Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5189
Revised: May 11, 2024
Accepted: May 30, 2024
Published online: August 6, 2024
Processing time: 90 Days and 19.3 Hours
This paper reports a rare presentation of multiple pulp stones (PSs) emerging in all teeth during mixed dentition. It offers valuable insights into the clinical diag
A 10-year-old girl presented with repeated pain in the mandibular right posterior teeth. Intraoral examination revealed carious lesions, abnormal tooth shapes, and anomalies in tooth number. Radiographic examinations showed multiple PSs with diverse shapes, sizes, and quantities in all teeth, alongside anomalies in tooth shape and number. Root canal therapy was initiated, but the patient initially lacked timely follow-up. Upon return for treatment completion, an extracted tooth revealed irregular calculus within the pulp cavity.
This case underscores the importance of considering multiple PSs in mixed dentition, necessitating comprehensive evaluation and management strategies.
Core Tip: This paper reports a rare clinical case of multiple pulp stones involving the entire mouth during the period of dentition. After two years of follow-up, we found that the occurrence of pulp stone did not have a significant negative impact on the development of the teeth.
- Citation: Lv Y, Zhu J, Fu CT, Liu L, Wang J, Li YF. Multiple pulp stones emerge across all teeth during mixed dentition: A case report. World J Clin Cases 2024; 12(22): 5189-5195
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5189.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5189
Pulp stones (PSs) represent a form of pulp calcification, appearing as calcified masses within the pulp cavity. They are frequently associated with dental pulp diseases but can also occur in healthy or unerupted teeth[1-4]. PSs are classified into true and false types, with a third category known as “diffuse” or “amorphous” PSs, which exhibit irregular shapes and often form near blood vessels[5]. Depending on their location, PSs can be embedded, adherent, or free[6]. Histologically, two types of PSs are recognized: Those with round or ovoid shapes, smooth surfaces, and concentric laminations, and those lacking distinct shapes, laminations, and featuring rough surfaces[7]. This case report highlights the presentation of a patient with repeated pain in the mandibular right posterior teeth over 1 mo, initially suggesting a straightforward diagnosis and treatment. However, accidental radiographic examination revealed multiple PSs in all teeth, exhibiting varied shapes, quantities, and sizes, alongside abnormalities in tooth shape and number. Such a presentation during the mixed dentition period is rare. This report offers valuable insights for the clinical diagnosis, treatment, and prognosis of multiple PSs.
A 10-year-old girl was referred to the Department of Stomatology in our hospital in October 2020, complaining of “repeated pain in the mandibular right posterior teeth for 1 mo”.
Upon intraoral examination (Figure 1), partial carious lesions were noted in the mesial buccal apex and the larger distal occlusal area of tooth No. 46 (Fédération Dentaire Internationale). Tooth No. 46 exhibited an atypical shape of the re
The patient had a clean bill of health previously, with no history of periodontal or orthodontic treatment, and her family history was unremarkable.
The patient’s family history was unremarkable.
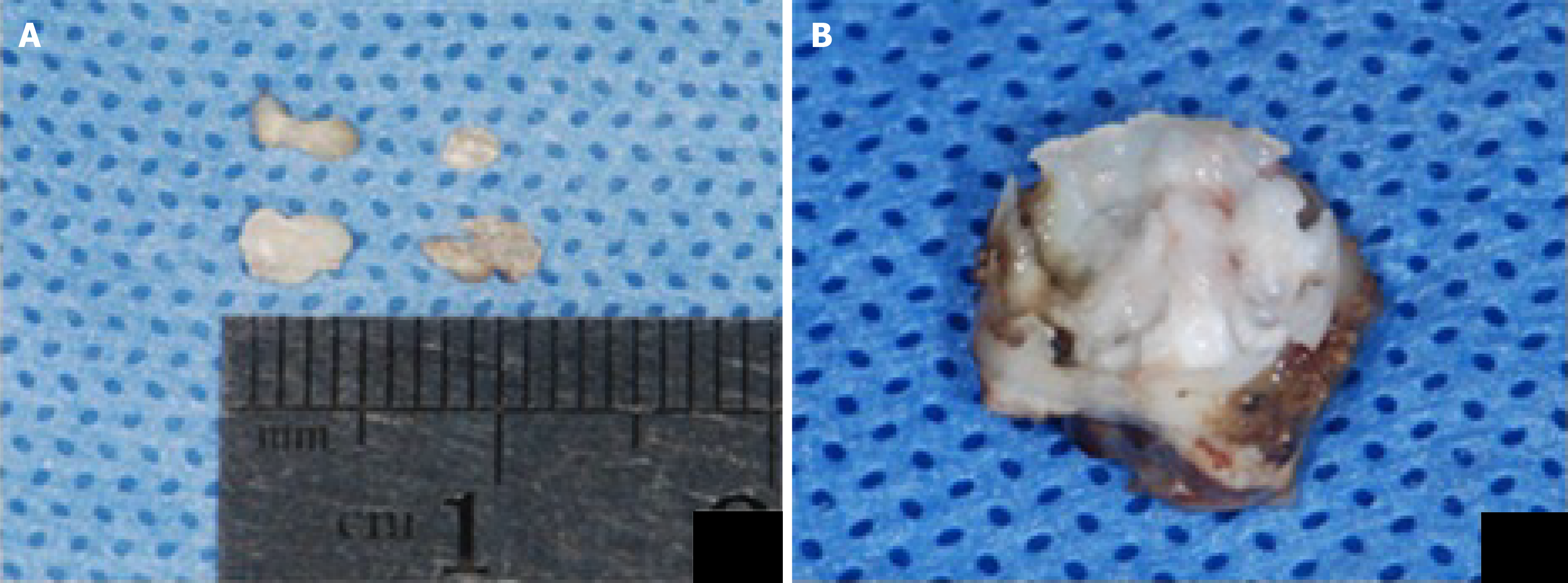
The primary diagnosis of the case was chronic periapical inflammation of tooth 46 with multiple PSs, warranting root canal therapy. On the day of the patient’s visit, the pulp of tooth 46 was opened, the root canal was meticulously cleaned, and a temporary seal was applied (Figure 1C). Additionally, some of the PSs were removed (Figure 2A). However, the patient failed to adhere to timely follow-up visits. During this period, they underwent crown repair for teeth 12-22 and filling for tooth 36 at an external hospital. It was not until November 2022 when the patient returned to our department to complete the root canal treatment for tooth 46. Subsequently, tooth 85 was extracted, revealing a substantial amount of irregular calculus within the pulp cavity (Figure 2B).
None.
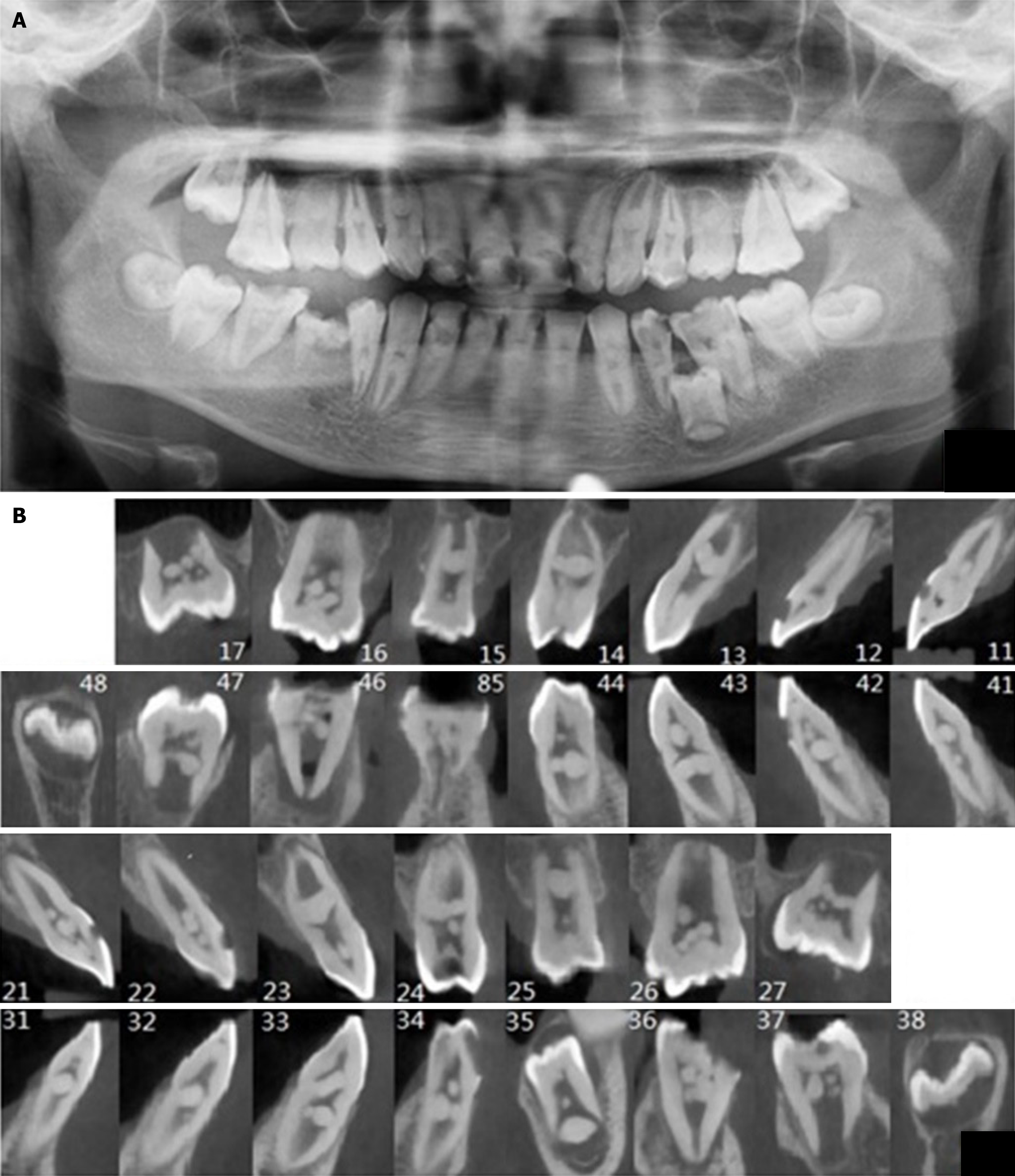
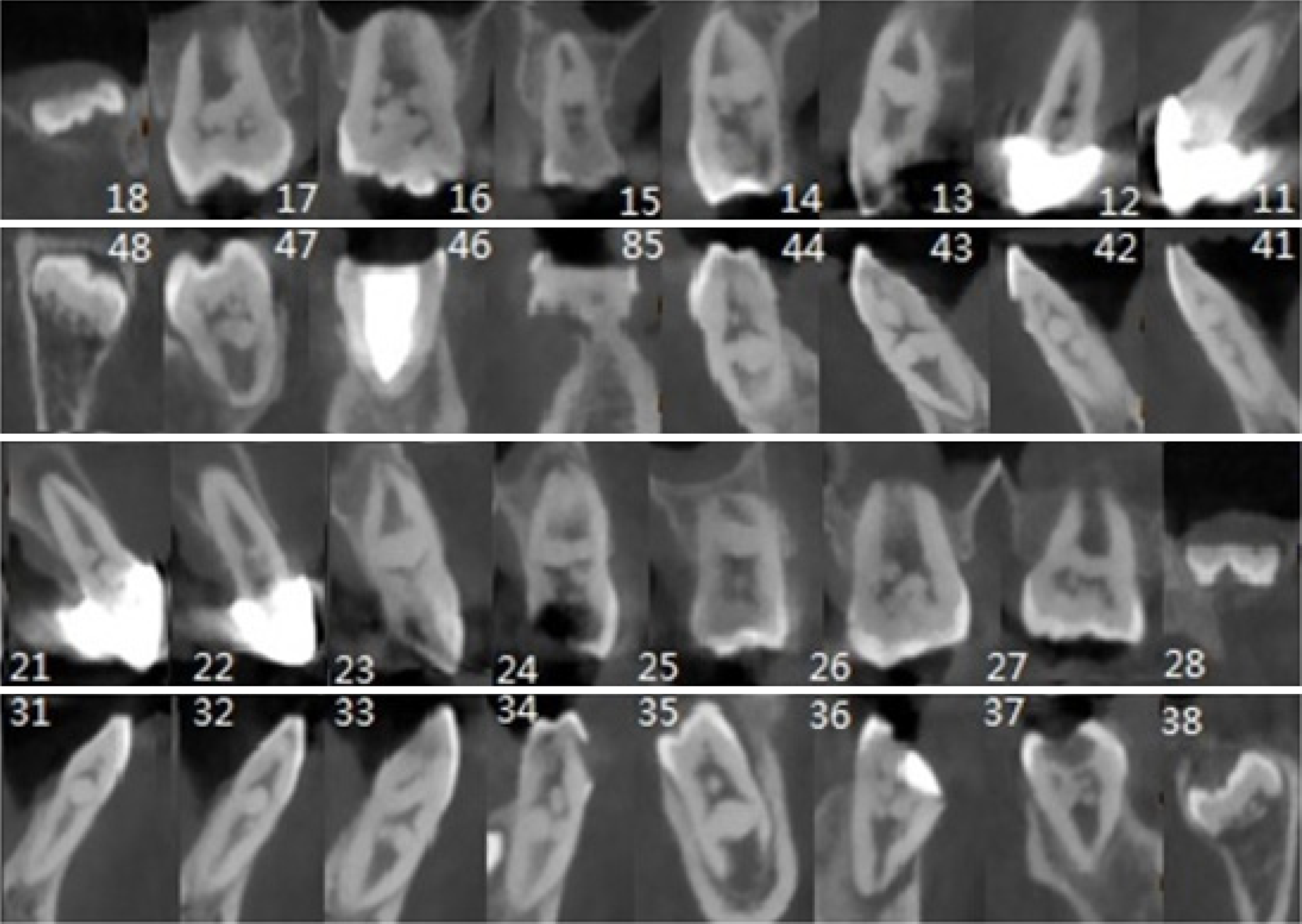
A panoramic oral radiogram (Figure 3A) was initially taken at the initial consultation in October 2020, followed by further cone-beam computed tomography (CBCT) imaging (Figure 3B). The radiographs revealed a tapered single root of tooth 46 with a periapical hypodense shadow and no evidence of root bifurcation. The pulp cavity appeared coarse, with an indistinct demarcation between the coronal and root pulp cavities. Multiple dense masses with irregular morphologies and obstructive shadows were observed near the crown. In all teeth except the wisdom teeth, blocked masses of varying sizes and numbers, presenting as round, oval, or irregularly margined, were visible within the pulp chamber. Addi
In December 2022, a repeat cone-beam CT scan was conducted, revealing that the morphology, number, and size of PSs in teeth with largely developed roots remained largely unchanged compared to previous scans. Most tooth apices were either largely closed or continuing to develop. In teeth 38 and 48, the crowns were observed to be in continued de
Chronic periapical inflammation of tooth 46 with multiple PSs.
On the day of the patient’s visit, the pulp of tooth 46 was opened, the root canal was meticulously cleaned, and a temporary seal was applied (Figure 1C). Additionally, some of the PSs were removed (Figure 4A).
The patient failed to adhere to timely follow-up visits. During this period, she underwent crown repair for teeth 12-22 and filling for tooth 36 at an external hospital.
The prevalence of PSs varies widely across different study populations and examination methods, with reported rates ranging from 9.57% to 71.07%[3,8,9]. Moss-Salentijn et al[10] noted that the radiographic incidence of PSs tended to be lower than the histological incidence, attributed to the inability of radiographs to detect calcified structures smaller than 200 μm. Sayegh et al[11] further highlighted that PSs can range from 5 μm to several millimeters in diameter, often leading to their oversight by dentists who rely more on imaging than histological analysis. In this case, a single tooth exhibited anywhere from 1 to 7 or even more stones, varying in size from minute particles to large masses. These stones were found embedded, adherent, or free within the pulp chamber, displaying round, ovoid, or irregular shapes. To gain deeper insights into these stones, we pursued CBCT, enabling clear identification of stone number, positional relationships, size, morphology, and other relevant details. Thus, CBCT emerges as a superior method for PS detection compared to panoramic radiographs, offering greater specificity and accuracy, and overcoming the limitations of overlapping images[12]. Observations over a two-year period, especially in the mandibular wisdom teeth, revealed early-stage crown development alongside increasing deposition of irregularly scattered calculus within the pulp chamber. For instance, in the lower left second premolar, images from 2020 showed an oval PS at the root tip already reaching a significant size, with a maximum diameter of 6 mm, indicating its formation in the early stages of root development. Two years later, this PS was observed to be completely encapsulated by the developing root wall. Additionally, the presence of irregular calculus in the pulp cavity of tooth 85, along with normal root resorption, suggests that PS or calculus formation may have initiated during deciduous dentition without disrupting the normal alternation of deciduous and permanent teeth. This observation, combined with the tendency of other root apices to close or trend towards closure, suggests minimal adverse effects on root development.
PSs are more commonly found on the coronal side of the pulp chamber than in the root pulp cavity, appearing free, attached, or embedded in the canal wall[13]. This observation has been supported by recent studies, which indicate that the relatively high cellularity of the coronal pulp cavity makes it more prone to displaying nodular calcification around damaged cells, while the larger diameter of the vascular bundles and high collagen fiber content in the root pulp result in a more diffusely calcified appearance[4]. Although our case initially seemed to deviate from this pattern, further analysis reveals its consistency. On one hand, the early formation of PS aligns with the developmental timeline of dentin. On the other hand, given that the patient was in the replacement phase and exhibited coarse features in the root canal, resembling characteristics of the coronal pulp described in the study[4], especially in the molar areas where roots were tapered with no clear demarcation between coronal and root pulp cavities, PSs were distributed in the middle of the wider pulp cavity and near the coronal pulp cavity, presenting as irregularly shaped nodular calcified masses. Numerous factors contribute to the development of PSs, including age, genetic susceptibility, pulpal degeneration, circulatory disorders, periodontitis[14], orthodontic procedures[15], and interactions between pulpal mesenchymal tissue and epithelial cells[16,17], as well as idiopathic factors of unknown origin[18].
This case involves a 10-year-old girl in the periodontal phase, with no history of periodontal or orthodontic treatment, no parental history of PSs, and no systemic diseases. Despite presenting with endodontic disease, healthy teeth and unerupted permanent teeth also exhibited PSs in the pulp cavity, suggesting that her PSs may not be directly linked to the accompanying endodontic condition. This finding resonates with Yaacob et al[19]'s report, which concluded that the presence of caries does not significantly influence pulp calcification formation. While the exact etiology of PSs remains elusive, it is evident that their formation commences during the early stages of tooth development. Considering the atypical coronal morphology of the first molar, tapered single roots in all molars, congenital absence of the lower right second premolar, and irregular calcification of the pulp cavity in one of the retained deciduous teeth, it is plausible to hypothesize an idiopathic origin or early developmental anomaly contributing to multiple PSs throughout the oral cavity. For instance, mutations affecting papillae, critical determinants of tooth morphology, could result in altered or even absent tooth forms. Additionally, studies[20] have suggested a link between PSs throughout dentition and systemic syndromes or genetic diseases such as dentin dysplasia and dentinogenesis imperfecta in parents. However, further investigation and the application of molecular genetics are warranted to validate these hypotheses and potentially uncover underlying mechanisms.
The presence of large PSs presents a considerable challenge in the root canal treatment of such patients. It is crucial for dentists to utilize CBCT to accurately assess the three-dimensional position and size of PSs. Additionally, strategies for safely removing large PSs through minimally invasive procedures and reinforcing weakened root canal walls are avenues for further exploration.
| 1. | Langeland K, Rodrigues H, Dowden W. Periodontal disease, bacteria, and pulpal histopathology. Oral Surg Oral Med Oral Pathol. 1974;37:257-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 124] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | S N, Chandran A, B S, S G, A M, Muddebihal F, Nayyar AS. Pulp Stones: Diagnostic Significance in Early Diagnosis and Radiographic Correlation with Ischemic Heart Diseases. Indian J Radiol Imaging. 2021;31:277-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Jannati R, Afshari M, Moosazadeh M, Allahgholipour SZ, Eidy M, Hajihoseini M. Prevalence of pulp stones: A systematic review and meta-analysis. J Evid Based Med. 2019;12:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Palatyńska-Ulatowska A, Fernandes MC, Pietrzycka K, Koprowicz A, Klimek L, Souza RA, Pradebon M, de Figueiredo JAP. The Pulp Stones: Morphological Analysis in Scanning Electron Microscopy and Spectroscopic Chemical Quantification. Medicina (Kaunas). 2021;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Alciati A, Shiffer D, Dipaola F, Barbic F, Furlan R. Psychogenic Pseudosyncope: Clinical Features, Diagnosis and Management. J Atr Fibrillation. 2020;13:2399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Maikhuri B, Sahoo N, Jena S. Prevalence of Pulp Stones After Orthodontic Treatment A Review. J Pharma Nega Results. 2023;71-77. [DOI] [Full Text] |
| 7. | Milcent CPF, da Silva TG, Baika LM, Grassi MT, Carneiro E, Franco A, de Lima AAS. Morphologic, Structural, and Chemical Properties of Pulp Stones in Extracted Human Teeth. J Endod. 2019;45:1504-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Ivanauskaitė D, Kubiliūtė D, Janavičienė D, Brukienė V. Prevalence of pulp stones in molars based on bitewing and periapical radiographs. Stomatologija. 2021;23:9-15. [PubMed] |
| 9. | Ravichandran S, Vadivel JK. Prevalence of pulp stones in IOPA radiographs. J Adv Pharm Technol Res. 2022;13:S63-S66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Moss-Salentijn L, Klyvert MH. Epithelially induced denticles in the pulps of recently erupted, noncarious human premolars. J Endod. 1983;9:554-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Sayegh FS, Reed AJ. Calcification in the dental pulp. Oral Surg Oral Med Oral Pathol. 1968;25:873-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Hsieh CY, Wu YC, Su CC, Chung MP, Huang RY, Ting PY, Lai CK, Chang KS, Tsai YC, Shieh YS. The prevalence and distribution of radiopaque, calcified pulp stones: A cone-beam computed tomography study in a northern Taiwanese population. J Dent Sci. 2018;13:138-144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Moss-Salentijn L, Hendricks-Klyvert M. Calcified structures in human dental pulps. J Endod. 1988;14:184-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Chen G, Huang LG, Yeh PC. Detecting calcified pulp stones in patients with periodontal diseases using digital panoramic and periapical radiographies. J Dent Sci. 2022;17:965-972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 15. | Ertas ET, Veli I, Akin M, Ertas H, Atici MY. Dental pulp stone formation during orthodontic treatment: A retrospective clinical follow-up study. Niger J Clin Pract. 2017;20:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Wang Z, Chen C, Zhang J, He J, Zhang L, Wu J, Tian Z. Epithelium-derived SCUBE3 promotes polarized odontoblastic differentiation of dental mesenchymal stem cells and pulp regeneration. Stem Cell Res Ther. 2023;14:130. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Stenvik A, Mjör IA. Epithelial remnants and denticle formation in the human dental pulp. Acta Odontol Scand. 1970;28:72-78. [PubMed] |
| 18. | Ravanshad S, Khayat S, Freidonpour N. The Prevalence of Pulp stones in Adult Patients of Shiraz Dental School, a Radiographic Assessment. J Dent (Shiraz). 2015;16:356-361. [PubMed] |
| 19. | Yaacob HB, Hamid JA. Pulpal calcifications in primary teeth: a light microscope study. J Pedod. 1986;10:254-264. [PubMed] |
| 20. | Parekh S, Kyriazidou A, Bloch-Zupan A, Roberts G. Multiple pulp stones and shortened roots of unknown etiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e139-e142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |