), n of mean ± SD | t | P value | |||
| Sex | Male | 25 | (25/40) | 27 | (27/40) | 0.815 | |
| Female | 15 | (15/40) | 13 | (13/40) | |||
| Mean age, years | 42.75 ± 13.23 | 40.75 ± 15.60 | 0.62 | 0.538 | |||
| Type of operation | Facial trauma | 26 | (26/40) | 25 | (25/40) | 0.717 | |
| Limb or trunk reconstruction | 3 | (3/40) | 3 | (3/40) | |||
| Corrective rhinoplasty | 2 | (2/40) | 1 | (1/40) | |||
| Benign tumor excision | 7 | (7/40) | 10 | (10/40) | |||
| Breast augmentation | 0 | (0/40) | 1 | (1/40) | |||
| etc. (Skin cancer, burn) | 2 | (2/40) | 0 | (0/40) | |||
To investigate satisfaction, the seven items in the questionnaire were scored on a 5-point Likert scale. Items 3 and 4 were designed as reverse questions, and considered in the following statistical analyses (Table 3).
| Strongly disagree (1) | Disagree (2) | Neutral (3) | Agree (4) | Strongly disagree (5) | |
| 1 Does the amount of time needed for preoperative education make sense? | |||||
| 2 Is a preoperative education making your job more difficult? | |||||
| 3 Does a preoperative education make you more physically stressed? | |||||
| 4 Does a preoperative education make you more mentally stressed? | |||||
| 5 After explaining the procedure to the patient, do you feel satisfied? | |||||
| 6 Do you believe that by giving the patient precise information, your preoperative education satisfied them? | |||||
| 7 Do you employ effective communication skills or tools in your preoperative education? |
To investigate usability of virtual reality system, we used two survey scales; The System Usability Scale and After-Scenario Questionnaire. The System Usability Scale (SUS) was developed in 1986 by John Brooke as a "Quick and Dirty" tool for measuring usability[23]. It consists of 10 items, each of which can be answered on a five-point scale from strongly agree to strongly disagree, and is a reliable tool used to evaluate the usability of various products and services (Table 4).
| System usability scale | |||||
| Strongly disagree (1) | Disagree (2) | Neutral (3) | Agree (4) | Strongly agree (5) | |
| I think that I would like to use this system frequently (SUS1) | |||||
| I found the system unnecessarily complex (SUS2) | |||||
| I thought the system was easy to use (SUS3) | |||||
| I think that I would need the support of a technical person to be able to use this system (SUS4) | |||||
| I found the various functions in this system were well integrated (SUS5) | |||||
| I thought there was too much inconsistency in this system (SUS6) | |||||
| I would imagine that most people would learn to use this system very quickly (SUS7) | |||||
| I found the system very cumbersome to use (SUS8) | |||||
| I felt very confident using the system (SUS9) | |||||
| I needed to learn a lot of things before I could get going with this system (SUS10) | |||||
Due to its effectiveness and ease of use—just three questions—the After-Scenario Questionnaire (ASQ)[24], a usability survey created in 1995 by J.R. Lewis, is widely in use today (Table 5).
| After-Scenario Questionnaire | |||||||
| Strongly disagree (1) | (2) | (3) | (4) | (5) | (6) | Strongly agree (7) | |
| I am satisfied with the ease of completing the task in this scenario (ASQ1) | |||||||
| I am satisfied with the amount of time it took to complete the task in this scenario (ASQ2) | |||||||
| I am satisfied with the support information (on-line help, messages, documentation) when completing the task (ASQ3) | |||||||
To measure burnout, we used the Maslach Burnout Inventory. The Maslach Burnout Inventory (MBI) is a widely used and rigorously validated psychometric instrument developed by Maslach et al[25] to assess and quantify burnout among healthcare professionals, including nurses. Comprising three distinct subscales—emotional exhaustion, depersonalization, and personal accomplishment—the MBI provides a comprehensive assessment of the multidimensional nature of burnout (Table 6).
| Questions | Never | Rarely | Sometimes | Frequently | Always |
| I Emotional Exhaustion | |||||
| I feel emotionally drained from my work | 1 | 2 | 3 | 4 | 5 |
| I feel used up at the end of the workday | 1 | 2 | 3 | 4 | 5 |
| I feel fatigued when I get up in the morning and have to face another day on the job | 1 | 2 | 3 | 4 | 5 |
| Working with people all day is really a strain for me | 1 | 2 | 3 | 4 | 5 |
| I feel burned out from my work | 1 | 2 | 3 | 4 | 5 |
| I feel frustrated by my job | 1 | 2 | 3 | 4 | 5 |
| I feel I’m working too hard on my job | 1 | 2 | 3 | 4 | 5 |
| Working with people directly puts too much stress on me | 1 | 2 | 3 | 4 | 5 |
| I feel like I’m at the end of my rope | 1 | 2 | 3 | 4 | 5 |
| II Personal Accomplishment | |||||
| I can easily understand how my recipients feel about things | 1 | 2 | 3 | 4 | 5 |
| I deal very effectively with the problems of my recipients | 1 | 2 | 3 | 4 | 5 |
| I feel I’m positively influencing other people’s lives through my work | 1 | 2 | 3 | 4 | 5 |
| I feel very energetic | 1 | 2 | 3 | 4 | 5 |
| I can easily create a relaxed atmosphere with my recipients | 1 | 2 | 3 | 4 | 5 |
| I feel exhilarated after working closely with my recipients | 1 | 2 | 3 | 4 | 5 |
| I have accomplished many worthwhile things in this job | 1 | 2 | 3 | 4 | 5 |
| In my work, I deal with emotional problems very calmly | 1 | 2 | 3 | 4 | 5 |
| III Depersonalization | |||||
| I feel I treat some recipients as if they were impersonal ‘objects’ | 1 | 2 | 3 | 4 | 5 |
| I’ve become more callous toward people since I took this job | 1 | 2 | 3 | 4 | 5 |
| I worry that this job is hardening me emotionally | 1 | 2 | 3 | 4 | 5 |
| I don’t really care what happens to some recipients | 1 | 2 | 3 | 4 | 5 |
| I feel recipients blame me for some of their problems | 1 | 2 | 3 | 4 | 5 |
A paired t-test was used to statistically compare the satisfaction before and after using VR by converting the Likert scale for each item in the satisfaction survey into a score.
After the survey of the nurses who performed the intervention for the control and experimental groups, the scores for each item of the SUS and the total score were calculated and compared using paired-t test. ASQ scores were also statistically compared in the same manner.
MBI scores were also calculated and compared statistically using a paired t test. Reverse-coded survey items were handled and statistically analyzed appropriately.
All analyses were conducted using Statistical Package for Social Science software (version 26.0, IBM).
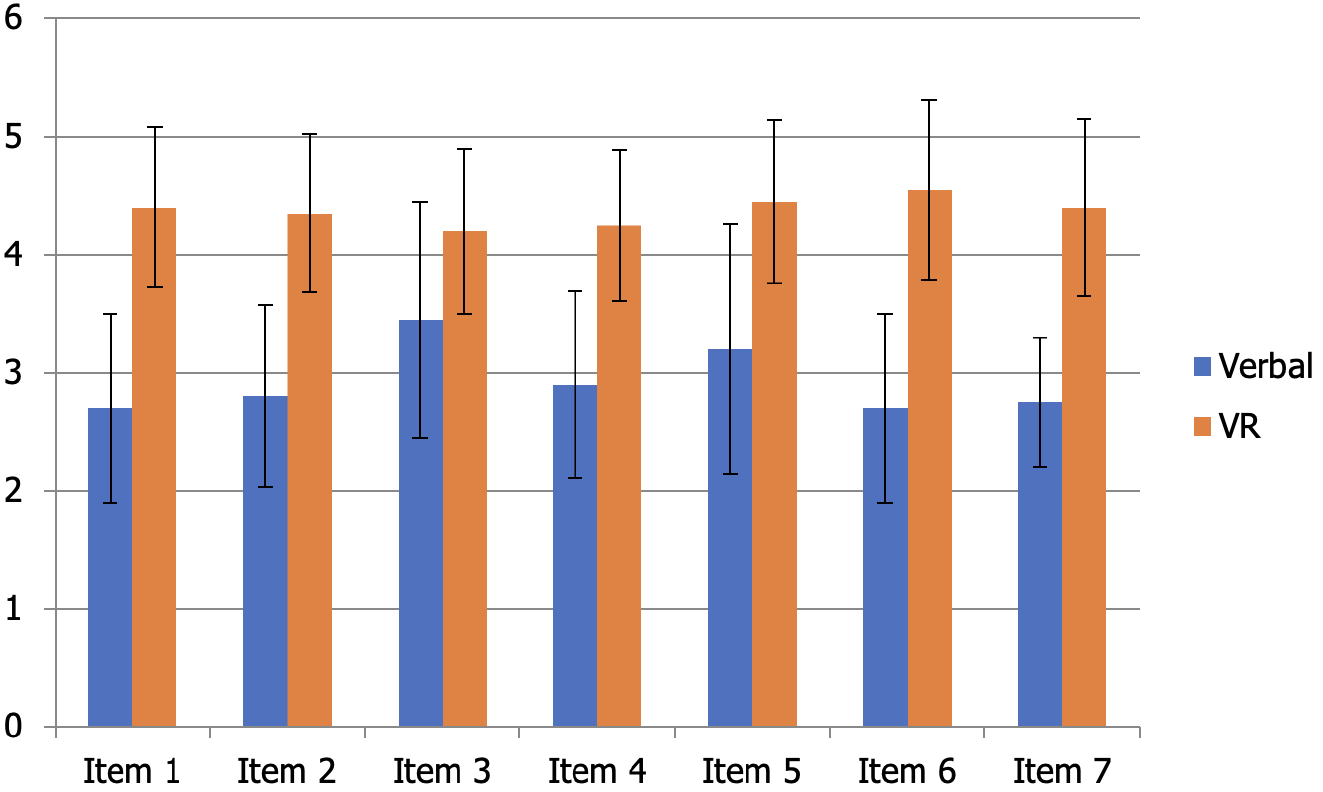
The average overall score in the satisfaction survey taken after giving the control group traditional verbal education was 20.50 ± 1.76 points. In addition, the experimental group received preoperative patient education through virtual reality, and a satisfaction survey was conducted. The average overall score was 30.60 ± 2.37. With a paired t-test P value of less than 0.05, the experimental group showed a statistically higher satisfaction than the control group (Table 7). The experimental group reported significantly higher satisfaction than the control group across all seven survey items when comparing each item (Table 8). Bar plots with error bars diagrams are shown in Figure 4.
| Item | Score | mean ± SD | t | P value (n = 20) | |||||
| 1 | 2 | 3 | 4 | 5 | |||||
| After verbal education | 1 | 9 (45.0) | 9 (45.0) | 1 (5.0) | 1 (5.0) | 20.50 ± 1.76 | 14.44 | < 0.001 | |
| 2 | 7 (35.0) | 11 (55.0) | 1 (5.0) | 1 (5.0) | |||||
| 3 | 3 (15.0) | 9 (45.0) | 4 (20.0) | 4 (20.0) | |||||
| 4 | 7 (35.0) | 8 (40.0) | 5 (25.0) | ||||||
| 5 | 6 (30.0) | 7 (35.0) | 4 (20.0) | 3 (15.0) | |||||
| 6 | 9 (45.0) | 9 (45.0) | 1 (5.0) | 1 (5.0) | |||||
| 7 | 6 (30.0) | 13 (65.0) | 1 (5.0) | ||||||
| After VR education | 1 | 2 (10.0) | 8 (40.0) | 10 (50.0) | 30.60 ± 2.37 | ||||
| 2 | 2 (10.0) | 9 (45.0) | 9 (45.0) | ||||||
| 3 | 3 (15.0) | 10 (50.0) | 7 (35.0) | ||||||
| 4 | 2 (10.0) | 11 (55.0) | 7 (35.0) | ||||||
| 5 | 2 (10.0) | 7 (35.0) | 11 (55.0) | ||||||
| 6 | 3 (15.0) | 3 (15.0) | 14 (70.0) | ||||||
| 7 | 3 (15.0) | 6 (30.0) | 11 (55.0) | ||||||
| Number | mean ± SD | t | P value | ||
| Item 1 | Verbal education | 20 | 2.70 ± 0.80 | 8.23 | < 0.001 |
| VR education | 20 | 4.40 ± 0.68 | |||
| Item 2 | Verbal education | 20 | 2.80 ± 0.77 | 6.31 | < 0.001 |
| VR education | 20 | 4.35 ± 0.67 | |||
| Item 3 | Verbal education | 20 | 3.45 ± 1.00 | 3.00 | 0.003 |
| VR education | 20 | 4.20 ± 0.70 | |||
| Item 4 | Verbal education | 20 | 2.90 ± 0.79 | 5.81 | < 0.001 |
| VR education | 20 | 4.25 ± 0.64 | |||
| Item 5 | Verbal education | 20 | 3.20 ± 1.06 | 4.19 | < 0.001 |
| VR education | 20 | 4.45 ± 0.69 | |||
| Item 6 | Verbal education | 20 | 2.70 ± 0.80 | 7.59 | < 0.001 |
| VR education | 20 | 4.55 ± 0.76 | |||
| Item 7 | Verbal education | 20 | 2.75 ± 0.55 | 7.47 | < 0.001 |
| VR education | 20 | 4.40 ± 0.75 |
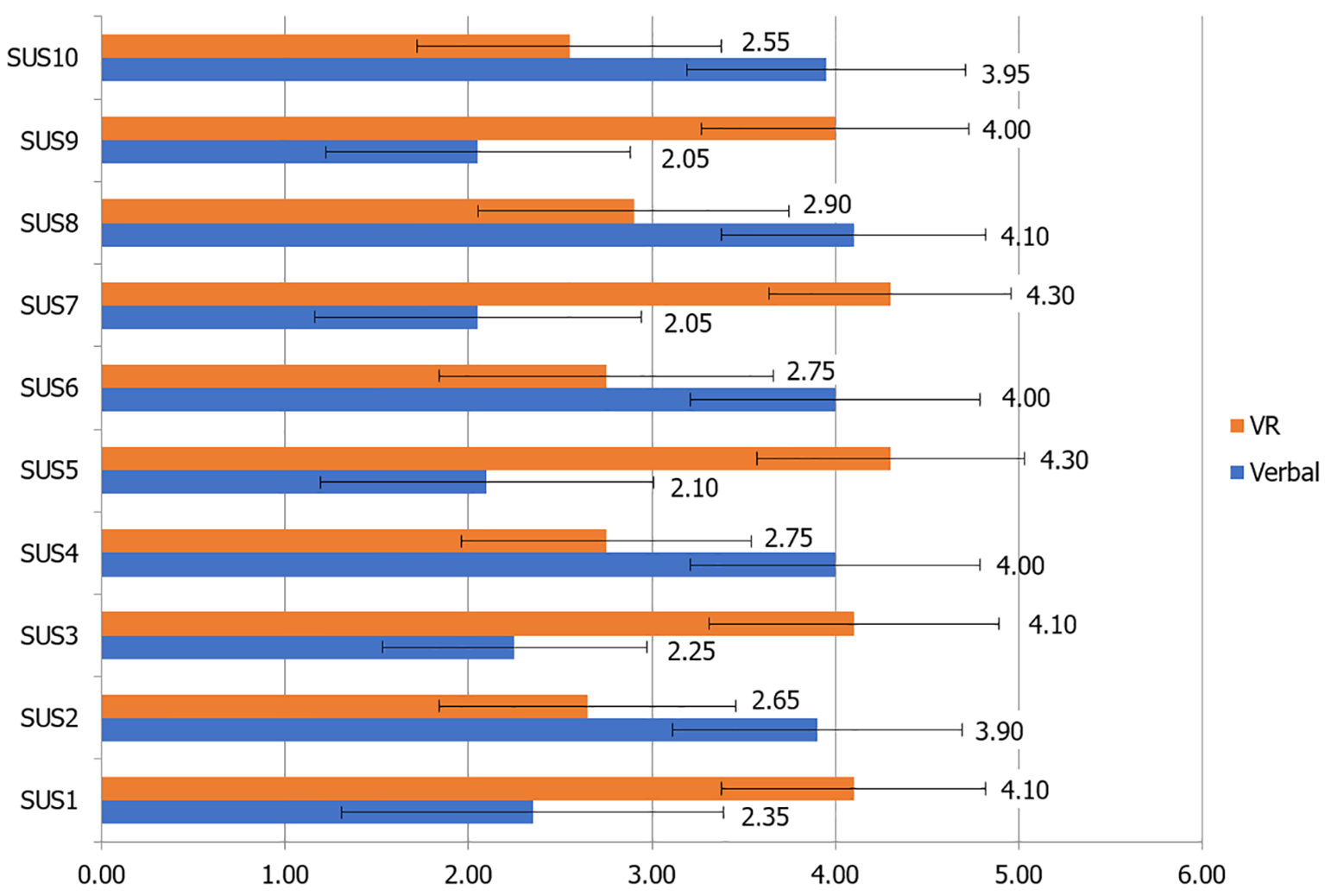
Based on the results of the SUS survey, the traditional paper-based method showed statistically significant results for the items "System too complex," "Need of post-support help," "Too much inconsistent," "Cumbersome to use," and "Need of pre-learn training." However, all 20 nurses in the study demonstrated statistically significant superior results for the VR-based patient education system for the items "It will be used frequently," "Easy to use," "Well integrated," "Learned very quickly," and "Confident to use." The results are shown in Table 9 and Figure 5. Although the total score was statistically significantly higher for the VR-enabled system compared to the traditional system (68.00 ± 5.42), this is only the average system usability scale found in other studies[26].
| Variables | Verbal education, mean ± SD | VR education, mean ± SD | t | P value |
| SUS1 | 2.35 ± 1.04 | 4.10 ± 0.72 | -7.68 | < 0.001 |
| SUS2 | 3.90 ± 0.79 | 2.65 ± 0.81 | 4.80 | < 0.001 |
| SUS3 | 2.25 ± 0.72 | 4.10 ± 0.79 | -7.00 | < 0.001 |
| SUS4 | 4.00 ± 0.79 | 2.75 ± 0.79 | 4.63 | < 0.001 |
| SUS5 | 2.10 ± 0.91 | 4.30 ± 0.73 | -7.03 | < 0.001 |
| SUS6 | 4.00 ± 0.79 | 2.75 ± 0.91 | 5.22 | < 0.001 |
| SUS7 | 2.05 ± 0.89 | 4.30 ± 0.66 | -8.64 | < 0.001 |
| SUS8 | 4.10 ± 0.72 | 2.90 ± 0.85 | 4.33 | < 0.001 |
| SUS9 | 2.05 ± 0.83 | 4.00 ± 0.73 | -7.06 | < 0.001 |
| SUS10 | 3.95 ± 0.76 | 2.55 ± 0.83 | 5.98 | < 0.001 |
| Score of SUS | 27.13 ± 8.82 | 68.00 ± 5.42 | -16.79 | < 0.001 |
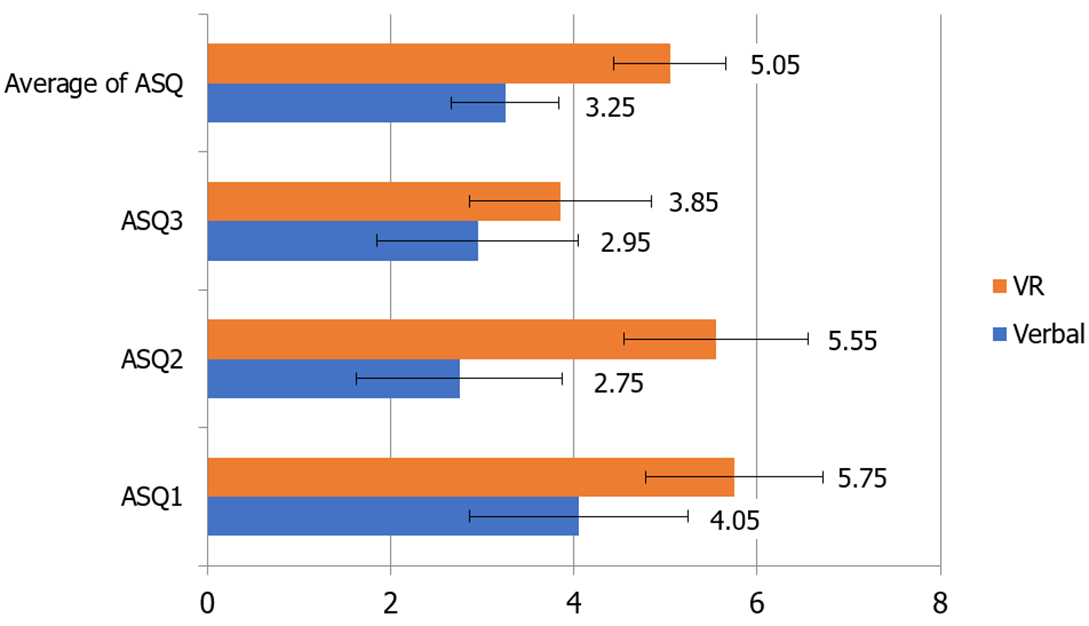
The ASQ survey also showed that the usability of the VR system was significantly higher than the traditional paper-based system. The results are shown in Table 10 and Figure 6.
| Variables | Verbal education, mean ± SD | VR education, mean ± SD | t | P value |
| ASQ1 | 4.05 ± 1.19 | 5.75 ± 0.97 | -5.23 | < 0.001 |
| ASQ2 | 2.75 ± 1.12 | 5.55 ± 1.00 | -11.33 | < 0.001 |
| ASQ3 | 2.95 ± 1.10 | 3.85 ± 0.99 | -4.72 | < 0.001 |
| Average of ASQ | 3.25 ± 0.59 | 5.05 ± 0.61 | -10.59 | < 0.001 |
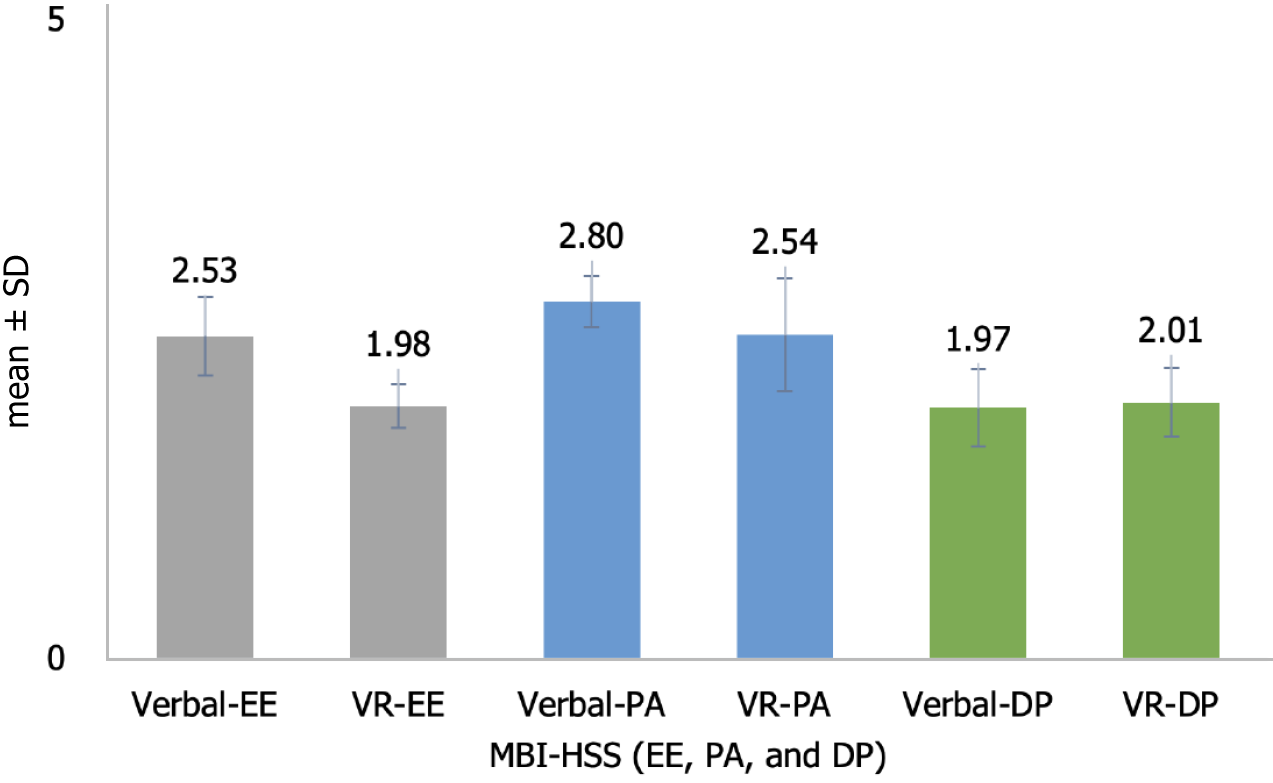
Among the three subscales of the MBI (emotional exhaustion, depersonalization, and personal accomplishment), emotional exhaustion and personal accomplishment improved statistically significantly from 2.53 ± 0.31 to 1.98 ± 0.17 and 2.80 ± 0.20 to 2.54 ± 0.44, respectively. However, Depersonalization increased from 1.97 ± 0.30 to 2.01 ± 0.27, which was not statistically significant. The results are shown in Table 11 and Figure 7.
| Variables | Verbal education, mean ± SD | VR education, mean ± SD | t | P value |
| Emotional exhaustion | 2.53 ± 0.31 | 1.98 ± 0.17 | 6.77 | < 0.001 |
| Personal accomplishment | 2.80 ± 0.20 | 2.54 ± 0.44 | 2.28 | 0.034 |
| Depersonalization | 1.97 ± 0.30 | 2.01 ± 0.27 | -0.54 | 0.599 |
This study demonstrates the effectiveness of preoperative patient education using appropriate technology for new nurses. For new nurses, the use of VR technology proved to be superior to the traditional paper-based method in terms of satisfaction, usability and wellness. However, this does not mean that VR is the tool of choice for preoperative patient education. Although the VR method scores higher on the System Usability Scale than the traditional paper-based method, it is only average at 68 points[26]. The System Usability Scale is not a diagnostic method, so a low System Usability Scale means that we need to further identify and improve the problem.
VR has been used in many healthcare fields. It has been used to train medical students[3], for preoperative planning and simulation by surgeons[27,28], and for rehabilitation therapy[29] and psychotherapy[30]. There are also studies showing the benefits of using VR to educate patients before surgery[7]. However, there is a lack of study on how beneficial the use of suitable technology is in terms of usability for healthcare professionals (especially for new nurses who are new to the job).
The problem with traditional paper-based education is that it must be repeated for each patient and cannot be performed concurrently when there are several patients. Numerous patients can be managed simultaneously if preoperative patient education in virtual reality is performed using a head-mounted display, as the present study. Additionally, the quality of education, which varies according to the healthcare professionals' abilities, has the benefit of remaining consistent. From the perspective of healthcare providers, patients may receive suitable and easy-to-understand information more readily than through conventional methods, and there may be a positive impact on lowering physical and mental stress.
Because it is simple to use and has high usability for new nurses who are challenging at work, virtual reality technology will assist improve the quality of nursing care. Since preoperative patient education using virtual reality technology is beneficial for patients and usable for medical staff (especially new nurses), it should be actively considered for acceptance and adoption.
The MBI was used in the study to compare traditional methods of patient education with virtual reality technology. The findings provided important insights into the impact of these two methods of instruction on the burnout levels of nurses, as evaluated by the three MBI subscales: Emotional exhaustion, depersonalization, and personal accomplishment. The first important finding was a statistically significant decrease in emotional exhaustion levels. Nurses who provided patient education via virtual reality technology exhibited a decrease in emotional exhaustion, dropping from 2.53 ± 0.31 to 1.98 ± 0.17. This is consistent with other studies that shown the use of VR technology reduces emotional weariness among ENT residents[31]. A decrease in emotional exhaustion is critical because it implies a possible improvement in emotional well-being and resilience in the face of the emotionally demanding nature of nursing. Similarly, the personal accomplishment subscale improved statistically significantly. Scores improved from 2.80 ± 0.20 to 2.54 ± 0.44, indicating an improvement in nurses' sense of accomplishment and efficacy. This advancement suggests that virtual reality methods of education contributed to the nursing staff's sense of professional growth and achievement. Such beneficial changes can be critical in increasing work happiness and lowering burnout, eventually improving not only nurses but also the quality of patient care. The results of the depersonalization subscale, on the other hand, were intriguing. The increase in depersonalization scores from 1.97 ± 0.30 to 2.01 ± 0.27 was not statistically significant. Because of the lack of statistical significance, virtual reality-based education appears to have had little effect on reducing depersonalization. Depersonalization is defined as an unfeeling and impersonal attitude to those who receive one's service, care, treatment, or education. Because there is little face-to-face interaction with the patient, the use of VR is not regarded to be a major improvement over the traditional method of nurses interacting and explaining to patients in person. It is necessary to investigate more why depersonalization was mostly unaffected and whether further interventions or modifications to methods of education are required to address this component of burnout.
The limitations of this study are obvious. These are as follows:
Patients with visual impairments or claustrophobia may find it challenging to understand the information provided in virtual reality. This potentially leads to biased satisfaction and usability ratings that do not accurately reflect the general patient population.
While the System Usability Scale and the After-Scenario Questionnaire are time-tested, valid, and reliable tools, they are not diagnostic tools in and of themselves, necessitating additional inquiry into the actual causes for low scores owing to a lack of context in the results.
The traditional paper-based method may be more intuitive to use than the VR one for experienced nurses as compared to younger, more familiar with technology new nurses. This difference could skew the results.
It is expensive to acquire equipment and provide VR content appropriate for each hospital environment. This financial barrier could limit the widespread adoption of VR, affecting the generalizability of the study findings to other settings that may not have the resources to implement such technology.
Even healthcare providers who have previously explained this need time to get trained on how to use the equipment and contents. This could introduce variability in how effectively VR is implemented across different users, potentially impacting the consistency and reliability of the study’s findings.
If the VR content needs to be changed owing to a change in the situation in the hospital, additional costs for reproducing the contents may be incurred. This limitation may affect the long-term feasibility and sustainability of VR as a patient education tool, influencing the study's implications for future practice.
The usability survey of a small number of healthcare providers (n = 20) was assessed using a subjective questionnaire; however, it would be preferable if actual stress reduction could be demonstrated through more objective indications.
This study provides a valuable reference for future research regarding the possible advantages and drawbacks of employing VR technology in a preoperative environment. In addition, the study provides valuable insights into the impact of patient education using VR technology on nurse burnout. Despite above limitations, the study demonstrates that VR technology is significantly more usable than traditional paper-based methods for healthcare providers (especially for new nurses) working in plastic surgery wards. In addition, it demonstrates the usefulness of virtual reality-based patient education in lowering emotional exhaustion and increasing personal accomplishment of nurses. However, the persistence of depersonalization in lack of a statistically significant changes implies that a more nuanced evaluation of educational content and methods to address this particular aspect of burnout among nurses is required. As this study has the limitation of being a subjective survey, it is crucial to assess qualitative changes to confirm the efficacy to the quality of nursing care, such as the change in the number of questions or the amount of time required for a preoperative patient education when the healthcare provider provides preoperative patient education using VR. Additionally, further research is required to confirm the impact of objective vital signs of healthcare providers, such as stress signs or heart rate variability, when the healthcare provider is offering the preoperative patient education.
| 1. | Li L, Yu F, Shi D, Shi J, Tian Z, Yang J, Wang X, Jiang Q. Application of virtual reality technology in clinical medicine. Am J Transl Res. 2017;9:3867-3880. [PubMed] |
| 2. | de Vries FS, van Dongen RTM, Bertens D. Pain education and pain management skills in virtual reality in the treatment of chronic low back pain: A multiple baseline single-case experimental design. Behav Res Ther. 2023;162:104257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 3. | Pottle J. Virtual reality and the transformation of medical education. Future Healthc J. 2019;6:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 310] [Article Influence: 51.7] [Reference Citation Analysis (0)] |
| 4. | Ahmadpour N, Randall H, Choksi H, Gao A, Vaughan C, Poronnik P. Virtual Reality interventions for acute and chronic pain management. Int J Biochem Cell Biol. 2019;114:105568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 134] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 5. | Howard MC. A meta-analysis and systematic literature review of virtual reality rehabilitation programs. CHB. 2017;70:317-327. [RCA] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 162] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 6. | Bekelis K, Calnan D, Simmons N, MacKenzie TA, Kakoulides G. Effect of an Immersive Preoperative Virtual Reality Experience on Patient Reported Outcomes: A Randomized Controlled Trial. Ann Surg. 2017;265:1068-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 122] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 7. | Kwon H, Lee J, Park YS, Oh SH, Kim J. Effects of preoperative education using virtual reality on preoperative anxiety and information desire: a randomized clinical trial. J Clin Monit Comput. 2023;37:1401-1407. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (2)] |
| 8. | Shepherd T, Trinder M, Theophilus M. Does virtual reality in the perioperative setting for patient education improve understanding? A scoping review. Surg Pract Sci. 2022;100101. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Bazi KN. Effective Training for Novice Nurses Transition to the Perioperative Role: An Integrative Literature Review. 2019. |
| 10. | Fitzpatrick E, Hyde A. Nurse-related factors in the delivery of preoperative patient education. J Clin Nurs. 2006;15:671-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Wu TY, Fox DP, Stokes C, Adam C. Work-related stress and intention to quit in newly graduated nurses. Nurse Educ Today. 2012;32:669-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 12. | Kim MH, Mazenga AC, Simon K, Yu X, Ahmed S, Nyasulu P, Kazembe PN, Ngoma S, Abrams EJ. Burnout and self-reported suboptimal patient care amongst health care workers providing HIV care in Malawi. PLoS One. 2018;13:e0192983. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 13. | Chandawarkar A, Chaparro JD. Burnout in clinicians. Curr Probl Pediatr Adolesc Health Care. 2021;51:101104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Bondagji D, Fakeerh M, Alwafi H, Khan AA. The Effects of Long Working Hours on Mental Health Among Resident Physicians in Saudi Arabia. Psychol Res Behav Manag. 2022;15:1545-1557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 15. | Zarei S, Fooladvand K. Mediating effect of sleep disturbance and rumination on work-related burnout of nurses treating patients with coronavirus disease. BMC Psychol. 2022;10:197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 16. | von Känel R, Princip M, Holzgang SA, Fuchs WJ, van Nuffel M, Pazhenkottil AP, Spiller TR. Relationship between job burnout and somatic diseases: a network analysis. Sci Rep. 2020;10:18438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Hamaideh SH. Burnout, social support, and job satisfaction among Jordanian mental health nurses. Issues Ment Health Nurs. 2011;32:234-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987-1993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3142] [Cited by in RCA: 3007] [Article Influence: 130.7] [Reference Citation Analysis (0)] |
| 19. | Olfson M, Cosgrove CM, Wall MM, Blanco C. Suicide Risks of Health Care Workers in the US. JAMA. 2023;330:1161-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 41] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 20. | Gold JI, Annick ET, Lane AS, Ho K, Marty RT, Espinoza JC. "Doc McStuffins: Doctor for a Day" Virtual Reality (DocVR) for Pediatric Preoperative Anxiety and Satisfaction: Pediatric Medical Technology Feasibility Study. J Med Internet Res. 2021;23:e25504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Llorens R, Colomer-Font C, Alcañiz M, Noé-Sebastián E. BioTrak virtual reality system: Effectiveness and satisfaction analysis for balance rehabilitation in patients with brain injury. Neurología. 2013;28:268-275. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Benner P. From novice to expert. Menlo Park. 1984;84:10-1097. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2192] [Cited by in RCA: 1861] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 23. | Brooke J. SUS: A “quick and dirty’ usability Scale. 1st Edition, Usability evaluation in industry. 1996; 189: 189-194. |
| 24. | Lewis JR. IBM computer usability satisfaction questionnaires: Psychometric evaluation and instructions for use. Int J Hum-Comput Int. 1995;7:57-78. [DOI] [Full Text] |
| 25. | Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory: Scarecrow Education; 1997. |
| 26. | Melnick ER, Dyrbye LN, Sinsky CA, Trockel M, West CP, Nedelec L, Tutty MA, Shanafelt T. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among US Physicians. Mayo Clin Proc. 2020;95:476-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 219] [Article Influence: 43.8] [Reference Citation Analysis (0)] |
| 27. | Ulbrich M, Van den Bosch V, Bönsch A, Gruber LJ, Ooms M, Melchior C, Motmaen I, Wilpert C, Rashad A, Kuhlen TW, Hölzle F, Puladi B. Advantages of a Training Course for Surgical Planning in Virtual Reality for Oral and Maxillofacial Surgery: Crossover Study. JMIR Serious Games. 2023;11:e40541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 28. | Freidin D, Singolda R, Tejman-Yarden S, Parmat I, Liran A, Ofir H, Saukhat O, Haik J, Barnea Y, Tessone A. Using Virtual Reality for Deep Inferior Epigastric Perforator Flap Preoperative Planning. Plast Reconstr Surg Glob Open. 2023;11:e4773. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 29. | Phelan I, Carrion-Plaza A, Furness PJ, Dimitri P. Home-based immersive virtual reality physical rehabilitation in paediatric patients for upper limb motor impairment: a feasibility study. Virtual Real. 2023;27:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Riches S, Jeyarajaguru P, Taylor L, Fialho C, Little J, Ahmed L, O'Brien A, van Driel C, Veling W, Valmaggia L. Virtual reality relaxation for people with mental health conditions: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2023;58:989-1007. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 31. | Weitzman RE, Wong K, Worrall DM, Park C, McKee S, Tufts RE, Teng MS, Iloreta AM. Incorporating Virtual Reality to Improve Otolaryngology Resident Wellness: One Institution's Experience. Laryngoscope. 2021;131:1972-1976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |