Published online Oct 6, 2024. doi: 10.12998/wjcc.v12.i28.6180
Revised: June 24, 2024
Accepted: July 23, 2024
Published online: October 6, 2024
Processing time: 109 Days and 4.5 Hours
Esophageal stricture is one of the complications after esophageal varices sclerotherapy injection (ESI), and the incidence rate is between 2%-10%.
To explore the efficacy of self-expanding metal stent (SEMS) for the stricture after endoscopic injection with cyanoacrylate (CYA) and sclerotherapy for esophageal varices.
We retrospectively analyzed the efficacy of SEMS to improve the stricture after endoscopic injection with CYA and sclerotherapy for esophageal varices in 4 patients from February 2023 to June 2023.
The strictures were improved in four patients after stenting. The stent was removed after two weeks because of chest pain with embedding into esophageal mucosa in one patient. The stent was removed after one month, however, the stent was reinserted because of the strictures happening again in two patients. The stent was removed after three months, however, the stent was reinserted because of the strictures happening again in one patient. The stent embedded into esophageal mucosa in three patients. There were 3 patients suffered reflux esophagitis, and the acid reflux was relieved by taking hydrotalcite. There was no other complication of esophageal perforation, bleeding from varices or infection.
SEMS may relieve the stricture which happened after endoscopic injection with CYA and sclerotherapy for esophageal varices. However, when we should remove the stent still needs to be explored.
Core Tip: Esophageal stricture is one of the complications after esophageal varices sclerotherapy injection (ESI), and the incidence rate is between 2%-10%. Esophageal stricture is related to local inflammation, ulceration, and fibrosis caused by multiple ESI. However, there is no report about esophageal stricture after endoscopic injection with cyanoacrylate (CYA) and sclerotherapy for esophageal varices. We want to explore the efficacy of the self-expanding metal stent for the stricture after endoscopic injection with CYA and sclerotherapy for esophageal varices in this article.
- Citation: Zhang FL, Xu J, Jiang YH, Zhu YD, Shi Y, Li X, Wang H, Huang CJ, Zhou CH, Zhu Q, Chen JW. Self-expanding metal stent for relieving the stricture after endoscopic injection for esophageal varices. World J Clin Cases 2024; 12(28): 6180-6186
- URL: https://www.wjgnet.com/2307-8960/full/v12/i28/6180.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i28.6180
Esophageal stricture is one of the complication after esophageal varices sclerotherapy injection (ESI), and the incidence rate is between 2%-10%[1]. Esophageal stricture is related to local inflammation, ulceration, and fibrosis caused by multiple ESI[2]. However, there is no report about esophageal stricture after endoscopic injection with cyanoacrylate (CYA) and sclerotherapy for esophageal varices. We want to explore the efficacy of the self-expanding metal stent (SEMS) for the stricture after endoscopic injection with CYA and sclerotherapy for esophageal varices in this article.
We retrospectively analyzed the efficacy of SEMS to improve the stricture after endoscopic injection with CYA and sclerotherapy for esophageal varices in 4 patients from February 2023 to June 2023.
Severity of dysphagia was assessed by Stooler grade[3]: Grade 0: Can eat normally; grade I: Can’t swallow some solid food; grade II: Can only swallow half liquid food; grade III: Can only swallow liquid food; grade IV: Can’t swallow liquid food. The effect was evaluated as follows[4]: Markedly effective: Lumen diameter > 1.2 cm, grade 0 dysphagia, and no recurrence during follow-up; effective: Lumen diameter between 0.6 and 1.1 cm, grade I dysphagia, and no aggravation during follow-up; ineffective: No change in lumen diameter, either no alleviation of dysphagia or aggravation of it. Criteria for the recurrence of the stricture: (1) The severity of the stricture deteriorated once more, reaching grade II-IV; and (2) Standard gastroscope’s body is incapable of traversing the esophagus without encountering resistance.
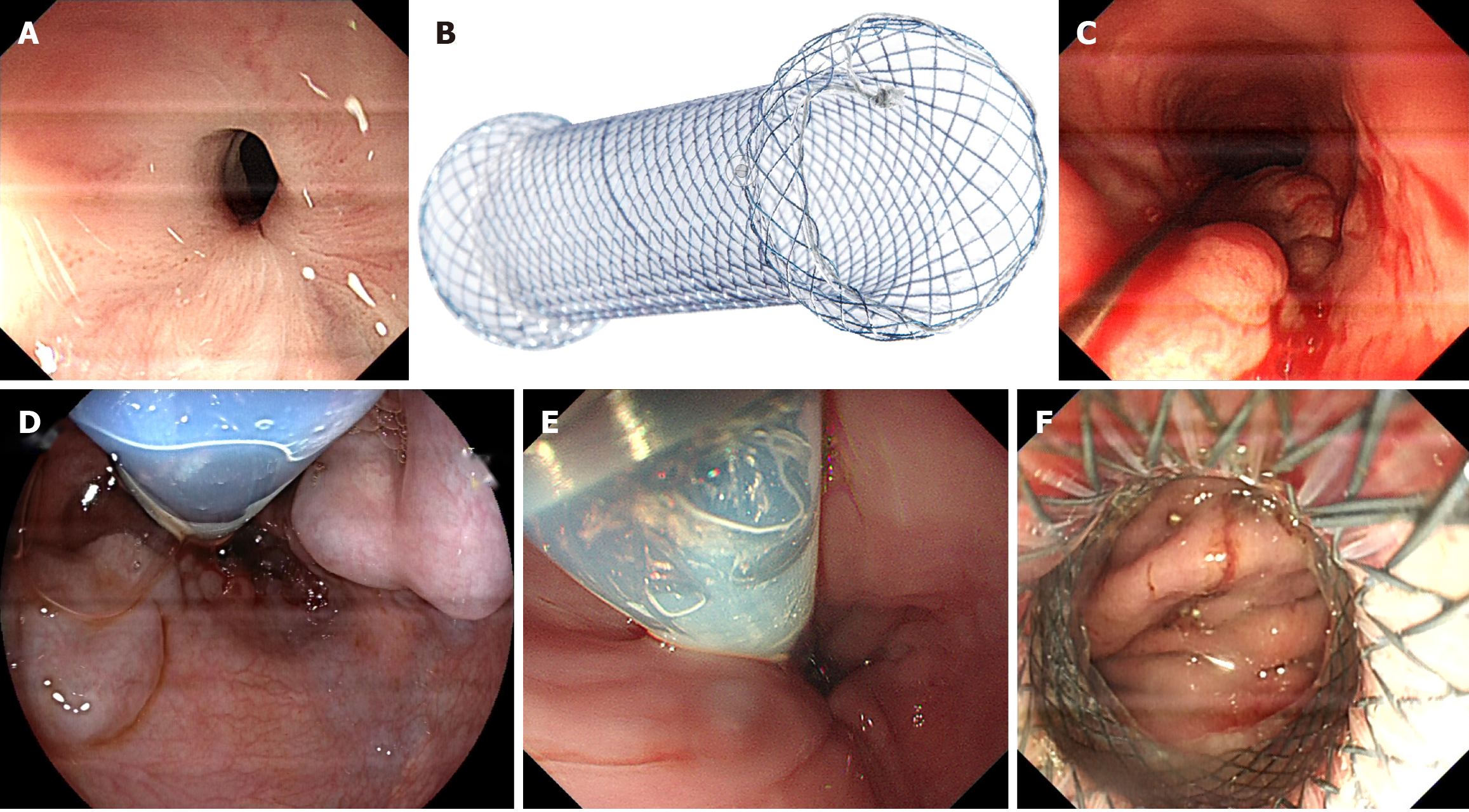
Before endoscopy the patients should been fasting for 12 hours, monitored blood pressure and prepared oxygen and emergency medicines. We should use an endoscope (EG-760R, diameter 9.3 mm, FUJIFILM, Japan) to observe the retention in the esophageal cavity, and we should be alert to residual varices. If a large amount of liquid and/or solid were blocked by stenosis, residues must be removed to expose the stenosis (Figure 1A). When the esophageal stricture exposed entirely, we performed the balloon dilatation (18 mm × 55 mm, Nanjing Minimally Invasive Medical Technology co., Ltd.) to improve stenosis until the endoscope body passes through the stenosis smoothly. If the bleeding was obvious after dilatation, we used the argon plasma coagulation to improve the bleeding. We inserted a covered SEMS (20 mm × 60 mm; Nanjing Minimally Invasive Medical Technology co., Ltd.) (Figure 1B) across the stenosis by a hard wire guarding (Figure 1C). We should be aware of the residual varices, when the SEMS was placed (Figure 1D). On the one hand, the anal side of stent should be passed over cardia (Figure 1E), on the other hand, the oral side of stent should be above the stricture (Figure 1F). And then, the endoscope should be passed through the stent into the stomach to confirm the posi
Gender: There were 3 males and 1 female. Age: The average age was 47 years. Etiology: There were 3 patients with hepatitis B, 1 patient with alcohol. Child-Pugh: There were 3 patients of grade A, 1 patient of grade B. Hepatocellular carcinoma (HCC): There was 1 patient with HCC. Portal thrombosis: There were 2 patients with portal thrombosis. Hypertension and/or diabetes: There was no patient with hypertension or diabetes. Splenectomy: There was 1 patient suffered splenectomy. The time of endoscopic injection: There were 2 to 4 times of endoscopic injection with CYA and sclerotherapy for esophageal varices. CYA: The average amount of CYA was 2.25 mL. Sclerotherapy: The average amount of lauromacrogol was 56.25 mL (Table 1).
| Case | 1 | 2 | 3 | 4 |
| Sex | Male | Female | Male | Male |
| Age (year) | 39 | 53 | 59 | 39 |
| Etiology | Hepatitis B | Hepatitis B | Alcohol | Hepatitis B |
| Child-Pugh | A | A | B | A |
| Portal thrombosis | Positive | Positive | Negative | Negative |
| Hepatocellular carcinoma | Negative | Negative | Positive | Negative |
| Splenectomy | Positive | Negative | Negative | Negative |
| Hypertension/diabetes | Negative | Negative | Negative | Negative |
| EIE (time) | 2 | 3 | 4 | 4 |
| Cyanoacrylate (mL) | 3 | 1 | 3 | 2 |
| Sclerotherapy (mL) | 50 | 60 | 60 | 55 |
| Balloon dilation (time) | 2 | 5 | 5 | 1 |
| Local incision (time) | 2 | 3 | 1 | 0 |
| Stooler grade | III | III | III | II |
| Location of stricture (distance from incisor teeth) | 38 cm | 36 cm | 37 cm | 36 cm |
| Length of stricture | 2 cm | 3 cm | 1 cm | 2 cm |
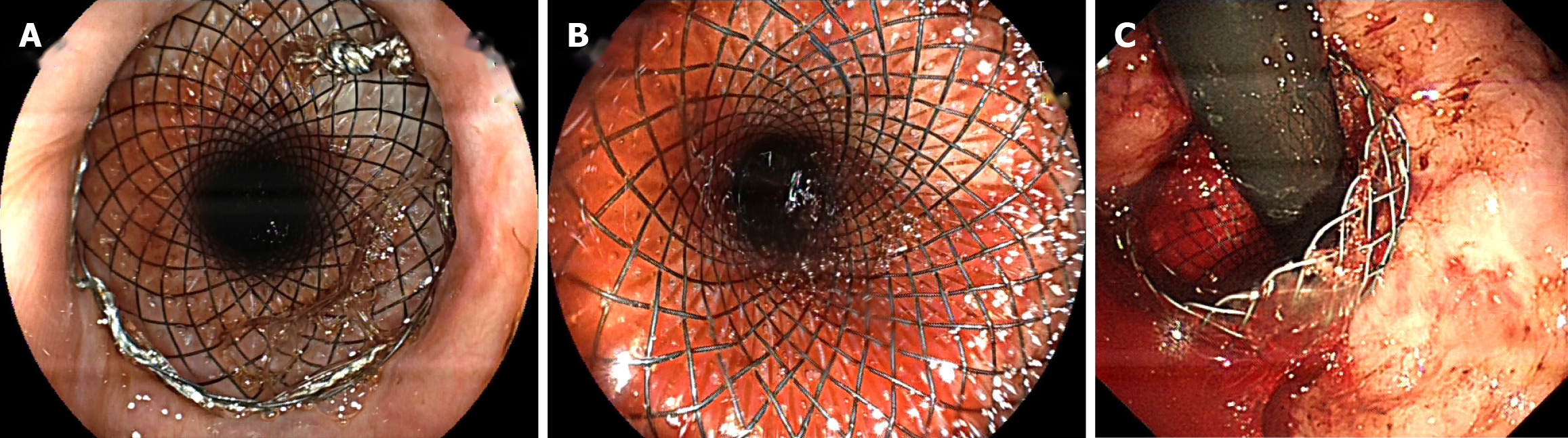
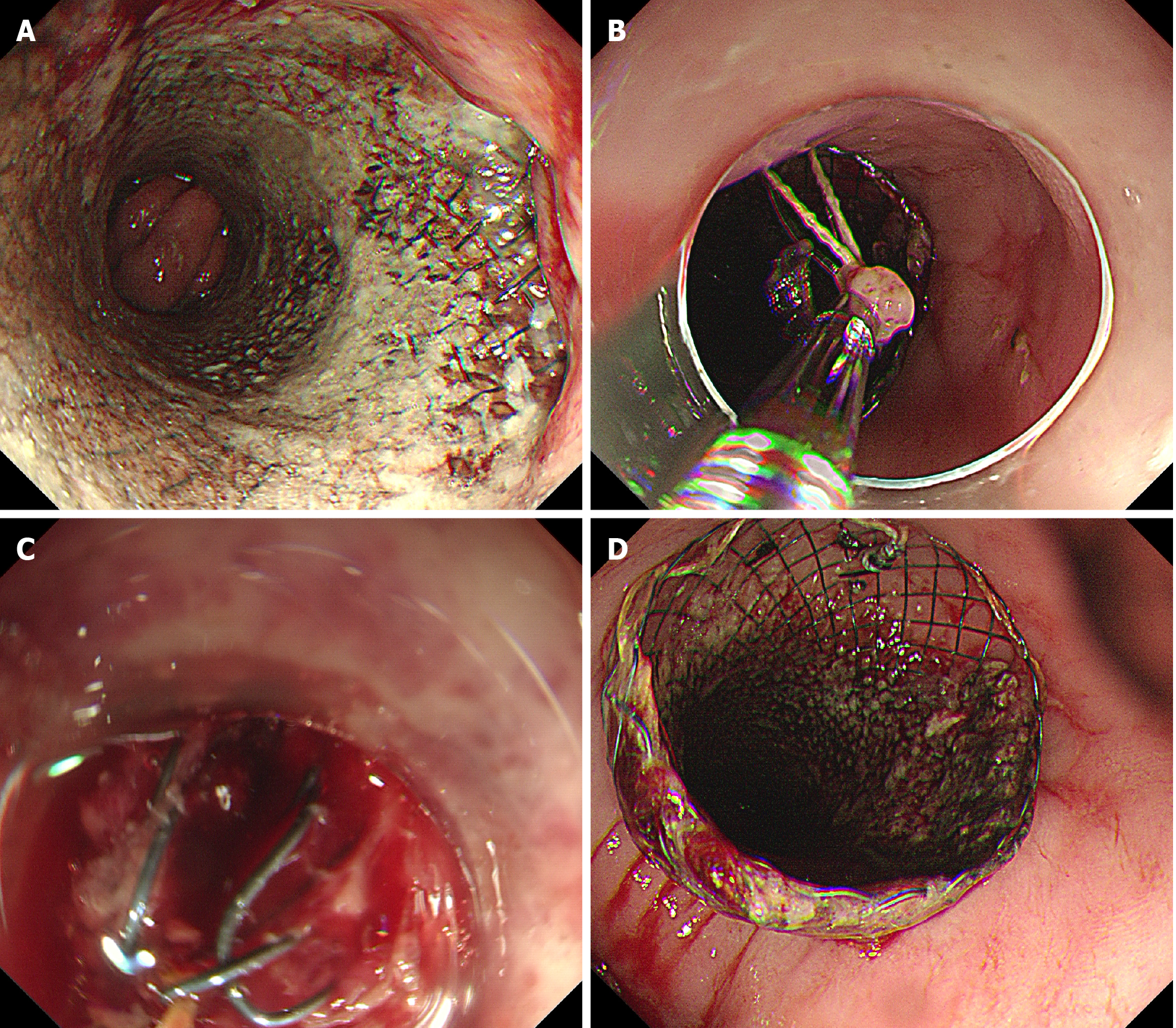
The strictures were improved in four patients after stenting. The stent was removed after two weeks because of chest pain with embedding into esophageal mucosa in one patient. The stent was removed after one month, however, the stent was reinserted because of the stricture happening again in two patients. The stent was removed after three months, however, the stent was reinserted because of the stricture happening again in one patient. The stent embedded into esophageal mucosa in three patients, and we adjusted the stent to relieve chest pain. There were 3 patients suffered reflux eso
| Case | 1 | 2 | 3 | 4 |
| Effectiveness | ME | ME | ME | ME |
| Chest-pain | Negative | Negative | Negative | Positive |
| Reflux esophagitis | Positive | Positive | Positive | Negative |
| Embedding | Positive | Positive | Positive | Negative |
| Migration | Negative | Negative | Negative | Negative |
| Perforation | Negative | Negative | Negative | Negative |
| Infection | Negative | Negative | Negative | Negative |
| Varices bleeding | Negative | Negative | Negative | Negative |
Patients suffering from liver cirrhosis begin bleeding due to burst esophageal varices, facing a 40 percent risk of succumbing to the initial bleeding incident[5]. The primary therapy for esophageal varices[6] was identified as endoscopic sclerotherapy. Lately, the administration of CYA has been consistently effective in treating esophageal varices, ensuring no return of bleeding[7]. Post endoscopic injection of CYA or sclerotherapy, esophageal varices often lead to complications such as esophageal stricture. Dysphagia stands as the primary indicator of esophageal stricture. International guidelines[8] do not reference the conventional therapy for esophageal narrowing post-ESI.
The primary methods for alleviating the benign esophageal stricture involved balloon dilation and localized incision[9,10]. The primary mechanism of balloon dilation is through the balloon’s mechanical tension; conversely, it leads to the tearing of the usual mucosal or muscular layers surrounding the esophagus[11]. A nearby cut must be vigilant for perforation complications, especially when the esophagus’s muscularis propria is severed[12]. Nonetheless, neither balloon dilation nor localized incision succeeded in alleviating the stricture in these four patients prior to the application of SEMS. The European Society of Gastrointestinal Endoscopy advised focusing on esophageal stents for benign esophageal strictures, particularly in cases of persistent or repeated benign strictures, noting that the placement of esophageal stents could be advantageous due to their constant enlargement, potentially resulting in changes to the stricture[13]. Inserting a stent prolongs the narrowing of the esophagus, yet it’s crucial to be vigilant about potential issues like chest discomfort, reflux esophagitis, displacement or detachment, and the presence of tissue-embedded stents[14,15]. In three cases, the stent was implanted into the esophageal mucosa, and the stent was modified to alleviate chest discomfort. Six months post-removal, the stent was reinserted due to repeated stenosis in three patients. Consequently, an extended period of monitoring is required to ascertain when SEME removal will occur, unless chest pain is the reason.
The advantages of SEMS for esophageal stricture after endoscopic injection for varices were as follow: (1) The symptom of dysphagia would relief immediately after placing the stent; (2) The stent could lead to stricture remodeling for convey foods; (3) The complication of perforation or bleeding was few during or after the endoscopic treatment; (4) The stent could cover residual esophageal varices and reduce the rebleed from varices; and (5) The stent could be adjusted, removed or replaced at any time.
However, there are several limitations of SEMS: (1) When the stent is removed, the patient will suffer from an esophageal stricture again, so when the stent has to be removed, other possibilities need to be explored; (2) The stent may become embedded into the esophageal mucosa, so endoscopy should be performed frequently to observe or adjust the stent; (3) If the stent migrates into the stomach, it should be removed immediately through endoscopy; and (4) Because of only four cases in this study, it is difficult to demonstrate the efficacy of SEMS for the stricture.
Stenting may relieve the stenosis which happened after endoscopic injection with CYA and sclerosis for esophageal varices. when we should remove the stent still needs to be explored. However, more cases, multicenter, prospective controlled studies are still needed to support this.
| 1. | de Franchis R, Primignani M. Endoscopic treatments for portal hypertension. Baillieres Clin Gastroenterol. 1997;11:289-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Linghu EQ. [Endoscopic diagnosis and treatment of upper gastrointestinal hemorrhage caused by esophagus-gastric varice]. Zhongguo Xiaohuabing Yv Yingxiangxve Zazhi. 2012;. |
| 3. | Wang F, Zhang D, Zeng J, Chen J. Comparison of endoscopic radial incision and Savary-Gilliard's bougie dilation in efficacy on refractory esophagogastric anastomosis strictures. Ann Palliat Med. 2021;10:10963-10970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices. Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med. 1988;319:983-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 996] [Cited by in RCA: 841] [Article Influence: 22.7] [Reference Citation Analysis (1)] |
| 5. | Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ, Waring JP, Fanelli RD, Wheeler-Harbaugh J; Standards Practice Committe, American Society for Gastrointestinal Endoscopy. The role of endoscopic therapy in the management of variceal hemorrhage. Gastrointest Endosc. 2002;56:618-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Kalista KF, Hanif SA, Nababan SH, Lesmana CRA, Hasan I, Gani R. The Clinical Role of Endoscopic Ultrasound for Management of Bleeding Esophageal Varices in Liver Cirrhosis. Case Rep Gastroenterol. 2022;16:295-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Sami SS, Haboubi HN, Ang Y, Boger P, Bhandari P, de Caestecker J, Griffiths H, Haidry R, Laasch HU, Patel P, Paterson S, Ragunath K, Watson P, Siersema PD, Attwood SE. UK guidelines on oesophageal dilatation in clinical practice. Gut. 2018;67:1000-1023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 8. | Huang J, Liao J, Yang S, Zhang Y, Zhao Y, Gu Y, Hua K, Li S, Xia L, Cai S. Anastomotic stricture indexes for endoscopic balloon dilation after esophageal atresia repair: a single-center study. Dis Esophagus. 2021;34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Kano Y, Kadota T, Inaba A, Sunakawa H, Takashima K, Nakajo K, Murano T, Shinmura K, Yoda Y, Ikematsu H, Akimoto T, Yano T. Efficacy and safety of repeated endoscopic radial incision and cutting procedure for benign esophageal stricture. Endosc Int Open. 2023;11:E230-E236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Zhai YQ, Linghu EQ, Li HK, Qin ZC, Feng XX, Wang XD, Dong H, Meng JY, Wang HB, Zhu J. [A comparative study of endoscopic tunneling and conventional mucosal dissection in the treatment of large superficial tumors of the esophagus]. Nanfang Yike Daxve Xvebao. 2014;34:36-40. [DOI] [Full Text] |
| 11. | Zhang F, Xu J, Zhu Y, Shi Y, Wu B, Wang H, Huang C. Endoscopic ultrasonography guided cutting scar of esophageal stricture after endoscopic injection sclerotherapy. BMC Gastroenterol. 2022;22:343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 12. | Spaander MCW, van der Bogt RD, Baron TH, Albers D, Blero D, de Ceglie A, Conio M, Czakó L, Everett S, Garcia-Pagán JC, Ginès A, Jovani M, Repici A, Rodrigues-Pinto E, Siersema PD, Fuccio L, van Hooft JE. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2021. Endoscopy. 2021;53:751-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 13. | Fugazza A, Lamonaca L, Mercante G, Civilini E, Pradella A, Anderloni A, Repici A. The worst adverse event for an endoscopist after esophageal stent placement: an aortoesophageal fistula. Endoscopy. 2022;54:E44-E45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Singla V, Khare S, Arora A, Kumar A, Sharma P, Bansal N, Anikhindi SA. Use of loop and clips to prevent migration of esophageal stent. Endoscopy. 2021;53:E421-E422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Ou Y, Chen L, Li J, Ye Y, Chen Z, Cai L, Liao J. Endoscopic removal of a migrated esophageal covered self-expandable metal stent: the nylon loop pusher-assisted method. Endoscopy. 2022;54:E744-E745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |