Published online Aug 16, 2024. doi: 10.12998/wjcc.v12.i23.5308
Revised: May 22, 2024
Accepted: June 3, 2024
Published online: August 16, 2024
Processing time: 77 Days and 2.7 Hours
In this editorial, we comment on an article by Alhammad et al that was published in a recent issue of the World Journal of Clinical Cases (Manuscript No.: 91134). We specifically focus on the mental health problems caused by coronavirus disease 2019 (COVID-19), their mechanisms, and targeted rehabilitation strategies. Severe acute respiratory syndrome coronavirus 2, via its spike protein, binds to angio
Core Tip: Epidemiological data from 2020 have revealed a worldwide escalation in major depressive disorders by 27.6% and in anxiety disorders by 25.6% amid the coronavirus disease 2019 (COVID-19) pandemic. The prevalence of mental health issues among patients with COVID-19 after rehabilitation is on the rise and is potentially linked to bereavement or the neurological impact of the virus. Implementing dietary interventions, health supplements, and traditional Chinese medicines with neuroprotective properties is imperative to safeguard the nervous systems of these individuals and improve their mental well-being.
- Citation: Hu HS, Sun BQ. Understanding the etiology of mental health problems in post-rehabilitation COVID-19 patients: Insights and strategies for effective intervention. World J Clin Cases 2024; 12(23): 5308-5312
- URL: https://www.wjgnet.com/2307-8960/full/v12/i23/5308.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i23.5308
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), originating in December 2019, is an RNA virus classified within the coronavirus family. Its entry into the body is facilitated by the spike protein (S protein), which binds to the angiotensin-converting enzyme 2 and other receptors. This enables the virus to infiltrate a variety of cells within the central nervous system (CNS), including endothelial cells, neurons, astrocytes, and oligodendrocytes[1]. This broad cellular invasion has profound implications on the host. Evidence suggests that infection of these CNS-resident cells may lead to enduring consequences and potentially contribute to the development of neurodegenerative disorders over time[2]. Epidemiological data from 2020 revealed a global surge in patients with major depressive disorders by 27.6% and in anxiety disorders by 25.6% amidst the pandemic[3]. Furthermore, a survey that involved 402 coronavirus disease 2019 (COVID-19) survivors indicated varying rates of posttraumatic stress disorder, depression, anxiety, obsessive-compulsive symptoms, and insomnia, with percentages reaching as high as 42% for anxiety[4]. Neurological symptoms, including headache, altered consciousness, and paresthesia, have been documented in 36.4% of patients with COVID-19, particularly among the severely affected[5]. The neurological impact is notably high, reaching levels up to 88% in severely infected individuals[6]. Autopsy findings have revealed brain tissue edema and neuronal degeneration. The Beijing Ditan Hospital reported a case of viral encephalitis induced by SARS-CoV-2 attacking the CNS[7]. Additionally, genome sequencing has confirmed the presence of the virus in cerebrospinal fluid (CSF), which highlights the potential of COVID-19 to inflict nervous system damage[8]. The study of interest showed that 30% of patients with COVID-19 in the Arabic region exhibited Hospital Anxiety and Depression scales scores that reflect anxiety and depression following discharge from the intensive care unit[9]. This underscores the importance of analyzing the potential causes of poor mental health of and offering rehabilitation recommendations for patients with COVID-19.
Years of trauma research indicate that, following negative life events, such as loss or exposure to disasters, most individuals experience either resilience, where there is minimal impact on symptoms of anxiety or depression, or recovery, marked by an initial increase in symptoms followed by improvement[10]. This trend aligns with the findings of extensive studies conducted during the COVID-19 pandemic. During this period, anxiety and depression symptoms peaked, likely as an acute response to an unforeseen crisis[11]. Therefore, we cannot rule out the possibility that the patients included in the study may have experienced mental health problems due to excessive longing or sadness caused by the passing of family or friends.
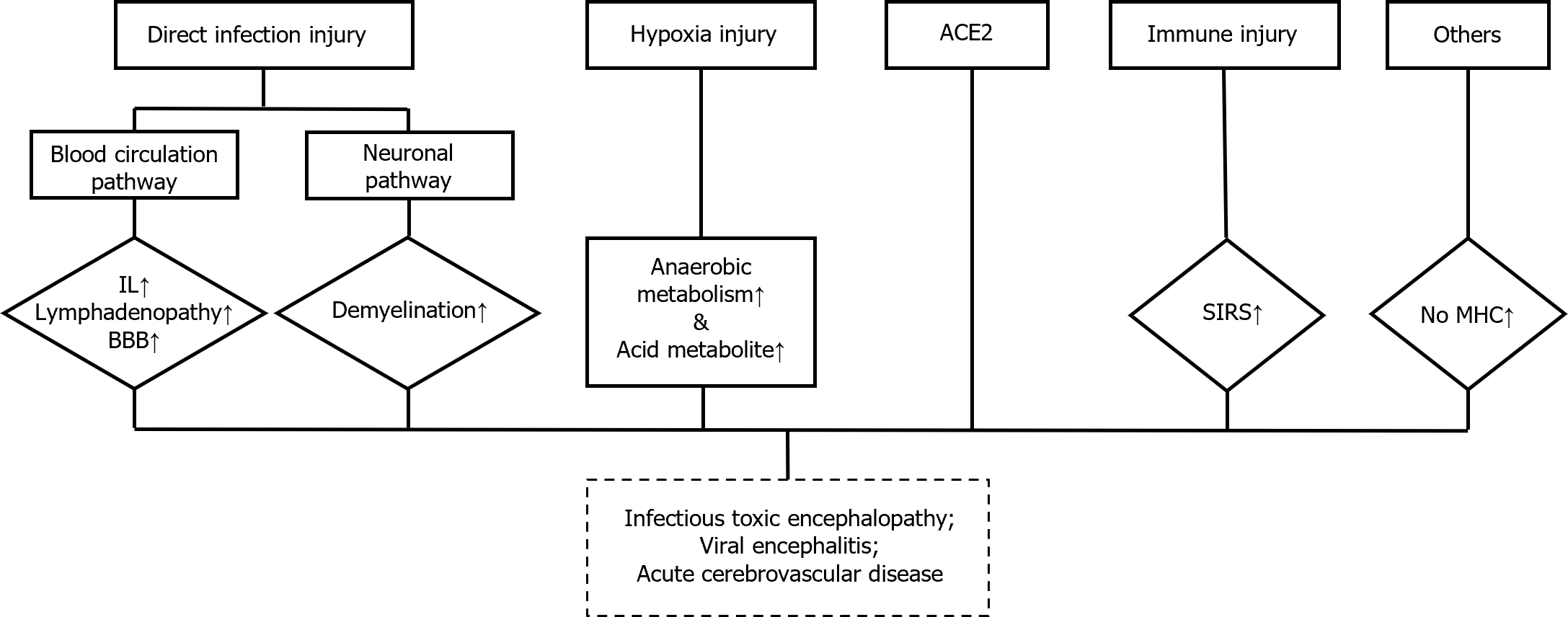
However, perturbations in the immune system triggered by an infection can also lead to psychopathological symptoms, as evidenced by past coronavirus outbreaks[12]. In a study conducted in India, postmortem examinations of the brains of rhesus and cynomolgus macaques following pulmonary disease induced by SARS-CoV-2 revealed T cell infiltration and microglial activation[13]. Damage to the immune system can diminish the ability of the nerve tissues to resist pathogen invasion and efficiently clear harmful substances, potentially resulting in mental health problems. Viral infections can also directly affect neurological function and potentially cause severe neurological damage. SARS-CoV-2 has been found to possess neurotropic properties and can induce neurological diseases. Evidence suggests that coronaviruses can be detected in the brain or colony-stimulating factor, thus potentially leading to psychopathological sequelae through direct infection of the CNS or indirectly via immune responses[14]. Various studies, including clinical observations, post-mortem analyses, animal experiments, and in vitro studies, have highlighted the neurotropic potential of coronaviruses and their ability to cause neuronal injury[15]. Additionally, research by Dantzer[16] suggests that the immune response to coronaviruses, characterized by a "cytokine storm," may contribute to psychiatric symptoms by triggering neuroinflammation. A possible mechanism for this is shown in Figure 1. Furthermore, preliminary findings suggest that SARS-CoV-2 instigates molecular and cellular alterations akin to those observed in Alzheimer's disease[17]. Another study indicates that neurotoxic amyloidogenic peptides derived from SARS-CoV-2 could be responsible for triggering neurological symptoms in patients with COVID-19[18], such as α-synuclein aggregates, which are involved in Parkinson's disease[19]. Moreover, a study from the United States suggested that SARS-CoV-2-infected mice displayed respiratory symptoms exhibiting increased expression of cytokines and chemokines, CCL11, in their CSF, resulting in hippocampal microglia activation. Subsequently, leading to impaired neurogenesis and loss of oligodendrocytes and myelinated axons[20]. Therefore, patients with severe clinical symptoms are more likely to experience mental-health problems.
Those with mental problems after a COVID-19 diagnosis should follow doctors’ advice regarding the reasonable use of psychotherapeutic drugs during the recovery period[21]. Herein, we discuss the prevention of mental illness in convalescent patients with COVID-19 who are mentally healthy or in a sub-healthy state. Research has shown that Hericium erinaceus contains erinacines and hericenones, which stimulate the release of nerve growth factors, regulate inflammatory processes, reduce oxidative stress, protect nerve cells from apoptosis, and can be used as a functional food[22]. In addition, the products of some health care companies can also be used to prevent mental problems in patients with COVID-19 after rehabilitation, such as Sour jujube kernel γ-aminobutyric acid tablets (nutrilite®) and Broken wall Ganoderma spore powder (nutrilite®). Prior studies have shown that traditional Chinese medicine has significant efficacy in protecting the nervous system. The research of Liu et al[23] showed that Panax ginseng (Meyer) and Panax notoginseng (Burkill) contain important bioactive ingredients such as ginsenosides and exert multiple pharmacological effects on the nervous system and immune diseases. Therefore, these methods can be used to improve the prognosis of patients with COVID-19 and effectively reduce the occurrence of mental diseases.
In general, mental illness or mental health issues are increasing in patients with COVID-19 after rehabilitation, which may be related to the loss of relatives or invasion of the nervous system of patients with COVID-19. Therefore, it is necessary to perform psychological rehabilitation for patients with COVID-19.
We express our gratitude to Dr. Hong W, Marketing Manager Kuang Junjie, and Professor He YZ from Amway for their suggestions on relevant health products.
| 1. | Jackson CB, Farzan M, Chen B, Choe H. Mechanisms of SARS-CoV-2 entry into cells. Nat Rev Mol Cell Biol. 2022;23:3-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1831] [Cited by in RCA: 1915] [Article Influence: 638.3] [Reference Citation Analysis (0)] |
| 2. | Weissert R. Nervous system-related tropism of SARS-CoV-2 and autoimmunity in COVID-19 infection. Eur J Immunol. 2024;54:e2250230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 3. | Daly M, Robinson E. Depression and anxiety during COVID-19. Lancet. 2022;399:518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 124] [Article Influence: 41.3] [Reference Citation Analysis (0)] |
| 4. | Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, Melloni EMT, Furlan R, Ciceri F, Rovere-Querini P; COVID-19 BioB Outpatient Clinic Study group, Benedetti F. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594-600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 967] [Cited by in RCA: 1014] [Article Influence: 202.8] [Reference Citation Analysis (0)] |
| 5. | Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4761] [Cited by in RCA: 4704] [Article Influence: 940.8] [Reference Citation Analysis (0)] |
| 6. | Iroegbu JD, Ifenatuoha CW, Ijomone OM. Potential neurological impact of coronaviruses: implications for the novel SARS-CoV-2. Neurol Sci. 2020;41:1329-1337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 7. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18987] [Cited by in RCA: 17641] [Article Influence: 3528.2] [Reference Citation Analysis (0)] |
| 8. | Scheuermeier M, Chaves KQ, Marín-Sanabria D, Acosta-Lazo H, Ulate-Campos A. First Pediatric Case of Autoimmune Encephalitis Associated With COVID-19 in Costa Rica. Cureus. 2022;14:e30616. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Alhammad AM, Aldardeer NF, Alqahtani A, Aljawadi MH, Alnefaie B, Alonazi R, Almuqbil M, Alsaadon A, Alqahtani RM, Alballaa R, Alshehri B, Alarifi MI, Alosaimi FD. Mental health status among COVID-19 patients survivors of critical illness in Saudi Arabia: A 6-month follow-up questionnaire study. World J Clin Cases. 2024;12:2560-2567. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Chen S, Bonanno GA. Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychol Trauma. 2020;12:S51-S54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 222] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 11. | Robinson E, Sutin AR, Daly M, Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before vs during the COVID-19 pandemic in 2020. J Affect Disord. 2022;296:567-576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 673] [Cited by in RCA: 640] [Article Influence: 213.3] [Reference Citation Analysis (0)] |
| 12. | Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, McKyer ELJ, Ahmed HU, Ma P. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 536] [Cited by in RCA: 559] [Article Influence: 111.8] [Reference Citation Analysis (0)] |
| 13. | Philippens IHCHM, Böszörményi KP, Wubben JAM, Fagrouch ZC, van Driel N, Mayenburg AQ, Lozovagia D, Roos E, Schurink B, Bugiani M, Bontrop RE, Middeldorp J, Bogers WM, de Geus-Oei LF, Langermans JAM, Verschoor EJ, Stammes MA, Verstrepen BE. Brain Inflammation and Intracellular α-Synuclein Aggregates in Macaques after SARS-CoV-2 Infection. Viruses. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 14. | Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1219] [Cited by in RCA: 1255] [Article Influence: 251.0] [Reference Citation Analysis (0)] |
| 15. | Desforges M, Le Coupanec A, Dubeau P, Bourgouin A, Lajoie L, Dubé M, Talbot PJ. Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System? Viruses. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 590] [Cited by in RCA: 707] [Article Influence: 117.8] [Reference Citation Analysis (0)] |
| 16. | Dantzer R. Neuroimmune Interactions: From the Brain to the Immune System and Vice Versa. Physiol Rev. 2018;98:477-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 622] [Article Influence: 88.9] [Reference Citation Analysis (0)] |
| 17. | Shen WB, Elahi M, Logue J, Yang P, Baracco L, Reece EA, Wang B, Li L, Blanchard TG, Han Z, Rissman RA, Frieman MB, Yang P. SARS-CoV-2 invades cognitive centers of the brain and induces Alzheimer's-like neuropathology. bioRxiv. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 18. | Charnley M, Islam S, Bindra GK, Engwirda J, Ratcliffe J, Zhou J, Mezzenga R, Hulett MD, Han K, Berryman JT, Reynolds NP. Neurotoxic amyloidogenic peptides in the proteome of SARS-COV2: potential implications for neurological symptoms in COVID-19. Nat Commun. 2022;13:3387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 19. | Brundin P, Nath A, Beckham JD. Is COVID-19 a Perfect Storm for Parkinson's Disease? Trends Neurosci. 2020;43:931-933. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 20. | Fernández-Castañeda A, Lu P, Geraghty AC, Song E, Lee MH, Wood J, O'Dea MR, Dutton S, Shamardani K, Nwangwu K, Mancusi R, Yalçın B, Taylor KR, Acosta-Alvarez L, Malacon K, Keough MB, Ni L, Woo PJ, Contreras-Esquivel D, Toland AMS, Gehlhausen JR, Klein J, Takahashi T, Silva J, Israelow B, Lucas C, Mao T, Peña-Hernández MA, Tabachnikova A, Homer RJ, Tabacof L, Tosto-Mancuso J, Breyman E, Kontorovich A, McCarthy D, Quezado M, Vogel H, Hefti MM, Perl DP, Liddelow S, Folkerth R, Putrino D, Nath A, Iwasaki A, Monje M. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell. 2022;185:2452-2468.e16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 293] [Cited by in RCA: 325] [Article Influence: 108.3] [Reference Citation Analysis (0)] |
| 21. | Mueller JK, Riederer P, Müller WE. Neuropsychiatric Drugs Against COVID-19: What is the Clinical Evidence? Pharmacopsychiatry. 2022;55:7-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Li TJ, Lee TY, Lo Y, Lee LY, Li IC, Chen CC, Chang FC. Hericium erinaceus mycelium ameliorate anxiety induced by continuous sleep disturbance in vivo. BMC Complement Med Ther. 2021;21:295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Liu H, Lu X, Hu Y, Fan X. Chemical constituents of Panax ginseng and Panax notoginseng explain why they differ in therapeutic efficacy. Pharmacol Res. 2020;161:105263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 187] [Article Influence: 37.4] [Reference Citation Analysis (0)] |