Published online Aug 26, 2024. doi: 10.12998/wjcc.v12.i24.5549
Revised: June 9, 2024
Accepted: June 24, 2024
Published online: August 26, 2024
Processing time: 86 Days and 4.1 Hours
Patients with stroke frequently experience pulmonary dysfunction.
To explore the effects of information-motivation-behavioral (IMB) skills model-based nursing care on pulmonary function, blood gas indices, complication rates, and quality of life (QoL) in stroke patients with pulmonary dysfunction.
We conducted a controlled study involving 120 stroke patients with pulmonary dysfunction. The control group received routine care, whereas the intervention group received IMB-model-based nursing care. Various parameters including pulmonary function, blood gas indices, complication rates, and QoL were asse
Baseline data of the control and intervention groups were comparable. Post-inter
IMB model-based nursing care significantly enhanced pulmonary function, improved blood gas indices, reduced complication rates, and improved the QoL of stroke patients with pulmonary dysfunction. Further research is needed to validate these results and to assess the long-term efficacy and broader applicability of the model.
Core Tip: Our study examined the impact of information-motivation-behavioral (IMB) model-based nursing on stroke patients with pulmonary dysfunction. The findings revealed that IMB care significantly improved pulmonary function and blood gas indices, reduced complications, and improved quality of life. The results highlight the potential of the IMB model to transform nursing practice and patient outcomes in cerebrovascular accident rehabilitation.
- Citation: Peng X, Ni HQ, Liu YM, Zhu JL, Bai YT. Information-motivation-behavioral guided nursing for stroke patients with pulmonary dysfunction: A randomized controlled trial. World J Clin Cases 2024; 12(24): 5549-5557
- URL: https://www.wjgnet.com/2307-8960/full/v12/i24/5549.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i24.5549
Stroke, classified as either ischemic or hemorrhagic, is a significant global health burden and a leading cause of long-term disability. The global incidence has witnessed an upward trend, largely attributed to evolving lifestyle factors[1,2]. Is
The information-motivation-behavioral skills (IMB) model of guided nursing care is a promising and innovative approach to address this unmet need. This model, characterized by interventions that involve information, motivation, and behavioral skills, allows comprehensive health guidance. The patient-centric approach ensures superior quality of care and has demonstrated promising results despite its relative novelty in clinical practice[9-11]. Although it has been widely adopted for the management of diverse health conditions, most research on the application of the IMB model involves patients with post-stroke cognitive impairment, post-stroke dysphagia, and cerebral hemorrhage. However, the application and effectiveness of this model in the context of stroke-induced pulmonary dysfunction is underreported[9]. This research gap necessitates further exploration and understanding of how the IMB model can guide nursing care and impact pulmonary function rehabilitation in patients with post-stroke pulmonary dysfunction.
Building on this context, our study aimed to contribute to the ongoing research in this field by investigating the effects of IMB-model-based guided nursing care on pulmonary function rehabilitation in stroke patients. We hypothesized that IMB-model-based guided nursing care would significantly improve pulmonary function, enhance blood gas indices, reduce complication rates, and improve QoL in stroke patients with pulmonary dysfunction. Our findings aim not only to fill the existing research gap, but also to provide valuable clinical insights that can improve nursing practice and patient outcomes in this underserved patient population.
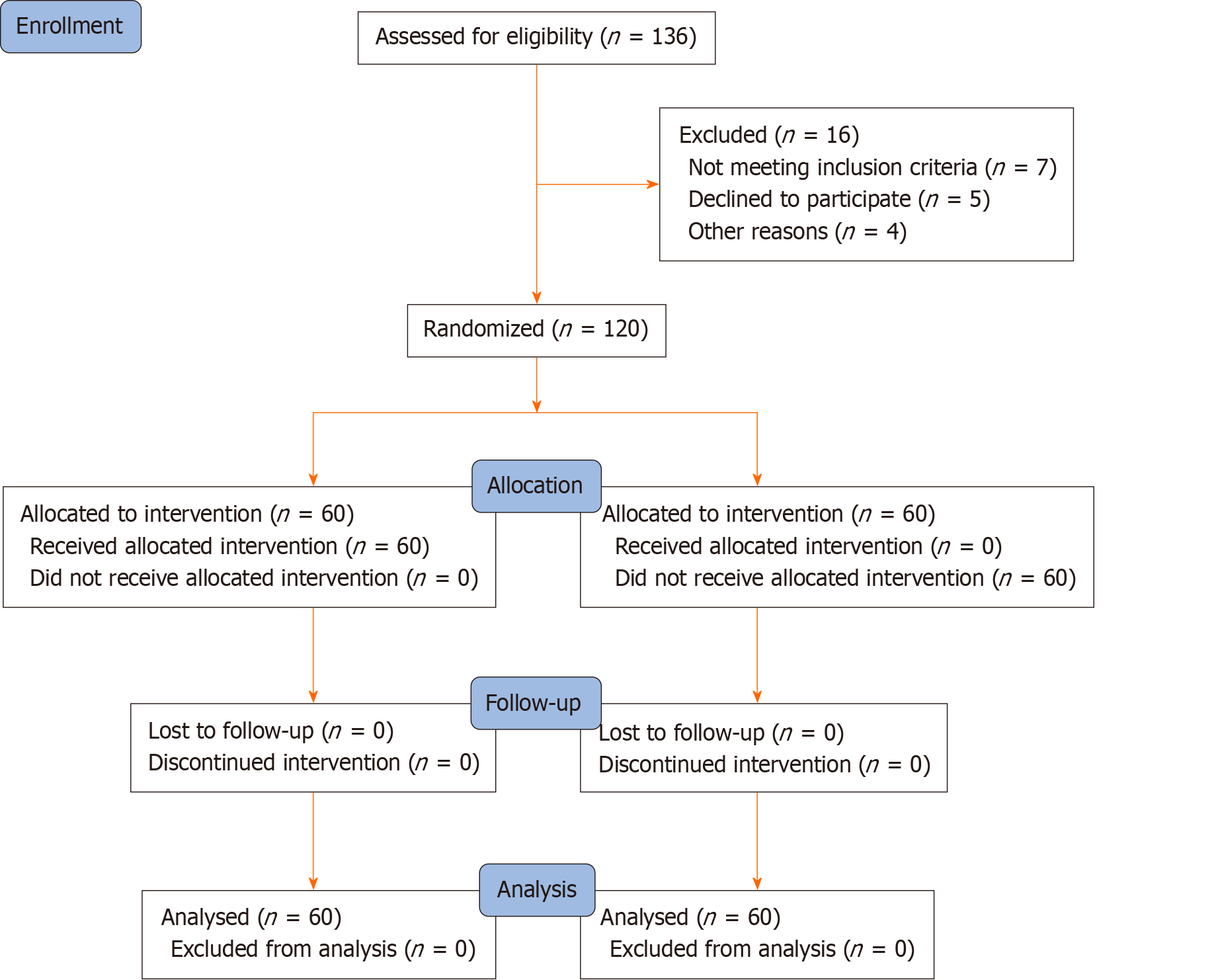
With the approval of the Yancheng First Hospital Affiliated to Nanjing University School of Medicine's Medical Ethics Committee (2021-059), we initiated the process of selecting stroke patients with pulmonary dysfunction treated at the hospital from May 2021 to December 2022 as study participants in this randomized controlled trial. Our inclusion criteria were: (1) Confirmed diagnosis of stroke (including cerebral infarction and cerebral hemorrhage); (2) First episode during the recovery period of stroke; (3) Impaired lung function characterized by notable deviations in parameters such as forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC), especially when considering the FEV1/FVC ratio in relation to established norms from clinical literature on respiratory complications; (4) Clear consciousness; and (5) Voluntary signing of the informed consent form. Potential participants were then assessed for eligibility. Those who met any of the following criteria were excluded: (1) Comorbidity with other severe nervous system disease; (2) Presence of cardiovascular disease; (3) Existing mental disorder; and (4) Inability to communicate normally. Following evaluation and application of the exclusion criteria, 120 eligible patients were randomized a control group and an intervention group, each consisting of 60 patients. Patient selection and allocation are illustrated in Figure 1.
Routine care was administered to the control group and included: (1) Health education and psychological intervention that introduced basic disease knowledge to patients, regularly monitored their emotional state, emphasized the importance of maintaining a positive attitude toward disease improvement, and used verbal soothing techniques to eliminate adverse psychological conditions. Family members were also instructed to encourage the patient to remain optimistic; (2) Dietary guidance by diet plans designed according to the patient's condition, emphasizing dietary restrictions, the importance of nutrition supplementation, and suggesting a light diet; (3) Regular sputum aspiration performed following the doctor's orders was followed by oxygen administration, generally for 2 min; and (4) Turning and. gentle back-tapping by the nursing staff once every 3 h to prevent secondary injuries, each session lasting 5-10 min. This was done 30 min before meals or 2 h after meals. The care was provided throughout the hospital stay.
The intervention group was given an IMB-model-based nursing intervention that included: (1) An informational intervention during which the medical staff engaged in regular communication with patients and their families, emphasizing targeted health education. The educational approach systematically addressed the etiology, clinical manifestations, risks, and preventive measures associated with post-stroke pulmonary dysfunction. Special emphasis was given to precautions during hospitalization and post-discharge. Guidance was also provided on adapting to a suitable lifestyle, dietary habits, the medication regimen, and engaging in respiratory muscle training exercises, including inspiratory muscle training and breathing retraining[5]; (2) A motivational intervention performed by nurses who int
The primary observational indicators were: (1) Pulmonary function indicators, including FEV1, FVC, and peak expiratory flow (PEF) measured both before and after nursing care using a SENSOR MEDIC-6200 volumetric scanner; (2) Blood gas analysis by arterial oxygen pressure (PaO2), arterial oxygen saturation (SaO2), and arterial carbon dioxide pressure (PaCO2) measured before and after nursing care using a Medica blood gas analyzer, (3) Complications that occurred during the hospital stay; (4) QoL was assessed by the SF-36 scale before and after nursing care; and (5) Nursing sa
Statistical analysis was performed using IBM SPSS Windows version 26.0. Quantitative data were reported as means ± SD, and between-group comparisons were made using independent sample t-tests. For categorical data, between-group comparisons of proportions between were performed using the χ2 test. Ranked data were analyzed using the Wilcoxon rank-sum test for two independent samples. Statistical significance was set at P < 0.05.
Our study included 120 stroke patients with pulmonary dysfunction. The patients were divided into observation and control groups of 60 each. The baseline data were similar, with the study groups well matched in age (P = 0.588), body mass index (P = 0.823), stroke duration (P = 0.885), pulmonary dysfunction duration (P = 0.941), and years of education (P = 0.759), ensuring between-group comparability. There were no statistically significant between-group differences of the baseline data (P > 0.05) (Table 1).
| Group | Number of cases | Sex, male/female | Age, years | Body mass index | Stroke duration, days | Pulmonary dysfunction duration, days | Education years |
| Intervention | 60 | 32/28 | 68.60 ± 5.77 | 24.89 ± 3.57 | 28.64 ± 3.57 | 25.58 ± 2.23 | 9.32 ± 1.26 |
| Control | 60 | 35/25 | 68.90 ± 5.88 | 25.01 ± 3.65 | 28.70 ± 3.62 | 25.73 ± 2.29 | 9.37 ± 1.30 |
| t value | - | 0.349 | 0.266 | 0.19 | 0.096 | 0.355 | 0.16 |
| P value | - | 0.588 | 0.823 | 0.885 | 0.941 | 0.759 | 0.494 |
Before the nursing intervention, there were no significant differences (P > 0.05) between the observation and control groups in terms of pulmonary function indicators, such as FVC, FEV1, and PEF. The measurements showed post-intervention improvement of FVC, FEV1, and PEF in both groups. However, the improvement in all three parameters was significantly greater in the intervention group than in control group (P < 0.001). This reveals the effectiveness of the nursing intervention, particularly in the intervention group, in enhancing pulmonary function. The results are shown in Table 2.
| Group | Number of cases | FVC pre-intervention, L | FVC post-intervention, L | FEV1 pre-intervention, L | FEV1 post-intervention, L | PEF pre-intervention, L/s | PEF post-intervention, L/s |
| Intervention | 60 | 2.38 ± 0.19 | 3.78 ± 0.25 | 1.78 ± 0.16 | 3.26 ± 0.19 | 5.27 ± 0.32 | 7.25 ± 0.25 |
| Control | 60 | 2.42 ± 0.21 | 3.07 ± 0.22 | 1.80 ± 0.19 | 2.28 ± 0.16 | 5.24 ± 0.36 | 5.83 ± 0.23 |
| t value | - | 0.868 | 16.605 | 0.665 | 30.908 | 0.499 | 32.288 |
| P value | - | 0.43 | < 0.001 | 0.553 | < 0.001 | 0.665 | < 0.001 |
Table 3 is a comparative analysis of the blood gas indicators in the observation and control groups, both pre- and post-nursing interventions. It shows improvement of PaO2, PaCO2, and oxygen saturation SaO2 in both groups following the intervention. The intervention group had significant post-intervention increases of PaO2 and SaO2 and a decrease in PaCO2 compared with the control group. These differences were statistically significant, suggesting that the nursing intervention had a more substantial positive effect on the blood gas parameters in the intervention group.
| Group | Number of cases | PaO2 pre-intervention, mmHg | PaO2 post-intervention, mmHg | PaCO2 pre-intervention, mmHg | PaCO2 post-intervention, mmHg | SaO2 pre-intervention, % | SaO2 post-intervention, % |
| Intervention | 60 | 61.32 ± 6.35 | 79.21 ± 5.16 | 73.52 ± 5.46 | 58.14 ± 6.10 | 76.70 ± 7.15 | 93.66 ± 7.71 |
| Control | 60 | 61.24 ± 6.31 | 62.96 ± 5.34 | 73.60 ± 5.54 | 73.07 ± 5.84 | 77.34 ± 7.11 | 86.79 ± 7.62 |
| t value | - | 0.074 | 17.061 | 0.084 | 13.77 | 0.495 | 4.93 |
| P value | - | 0.941 | < 0.001 | 0.933 | < 0.001 | 0.671 | < 0.001 |
The monitored complications included aspiration, pulmonary atelectasis, pulmonary infection, and shoulder-hand syndrome. Following the nursing intervention, the intervention group experienced fewer complications than the control group, with overall incidence rates of 6.67% and 23.33%, respectively. This finding highlights the efficacy of nursing interventions in reducing the occurrence of complications, thereby enhancing patient care and recovery (Table 4).
| Group | Cases, n | Aspiration | Pulmonary atelectasis | Pulmonary infection | Shoulder-Hand syndrome | Total cases | Incidence rate, % |
| Intervention | 60 | 2 | 1 | 1 | 0 | 4 | 6.67 |
| Control | 60 | 3 | 3 | 2 | 6 | 14 | 23.33 |
Table 5 shows the quality of life scores across eight different domains of patients in the observation and control groups before and after nursing care. Each domain was considered as pre- and post-nursing care. After the nursing intervention, the intervention group scores in all domains were significantly improved compared with the control group. This suggests the effectiveness of nursing care in enhancing patient QoL in various aspects, further highlighting the benefits of such interventions.
| Group | Cases, n | Physical function | Social function | Mental health | Physiological role | Body pain | Energy | Emotional role | General health status | ||||||||
| Before | After | Before | After | Before | After | Before | After | Before | After | Before | After | Before | After | Before | After | ||
| Intervention | 60 | 55.50 ± 4.15 | 78.05 ± 4.52 | 53.55 ± 4.89 | 77.30 ± 5.11 | 54.25 ± 4.94 | 78.35 ± 5.00 | 56.65 ± 4.10 | 78.76 ± 4.80 | 56.60 ± 4.24 | 80.12 ± 4.60 | 54.30 ± 4.93 | 79.30 ± 5.14 | 55.45 ± 4.95 | 78.80 ± 4.85 | 56.70 ± 4.08 | 79.05 ± 4.70 |
| Control | 60 | 55.46 ± 4.22 | 67.70 ± 4.56 | 53.81 ± 4.95 | 66.82 ± 5.40 | 54.58 ± 5.15 | 67.85 ± 5.00 | 56.90 ± 4.30 | 69.33 ± 4.60 | 56.05 ± 4.32 | 68.30 ± 4.56 | 53.90 ± 4.97 | 66.70 ± 5.25 | 55.60 ± 5.07 | 69.47 ± 5.00 | 56.98 ± 4.18 | 70.05 ± 4.60 |
| t value | 0.049 | 13.061 | 0.27 | 10.6 | 0.332 | 10.994 | 0.308 | 11.68 | 0.648 | 14.21 | 0.402 | 12.511 | 0.151 | 10.8 | 0.331 | 10.09 | |
| P value | 0.961 | 0 | 0.788 | 0 | 0.741 | 0 | 0.759 | 0 | 0.518 | 0 | 0.689 | 0 | 0.881 | 0 | 0.741 | 0 | |
This study introduced a novel IMB-model-based nursing intervention tailored specifically for stroke patients with pulmonary dysfunction. It distinguished itself by systematically incorporating informational, motivational, and behavioral strategies. Our findings demonstrate that this comprehensive approach significantly improved pulmonary function and QoL compared to conventional care. Particularly noteworthy is the substantial enhancement of FEV1, FVC, and PEF values in the intervention group, which are crucial metrics for assessing pulmonary efficacy. Additionally, our intervention notably reduced the incidence of common complications such as aspiration and pulmonary atelectasis, further underlining its potential to mitigate secondary health issues frequently encountered in post-stroke management. These results underscore the pivotal role of structured nursing interventions in the rehabilitation of stroke patients and highlight the potential for significant improvement of clinical outcomes, emphasizing the need for their integration into routine clinical practice. This study not only fills a critical gap in stroke rehabilitation but also sets a foundation for future research to explore the longitudinal impact of such interventions on the trajectory of patient recovery.
Stroke is a cerebrovascular event of profound medical significance that occurs with varying degrees of severity in affected individuals. The dysfunctions span limb motor impairment, linguistic incapability, and cognitive deficits, which in turn impose a significant burden on patient QoL and elevate the responsibilities shouldered by their caregivers[12]. The ongoing clinical quest for effective treatment modalities for stroke encompasses two main categories: Conservative management and surgical intervention. The selection of these therapeutic strategies depends on an individual patient-specific clinical profiles. Stroke patients often present with severe and complex disease manifestations, harboring high risks even with immediate medical rescue. Despite expedited treatment, a large proportion of stroke survivors encounter numerous complications, aggravating their condition and undermining their prognosis[13,14].
In this context, high-quality nursing services have been recognized as significant contributors to improved treatment outcomes and improve disease conditions in stroke patients[15]. Therefore, it is imperative that the role of nursing services in treating these patients should be thoroughly emphasized. One commonly associated complication in post-stroke patients is cardiopulmonary functional impairment, with pulmonary dysfunction playing a significant role in overall morbidity[16,17]. This functional limitation often affects physical ability, hinders daily activity, and consequently has a substantial negative impact on their QoL, which increases their psychological distress. For stroke survivors with pulmonary dysfunction, interventions, including respiratory training, aerobic exercise in conjunction with isotonic limb muscle training, abdominal breathing training, and combined respiratory muscle-swallowing training, have been re
The IMB model-based nursing paradigm, characterized by a shift from a disease-centric to a patient-centric approach, marks a transformative phase in the healthcare of stroke patients with pulmonary dysfunction. This innovative model emphasizes the delivery of high-quality nursing services during hospitalization, thereby enhancing the patient’s con
The key findings of our study highlight the potential benefits of implementing the IMB skills model in nursing care for post-stroke patients with pulmonary dysfunction. The empirical evidence we accumulated points to the effectiveness of the model in fostering marked enhancement of pulmonary function and blood gas analysis indices. These improvements are not merely statistical figures; they represent substantial health advancements for patients who, in the aftermath of stroke, deal with complex and debilitating pulmonary dysfunction. The positive outcomes that we observed can be largely credited to the unique aspects of the IMB model, which includes informational and motivational interventions together with the development of key behavioral skills. The informational aspect of the IMB model empowers patients by providing comprehensive, comprehensible, and actionable health information. This approach aims to equip patients with knowledge about their condition, the importance of adhering to prescribed treatments, and the potential consequences of noncompliance.
Meanwhile, motivational interventions facilitate patients' internalization of the value and critical need to maintain their health and adhere to the prescribed regimen. These motivational interventions, which often involve counseling and emotional support, help patients foster the motivation to make positive health decisions. Behavioral skills interventions, the final component of the IMB model, focus on enhancing patients' capabilities to carry out necessary actions for their health maintenance. This might involve teaching them how to use medical equipment, adhere to medication schedules, or perform physical exercise. Our research further demonstrates that IMB-model-based nursing care significantly reduces the complication rates in patients. This reduction in complications can be seen as a testament to the IMB model's effectiveness as a proactive approach that not only manages the patient’s existing conditions but also pre-empts potential complications. An additional significant finding of our study was the apparent beneficial effect of the IMB model on the QoL of patients. The model's emphasis on the psychological health of patients, its focus on mitigating negative emotions, and its efforts to boost the physical capabilities all contribute to enhancing QoL. This improved QoL is vital because it allows patients to regain a semblance of normalcy in their post-stroke, lives, enabling them to more effectively reintegrate into society.
Despite these promising results, our study had several limitations. The findings were influenced by specific geographic and healthcare contexts that may have affected generalizability. The sample was relatively small and the follow-up duration was short, which means that the long-term effects of the IMB model remain unclear. We also primarily focused on quantitative health outcomes by downplaying the subjective experience of patients with the IMB model. These areas underline the necessity for more comprehensive research to validate our findings and assess the full potential of the IMB model in various contexts.
In conclusion, this study suggests that IMB model-based nursing care effectively enhanced pulmonary function, impro
We are grateful to the participants of this study for providing informed consent and enabling this study. We also extend our appreciation to the Yancheng First Hospital Affiliated to Nanjing University School of Medicine for their comprehensive review and endorsement of our study procedures. Their guidance was instrumental in ensuring that the study adhered to the highest ethical standard.
| 1. | Feigin VL, Norrving B, Mensah GA. Global Burden of Stroke. Circ Res. 2017;120:439-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1022] [Cited by in RCA: 1348] [Article Influence: 168.5] [Reference Citation Analysis (0)] |
| 2. | Hostettler IC, Seiffge DJ, Werring DJ. Intracerebral hemorrhage: an update on diagnosis and treatment. Expert Rev Neurother. 2019;19:679-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 195] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 3. | Feske SK. Ischemic Stroke. Am J Med. 2021;134:1457-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 426] [Article Influence: 106.5] [Reference Citation Analysis (0)] |
| 4. | Tjahjadi M, König R, Wirtz CR, Woischneck D, Kapapa T. Cerebral vasospasm and health-related quality of life after subarachnoid hemorrhage. World Neurosurg. 2013;80:113-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Sutbeyaz ST, Koseoglu F, Inan L, Coskun O. Respiratory muscle training improves cardiopulmonary function and exercise tolerance in subjects with subacute stroke: a randomized controlled trial. Clin Rehabil. 2010;24:240-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 118] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Battaglini D, Robba C, Lopes da Silva A, Dos Santos Samary C, Leme Silva P, Dal Pizzol F, Pelosi P, Rocco PRM. Brain-heart interaction after acute ischemic stroke. Crit Care. 2020;24:163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 7. | Spruit MA. Pulmonary rehabilitation. Eur Respir Rev. 2014;23:55-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Liaw MY, Hsu CH, Leong CP, Liao CY, Wang LY, Lu CH, Lin MC. Respiratory muscle training in stroke patients with respiratory muscle weakness, dysphagia, and dysarthria - a prospective randomized trial. Medicine (Baltimore). 2020;99:e19337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 9. | Kim SR, Kim S, Kim HY, Cho KH. Predictive Model of Self-management in Patients With Stroke Based on the Information-Motivation-Behavioral Skills Model. J Cardiovasc Nurs. 2023;38:158-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | You H, Wang YY, Zhang C, Walker AN, Ge JJ, Zhao SQ, Peng XQ. Empirical validation of the information-motivation-behavioral skills model of gestational weight management behavior: a framework for intervention. BMC Public Health. 2023;23:130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 11. | Lim KE, Kim SR, Kim HY, Kim SR, Lee YC. Self-management model based on information-motivation-behavioral skills model in patients with chronic obstructive pulmonary disease. J Adv Nurs. 2022;78:4092-4103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Cai W, Zhang K, Li P, Zhu L, Xu J, Yang B, Hu X, Lu Z, Chen J. Dysfunction of the neurovascular unit in ischemic stroke and neurodegenerative diseases: An aging effect. Ageing Res Rev. 2017;34:77-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 213] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 13. | Markus HS, Michel P. Treatment of posterior circulation stroke: Acute management and secondary prevention. Int J Stroke. 2022;17:723-732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 14. | Muresanu DF, Strilciuc S, Stan A. Current Drug Treatment of Acute Ischemic Stroke: Challenges and Opportunities. CNS Drugs. 2019;33:841-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 15. | Camicia M, Lutz B, Summers D, Klassman L, Vaughn S. Nursing's Role in Successful Stroke Care Transitions Across the Continuum: From Acute Care Into the Community. Stroke. 2021;52:e794-e805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Dreyer P, Angel S, Langhorn L, Pedersen BB, Aadal L. Nursing Roles and Functions in the Acute and Subacute Rehabilitation of Patients With Stroke: Going All In for the Patient. J Neurosci Nurs. 2016;48:108-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Aadal L, Angel S, Dreyer P, Langhorn L, Pedersen BB. Nursing roles and functions in the inpatient neurorehabilitation of stroke patients: a literature review. J Neurosci Nurs. 2013;45:158-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Pitthayapong S, Thiangtam W, Powwattana A, Leelacharas S, Waters CM. A Community Based Program for Family Caregivers for Post Stroke Survivors in Thailand. Asian Nurs Res (Korean Soc Nurs Sci). 2017;11:150-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Ugur HG, Erci B. The Effect of Home Care for Stroke Patients and Education of Caregivers on the Caregiver Burden and Quality of Life. Acta Clin Croat. 2019;58:321-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |