Published online Aug 26, 2024. doi: 10.12998/wjcc.v12.i24.5483
Revised: June 3, 2024
Accepted: June 26, 2024
Published online: August 26, 2024
Processing time: 80 Days and 0.4 Hours
Radical surgery is a preferred treatment for colorectal carcinoma, wherein nursing intervention is essential for postoperative recovery and prevention of compli
To investigate the influence of humanistic care-based operating room nursing on the safety, postoperative recovery, and nursing satisfaction of patients who have undergone radical surgery for colorectal carcinoma.
In total, 120 patients with rectal cancer who underwent surgery in Zhongnan Hospital of Wuhan University between August 2023 and March 2024 were se
During emergence from anesthesia, SBP, DBP, and BPM levels were found to be lower in the research group than those in the control group, also serum Cor, AD, and NE levels were lower. In addition, the research group had shorter operative, awakening, anal exhaust, first postoperative ambulation, drainage tube removal, intestinal re
Humanistic care-based operating room nursing can mitigate physiological stress responses, reduce postoperative complications, promote postoperative recovery, relieve adverse psychological emotions, and enhance life hope and nursing satisfaction in patients undergoing radical surgery for colorectal carcinoma, which can be popularized in clinical practice.
Core Tip: Currently, no clinical studies have reported the application of humanistic care-based operating room nursing in patients who underwent radical surgery for colorectal carcinoma. This study explored the impact of humanistic care-based operating room nursing on the physiological stress, postoperative recovery, and nursing satisfaction of such patients. The results revealed that humanistic care-based operating room nursing can significantly relieve patients’ physiological stress responses, reduce postoperative complications, promote postoperative recovery, alleviate negative psychological emotions, and increase life hope and nursing satisfaction. This indicated promising clinical promotion value of this nursing model.
- Citation: Wang XP, Niu M. Influence of humanistic care-based operating room nursing on safety, recovery, and satisfaction after radical surgery for colorectal carcinoma. World J Clin Cases 2024; 12(24): 5483-5491
- URL: https://www.wjgnet.com/2307-8960/full/v12/i24/5483.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i24.5483
Colorectal carcinoma (CRC) is one of the most common gastrointestinal malignancies, with nearly 1.8 million new cases and 881000 related deaths worldwide, accounting for approximately 10% of cancer-related deaths[1]. As a CRC subtype, rectal cancer accounts for one-third of newly diagnosed CRC cases annually[2]. The etiology of rectal cancer is currently unknown; however, it may be related to environmental factors, eating habits, and genetic factors[3]. Currently, surgical treatment remains the first choice for rectal cancer treatment. However, because of varying degrees of pain, vomiting, dizziness, anxiety, depression, and fear perioperatively, patients’ ability to cope with cancer and compliance with treat
Traditional nursing is mainly disease-centered, lacking planning, pertinence, and enthusiasm, resulting in difficulty in meeting people’s increasingly demanding nursing needs. In this context, several new patient-centered nursing models have emerged and have achieved better nursing quality than traditional nursing in various nursing settings, demon
In this study, 120 patients who underwent surgery for rectal cancer at our hospital were collected and grouped into receiving routine operating room nursing or humanistic care-based nursing. The application value of humanistic care-based operating room nursing in rectal cancer surgery was evaluated by comparing physiological stress, postoperative recovery, emotions, and complications between the two groups.
A total of 120 patients with rectal cancer who underwent surgery at Zhongnan Hospital of Wuhan University between January 2023 and January 2024 were included in the study. They were grouped based on differences in nursing moda
Treatment-naive patients (aged 18–70 years) who were diagnosed with rectal cancer by digital rectal examination, pa
The control group received routine care, which included basic nursing services as instructed by the doctor, vital sign monitoring, infusion care, medication care, scheduled patrols, and dietary guidance.
The research group received humanistic care-based operating room nursing, as specified below:
Strengthening preoperative inspection: The medical staff assessed patients’ vital signs, understood their past medical history, understood the specific conditions, and developed individualized nursing plans according to the actual patient situation. To enhance patients’ rehabilitation beliefs and compliance behaviors and improve their cooperation with treat
Strengthening preoperative preparation: The operating bed was preheated 30 min before surgery, and the temperature and humidity in the operating room were adjusted reasonably. To eliminate the patient’s nervousness about the unfa
Enhancing intraoperative care: To reduce patients’ fear of medical procedures, nurses explained the purpose of each procedure before the administration of anesthesia. During anesthesia, nurses gently held the patient’s hands or shoulders, gave him/her spiritual comfort, and distracted his/her attention via conversation to ensure smooth completion of the process. Regarding body positioning, nurses moved the patient gently to ensure patient comfort. Intraoperatively, pressure sores were prevented by cotton pads, and insulation measures were taken by covering patients with heated blankets, reducing unnecessary exposure, and heating the infusion liquid. Aseptic operation was performed in strict accordance with the specific operating room requirements during the procedure. Nurses also closely monitored the changes in patients’ vital signs and reported them to doctors on time during emergencies such as dyspnea or increased heart rate. During surgery, the nursing staff closely cooperated with the physicians to execute surgery-related care, such as assisting the physicians in providing the operation-related equipment and removing related obstacles affecting the surgical process.
Strengthening postoperative care: Postoperatively, nurses adjusted the patient to a comfortable position, encouraged him/her to exercise according to the recovery status, and massaged his/her limbs regularly to prevent lower limb venous thrombosis. Strict postoperative nursing care of the indwelling catheter was also performed. Vital signs of the patients were monitored in real time to avoid risk factors leading to incisional infection. Patients were allowed to eat liquid food rather than solid when intestinal peristalsis was not restored, and small and frequent meals were advocated after re
Vital signs, including systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart beats per minute (BPM), were recorded. Venous blood was collected before and during emergence from anesthesia and centrifuged to collect se
The operative, awakening, anal exhaust, first postoperative ambulation, drainage tube removal, intestinal function recovery, and hospitalization times were recorded. The occurrence of common complications such as infection, agitation, anastomotic fistula, nausea and vomiting, and ileus were also recorded.
Changes in negative emotions before and after nursing interventions were assessed using the Self-rating Depression/Anxiety Scale (SDS/SAS). The SDS consists of 20 items using a 4-point scale. Higher SDS and SAS scores indicate severe depression and anxiety.
The Herth Hope Index (HHI) was used in life hope assessment of patients. The scale is divided into three dimensions: Temporality and future, positive readiness and expectancy, and interconnectedness, each with four items scored on a 4-point scale. With a total score ranging 12–48, a higher score indicated a higher degree of hope. Scores of 12–23, 24–35, and 36–48 points indicate a low, moderate, and high level of hope, respectively.
Nursing satisfaction surveys were used to assess patients’ satisfaction with nursing tasks, which were divided into three levels: Satisfied (high recognition and affirmation), basically satisfied (recognition and affirmation), and dissatisfied (disapproval)[11]. Satisfaction = (very satisfied cases + basically satisfied cases)/total number of cases × 100%.
Statistical analysis and image rendering of data was conducted using SPSS 21.0 and GraphPad Prism 6, respectively. Chi-square or Fisher’s exact test was used to compare the counting data. The Kolmogorov-Smirnov test was used to analyze the distribution of continuous data, in which normally distributed data were described as the mean ± SD. Independent samples t-test (two-tailed) was used for intergroup comparisons of measurement data and paired t-test (two-tailed) for intragroup comparisons between different periods, with P < 0.05 representing statistical significance.
No significant differences were found in terms of sex, age, eating habits, working status, education level, ASA grade, TNM stage, pathological type, and other general clinical data between the two groups (P > 0.05) (Table 1).
| Groups | Control group (n = 55) | Research group (n = 65) | χ2/t | P value |
| Age (years) | 51.23 ± 11.28 | 54.55 ± 10.77 | 1.646 | 0.102 |
| Sex | 0.616 | 0.432 | ||
| Female | 19 (34.55) | 27 (41.54) | ||
| Male | 36 (65.45) | 38 (58.46) | ||
| Eating habits | 0.677 | 0.411 | ||
| Light | 14 (25.45) | 21 (32.31) | ||
| Greasy | 41 (74.55) | 44 (67.69) | ||
| Working status | 0.271 | 0.603 | ||
| Employed | 22 (40.00) | 23 (35.38) | ||
| Unemployed | 33 (60.00) | 42 (64.62) | ||
| Educational level | 0.808 | 0.369 | ||
| ≥ high school | 23 (41.82) | 22 (33.85) | ||
| < high school | 32 (58.18) | 43 (66.15) | ||
| ASA grade | 0.103 | 0.748 | ||
| I | 27 (49.09) | 30 (46.15) | ||
| II | 28 (50.91) | 35 (53.85) | ||
| TNM stage | 0.073 | 0.788 | ||
| T1 | 19 (34.55) | 24 (36.92) | ||
| T2 | 36 (65.45) | 41 (63.08) | ||
| Pathological type | 0.809 | 0.667 | ||
| Papillary adenocarcinoma | 29 (52.73) | 37 (56.92) | ||
| Tubular adenocarcinoma | 16 (29.09) | 20 (30.77) | ||
| Mucinous adenocarcinoma | 10 (18.18) | 8 (12.31) |
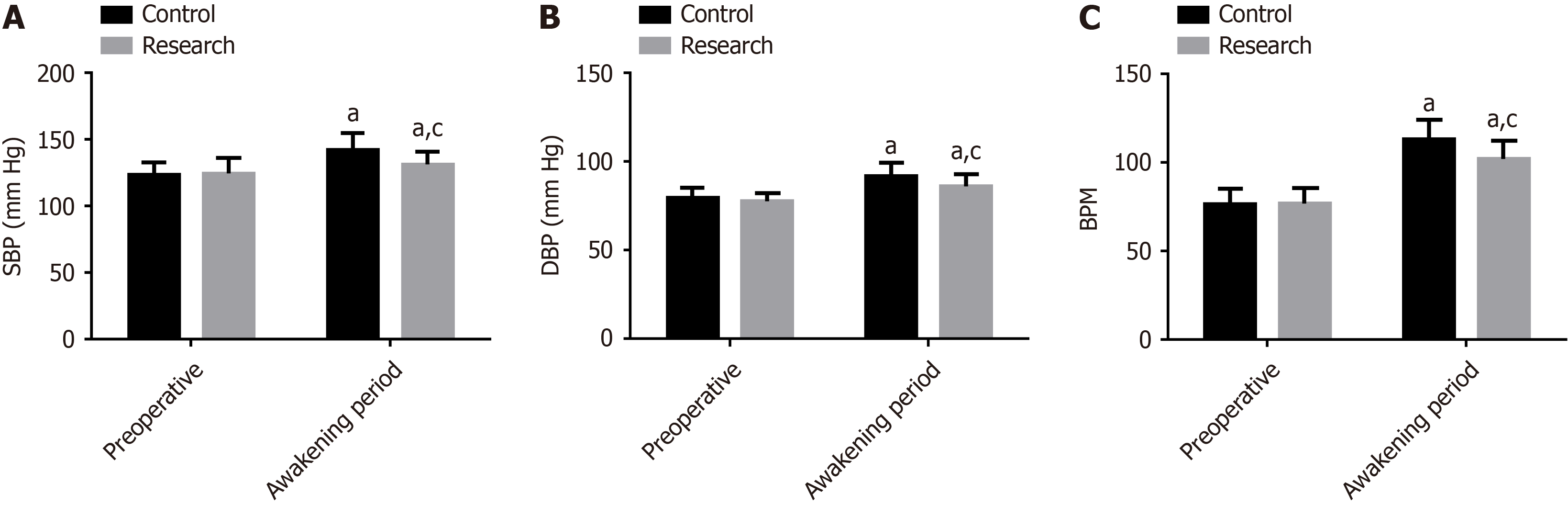
Preoperative SBP, DBP, and BPM were comparable between the groups (P > 0.05). Postoperative SBP, DBP, and BPM significantly increased in both groups, with levels lower in the research group than in the control group (P < 0.05) (Figure 1).
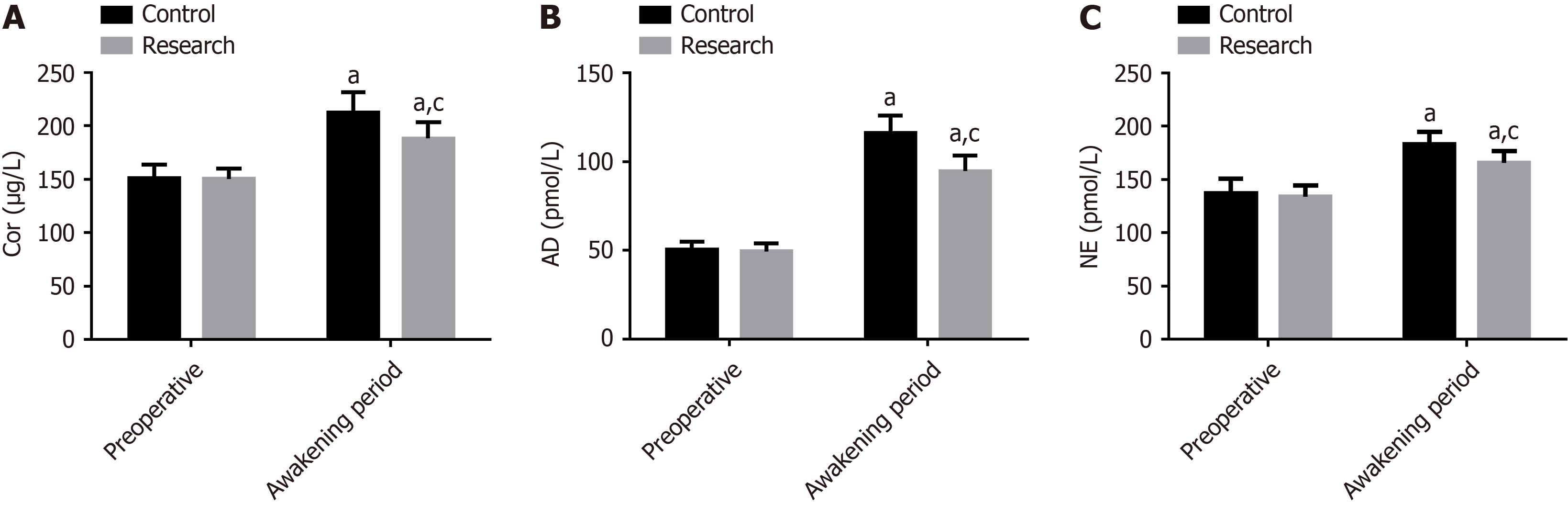
No significant intergroup differences were found in the preoperative levels of Cor, AD, and NE (P > 0.05). Compared with the preoperative values, preoperative Cor, AD, and NE levels increased markedly in both groups, with lower levels in the research group than that in the control group (P < 0.05) (Figure 2).
Compared with the control group, research group had shorter operative, awakening, anal exhaust, first postoperative ambulation, drainage tube removal, intestinal function recovery, and hospitalization times (P < 0.05) (Table 2).
| Groups | Control group (n = 55) | Research group (n = 65) | χ2 | P value |
| Operation time (min) | 54.91 ± 9.08 | 47.95 ± 7.23 | 4.673 | < 0.001 |
| Awakening time (h) | 34.05 ± 6.30 | 27.26 ± 4.68 | 6.762 | < 0.001 |
| Anal exhaust time (h) | 19.16 ± 4.16 | 15.28 ± 3.77 | 5.357 | < 0.001 |
| First postoperative ambulation time (h) | 8.42 ± 2.64 | 7.14 ± 2.28 | 2.850 | 0.005 |
| Drainage tube removal time (h) | 6.16 ± 1.41 | 5.35 ± 1.87 | 2.639 | 0.009 |
| Intestinal function recovery time (h) | 28.22 ± 5.56 | 22.85 ± 5.65 | 5.226 | < 0.001 |
| Hospitalization time (d) | 8.73 ± 2.74 | 7.57 ± 2.38 | 2.482 | 0.015 |
Postoperative complications were recorded in both groups. In the control group, 2 cases of infection, 4 of agitation, 1 of anastomotic fistula, 6 of nausea and vomiting, and 2 of ileus were recorded, with a total incidence of 27.27%. In the research group, only 1 case of infection, 4 of nausea and vomiting, and 1 of ileus were noted, with an overall incidence of 9.23%. The research group had a lower total complication rate than that of the control group (P < 0.05) (Table 3).
| Groups | Control group (n = 55) | Research group (n = 65) | t | P value |
| Infection | 2 (3.64) | 1 (1.54) | - | - |
| Agitation | 4 (7.27) | 0 | - | - |
| Anastomotic fistula | 1 (1.82) | 0 | - | - |
| Nausea and vomiting | 6 (10.91) | 4 (6.15) | - | - |
| Ileus | 2 (3.64) | 1 (1.54) | - | - |
| Total incidence | 15 (27.27) | 6 (9.23) | 6.717 | 0.010 |
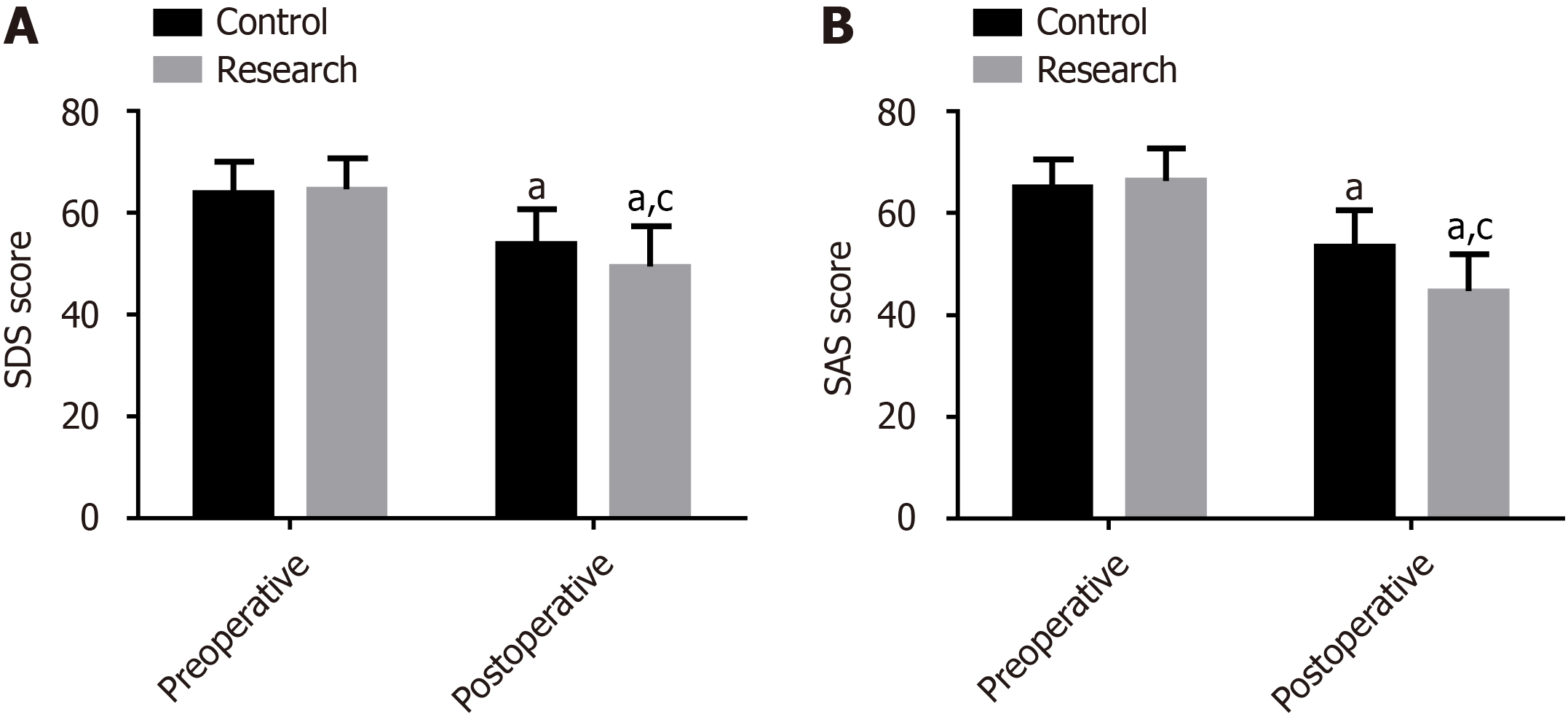
The preoperative SDS and SAS scores were comparable between the groups (P > 0.05). Compared with preoperative scores, the scores on both scales reduced statistically after surgery, particularly in the research group (P < 0.05) (Figure 3).
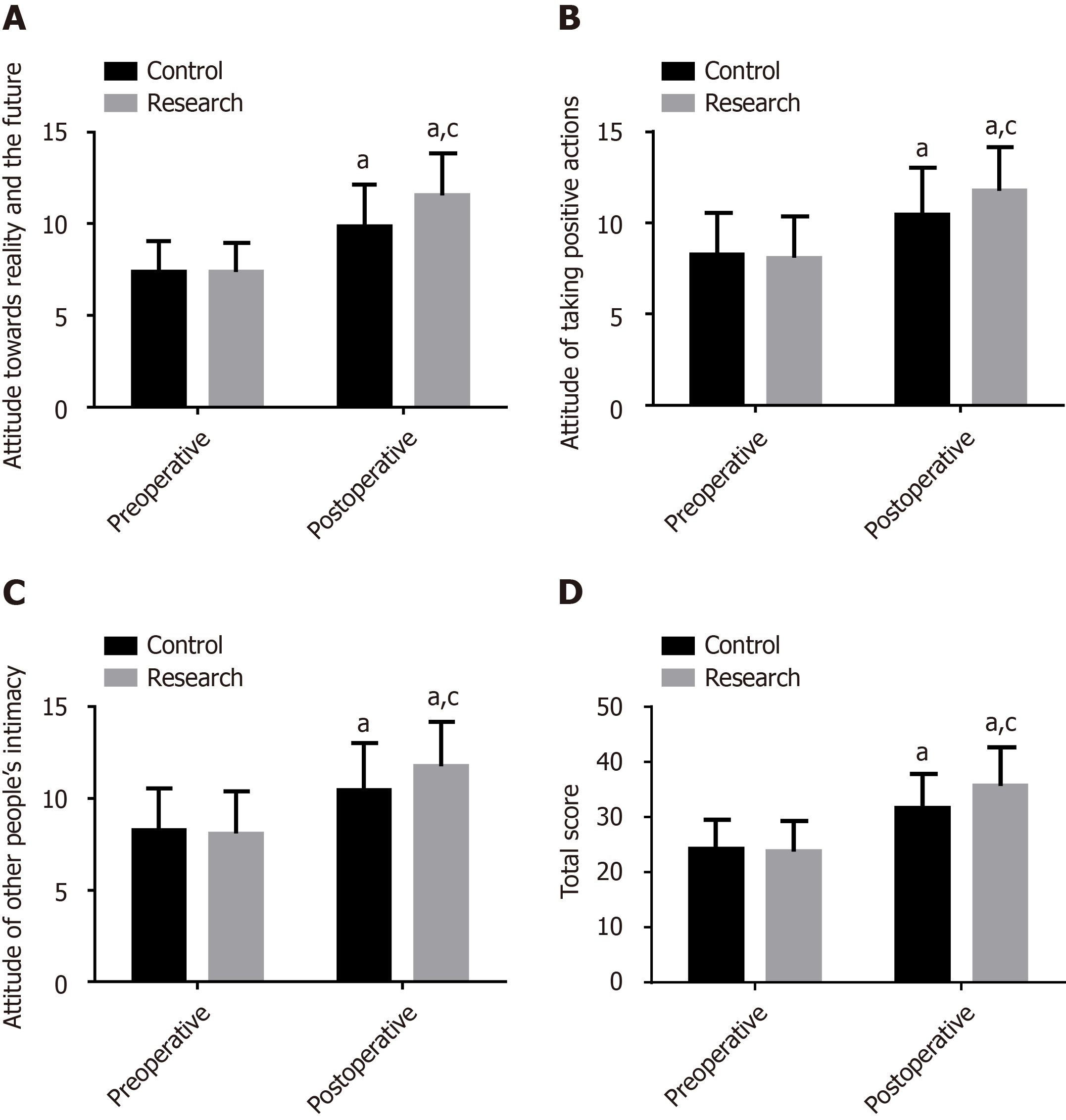
The two groups showed no notable differences in the scores of various dimensions of the HHI scale and the total score (P > 0.05). Both groups had high HHI scores after surgery, in terms of each dimension or the overall scale, with even more noticeable increases in the research group (P < 0.05) (Figure 4).
In the analysis of patient nursing satisfaction, the satisfaction rate (76.36%) of the control group was significantly lower (95.38%) than that of the research group (P < 0.05) (Table 4).
| Groups | Control group (n = 55) | Research group (n = 65) | χ2 | P value |
| Satisfied | 12 (21.82) | 30 (46.15) | - | - |
| Basically satisfied | 30 (54.55) | 32 (49.23) | - | - |
| Dissatisfied | 13 (23.64) | 3 (4.62) | - | - |
| Overall satisfaction | 42 (76.36) | 62 (95.38) | 9.328 | 0.002 |
Compared with other surgeries, tumor resection is characterized by great trauma, complex procedure, and long duration; hence, increased assistance of nurses is required. Most current nursing tasks in the operating room involve functional nursing, focusing on simply caring for diseases, which makes it difficult to meet the diverse needs of patients[12]. Huma
Rectal cancer is a major digestive disorder, and the inevitable mechanical stimulation during abdominal surgery, severe pain at the end of anesthesia, and adverse emotions can excite the sympathetic nervous system, triggering stress reactions, hindering gastrointestinal peristalsis, and making it impossible for patients to exhaust and defecate normally[16-18]. If the condition worsens, flatulence, intestinal adhesion, abdominal wall adhesion, and even intestinal infarction may occur, thereby endangering the patient’s life. Previous studies have shown that reducing the perioperative stress response of patients undergoing radical surgery for CRC is conducive to gastrointestinal function recovery[19]. Intraoperative hypothermia may cause sympathetic nerve excitement, resulting in intraoperative hemodynamic fluctuations. In addition, hypothermia is associated with various adverse effects, such as increased infection risk, prolonged hospitalization, high healthcare costs, and coagulopathy[20]. Therefore, individualized psychological care can effectively alleviate patients’ negative psychological emotions, enhance their confidence in facing diseases, and reduce their psychological stress responses[21]. Considering that patients may have poor surgical outcomes because of physiological or psychological stress, they require psychological support and intraoperative thermal insulation measures.
The results of this study showed that compared with the patients of the control group, patients of research group had more stable vital signs during emergence from anesthesia, better serum stress response levels, shorter operative and postoperative recovery times, greater relief of negative emotions, and lower overall complication rates.
Rectal cancer is a life-threatening condition that predisposes patients to severe psychological stress and significant changes in lifestyle and habits postoperatively. Patients are susceptible to negative emotions such as depression and anxiety[22], adversely affecting their physiology, immunity, and social activities if not tended to properly[23]. Mean
This study has some limitations that must be addressed. First, the sample size was small, which led to statistical calculations when comparing some results. Second, each operating room did not have the same nursing team; the professional ability of nurses may be different, which may affect the quality of care to varying degrees. Third, the long-term postoperative recovery of the patients was not assessed because of the short research period. Hence, in-depth and com
In summary, humanistic care-based operating room nursing has high application value in radical surgery for rectal cancer, which can mitigate negative emotions, facilitate postoperative recovery, reduce postoperative complications, and improve the life hope and nursing satisfaction of patients, with high clinical promotion value.
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64542] [Article Influence: 16135.5] [Reference Citation Analysis (176)] |
| 2. | Qi X, Lin Y, Liu X, Chen J, Shen B. Biomarker Discovery for the Carcinogenic Heterogeneity Between Colon and Rectal Cancers Based on lncRNA-Associated ceRNA Network Analysis. Front Oncol. 2020;10:535985. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Tang T, Yu S, Song Z, Pan X, Xu F, Wu Y, Zhang L. Comprehensive Analysis of miRNA-Mediated Regulatory Network and Identification of Prognosis Biomarkers in Rectal Cancer. Front Genet. 2022;13:792984. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Ma F, Zhu Y, Liu Y. The relationship between psychological distress and the nursing humanistic care demands in postoperative cancer inpatients: a cross-sectional study. BMC Nurs. 2024;23:26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 5. | Xu Y, Yang J. The effect of 5A nursing combined with psychological nursing on the immune function, cancer-related fatigue and complications of patients undergoing radical resection of colorectal cancer. Cell Mol Biol (Noisy-le-grand). 2022;68:169-176. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Gao M, Wang Y, Lei Y, Zhang L, Li L, Wang C, Liao Y, Liao B. Applying the Carolina care model to improve nurses' humanistic care abilities. Am J Transl Res. 2021;13:3591-3599. [PubMed] |
| 7. | Liu X, Li C, Yan X, Shi B. Psychological capital has a positive correlation with humanistic care ability among nurses. Front Psychol. 2022;13:955627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 8. | Xu H, Xu G, Liu Y, Mu X, Liu Y, Hu H. Effect of Narrative Nursing Intervention Based on Targeted Nursing Intervention on Anxiety and Nursing Satisfaction of Patients with Malignant Tumors Undergoing Chemotherapy. J Healthc Eng. 2021;2021:4438446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Gao M, Zhang L, Wang Y, Li L, Wang C, Shen Q, Wang Y, Liao B. Influence of humanistic care based on Carolina care model for ovarian cancer patients on postoperative recovery and quality of life. Am J Transl Res. 2021;13:3390-3399. [PubMed] |
| 10. | Lv L, Liu Y, Tian T, Li J. Effect of Self-Efficacy Intervention Combined with Humanistic Nursing on Self-Care Ability and Quality of Life in Patients Receiving Chemotherapy for Malignant Tumors. Iran J Public Health. 2022;51:345-354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Gao N, Li Y, Sang C, He J, Chen C. Effect of high-quality nursing on neurological function psychological moods quality of life of elderly patients with stroke. Front Neurol. 2023;14:1259737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 12. | Li C, Duan J. Effect of high-quality nursing intervention on psychological emotion, life quality and nursing satisfaction of patients with nasopharyngeal carcinoma undergoing radiotherapy. Am J Transl Res. 2021;13:4928-4938. [PubMed] |
| 13. | Liu Y, Zhang F, Guan C, Song B, Zhang H, Fu M, Wang F, Tang C, Chen H, Guo Q, Fan L, Hou X, Wang H, Wu B, Shan G, Zhang H, Yu F, Lou X, Xie H, Zhou Y, Lu G, Xin X, Pan S, Guo S. Patient satisfaction with humanistic nursing in Chinese secondary and tertiary public hospitals: a cross-sectional survey. Front Public Health. 2023;11:1163351. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Liu H, Zhang L, Yan J, Huang H, Yi Q, Peng L. The Relationship between Social Support, Empathy, Self-Efficacy, and Humanistic Practice Ability among Clinical Nurses in China: A Structural Equation Model. Journal of Nursing Management. 2023;2023:1-9. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Zhu Y, Liu G, Shen Y, Wang J, Lu M, Wang J. Humanistic Nursing Care for Patients in Low-Resourced Clinical Settings from Students' Perspectives: A Participatory Qualitative Study. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Ren L, Zhu D, Wei Y, Pan X, Liang L, Xu J, Zhong Y, Xue Z, Jin L, Zhan S, Niu W, Qin X, Wu Z, Wu Z. Enhanced Recovery After Surgery (ERAS) program attenuates stress and accelerates recovery in patients after radical resection for colorectal cancer: a prospective randomized controlled trial. World J Surg. 2012;36:407-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 163] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 17. | Ghoneim MM, O'Hara MW. Depression and postoperative complications: an overview. BMC Surg. 2016;16:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 255] [Cited by in RCA: 294] [Article Influence: 32.7] [Reference Citation Analysis (0)] |
| 18. | Shibutani M, Nakao S, Maeda K, Nagahara H, Fukuoka T, Iseki Y, Hirakawa K, Ohira M. Inflammation Caused by Surgical Stress Has a Negative Impact on the Long-term Survival Outcomes in Patients With Colorectal Cancer. Anticancer Res. 2020;40:3535-3542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Zhu G, Kang Z, Chen Y, Zeng J, Su C, Li S. Ultrasound-guided stellate ganglion block alleviates stress responses and promotes recovery of gastrointestinal function in patients. Dig Liver Dis. 2021;53:581-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 20. | Liu M, Qi L. The related factors and countermeasures of hypothermia in patients during the anesthesia recovery period. Am J Transl Res. 2021;13:3459-3465. [PubMed] |
| 21. | Wang S, Huang H, Wang L, Wang X. A Psychological Nursing Intervention for Patients With Thyroid Cancer on Psychological Distress and Quality of Life: A Randomized Clinical Trial. J Nerv Ment Dis. 2020;208:533-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Li L, Liu L, Kang H, Zhang L. The influence of predictive nursing on the emotions and self-management abilities of post-colostomy rectal cancer patients. Am J Transl Res. 2021;13:6543-6551. [PubMed] |
| 23. | Shi X, Ma L, Hao J, Yan W. Regulatory effects of comprehensive psychological intervention on adverse emotions and immune status of cervical cancer patients during the perioperative period. Am J Transl Res. 2021;13:6362-6371. [PubMed] |
| 24. | Tu M, Wang F, Shen S, Wang H, Feng J. Influences of Psychological Intervention on Negative Emotion, Cancer-Related Fatigue and Level of Hope in Lung Cancer Chemotherapy Patients Based on the PERMA Framework. Iran J Public Health. 2021;50:728-736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |