Published online Sep 6, 2024. doi: 10.12998/wjcc.v12.i25.5761
Revised: June 11, 2024
Accepted: July 3, 2024
Published online: September 6, 2024
Processing time: 197 Days and 2.5 Hours
This case report contributes to the medical literature by highlighting the succe
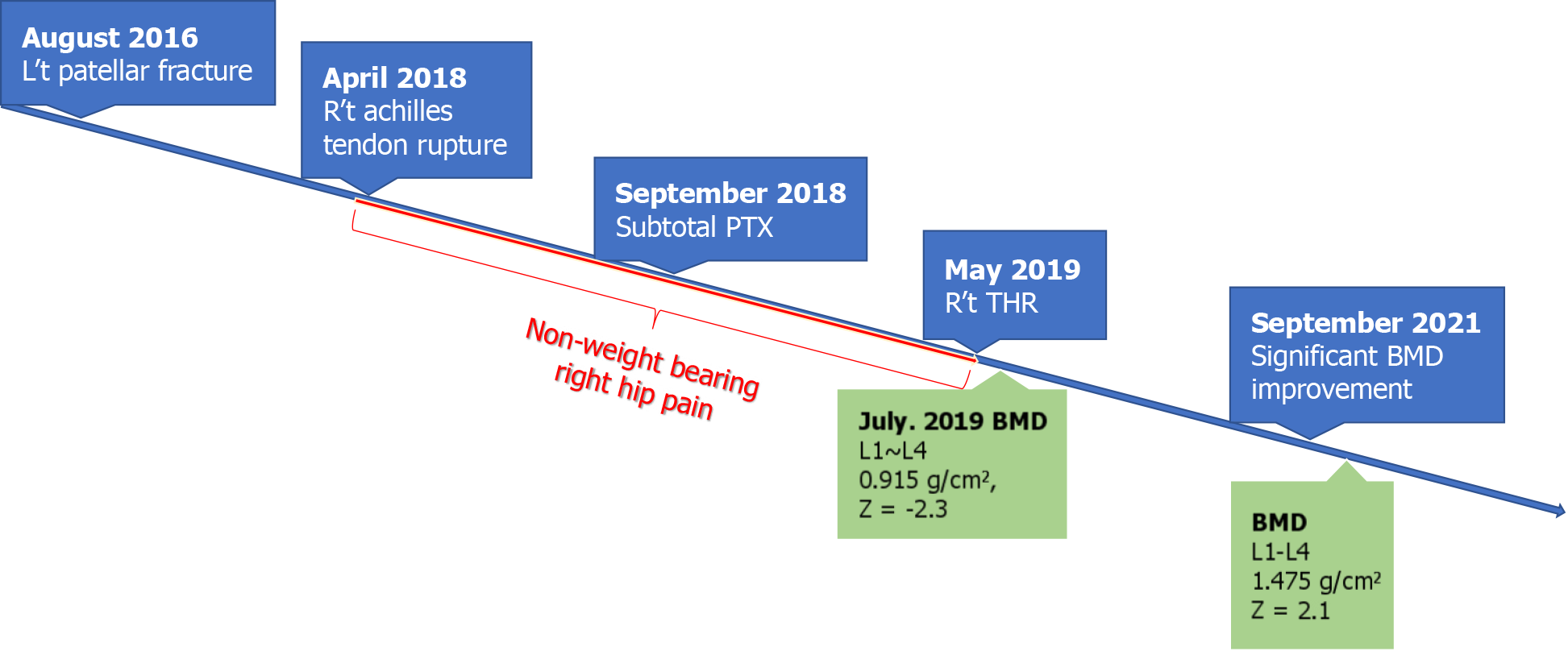
A 36-year-old female with renal osteodystrophy and on dialysis due to ESRD presented with a history of left patellar tendon rupture and later, a right achilles tendon avulsion fracture. Persistent right hip pain led to the discovery of a neglected right femoral neck fracture, which was initially overlooked due to the patient’s complex medical history. Two months post-achilles tendon repair, the patient underwent PTX to manage the refractory SHPTH. The postoperative course included rehabilitation and weight-bearing exercises. Remarkably, 2 years after osteosynthesis, radiographic assessments indicated a solid union of the periprothesis fracture and significant improvement in BMD, showcasing the efficacy of the treatment approach.
PTX, combined with appropriate rehabilitation, is crucial for improving BMD and fracture healing in ESRD patients with SHPTH.
Core Tip: This case report illustrates the successful treatment of a neglected femoral neck fracture in a patient with renal osteodystrophy and secondary hyperparathyroidism (SHPTH). The patient, suffering from end-stage renal disease (ESRD) on dialysis, experienced significant improvement in bone mineral density and fracture healing post-parathyroidectomy. This intervention, along with tailored rehabilitation and weight-bearing exercises, highlights the importance of managing SHPTH in ESRD patients to enhance bone health and reduce fracture risks. This multidisciplinary approach demonstrates a vital strategy for improving outcomes for patients with complex skeletal disorders associated with chronic kidney disease.
- Citation: Lin TC, Lin SW, Yeh KT. Parathyroidectomy restored bone mineral density in a neglected femoral neck fracture with renal osteodystrophy: A case report. World J Clin Cases 2024; 12(25): 5761-5768
- URL: https://www.wjgnet.com/2307-8960/full/v12/i25/5761.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i25.5761
Secondary hyperparathyroidism (SHPTH) occurs due to an increase in parathyroid hormone, which begins as the estimated glomerular filtration rate declines below 60 mL/min/1.73 m2. It is an adaptive process of the parathyroid gland to mitigate the deficit of serum calcium and 1,25-dihydroxy vitamin D and the inability of the kidney to excrete phosphorus into the urine[1]. SHPTH is an independent predictor of fractures, cardiovascular events, and death; therefore, it requires early intervention to improve the prognosis[2]. Despite the development of several pharmaceutical options to maintain serum calcium, vitamin D3, and phosphorus levels in patients with chronic kidney disease grade 3A-5D[3], 15% of them eventually develop medically refractory SHPTH and require parathyroidectomy (PTX), an established indication according to the 2017 Kidney Disease Improving Global Outcomes (KDIGO) guidelines[4].
We report the case of a hemodialysis patient who underwent subtotal PTX 8 months before the discovery of a right femoral neck fracture and total hip replacement (THR) at our facility. At the 3-year follow-up, good clinical outcomes were achieved, as reflected by increased bone mineral density (BMD), alleviation of bone pain, and termination of low-energy fracture episodes. The patient provided consent for the collection and publication of her medical records.
A 36-year-old woman presented to the orthopedic clinic with right hip pain and impaired weight-bearing for 1 year despite medical treatment.
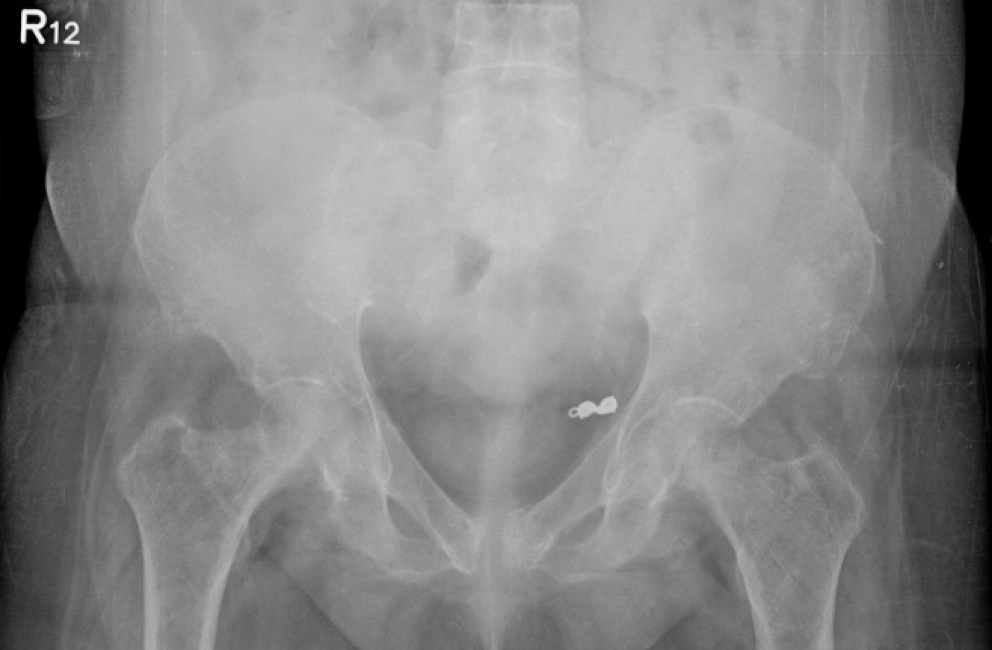
Right hip pain occurred after she fell to the ground and was trapped by her motorcycle 1 year prior. The patient’s symptoms, which were thought to be due to a muscular strain, were managed medically as the right hip radiograph showed no apparent right hip fracture after the accident (Figure 1). One year later, the patient could not fully bear the weight of her right foot because of persistent right hip pain. The patient had no history of steroid use or substance abuse and had no further hip trauma since the fall of the previous year.
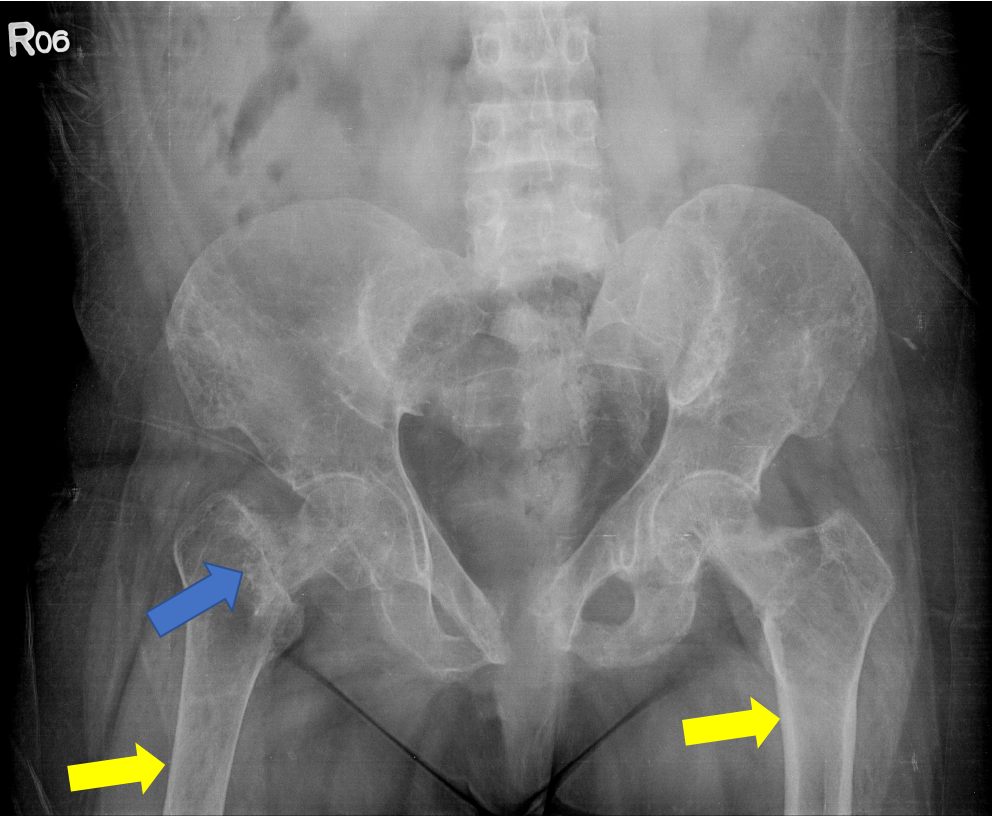
The patient had a history of type one diabetes mellitus, with 10 years of end-stage renal disease (ESRD) and undergoing hemodialysis three times a week. Furthermore, she had diffused bone pain for many years, one episode of left patellar fracture after a slip injury, status post tendon repair (Figure 2), one episode of right achilles tendon rupture due to a low-energy impact status 8 months after the tendon repair (Figure 3), and subtotal PTX for SHPTH 8 months ago.
The patient was not a smoker. She did not drink alcohol or use illicit drugs, and her family history was non-contributory.
The patient was able to ambulate with a walker on review, but an antalgic gait was noted. The patient could not stand on her right leg because of pain in her right hip.
The patient’s preoperative laboratory values for the right THR were hemoglobin level, 9.0 g/dL, alkaline phosphatase level, 224 U/L; calcium level, 7.8 mg/dL, phosphorus level, 3.0 mg/dL, and intact parathyroid hormone (iPTH) level, 42 pg/mL.
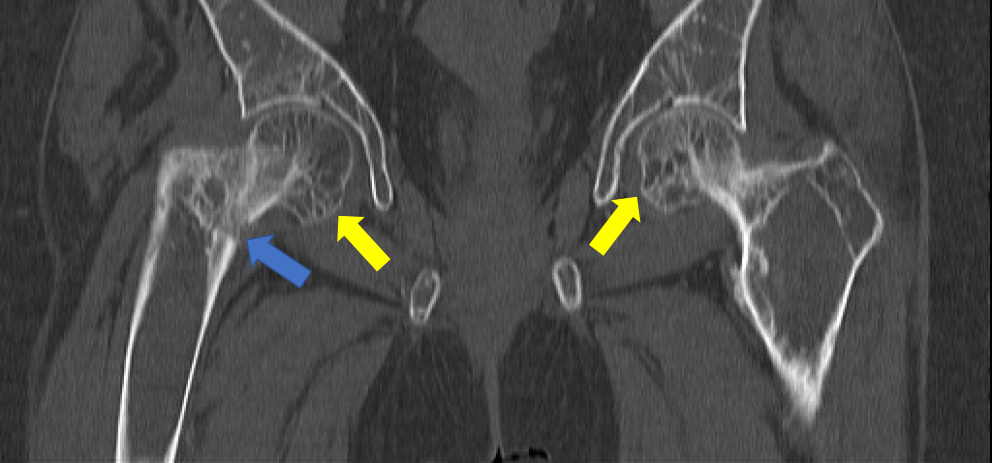
An anteroposterior view of the patient’s right hip showed no apparent fracture immediately after the fall (Figure 1); however, one year later, hip radiography (Figure 4) and computed tomography (Figure 5) for persistent right hip pain indicated an occult right femoral neck fracture.
Neglected right femoral neck fracture, SHPTH with renal osteodystrophy, and osteoporosis.
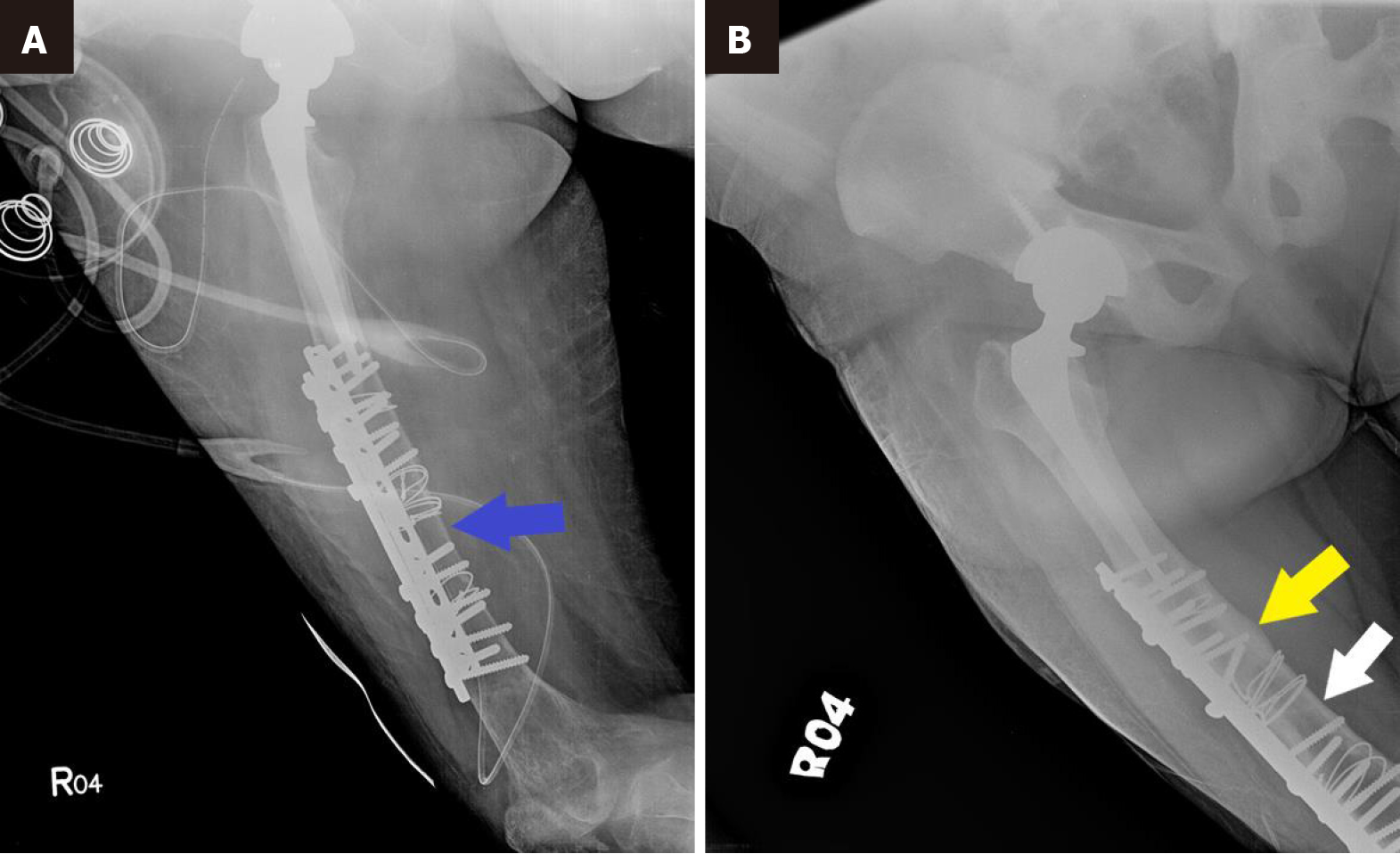
The patient underwent right THR for a neglected right femoral neck fracture via the posterior approach; however, due to severe osteoporosis of the diaphysis, an iatrogenic femoral shaft fracture occurred during manual maneuvering of the right hip. Therefore, an additional open reduction and internal fixation of the fracture was performed with cerclage wire and double plating (Figure 6). Postoperative rehabilitation and increased weight bearing were encouraged.
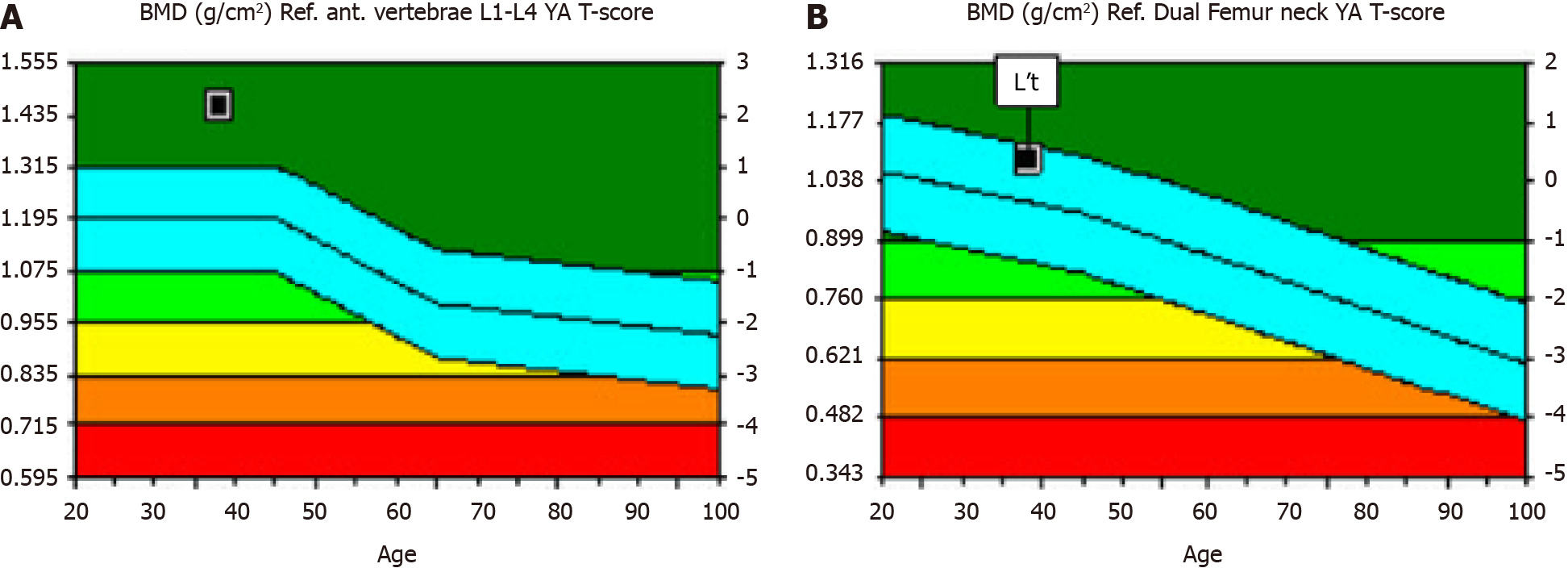
Ten months after subtotal PTX and 2 months after right THR, the patient’s bone density scan still showed osteopenia [lumbar spine (L1-L4) bone density = 0.915 g/cm2, Z score = -2.3] (Figure 7).
Three years after subtotal PTX and 2 years after right hip surgery, an excellent clinical outcome was achieved, which was reflected by a significant improvement in the BMD (lumbar spine L1-L4 level, bone marrow density = 1.475 g/cm2, Z score = 2.1) (Figure 8) and in the repeat radiographic study (Figure 6). SHPTH and hyperphosphatemia had also resolved according to laboratory follow-ups (Table 1). Six years after subtotal PTX and 5 years after hip surgery, the patient experienced no further generalized bone pain and was free from new episodes of stress fractures (Figure 9).
| The 12 months before PTX | The 6 months before PTX | The 1 day before PTX | The 1 day after PTX | The 6 months after PTX | The 12 months after PTX | |
| PTH (pg/mL) | 1016 | 1141 | 4579 | 42 | 250 | 341 |
| P (mg/dL) | 5.4 | 8.5 | 8.5 | 7.6 | 2.9 | 2.8 |
| Ca2+ (mg/dL) | 9.5 | 8.0 | 8.9 | 9.1 | 7.1 | 8.8 |
SHPTH affects more than half of patients with chronic renal disease above stage 3 or 4[2,5] in the setting of deranged electrolytes and hormonal status[6]. It is an adaptive process of the parathyroid gland to compensate for hypocalcemia, low 1,25-α dihydroxy vitamin D levels, and hyperphosphatemia in the failing kidney to maintain normal bone remo
The relationship between renal replacement therapy (RRT) and hip fracture is well established, with previous studies reporting a 14 times higher incidence and three times 1-year postoperative mortality rate in patients undergoing RRT than in those who are not[8,9]. Moreover, hyperparathyroidism-related hypercalcemia and hyperphosphatemia lead to vascular calcification, resulting in cardiovascular mortality[10].
Therefore, early treatment of SHPTH to maintain a target range of iPTH, serum calcium, and phosphate is critical, as it prevents the development of the aforementioned complications after monoclonal expansion of the parathyroid gland, where standard medication becomes ineffective[1].
According to the 2017 KDIGO guidelines, the standard treatment for patients with ESRD above stage 4 includes calcitriol and vitamin D analogs, whereas in chronic kidney disease, stage 5D calcimimetics and phosphate binders should be utilized, with monthly monitoring of serum calcium, PTH, and phosphorus[3,4]. The guidelines further suggest PTX if the intact PTH (iPTH) level is persistently elevated ( > 500 pg/mL) despite maximal medical treatment rather than relying on a single PTH level. Compared with medical treatment PTX is related to a decreased risk of vertebral fracture and improved BMD 5 years postoperatively in a randomized trial[11,12]. The patient underwent PTX as suggested due to consistently highly elevated intact PTH (> 1000 pg/mL for years) despite receiving standard medications including 1,25-α dihydroxy vitamin D, phosphate binders, and calcimimetics, with the iPTH value measured at 4579 pg/mL/day preoperatively.
The long-term adverse effects of SHPTH (renal osteodystrophy) were apparent in the present case, as evidenced by her susceptibility to low-energy tendon rupture, diffuse bone pain, and osteitis fibrosa cystica of the femoral head according to the radiographic survey. Adding to the severe bone loss in the presented case was pain-related disuse osteopenia[13], reflected by the preferential thinning of the right femoral cortical bone compared with the left seen in the radiograph.
We believed that disuse bone loss further aggravated bone strength, which predisposed the patient to iatrogenic fracture during hip maneuvering, even though she had undergone subtotal PTX 1 year prior.
The multiloculated cystic lesions with varying degrees of central radiolucency in the bilateral femoral heads (Figure 5) likely reflect increased bone remodeling and negative bone balance, indicating renal osteodystrophy of the high bone turnover type in the present case[14-16]. Three years after receiving PTX and 2 years after right THR, our patient showed significantly improved BMD of the left femoral neck, which aligns with the previous study[17]. We believe the impro
In summary, we report the case of a young female with persistent hyperparathyroidism complicated by recurrent fragility and neglected fractures, with a neglected right femoral neck fracture who achieved a significant increase in BMD 3 years after subtotal PTX, THR combined with weight-bearing rehabilitation. By presenting a case of a SHPTH with typical features of renal osteodystrophy, orthopedists should be aware of bone mineral disease as the major cause and initiate a multidisciplinary approach involving orthopedists, nephrologists, and endocrine surgeons. Moreover, weight-bearing following fracture fixation is critically important to prevent further bone loss, even if PTX has been performed.
Our case report shows the effectiveness of PTX in reducing the risk of fragility fractures and improving BMD and the quality-of-life following surgery. Sufficient weight bearing and PTX are equally important in maintaining BMD. Stress shielding may further aggravate bone loss, even after PTX, as demonstrated in this case. Finally, a multidisciplinary approach involving orthopedists, nephrologists, and endocrine surgeons is required for optimal disease management in this group of patients.
| 1. | Lau WL, Obi Y, Kalantar-Zadeh K. Parathyroidectomy in the Management of Secondary Hyperparathyroidism. Clin J Am Soc Nephrol. 2018;13:952-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 125] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 2. | Geng S, Kuang Z, Peissig PL, Page D, Maursetter L, Hansen KE. Parathyroid hormone independently predicts fracture, vascular events, and death in patients with stage 3 and 4 chronic kidney disease. Osteoporos Int. 2019;30:2019-2025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Christodoulou M, Aspray TJ, Schoenmakers I. Vitamin D Supplementation for Patients with Chronic Kidney Disease: A Systematic Review and Meta-analyses of Trials Investigating the Response to Supplementation and an Overview of Guidelines. Calcif Tissue Int. 2021;109:157-178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 4. | Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl (2011). 2017;7:1-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 761] [Cited by in RCA: 1147] [Article Influence: 143.4] [Reference Citation Analysis (0)] |
| 5. | Rodríguez-Ortiz ME, Rodríguez M. Recent advances in understanding and managing secondary hyperparathyroidism in chronic kidney disease. F1000Res. 2020;9:F1000 Faculty Rev-1077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 6. | Modest JM, Sheth H, Gohh R, Aaron RK. Osteomalacia and Renal Osteodystrophy. R I Med J (2013). 2022;105:22-27. [PubMed] |
| 7. | Torregrosa JV, Bover J, Rodríguez Portillo M, González Parra E, Dolores Arenas M, Caravaca F, González Casaus ML, Martín-Malo A, Navarro-González JF, Lorenzo V, Molina P, Rodríguez M, Cannata Andia J. Recommendations of the Spanish Society of Nephrology for the management of mineral and bone metabolism disorders in patients with chronic kidney disease: 2021 (SEN-MM). Nefrologia (Engl Ed). 2023;43 Suppl 1:1-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 8. | Robertson L, Black C, Fluck N, Gordon S, Hollick R, Nguyen H, Prescott G, Marks A. Hip fracture incidence and mortality in chronic kidney disease: the GLOMMS-II record linkage cohort study. BMJ Open. 2018;8:e020312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Xie L, Hu X, Li W, Ouyang Z. A retrospective study of end-stage kidney disease patients on maintenance hemodialysis with renal osteodystrophy-associated fragility fractures. BMC Nephrol. 2021;22:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Hu L, Napoletano A, Provenzano M, Garofalo C, Bini C, Comai G, La Manna G. Mineral Bone Disorders in Kidney Disease Patients: The Ever-Current Topic. Int J Mol Sci. 2022;23:12223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 58] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 11. | Lundstam K, Heck A, Godang K, Mollerup C, Baranowski M, Pernow Y, Aas T, Hessman O, Rosén T, Nordenström J, Jansson S, Hellström M, Bollerslev J; SIPH Study Group. Effect of Surgery Versus Observation: Skeletal 5-Year Outcomes in a Randomized Trial of Patients With Primary HPT (the SIPH Study). J Bone Miner Res. 2017;32:1907-1914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 12. | Lundstam K, Heck A, Mollerup C, Godang K, Baranowski M, Pernow Y, Varhaug JE, Hessman O, Rosén T, Nordenström J, Jansson S, Hellström M, Bollerslev J; SIPH Study Group. Effects of parathyroidectomy versus observation on the development of vertebral fractures in mild primary hyperparathyroidism. J Clin Endocrinol Metab. 2015;100:1359-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Walton DM, Farrar N, Eichman J, Fuster FJ, Perdue A, Hake M, Ahn J. Disuse Osteopenia Development with Non Weight-Bearing in Lower Extremity Trauma: CT Hounsfield-Unit-Based Analysis. Foot Ankle Orthop. 2022;7:2473011421S0049. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 14. | Pimentel A, Ureña-Torres P, Zillikens MC, Bover J, Cohen-Solal M. Fractures in patients with CKD-diagnosis, treatment, and prevention: a review by members of the European Calcified Tissue Society and the European Renal Association of Nephrology Dialysis and Transplantation. Kidney Int. 2017;92:1343-1355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 149] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 15. | Grygorieva N, Dedukh N, Parubets M, Bystrytska M. Disuse (post-mobilization) osteoporosis: literature review and clinical case series. PJS. 2022;12:94-107. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Silva BC, Bilezikian JP. Parathyroid hormone: anabolic and catabolic actions on the skeleton. Curr Opin Pharmacol. 2015;22:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 355] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 17. | Isaksson E, Ivarsson K, Akaberi S, Muth A, Sterner G, Karl-Göran P, Clyne N, Almquist M. The Effect of Parathyroidectomy on Risk of Hip Fracture in Secondary Hyperparathyroidism. World J Surg. 2017;41:2304-2311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |