Published online Sep 26, 2024. doi: 10.12998/wjcc.v12.i27.6117
Revised: July 1, 2024
Accepted: July 15, 2024
Published online: September 26, 2024
Processing time: 151 Days and 17.5 Hours
Tuberculous peritonitis (TBP) is a chronic, diffuse inflammation of the peritoneum caused by Mycobacterium tuberculosis. The route of infection can be by direct spread of intraperitoneal tuberculosis (TB) or by hematogenous dissemination. The former is more common, such as intestinal TB, mesenteric lymphatic TB, fa
We present an older male patient with TBP complicated by an abdominal mass. The patient's preoperative symptoms, signs and imaging data suggested a poss
This case report analyses the management of TBP complicated by intraperitoneal tuberculous abscess and highlights the importance of early definitive diagnosis in the hope of improving the clinical management of this type of disease.
Core Tip: We present an older male patient with tuberculous peritonitis (TBP) complicated by an abdominal mass. The patient's preoperative symptoms, signs and imaging data suggested a possible abdominal tumor. After surgical treatment, the patient's primary diagnosis of TBP complicated by an intraperitoneal tuberculous abscess was established by previous medical history, postoperative pathology and positive results of tuberculosis-related laboratory tests. Our aim is to report and analyze the diagnostic and therapeutic course of the disease and to highlight the importance of an early and definitive diagnosis in the hope of improving the clinical diagnosis and management of this type of disease.
- Citation: Liu WP, Ma FZ, Zhao Z, Li ZR, Hu BG, Yang T. Tuberculous peritonitis complicated by an intraperitoneal tuberculous abscess: A case report. World J Clin Cases 2024; 12(27): 6117-6123
- URL: https://www.wjgnet.com/2307-8960/full/v12/i27/6117.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i27.6117
According to World Health Organization, 106 million people will develop tuberculosis (TB) in 2021, and 1.6 million peo
A 72-year-old man was admitted to the Binzhou Medical University Hospital with abdominal pain and discomfort for > 1 month.
About 1 month ago, the patient had abdominal pain without any obvious cause, which was most obvious in the upper abdomen around the umbilicus. The abdominal pain was intermittent and dull, with no obvious radiating pain in the back and waist. The patient had no fever, nausea or vomiting, and no abdominal distension or diarrhea. Since the onset of the disease, the patient was clear and in good spirits, with normal diet, normal sleep, no significant change in body weight, and normal urination and defecation.
The patient had a history of exposure to TB 30 years ago and developed abdominal effusion. The patient had undergone surgery for heart valve disease and had been taking warfarin orally since the surgery.
The patient denied any family history of malignant tumors.
On physical examination, the vital signs were as follows: Body temperature, 36.4 °C; blood pressure, 129 mmHg/66 mmHg; heart rate, 85 beats per minute; respiratory rate, 20 breaths per minute. His abdomen was flat, with no scarring, or gastric or intestinal pattern, no peristaltic wave, normal umbilicus, and no abdominal wall varices. His abdomen was soft, but there was a palpable hard abdominal mass on the right side of the umbilicus, about 6 cm 5 cm in size, with tenderness, poor mobility, and no abdominal compression. The liver was not palpable at the subcostal margin, and the gallbladder and spleen were not palpable. Abdominal mobile turbidity was negative, bowel sounds were normal at 4 beats/minute, and no vascular murmurs were heard in the abdomen.
Erythrocyte count 3.5 1012/L (normal reference range: 4.3 1012/L–5.8 1012/L), hemoglobin 98 g/L (normal reference range: 130 g/L–175 g/L), hematocrit 31% (normal reference range: 40%–50%), lymphocyte percentage 15.4% (normal reference range: 20%–50%), neutrophil percentage 77.9% (normal reference range: 40%–75%), eosinophil percentage 0.3% (normal reference range: 0.4%–8%). The white blood cell count, platelet count, monocyte percentage, and eosinophil percentage were normal.
Total protein 60.50 g/L (normal reference range: 65 g/L–85 g/L), albumin 34.30 g/L (normal reference range: 40 g/L–55 g/L), lipoprotein A 55.05 mg/dL (normal reference range: 0 mg/dL–30 mg/dL), lactate dehydrogenase 305.80 U/L (normal reference range: 120 U/L–250 U/L), α-hydroxybutyrate dehydrogenase 205.70 U/L (normal reference range: 72 U/L–182 U/L), uric acid 183.0 μmol/L (normal reference range: 208 μmol/L–428 μmol/L). Glutamatergic aminotransferase, alanine aminotransferase, globulin, total bilirubin, direct bilirubin, indirect bilirubin, alkaline phosphatase, urea nitrogen, creatinine, and electrolytes were normal. Fibrinogen level was 4.4 g/L (normal reference range: 2 g/L–4 g/L). Prothrombin time, activated partial thromboplastin time, prothrombin time and D-dimer quantification were normal. Carcinoembryonic antigen was negative.
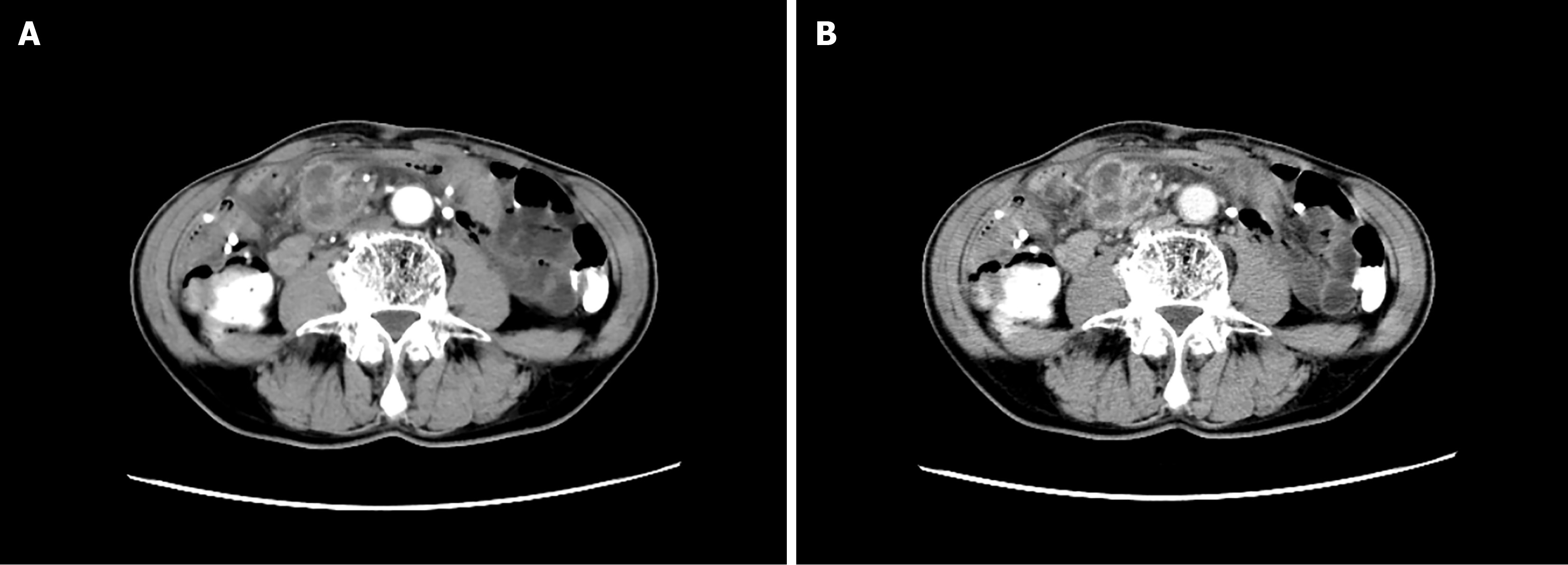
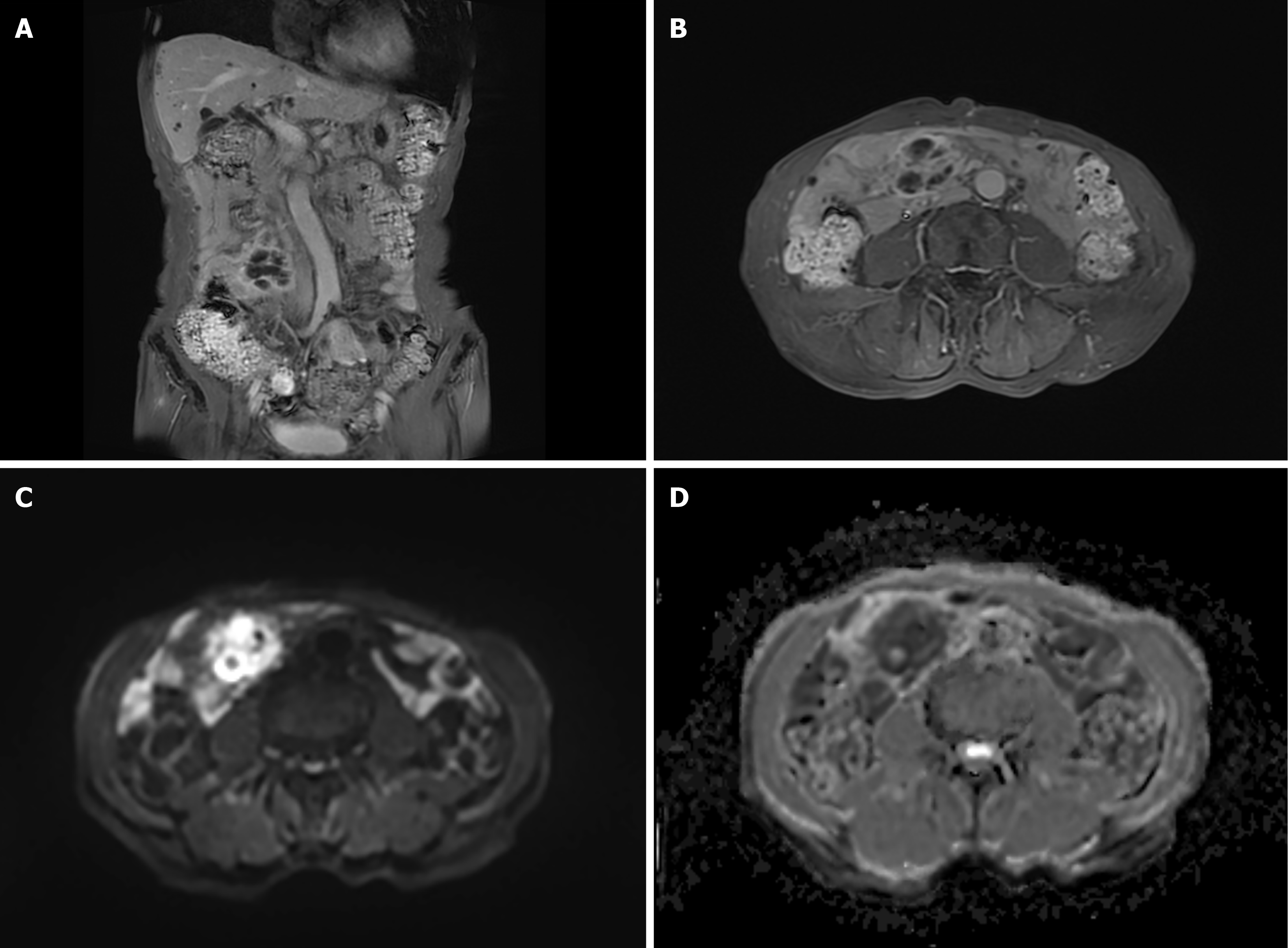
Enhanced computed tomography (CT) of the abdomen at the local hospital suggested a right lower abdominal mass, and scattered multiple nodules in the abdominal cavity (Figure 1A and B). Magnetic resonance (MR) dynamic enhancement + diffusion-weighted imaging of the upper abdomen suggested abnormally enhanced foci in the right lower abdominal cavity (Figure 2A–D) and further examination was recommended. An abnormal signal in the liver was indicative of mul
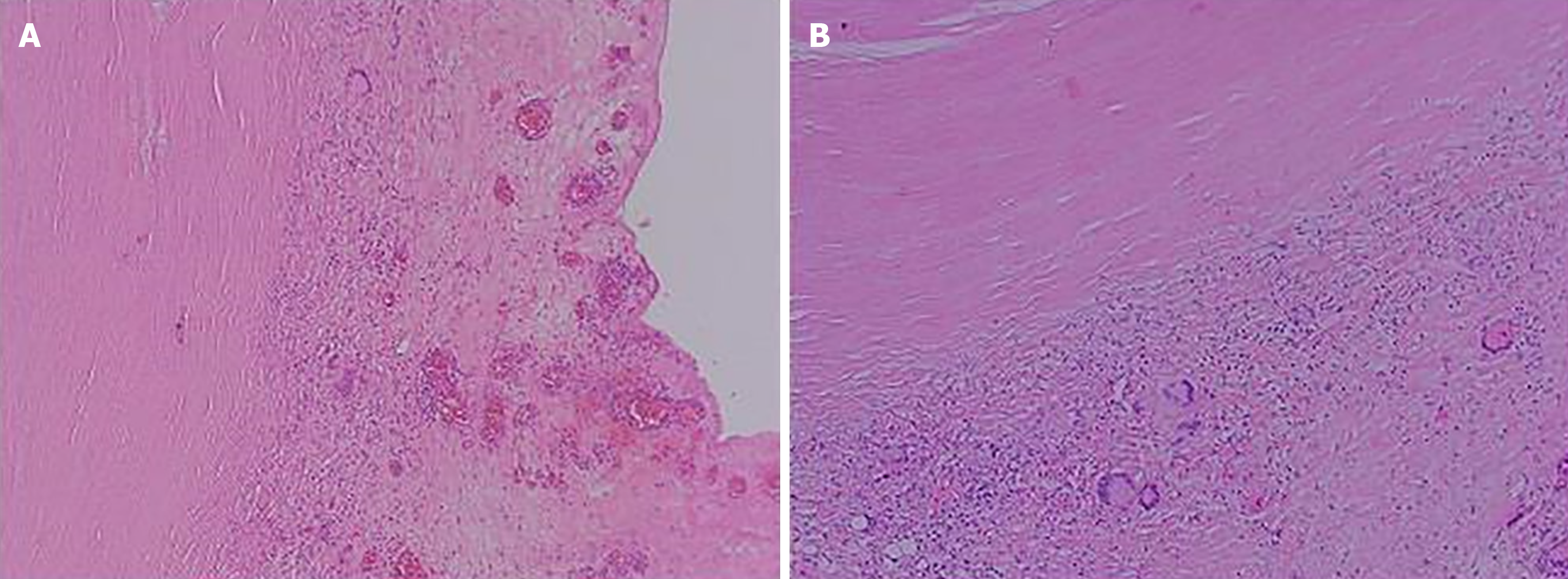
After ruling out contraindications for surgery, the patient underwent laparoscopic exploration on January 1, 2024. During the operation, the mass was incised and drained, and part of the mass tissues and several surrounding nodules were excised and sent for pathological examination. Postoperatively, T-cell test for TB infection, and nucleic acid test for M. tuberculosis (constrained proportional assignment method) were positive, and antacid staining was negative, and no antacid bacilli were seen. Postoperative pathology of the abdominal mass and intra-abdominal nodule suggested peripheral fibrotic tissue proliferation combined with multinucleated giant cell reaction (Figure 3A and B).
Combined with the past medical history, postoperative pathology and positive results of TB-related laboratory tests, the patient's primary diagnosis was determined to be TBP complicated by intraperitoneal tuberculous abscess.
Anti-inflammatory, rehydration, dressing change, nutritional support and other treatments were given after the opera
More than 1 month after surgery, the patient is on anti-TB treatment.
Patients with TBP often have comorbid TB infection in other organs. TBP is an insidious disease with subacute manifestations and is difficult to diagnose if it is not suspected.
Clinical history has revealed that most patients have a history and present with symptoms of TB, including low afternoon fever, night sweats, malaise, poor appetite, and emaciation[5]. Some studies have reported that the two most common symptoms of TBP are abdominal pain (31%–94%) and fever (45%–100%)[3,6-9]. The average duration of sym
Blood analysis, erythrocyte sedimentation rate and tuberculin test show that some patients have mild to moderate anemia, mostly normocytic normochromic. Leukocyte counts are mostly normal and increased in caseous patients or in those with acute spread of abdominal tuberculous foci. Erythrocyte sedimentation rate is increased in most patients and can be an indicator of active disease. A strong positive tuberculin test helps with the diagnosis of TB infection.
Ascites examination may show straw yellow exudate, a few being pale blood in color, specific gravity is usually more than 1.018, and protein content is more than 30 g/L, mainly lymphocytes. However, sometimes due to hypovitaminosis or combined cirrhosis, the nature of ascites fluid can resemble leakage fluid. If ascites glucose < 3.4 mmol/L and pH < 7.35, it suggests bacterial infection. If ascites adenosine deaminase activity is increased, it suggests TBP.
Ultrasound, CT and magnetic resonance imaging show thickened peritoneum, ascites, intra-abdominal masses and fistula. Scattered calcified shadows of mesenteric lymph nodes can be seen on abdominal ultrasound. Gastrointestinal x-ray barium meal examination can identify intestinal adhesions, intestinal TB, intestinal fistula, mass outside the intestinal lumen, and other signs.
Laparoscopy shows that the visceral surface of the peritoneum and omentum can have seen scattered or aggregated grey–white nodules. Laparoscopic biopsy is valuable in confirming the diagnosis of TBP. This examination is generally applicable to patients with free ascites, but is contraindicated in patients with extensive peritoneal adhesions. Laparo
Early diagnosis and treatment of TBP are important to improve the patient's condition, and some studies have noted that delayed anti-TB treatment is associated with high mortality[4]. Current TBP treatment follows that for extrapulmonary TB, with systemic anti-TB drug therapy as the mainstay, supplemented by nutritional support and abdominal local therapy. The principles of treatment are to adhere to early, combined, standardized anti-TB drugs and to strengthen systemic supportive therapy, to achieve complete cure, avoid recurrence and prevent complications. Strengthening supportive therapy includes: Bed rest, high protein, high calorie, high vitamin and easy-to-digest diet, daily supplementation of fresh fruits and milk, intravenous infusion when needed, and regular injection of albumin. Anti-TB drugs: Usually, three or four drugs are used for intensive treatment. Isoniazid 0.3 g–0.4 g, daily morning dose; rifampicin 0.45 g, once a day orally; ethambutol 0.75 g once a day orally. If necessary, streptomycin 0.75 g once daily intramuscularly or pyrazinamide 0.25 g–0.5 g three times daily can be added. Combined treatment with four drugs for 2 months, and then continued treatment with isoniazid and rifampicin for at least 7 months. For those with hematogenously disseminated lesions or significant TB toxemia, short-term treatment with prednisone can be added to anti-TB drugs, with 30 mg/d–40 mg/d, orally in divided doses.
For patients who have obvious exudative type ascites, the fluid can be drained once a week, followed by intraperitoneal injection of 100 mg isoniazid and 0.25 g streptomycin.
Surgical treatment is limited to patients with complete intestinal obstruction, intestinal fistula or complications of intestinal perforation[24,25]. When the disease is difficult to diagnose and cannot be differentiated from intra-abdominal tumor or some causes of acute abdomen, a cesarean section may be considered.
The final diagnosis of our case was TBP complicated by intraperitoneal tuberculous abscess. When an abdominal tumor is suspected, we should ask patients whether they have a history of TB or contact with someone else with TB. This will help to diagnose and treat more accurately, avoid missed diagnosis or misdiagnosis, and improve the therapeutic effect and prognosis of the patient.
| 1. | Bagcchi S. WHO's Global Tuberculosis Report 2022. Lancet Microbe. 2023;4:e20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 670] [Cited by in RCA: 564] [Article Influence: 282.0] [Reference Citation Analysis (0)] |
| 2. | Wu N, Xu Z, Huang WF. Tuberculous peritonitis. Dig Liver Dis. 2024;56:367-368. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Sanai FM, Bzeizi KI. Systematic review: tuberculous peritonitis--presenting features, diagnostic strategies and treatment. Aliment Pharmacol Ther. 2005;22:685-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 239] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 4. | Chow KM, Chow VC, Hung LC, Wong SM, Szeto CC. Tuberculous peritonitis-associated mortality is high among patients waiting for the results of mycobacterial cultures of ascitic fluid samples. Clin Infect Dis. 2002;35:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 132] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Vaid U, Kane GC. Tuberculous Peritonitis. Microbiol Spectr. 2017;5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Tan KK, Chen K, Sim R. The spectrum of abdominal tuberculosis in a developed country: a single institution's experience over 7 years. J Gastrointest Surg. 2009;13:142-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Chen HL, Wu MS, Chang WH, Shih SC, Chi H, Bair MJ. Abdominal tuberculosis in southeastern Taiwan: 20 years of experience. J Formos Med Assoc. 2009;108:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 8. | Muneef MA, Memish Z, Mahmoud SA, Sadoon SA, Bannatyne R, Khan Y. Tuberculosis in the belly: a review of forty-six cases involving the gastrointestinal tract and peritoneum. Scand J Gastroenterol. 2001;36:528-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Demir K, Okten A, Kaymakoglu S, Dincer D, Besisik F, Cevikbas U, Ozdil S, Bostas G, Mungan Z, Cakaloglu Y. Tuberculous peritonitis--reports of 26 cases, detailing diagnostic and therapeutic problems. Eur J Gastroenterol Hepatol. 2001;13:581-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 81] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Huang B, Cui DJ, Ren Y, Han B, Yang P, Zhao X. Comparison between laparoscopy and laboratory tests for the diagnosis of tuberculous peritonitis. Turk J Med Sci. 2018;48:711-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Wu CH, Changchien CC, Tseng CW, Chang HY, Ou YC, Lin H. Disseminated peritoneal tuberculosis simulating advanced ovarian cancer: a retrospective study of 17 cases. Taiwan J Obstet Gynecol. 2011;50:292-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Bilgin T, Karabay A, Dolar E, Develioğlu OH. Peritoneal tuberculosis with pelvic abdominal mass, ascites and elevated CA 125 mimicking advanced ovarian carcinoma: a series of 10 cases. Int J Gynecol Cancer. 2001;11:290-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 77] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Ozalp S, Yalcin OT, Tanir HM, Kabukcuoglu S, Akcay A. Pelvic tuberculosis mimicking signs of abdominopelvic malignancy. Gynecol Obstet Invest. 2001;52:71-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Mahdavi A, Malviya VK, Herschman BR. Peritoneal tuberculosis disguised as ovarian cancer: an emerging clinical challenge. Gynecol Oncol. 2002;84:167-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Zaidi SN, Conner M. Disseminated peritoneal tuberculosis mimicking metastatic ovarian cancer. South Med J. 2001;94:1212-1214. [PubMed] |
| 16. | Thakur V, Mukherjee U, Kumar K. Elevated serum cancer antigen 125 levels in advanced abdominal tuberculosis. Med Oncol. 2001;18:289-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Rai S, Thomas WM. Diagnosis of abdominal tuberculosis: the importance of laparoscopy. J R Soc Med. 2003;96:586-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Wu JF, Li HJ, Lee PI, Ni YH, Yu SC, Chang MH. Tuberculous peritonitis mimicking peritonitis carcinomatosis: a case report. Eur J Pediatr. 2003;162:853-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Lal N, Soto-Wright V. Peritoneal tuberculosis: diagnostic options. Infect Dis Obstet Gynecol. 1999;7:244-247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Bouma BJ, Tytgat KM, Schipper HG, Kager PA. Be aware of abdominal tuberculosis. Neth J Med. 1997;51:119-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Protopapas A, Milingos S, Diakomanolis E, Elsheikh A, Protogerou A, Mavrommatis K, Michalas S. Miliary tuberculous peritonitis mimicking advanced ovarian cancer. Gynecol Obstet Invest. 2003;56:89-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Sandikçi MU, Colakoglu S, Ergun Y, Unal S, Akkiz H, Sandikçi S, Zorludemir S. Presentation and role of peritoneoscopy in the diagnosis of tuberculous peritonitis. J Gastroenterol Hepatol. 1992;7:298-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Chow KM, Chow VC, Szeto CC. Indication for peritoneal biopsy in tuberculous peritonitis. Am J Surg. 2003;185:567-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 83] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 24. | Rasheed S, Zinicola R, Watson D, Bajwa A, McDonald PJ. Intra-abdominal and gastrointestinal tuberculosis. Colorectal Dis. 2007;9:773-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Khan AR, Morris LM, Keswani SG, Khan IR, Le L, Lee WC, Hunt JP. Tuberculous peritonitis: a surgical dilemma. South Med J. 2009;102:94-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |