Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5271
Revised: May 31, 2024
Accepted: June 18, 2024
Published online: August 6, 2024
Processing time: 60 Days and 19.8 Hours
Facial herpes is a common form of the herpes simplex virus-1 infection and usually presents as vesicles near the mouth, nose, and periocular sites. In contrast, we observed a new facial symptom of herpes on the entire face without vesicles.
A 33-year-old woman with a history of varicella infection and shingles since an early age presented with sarcoidosis of the entire face and neuralgia without oral lesions. The patient was prescribed antiviral treatment with valacyclovir and acyclovir cream. One day after drug administration, facial skin lesions and neuro
As acute herpes simplex is accompanied by neuralgia, prompt diagnosis and prescription are necessary, considering the pathological history and health conditions.
Core Tip: Unlike common facial herpes, this case introduces a new pan-facial herpes symptom: Swollen redness on the patient’s entire face without herpetic vesicles. The patient had experienced recurrent infections with herpes simplex and herpes zoster viruses since the age of 7 years. On the visit day, the patient complained of headache and neuralgia; hence, a prompt antiviral prescription was advised based on the patient’s pathological history and current condition.
- Citation: Bae EB. Recurrent herpes infection showing a new facial phenotype: A case report. World J Clin Cases 2024; 12(22): 5271-5275
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5271.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5271
In cases of fatigue and stress, people can be infected with herpes simplex virus-1 (HSV-1), which lies dormant in the nervous system[1]. It appears on the surface of the skin, especially in the face, nose, lips, and eyes. Orofacial herpes infection, also known as herpes labialis or cold sores, is caused by HSV-1 and commonly occurs as blisters or cold sores around the mouth and nose; it is rarely reported as a facial infection[2,3]. Many cases present with infections on the lip and near the mouth. Some rare cases have reported infections in the palate or nose caused by filler injection, eye infections known as herpes simplex ophthalmicus, and head infections known as herpes simplex encephalitis. Based on the specific visual characteristics of herpes, which are vesicular eruptions near the mouth and nose, most orofacial cases are first diagnosed through visual examination at an outpatient clinic. However, cases of facial HSV-1 infection are rarely identified and can be misdiagnosed as other dermatological diseases[4-6]. Here, we present the case of a 33-year-old female HSV-1 who was misdiagnosed.
A 33-year-old healthy woman complained of neuralgia that started at the periocular site and severe headache.
On that day, she visited two clinics and was misdiagnosed with urticaria and pimples. She then visited a third clinic. Considering the recent three consecutive days of her health condition (lack of sleep and physical burden), pan-facial herpes symptoms seemed to result in a weakened immune system, as manifested by cutaneous sarcoidosis.
She had a prescription history of antiviral drugs (14 days) for herpetic symptoms on the left forehead, assuming herpes encephalitis, from 2018 to 2019.
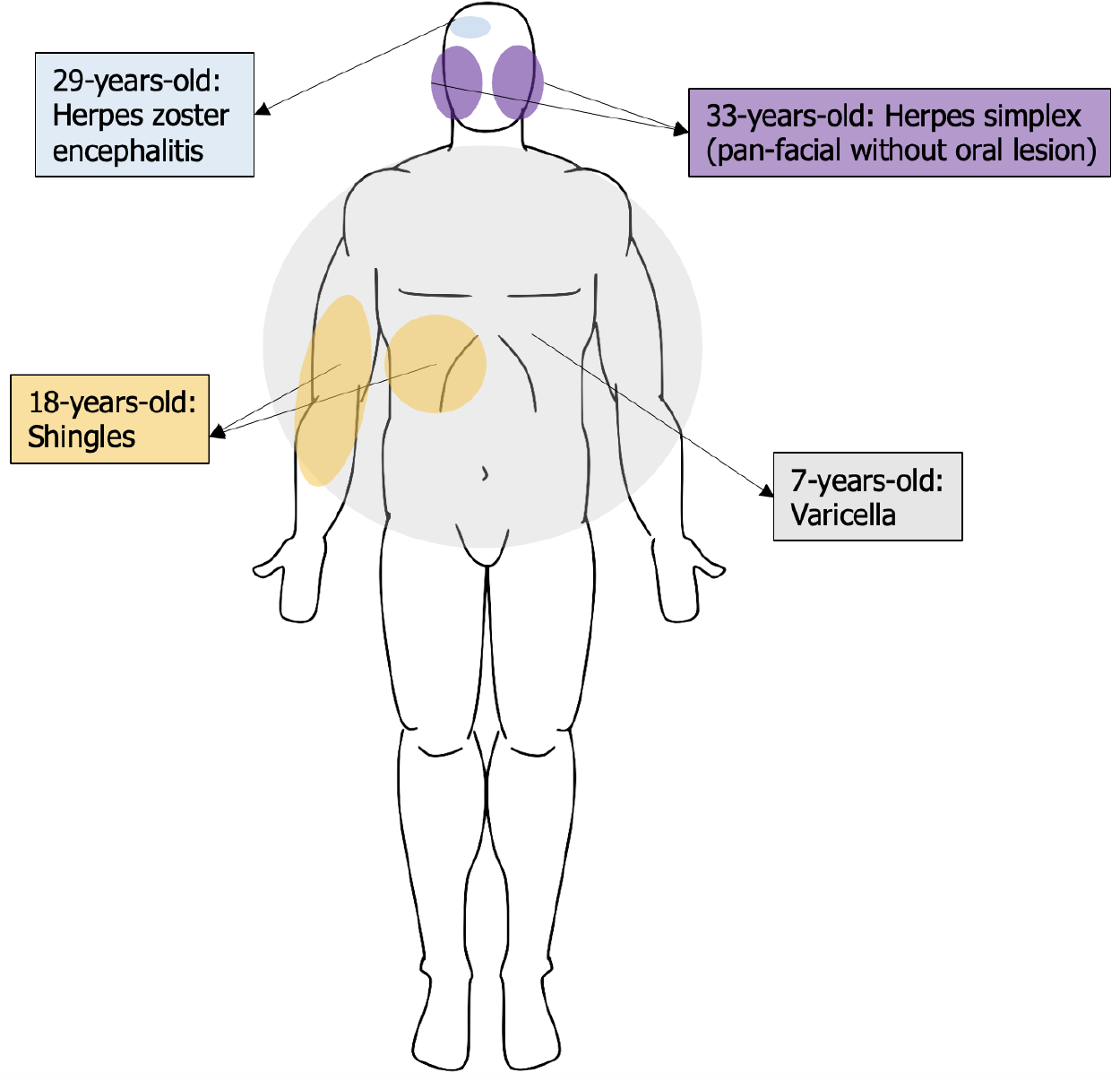
According to the patient’s clinical history (Figure 1), the first herpes virus infection was varicella zoster at seven years of age. The second varicella zoster infection occurred when she was 18 years old and preparing for a national exam; she was diagnosed with shingles on the right side of her arm and abdomen with large multiple vesicles. When she was under a lot of stress at 29 years of age, unusual right-sided headaches often occurred on the same side as the prior skin rash, right side of her upper forehead, and blisters on her fingers. She was prescribed antiviral medication twice for suspected herpes zoster encephalitis symptoms between 2018 and 2019.
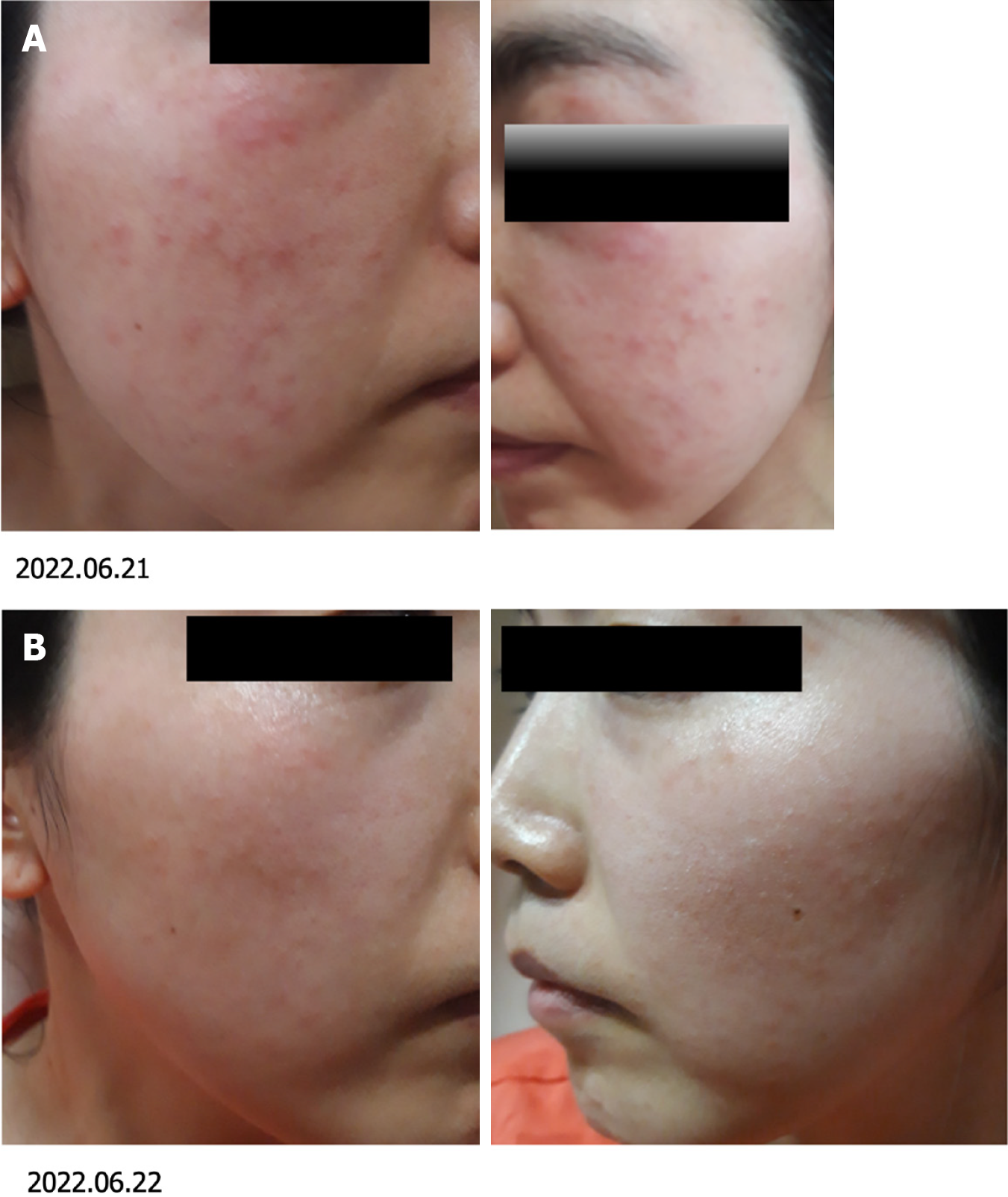
Numerous small pimples covered the patient’s face, and the bilateral eyelids and cheeks were swollen (Figure 2A). However, few blisters or vesicles such as cold sore were identified on the face, and none were near the mouth, palate, or nose. Because of the numerous pimple-like redness, small vesicles at periocular sites are rarely distinguished from other skin diseases, such as acne and urticaria. When the patient washed and cleaned the lesions, multiple tiny vesicles, formed under the bilateral periocular sites, were observed.
In this urgent situation, medication was prescribed based on the patient's herpes history without a polymerase chain reaction (PCR) examination.
Considering the patient’s pathological history, current health condition, and chief complaint, HSV-1 with a new form of facial herpes was suspected.
Antiviral treatment was prescribed on the first day of treatment (Figure 3): Valtmax (Valaciclovir HCl Sesquihydrate) tablets (500 mg) three times a day for two days and acyclovir cream every 5 hours for two days.
On the second day of treatment (treatment day 2 in Figure 3), pan-facial herpetic symptoms disappeared (Figure 2B).
Facial HSV-1 is uncommon and can be easily misdiagnosed when vesicles are not present near the mouth[4-6]. The foremost option to accurately diagnose herpes virus subspecies in the clinic is PCR[7-10]. However, this test has a major limitation: In the case of small clinics in South Korea, it takes about 2-3 days from testing to receiving the results, which often results in patients not receiving prescriptions on time. Another delay in the timely treatment of herpes is the involvement of different departments based on the physical region affected: For example, dermatology for skin symptoms, otorhinolaryngology for nose and mouth herpetic lesions, ophthalmology for ocular lesions, dentistry for oral lesions, and neurology for infection of the facial nerve and neuralgia. Under these circumstances, patients with a long history and having several different presentations of herpes and varicella-zoster infections are difficult to accurately diagnose. Therefore, in this case, the diagnosis based on the history of herpes was more accurate because of the new facial presentation of herpes.
Whereas one symptom of herpes, recurrent cold sore, is well-known, recurrent infection of varicella zoster virus has been rarely reported. In one study, Heskel and Hanifin[11] reported “recurrent zoster,” misdiagnosed cases of herpes symptoms that appeared on the entire face of patients who had experienced recurrent herpes infections previously. Yamauchi et al[12] reported the recurrence of cutaneous sarcoidosis after herpes zoster infection. Similarly, Chovatiya and Silverberg[13] studied the association between herpes zoster and chronic inflammatory skin diseases in patients, including sarcoidosis (adjusted odds: 1.52), psoriasis (4.78), pemphigus (1.77), mycosis fungoides (3.79), dermatomyositis (7.31), systemic sclerosis (1.92), and cutaneous lupus erythematosus (1.94). Those studies and our case suggest that herpes zoster can vary in dermatological symptoms when a person is immuno-compromised. Still, recurrent infections or variations in the herpes virus have rarely been reported in longitudinal studies, and this is the first case of a new symptom on the face of a person with a long history of recurrent cross-infection between HSV-1 and varicella zoster virus. This case report is consistent with previous cases that imply that the long-term morbidity of varicella zoster virus could lead to unexpected physical symptoms of HSV-1.
This case demonstrated that those who experienced herpes zoster could be recurrently and acutely infected with a new form of HSV-1 and show inflammatory skin rash, such as cutaneous sarcoidosis, that is visually unlike commonly known herpetic symptoms. Facial herpes is often accompanied by neuralgia or headache and requires prompt antiviral treatment to prevent the development of severe nervous system diseases. In future studies, the association between acute inflammatory skin rashes such as cutaneous sarcoidosis and herpes subtypes should be studied using molecular tests.
| 1. | Worrall G. Herpes labialis. BMJ Clin Evid. 2009;2009. [PubMed] |
| 2. | Patel AR, Romanelli P, Roberts B, Kirsner RS. Treatment of herpes simplex virus infection: rationale for occlusion. Adv Skin Wound Care. 2007;20:408-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Bodur M, Toker RT, Özmen AH, Okan MS. Facial colliculus syndrome due to a Herpes simplex virus infection following Herpes labialis. Turk J Pediatr. 2021;63:727-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Dworkin MS, Shoemaker PC, Spitters C, Cent A, Hobson AC, Vieira J, Corey L, Frumkin LR. Endemic spread of herpes simplex virus type 1 among adolescent wrestlers and their coaches. Pediatr Infect Dis J. 1999;18:1108-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Jalali S, Kolari RS, Pathengay A, Athmanathan S. Severe hemorrhagic retinopathy as initial manifestation of acute retinal necrosis caused by herpes simplex virus. Indian J Ophthalmol. 2007;55:308-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Whallett EJ, Pahor AL. Herpes and the head and neck: the difficulties in diagnosis. J Laryngol Otol. 1999;113:573-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Xie G, Wei Q, Guo W, Li D, Sun P, Wang J, Liu H. An adult co-presented with varicella and herpes zoster caused by varicella zoster virus genotype J, China: a case report. BMC Infect Dis. 2020;20:454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Costa-Silva M, Sobrinho-Simões J, Azevedo F, Lisboa C. Concurrent reactivation of varicella zoster virus and herpes simplex virus in an immunocompetent elderly male. An Bras Dermatol. 2019;94:762-763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Joo T, Lee YC, Kim TG. Herpes zoster involving the abducens and vagus nerves without typical skin rash: A case report and literature review. Medicine (Baltimore). 2019;98:e15619. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Pelloni LS, Pelloni R, Borradori L. Herpes zoster of the trigeminal nerve with multi-dermatomal involvement: a case report of an unusual presentation. BMC Dermatol. 2020;20:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Heskel NS, Hanifin JM. "Recurrent herpes zoster": an unproved entity? J Am Acad Dermatol. 1984;10:486-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Yamauchi K, Oiso N, Iwanaga T, Tatsumi Y, Matsumura I, Tohda Y, Kawada A. Post-herpes zoster sarcoidosis as a recurrence. J Dermatol. 2018;45:e150-e151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Chovatiya R, Silverberg JI. Association of herpes zoster and chronic inflammatory skin disease in US inpatients. J Am Acad Dermatol. 2021;85:1437-1445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |