Published online Sep 16, 2024. doi: 10.12998/wjcc.v12.i26.5946
Revised: June 20, 2024
Accepted: June 27, 2024
Published online: September 16, 2024
Processing time: 167 Days and 19.2 Hours
Primary light chain amyloidosis is a rare and complex disease with complex clinical features and is highly susceptible to misdiagnosis and underdiagnosis in the early stages.
We report a case of a 47-year-old female patient whose only initial symptom was periorbital purpura, which was not taken seriously enough. As the disease progressed, pleural effusion gradually appeared, and after systematic diagnosis and treatment, she was diagnosed with “primary light chain amyloidosis”. She achieved rapid hematological remission after treatment with a daratumumab + bortezomib + cyclophosphamide + dexamethasone regimen.
Periorbital purpura can be the only initial symptom of primary light chain amy
Core Tip: Amyloidosis is a rare and difficult to diagnose disease. Periorbital purpura can be the only initial symptom of primary light chain amyloidosis, and we should pay attention to these cases.
- Citation: Wang XF, Li T, Yang M, Huang Y. Periorbital purpura can be the only initial symptom of primary light chain amyloidosis: A case report. World J Clin Cases 2024; 12(26): 5946-5951
- URL: https://www.wjgnet.com/2307-8960/full/v12/i26/5946.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i26.5946
Amyloidosis is a rare disease that is difficult to diagnose, which is a collective term for clinical disorders that occur due to localized or systemic accumulation of amyloid. Amyloid protein misfolds into β-fold and deposits in human tissues and organs, leading to organ dysfunction[1]. In 1923, Bennhold found Congo red stained amyloid deposits with typical apple green birefringence under polarized light microscopy, becoming the gold standard for the pathology of amyloidosis. More than thirty types of amyloidosis have been identified, the most common being the light chain (AL) type of amyloidosis due to deposition of immunoglobulin light chains secreted by aberrant clonal plasma cells, as well as the transthyretin (ATTR) type, serum amyloid (AA) type, and others[2].
Owing to the rarity and complexity of amyloidosis, many clinicians do not recognize it and it is easily misdiagnosed and underdiagnosed in its early stage. Here, we report the case of a patient with periorbital purpura as the initial symptom that was not effectively diagnosed, progressed to pleural effusion, and was finally diagnosed with primary light-chain amyloidosis.
A 47-year-old female patient with petechiae formed when she rubbed her eyelids lightly for half a year, without any other bleeding symptoms such as epistaxis, vomiting blood, black stools, etc, as well as any systemic symptom.
The patient was treated at several hospitals as allergies or bleeding; however, the treatment was ineffective. One week prior, she had shortness of breath after activity and was admitted to our hospital after ultrasonography revealed pleural effusion at a local hospital.
The patient had no significant previous medical history.
The patient denied any family history of malignancy.
During the physical examination upon admission, periorbital purpura were seen (Figure 1), and the right lower lung was hypopneic, with turbid tones on percussion, and no dry or wet rales.
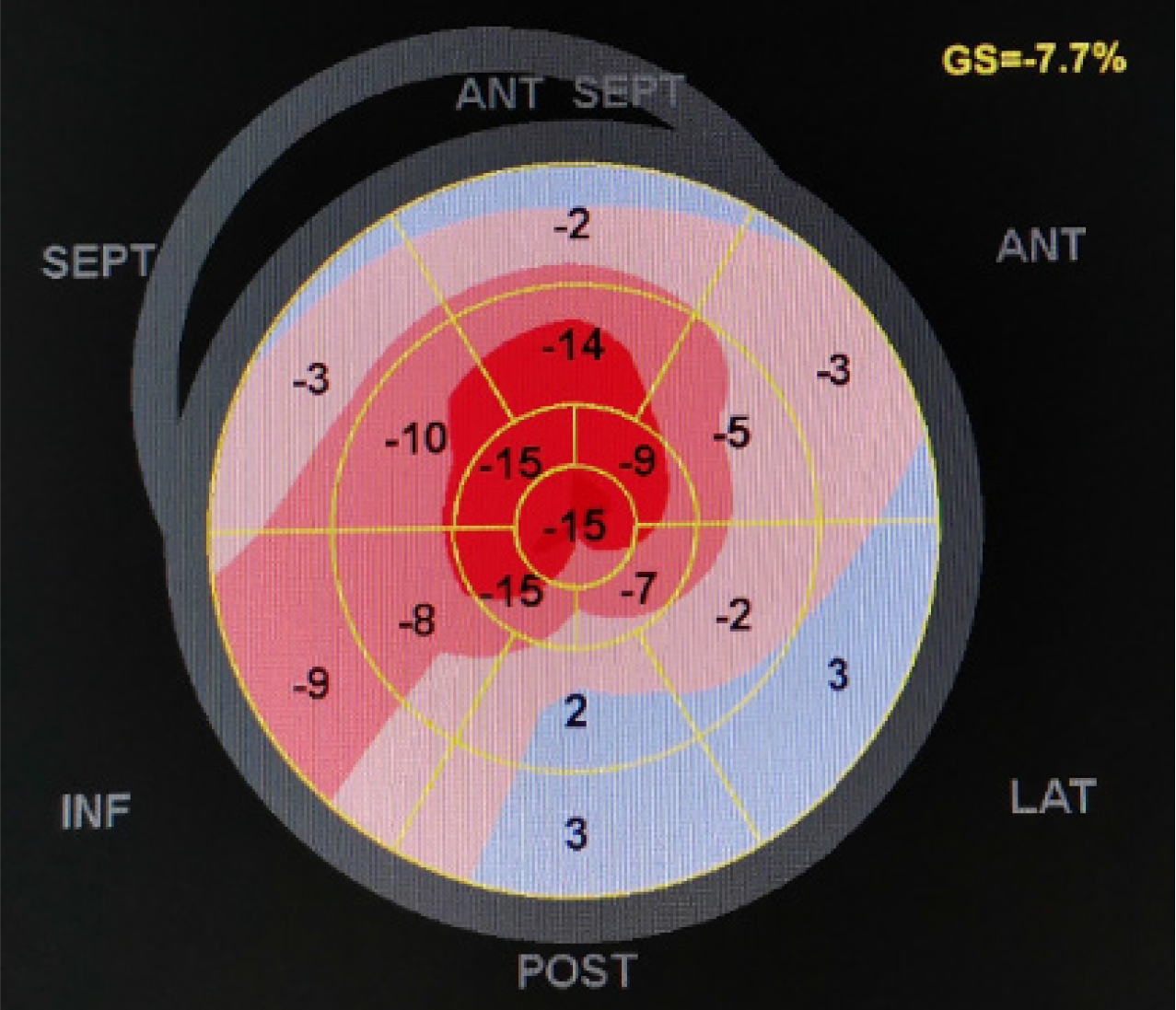
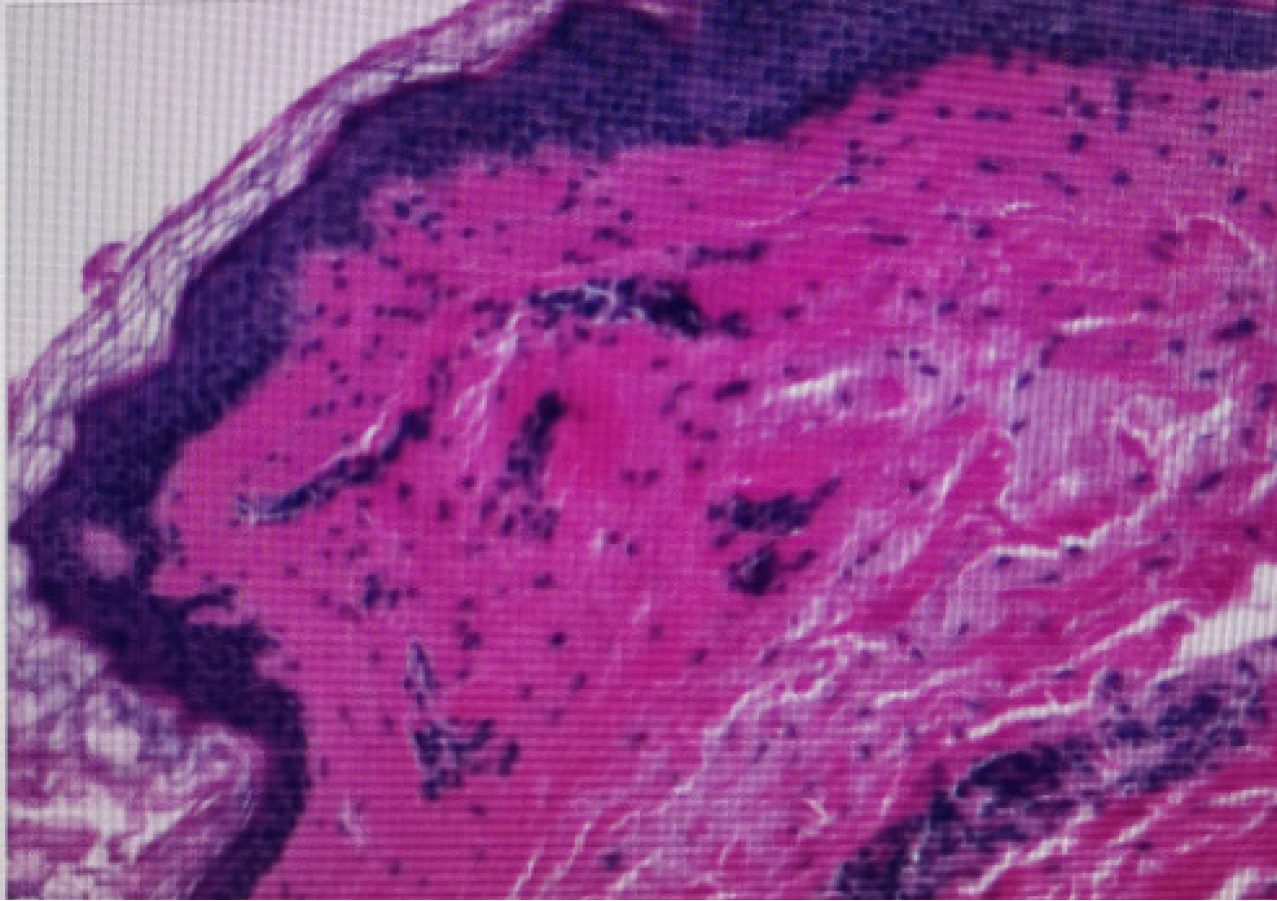
Admission routine blood and coagulation function tests did not show any abnormality, denied long-term oral antiplatelet aggregation drugs, the nature of the pleural fluid was leakage fluid, cardiac ultrasound showed that the interventricular septum was 12 mm, left ventricular ejection fractions was 62%; two-dimensional speckle tracking strain and strain rate imaging of the myocardium with significant reduction in overall longitudinal strain of the left ventricle and visible apical exemption phenomenon (Figure 2); Brain natriuretic peptide: 3400 pg/mL, further immunofixation electrophoresis showed that the IgA-L was positive, the median value of difference between involved and uninvolved serum immunoglobulin free light chain levels (dFLC) was 320 ng/mL, and bone marrow cytology showed 12% plasma cells; abdominal fat biopsy showed amyloid deposition in collagen fibers of the dermis and positive Congo red staining (Figure 3).
Primary light chain amyloidosis (cardiac and soft tissue involvement).
The patient was treated with a daratumumab + bortezomib + cyclophosphamide + dexamethasone (D-VCD) regimen.
The patient achieved a stringent complete response in one cycle and is now undergoing regular treatment.
Primary light chain amyloidosis (AL type) is a rare hematologic disorder primarily associated with abnormal proliferation of clonal plasma cells and, to a lesser extent, with lymphoproliferative disorders[3]. Currently, according to statistical data in Europe and the United States, the incidence of the disease is about 9-14 per million person-years. AL amyloidosis is most commonly seen in the elderly, with a median age at diagnosis of about 60 years, and the proportion of male patients is slightly higher than that of females[4]. Currently, the majority of AL patients are not recognized and diagnosed early, and even in referral centers it takes a median of 10 months to diagnose patients with pre-existing plasma cell malignancy[4], yet even a few months of delay can irreversibly result in the loss of the opportunity for patients to benefit from effective treatments. Therefore, early recognition and diagnosis of AL is a pressing concern.
In our case, the initial symptom was periorbital purpura without other systemic symptoms. The patient was seen in the dermatology department of several hospitals, but the etiology had not been recognized. As the disease progressed, the patient gradually developed pleural effusion, which on detailed examination revealed ventricular septal hyperplasia, ejection fraction preserved heart failure, positive monoclonal immunoglobulin, plasma cell hyperplasia in the bone marrow, and positive Congo red staining of an abdominal fat biopsy. Therefore, she was diagnosed with “primary light chain amyloidosis (cardiac and soft tissue involvement)”.
In this case, periorbital purpura was the only initial symptom of primary light chain amyloidosis. The European Society of Cardiology statement also indicates that unexplained skin bruising may be a red flag for amyloidosis, especially in combination with heart failure with preserved ejection fraction[5]. Although periorbital purpura is pathognomonic for AL amyloidosis, it is rare, occurring in 1%-10% of cases, especially in patients whose initial symptom is only periorbital purpura. Primary light chain amyloidosis may also present with other cutaneous and mucosal manifestations, such as waxing and thickening, petechiae, and subcutaneous nodules or plaques, which need to be differentiated from the cutaneous manifestations of xanthomatosis, progressive necrotizing yellow granuloma, dermatomyositis, and senile purpura[6]. The cause of periorbital purpura may be related to amyloid deposition within the vessel wall, leading to increased vascular fragility, and when large amounts of amyloid are deposited in the skin, papules, plaques, and even nodules with bleeding manifestations may appear[5,6].
We suggest that patients with unexplained periorbital purpura should be examined in detail and be aware of the presence of comorbid systemic symptoms such as edema, proteinuria, hypotension, peripheral neuropathy, etc. If there is such a condition, then there is a need to be vigilant against systemic amyloidosis, which requires further blood/urine immunoprotein electrophoresis, free light chain and other tests, and, if necessary, a biopsy of the affected tissues and bone marrow or abdominal wall fat to make a definitive diagnosis.
The current diagnosis of AL-type amyloidosis requires the following[7]: Clinical manifestations of typical organ involvement + evidence of M protein (for M protein detection, serum free light chain, serum immunofixation electrophoresis combined with urine immunofixation electrophoresis is recommended, and the combination of all three can achieve a positive rate of up to 98.4%[8]) + positive Congo red staining of the tissue biopsy (the highest positivity is detected in the involved organs, and abdominal wall fat and bone marrow can also be part of the available biopsy[9]) + deposited amyloid material identified as immunoglobulin light chains.
All patients with AL amyloidosis should begin treatment for the primary disease as soon as possible after diagnosis. The primary goal is to achieve rapid and deep hematologic remission, with a greater proportion of organ remission achieved as hematologic remission deepens (from very good partial response to microscopic residual disease-negative), although organ remission tends to lag behind hematologic remission by several months[10]. Current therapeutic options target plasma cells. Daltolizumab is a humanized IgG-κ monoclonal antibody targeting the CD38 antigen on the surface of plasma cells, and a prospective randomized controlled study published in the July 2021 issue of the New England Journal of Medicine explored the value of chemotherapy in combination with or without daltolizumab in patients with primary AL-type amyloidosis, showing that combination of daratumumab with a regimen of bortezomib + cyclophosphamide + dexamethasone significantly improved hematologic complete remission. Monoclonal antibody significantly increased the rates of hematologic complete remission (53.3% vs 18.1%) and cardiac remission (41.5% vs 22.2%), and prolonged the progression-free survival of patients[11]. Therefore, daratumumab was included in the first-line treatment. Our patient was also treated with the D-VCD regimen, which led to a rapid hematologic remission. It is believed that organ remission will slowly appear with time.
Progress in anti-amyloid therapy has been relatively slow. Ward et al[12] found that oral doxycycline reduced amyloid deposition in the stomachs of mice with AL-type amyloidosis, while a European retrospective cohort study found that the combination of doxycycline on the basis of chemotherapy improved the rate of cardiac remission and survival time[13]. As a result, doxycycline has been included in the NCCN guidelines as a treatment option for AL-type amyloidosis, but a multicenter randomized controlled study led by Peking Union Medical College Hospital showed that chemotherapy-based combination of doxycycline did not prolong progression-free survival and cardiac remission rate in patients[14]. CAEL-101 is a monoclonal antibody targeting misfolded light chains that promotes phagocytosis and clearance of amy
Periorbital purpura may be the only initial symptom of primary light chain amyloidosis. We suggest that when seeing a patient with periorbital purpura, we should be aware of the possibility of amyloidosis. The earlier the diagnosis, the faster treatment can begin, thus delaying or avoiding the progression of irreversible disease such as renal failure and cardiomyopathy.
| 1. | Chiti F, Dobson CM. Protein Misfolding, Amyloid Formation, and Human Disease: A Summary of Progress Over the Last Decade. Annu Rev Biochem. 2017;86:27-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1684] [Cited by in RCA: 1859] [Article Influence: 232.4] [Reference Citation Analysis (1)] |
| 2. | Dogan A. Amyloidosis: Insights from Proteomics. Annu Rev Pathol. 2017;12:277-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Wechalekar AD, Gillmore JD, Hawkins PN. Systemic amyloidosis. Lancet. 2016;387:2641-2654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 557] [Cited by in RCA: 663] [Article Influence: 73.7] [Reference Citation Analysis (0)] |
| 4. | Quock TP, Yan T, Chang E, Guthrie S, Broder MS. Epidemiology of AL amyloidosis: a real-world study using US claims data. Blood Adv. 2018;2:1046-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 274] [Article Influence: 45.7] [Reference Citation Analysis (0)] |
| 5. | Gertz MA, Dispenzieri A. Systemic Amyloidosis Recognition, Prognosis, and Therapy: A Systematic Review. JAMA. 2020;324:79-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 180] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 6. | Merlini G, Seldin DC, Gertz MA. Amyloidosis: pathogenesis and new therapeutic options. J Clin Oncol. 2011;29:1924-1933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 359] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 7. | Chen-Xu M, Achilleos K. Periorbital purpura of AL amyloidosis. Rheumatology (Oxford). 2021;60:1165. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Zhang CL, Feng J, Shen KN, Su W, Zhang CL, Huang XF, Cao XX, Zhang L, Zhou DB, Li J. [The diagnostic and prognostic values of serum free light chain in patients with primary light chain amyloidosis]. Zhonghua Xue Ye Xue Za Zhi. 2016;37:942-945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Gertz MA. Immunoglobulin light chain amyloidosis: 2016 update on diagnosis, prognosis, and treatment. Am J Hematol. 2016;91:947-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 86] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 10. | Manwani R, Cohen O, Sharpley F, Mahmood S, Sachchithanantham S, Foard D, Lachmann HJ, Quarta C, Fontana M, Gillmore JD, Whelan C, Hawkins PN, Wechalekar AD. A prospective observational study of 915 patients with systemic AL amyloidosis treated with upfront bortezomib. Blood. 2019;134:2271-2280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 140] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 11. | Kastritis E, Palladini G, Minnema MC, Wechalekar AD, Jaccard A, Lee HC, Sanchorawala V, Gibbs S, Mollee P, Venner CP, Lu J, Schönland S, Gatt ME, Suzuki K, Kim K, Cibeira MT, Beksac M, Libby E, Valent J, Hungria V, Wong SW, Rosenzweig M, Bumma N, Huart A, Dimopoulos MA, Bhutani D, Waxman AJ, Goodman SA, Zonder JA, Lam S, Song K, Hansen T, Manier S, Roeloffzen W, Jamroziak K, Kwok F, Shimazaki C, Kim JS, Crusoe E, Ahmadi T, Tran N, Qin X, Vasey SY, Tromp B, Schecter JM, Weiss BM, Zhuang SH, Vermeulen J, Merlini G, Comenzo RL; ANDROMEDA Trial Investigators. Daratumumab-Based Treatment for Immunoglobulin Light-Chain Amyloidosis. N Engl J Med. 2021;385:46-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 370] [Article Influence: 92.5] [Reference Citation Analysis (0)] |
| 12. | Ward JE, Ren R, Toraldo G, Soohoo P, Guan J, O'Hara C, Jasuja R, Trinkaus-Randall V, Liao R, Connors LH, Seldin DC. Doxycycline reduces fibril formation in a transgenic mouse model of AL amyloidosis. Blood. 2011;118:6610-6617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 120] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 13. | Wechalekar AD, Whelan C. Encouraging impact of doxycycline on early mortality in cardiac light chain (AL) amyloidosis. Blood Cancer J. 2017;7:e546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 14. | Shen KN, Fu WJ, Wu Y, Dong YJ, Huang ZX, Wei YQ, Li CR, Sun CY, Chen Y, Miao HL, Zhang YL, Cao XX, Zhou DB, Li J. Doxycycline Combined With Bortezomib-Cyclophosphamide-Dexamethasone Chemotherapy for Newly Diagnosed Cardiac Light-Chain Amyloidosis: A Multicenter Randomized Controlled Trial. Circulation. 2022;145:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 15. | Edwards CV, Rao N, Bhutani D, Mapara M, Radhakrishnan J, Shames S, Maurer MS, Leng S, Solomon A, Lentzsch S, Eisenberger A. Phase 1a/b study of monoclonal antibody CAEL-101 (11-1F4) in patients with AL amyloidosis. Blood. 2021;138:2632-2641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |