Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5145
Revised: May 10, 2024
Accepted: June 3, 2024
Published online: August 6, 2024
Processing time: 130 Days and 19.6 Hours
With the popularization of various cerebrovascular imaging methods and increased attention to the field, more cerebrovascular diseases are being detected in asymptomatic patients. Different cerebrovascular diseases are typically isolated but occasionally occur simultaneously, causing difficulties in diagnosis and treatment. Morphological changes in the collateral circulation of blood vessels in chronic cerebral artery occlusion patients are slow and dynamic, intercepting morphological development at a specific moment. Excessive reliance on single imaging tests such as digital subtraction cerebral angiography (DSA) can lead to misdiagnosis.
We report a 52-year-old male who was admitted to our department for treatment of an unruptured aneurysm during a follow-up examination for brain trauma after 1 mo. Computed tomography (CT) scan was negative, but CT angiography (CTA) revealed a sac-like bulge at the bifurcation of the left middle cerebral artery. DSA revealed an unruptured aneurysm with unique scapular morphology. The stump of a middle cerebral artery occlusion was observed during exposure during aneurysm clipping surgery, and the diagnosis of chronic cerebral artery occlusion was confirmed intraoperatively. This case was confusing because of the peculiar morphology of the arterial stump and compensatory angiogenesis due to multiple cerebral artery stenoses observed on preoperative CTA and DSA. The surgery did not cause secondary damage to the patient, and medical treatment for risk factors was continued postoperatively.
Multiple cerebral arterial stenoses can occur in conjunction with aneurysms or arteriovenous malformations, and their unique morphology can lead to misdiagnosis.
Core Tip: We present an asymptomatic patient with chronic occlusion of the left middle cerebral artery who was diagnosed with an aneurysm at the bifurcation of the left middle cerebral artery. This case was confusing because of the peculiar morphology of the arterial stump and compensatory angiogenesis due to multiple cerebral artery stenoses observed on preoperative computed tomography angiography and digital subtraction cerebral angiography. In the absence of comprehensive preoperative imaging, the patient underwent aneurysm clipping, and chronic intracranial artery occlusion was confirmed intraoperatively. The importance of comprehensive imaging evaluations in the routine diagnosis of aneurysms was emphasized.
- Citation: Yang S, Mai RK. Mimicking aneurysm in a patient with chronic occlusion of the left middle cerebral artery: A case report. World J Clin Cases 2024; 12(22): 5145-5150
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5145.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5145
The risk factors for chronic cerebral artery occlusion include hypertension, diabetes, dyslipidemia and genetic factors. Approximately 6%–20% of cases of recurrent stroke symptoms on the same side can be attributed to this condition each year. The process of vascular occlusion is slow, and some patients remain asymptomatic because they are in the early stages of vascular occlusion or because of the development of a sufficient compensatory blood supply[1,2].
Typically, chronic vascular occlusion is defined as a disease that lasts for > 4 wk, and recanalization of chronic cerebral artery occlusion is a promising treatment for symptomatic patients. However, the duration of onset in asymptomatic patients is difficult to determine, and other intracranial vascular diseases may be involved. Currently, the commonly used clinical examination methods include computed tomography angiography (CTA)/magnetic resonance imaging (MRI) and digital subtraction cerebral angiography (DSA). DSA is considered to be the most important diagnostic tool because of its high resolution, real-time imaging, vascular pathway mapping, and interventional capability at the time of diagnosis. However, because of the over-reliance on DSA and the neglect of other comprehensive assessments, the unique morphology of the residual lumen at a specific moment and anatomical location may lead to misdiagnosis and incorrect treatment in rare cases.
A 52-year-old male was found to have an unruptured aneurysm of the left middle cerebral artery during a follow-up examination for brain trauma after 1 mo.
CTA at a local hospital suggested an aneurysm at the bifurcation of the left middle cerebral artery.
One month prior, the patient was hospitalized for > 1 wk because of craniocerebral injury and traumatic subarachnoid hemorrhage caused by an accidental fall, and medication was administered as symptomatic treatment. He was discharged after CT re-examination, which revealed absorption of the intracranial hemorrhage, and remission of clinical symptoms such as headache, dizziness and nausea. The latest CT scan 2 d prior showed that the intracranial condition was stable, and CTA revealed an aneurysm of the left middle cerebral artery bifurcation. He was admitted to our department for further treatment of the intracranial aneurysm.
The patient had hypertension for > 10 years and diabetes for 8 years, and he took amlodipine and valsartan daily to control blood pressure, and metformin and glimepiride daily to control blood sugar. Nine months ago, he underwent balloon dilation surgery for distal stenosis of the left anterior descending artery caused by coronary heart disease.
On physical examination, the vital signs were as follows: Body temperature, 36.5 °C; blood pressure, 120/95 mmHg; heart rate, 82 beats/min; and respiratory rate, 19 breaths/min. No abnormalities were observed on cranial nerve examination, physiological reflexes were normal, and pathological reflexes were negative.
The laboratory examination results were as follows: fasting blood glucose, 4–5 mmol/L; postprandial blood glucose, 6–8 mmol/L; glycated hemoglobin, 6.5%; blood urea nitrogen, 8.91 mmol/L; creatinine, 119.02 μmol/L; uric acid, 524.59 μmol/L; and homocysteine, 16.49 μmol/L. No other abnormalities were found in routine blood and urine analyses.
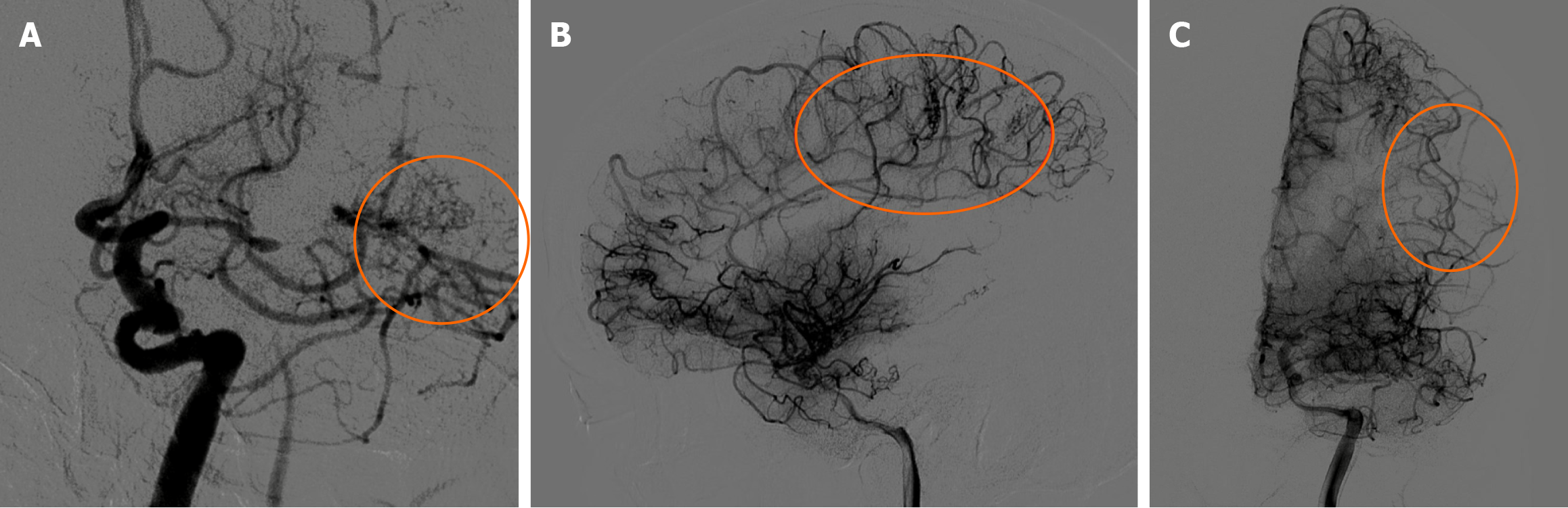
Head CTA and whole cerebral DSA revealed left middle cerebral artery stenosis and an aneurysm of the left middle cerebral artery bifurcation (Figure 1). Arteriosclerotic plaques and compensatory vascular network formation in multiple brain arteries were observed.
Chronic left middle cerebral artery occlusion.
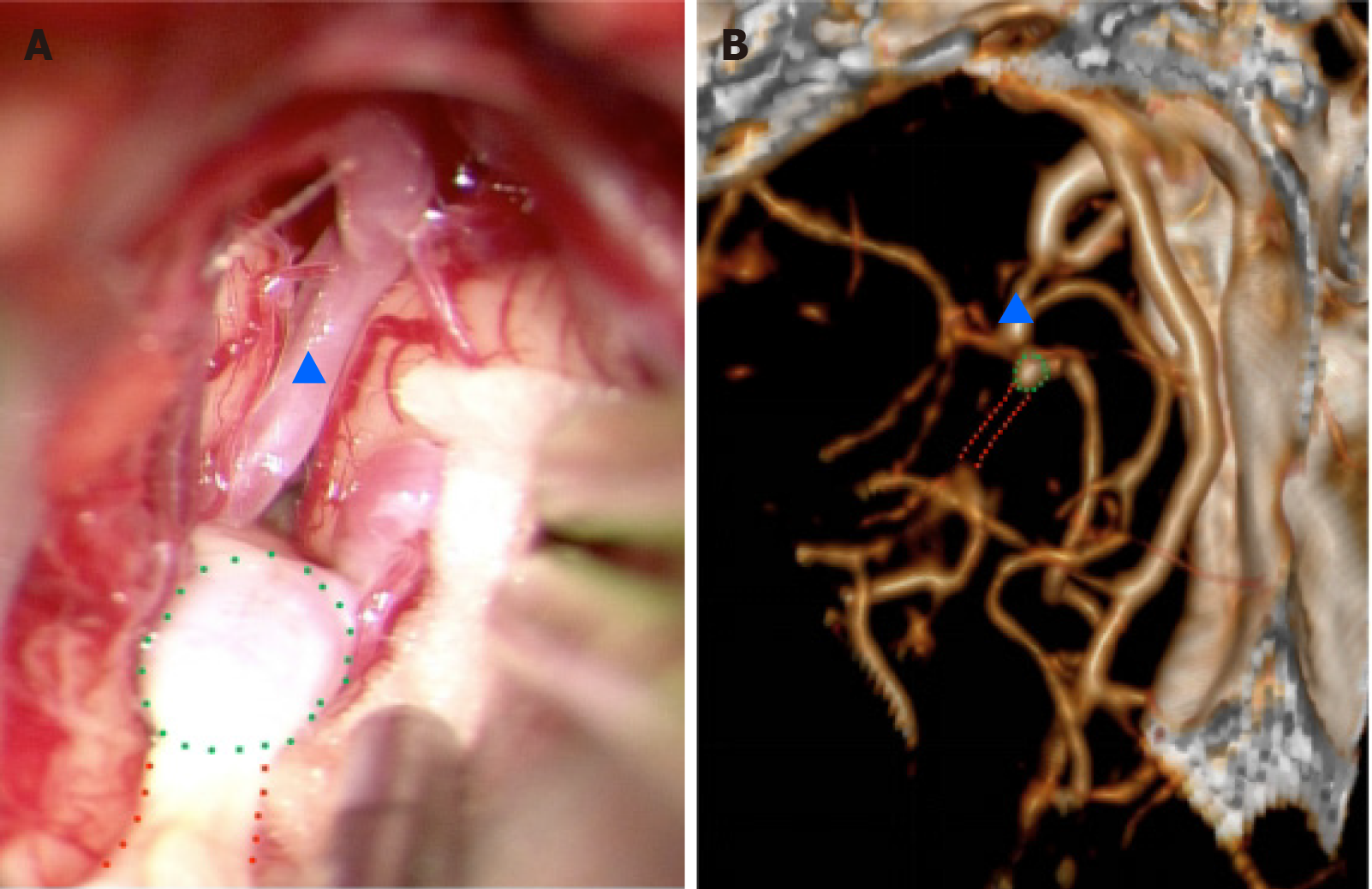
The patient underwent left middle cerebral aneurysm clipping surgery under venous and inhaled compound anesthesia. Craniotomy was performed using the pterygoid approach; cerebrospinal fluid was released along the lateral fissure under microscopy; the false bifurcation of the middle cerebral artery was gradually exposed; and no aneurysm was found during the operation. Thick, white, cord-like, tough tissue was observed in the corresponding region, with a few nourishing blood vessels on the surface. The distal end of the artery was anastomosed with smaller arterioles in the lateral fissure, and the proximal end was partially enlarged and connected to the M1 portion of the middle cerebral artery (Figure 2). No further surgical procedures were performed, and the surgery was terminated according to the typical procedure.
Postoperatively, the patient experienced no complications and recovered well. The patient was discharged on post
This patient had a medical history that included hypertension, hyperglycemia, prolonged duration of chronic renal insufficiency, and coronary heart disease. These risk factors may play a role in the development of intracranial vascular stenosis, acute and chronic occlusion, and aneurysms. These pathological changes might occur simultaneously, which can cause challenges in diagnosis and treatment, and the treatment option is primarily determined by the patient's clinical presentation.
Once symptomatic cerebral artery stenosis with intracranial aneurysm is diagnosed, the narrowed vessels are typically the primary focus[3,4]. Notably, endovascular treatment does not significantly increase the risk of aneurysm rupture[5]. Treatment of the aneurysm should take precedence[6,7] when cerebral artery stenosis is asymptomatic or exhibits high-risk signs, such as an aneurysm > 7 mm, corresponding to exacerbated neurological symptoms and irregular morphology[8-10]. The patient's chronic cerebral artery stenosis was considered asymptomatic because there was no history of cerebral infarction and no prior encephalomalacia detected by head MRI. DSA showed that the proximal vascular condition of the M1 segment of the left middle cerebral artery was not ideal for interventional treatment, and the systemic condition was good; therefore, craniotomy aneurysm clipping surgery was performed.
During the operation, the distal end of the M1 segment of the middle cerebral artery was observed to have a cord-like appearance and was waxy yellow in color and hard in texture, consistent with the changes observed in atherosclerosis. The occlusion extended to the lateral fissure and connected with other blood vessels with a few small trophic blood vessels on its surface. The proximal end of the middle cerebral artery occlusion appeared sac-like and dilated, which was consistent with the DSA changes that had been misdiagnosed as an aneurysm. The correct diagnosis in this case was highly obscured because the chronic complete occlusion resulted in a blunt stump with compensating thickened branch vessels, which gave the appearance of a typical middle cerebral artery bifurcation aneurysm. The absence of a threadlike blood flow and distal true lumen visibility of the occluded lesion contributed to its camouflage.
The majority of current research efforts are focused on investigating the development and collateral circulation mechanisms of chronic cerebral artery stenosis and occlusion and assessing the efficacy of both pharmaceutical and surgical treatments. Common clinical diagnostic methods, including CTA, magnetic resonance angiography (MRA), and transcranial doppler, provide multiple perspectives for assessing blood vessel conditions[11,12]. However, DSA continues to be the benchmark for precise diagnosis.
The diagnostic process and treatment of this patient produced several notable insights. In asymptomatic patients with multiple cerebral arterial stenoses or occlusions, special attention should be given to the mode of compensation[13]. Successful compensatory collateralization is considered a defensive measure against ischemic stroke or hemorrhage and is achieved through three primary routes: (1) The leptomeningeal anastomosis branch of the cerebral cortex, which plays the most important role; (2) the dural–leptomeningeal branch of the external carotid artery; and (3) the perforator artery and neovascularization[14]. DSA of this patient revealed significant thickening and lengthening of the anterior cerebral artery, with distal branches extending into the blood supply area of the middle cerebral artery (Figure 3). The dural–leptomeningeal branch mainly consists of the middle meningeal artery and the meningeal branch of the occipital artery, while the perforator arteries mainly depend on the Heubner reentrant artery and the proximal part of the anterior cerebral artery[15]. The presence of these two modalities and neovascularization were not observed in this patient.
The occlusion process is chronic and irreversible, and the morphological changes in the occluded blood vessels and collateral circulation are dynamic[16,17]. Intercepting the morphology at a specific moment is the main cause of misdiagnosis. DSA revealed that the M1 segment of the left middle cerebral artery was significantly shorter, and once the stump (
CTA and MRA are suitable in most clinical scenarios, but they have limitations in regard to providing specific details about areas that lack blood flow, such as occluded arterial segments, and the properties of the blood vessel wall. DSA is a widely accepted gold standard and requires extra attention in the diagnosis of other vascular lesions, such as multiple cerebral vascular stenoses combined with acute or chronic vascular occlusion. Tapered stumps or crater-like changes can often be observed in acute occlusions, while morphological characteristics of the chronic phase have not been systematically described. Overreliance on DSA and the neglect of other comprehensive assessments may lead to misdiagnosis and incorrect treatment.
The occlusion process of cerebral vessels is chronic and irreversible, and morphological changes in the vessel stump can be described as tapered, blunt or invisible. In this patient, a blunt stump was located in the middle cerebral artery with compensated thickened branch vessels, which resembled a typical middle cerebral artery bifurcation aneurysm. Diagnosis based solely on the morphology of the aneurysm is not dependable, especially for patients with additional cerebrovascular abnormalities. With the development and refinement of conventional MRAs, such as 3D time-of-flight MRA, contrast-enhanced MRA, and noncontrast 3D-multiple-echo recalled gradient echo, the diagnosis of chronic occlusion of intracranial medium- and small-diameter blood vessels will be more accurate[18-20]; when performed as a supplement to DSA examination, similar misdiagnoses can be prevented.
The authors are grateful to the patient in this study for his collaboration.
| 1. | Dong J, Ma Y, Chen Y, Guo J, Zhang T, Yang T, Zhang H, Yan F, Han L. Prevalence and influencing factors of patient delay in stroke patients: a systematic review and meta-analysis. Neurosurg Rev. 2024;47:202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 2. | Flaherty ML, Flemming KD, McClelland R, Jorgensen NW, Brown RD Jr. Population-based study of symptomatic internal carotid artery occlusion: incidence and long-term follow-up. Stroke. 2004;35:e349-e352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 131] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Jou LD, Shaltoni HM, Morsi H, Mawad ME. Hemodynamic relationship between intracranial aneurysm and carotid stenosis: review of clinical cases and numerical analyses. Neurol Res. 2010;32:1083-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Héman LM, Jongen LM, van der Worp HB, Rinkel GJ, Hendrikse J. Incidental intracranial aneurysms in patients with internal carotid artery stenosis: a CT angiography study and a metaanalysis. Stroke. 2009;40:1341-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Dornbos D 3rd, Katz JS, Youssef P, Powers CJ, Nimjee SM. Glycoprotein IIb/IIIa Inhibitors in Prevention and Rescue Treatment of Thromboembolic Complications During Endovascular Embolization of Intracranial Aneurysms. Neurosurgery. 2018;82:268-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Espinosa G, Dzieciuchowicz L, Grochowicz L. Endovascular treatment of carotid stenosis associated with incidental intracranial aneurysm. Ann Vasc Surg. 2009;23:688.e1-688.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Gallego León JI, Concepción Aramendía L, Ballenilla Marco F, Vázquez Suárez JC. Concomitant endovascular treatment of concomitant extracranial carotid stenosis and intracranial aneurysm. Our experience. Interv Neuroradiol. 2009;15:53-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Levinson S, Pendharkar AV, Gauden AJ, Heit JJ. Modern Imaging of Aneurysmal Subarachnoid Hemorrhage. Radiol Clin North Am. 2023;61:457-465. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Tawk RG, Hasan TF, D'Souza CE, Peel JB, Freeman WD. Diagnosis and Treatment of Unruptured Intracranial Aneurysms and Aneurysmal Subarachnoid Hemorrhage. Mayo Clin Proc. 2021;96:1970-2000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 109] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 10. | Mehta VA, Spears CA, Abdelgadir J, Wang TY, Sankey EW, Griffin A, Goodwin CR, Zomorodi A. Management of unruptured incidentally found intracranial saccular aneurysms. Neurosurg Rev. 2021;44:1933-1941. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Yuan HW, Ji RJ, Wang AL, Lin YJ, Chen HF, Xu ZQ, Peng GP, Luo BY. A Grading Scale for Pial Collaterals in Middle Cerebral Artery Total Occlusion Based on Time-of-flight MR Angiography Source Images. Magn Reson Med Sci. 2019;18:62-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Liang J, Guo J, Liu D, Shi C, Luo L. Application of High-Resolution CUBE Sequence in Exploring Stroke Mechanisms of Atherosclerotic Stenosis of Middle Cerebral Artery. J Stroke Cerebrovasc Dis. 2019;28:156-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Liu ZW, Han C, Zhao F, Qiao PG, Wang H, Bao XY, Zhang ZS, Yang WZ, Li DS, Duan L. Collateral Circulation in Moyamoya Disease: A New Grading System. Stroke. 2019;50:2708-2715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 14. | Fanou EM, Knight J, Aviv RI, Hojjat SP, Symons SP, Zhang L, Wintermark M. Effect of Collaterals on Clinical Presentation, Baseline Imaging, Complications, and Outcome in Acute Stroke. AJNR Am J Neuroradiol. 2015;36:2285-2291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 15. | Han C, Li ML, Xu YY, Ye T, Xie CF, Gao S, Duan L, Xu WH. Adult moyamoya-atherosclerosis syndrome: Clinical and vessel wall imaging features. J Neurol Sci. 2016;369:181-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, Wang Y, Zou X, Leung TW, Cai Y, Bai Q, Wu Y, Wang C, Pan X, Luo B, Wong KS; CICAS Study Group. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. 2014;45:663-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 535] [Article Influence: 48.6] [Reference Citation Analysis (0)] |
| 17. | Xu B, Li C, Guo Y, Xu K, Yang Y, Yu J. Current understanding of chronic total occlusion of the internal carotid artery. Biomed Rep. 2018;8:117-125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Wang E, Shao S, Li S, Yan P, Xiang Y, Wang X, Li J, Wang G, Sun Q, Du Y. A High-Resolution MRI Study of the Relationship Between Plaque Enhancement and Ischemic Stroke Events in Patients With Intracranial Atherosclerotic Stenosis. Front Neurol. 2018;9:1154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Dieleman N, Yang W, Abrigo JM, Chu WC, van der Kolk AG, Siero JC, Wong KS, Hendrikse J, Chen XY. Magnetic Resonance Imaging of Plaque Morphology, Burden, and Distribution in Patients With Symptomatic Middle Cerebral Artery Stenosis. Stroke. 2016;47:1797-1802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 20. | Zhang J, Ding S, Zhao H, Sun B, Li X, Zhou Y, Wan J, Degnan AJ, Xu J, Zhu C. Evaluation of chronic carotid artery occlusion by non-contrast 3D-MERGE MR vessel wall imaging: comparison with 3D-TOF-MRA, contrast-enhanced MRA, and DSA. Eur Radiol. 2020;30:5805-5814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |