Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5108
Revised: May 27, 2024
Accepted: June 14, 2024
Published online: August 6, 2024
Processing time: 71 Days and 21.3 Hours
Acupuncture (AT) is widely used in treatment of ovulatory disorder infertility (ODI), but the safety and efficacy of AT for ODI still lack an evidence-based basis.
To evaluate the feasibility and effectiveness of AT as an adjunct intervention for ODI.
The Cochrane Library, Embase, PubMed, VIP, China National Knowledge Infrastructure, WanFang Data, and Chinese biomedical literature databases were searched from inception to January 20, 2024. Two reviewers independently selected studies, collected data, and evaluated methodological quality through the Cochrane Risk of Bias tool. Revman 5.4 was used for meta-analysis, and the Grade system was performed to evaluate the level of evidence for the outcomes of the meta-analysis.
A total of 20 randomized controlled trials with 1677 ODI patients were included. Compared with the clomiphene citrate (CC) group, the AT plus CC group exhi
AT can improve the pregnancy outcomes and sex hormone levels for patients with ODI. However, further studies are needed to confirm these findings.
Core Tip: Ovulation dysfunction is the most common cause of infertility. This meta-analysis aimed to evaluate the feasibility and effectiveness of acupuncture as an adjunctive intervention to ovulatory disorder infertility (ODI). The results showed that acupuncture effectively improved pregnancy outcomes and sex hormone levels in patients with ODI, indicating its potential as a treatment strategy for ODI. However, further studies are needed to confirm these findings.
- Citation: Chen YQ, Shen T, Lv Y, Shen MH. Feasibility of acupuncture as an adjunct intervention for ovulatory disorder infertility: A systematic review and meta-analysis. World J Clin Cases 2024; 12(22): 5108-5123
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5108.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5108
Infertility is defined as the failure of a couple of reproductive age to achieve pregnancy after 12 mo of regular unprotected sexual intercourse[1]. For couples over the age of 35, this timeframe is reduced to 6 mo or six menstrual cycles. According to the World Health Organization, ovulation dysfunction is the most common cause of infertility, accounting for approximately 25% of infertility diagnoses[2]. In China, ovulation disorders are responsible for 29.78% of infertility diagnoses[3]. The main mechanism of anovulation and infertility is ovulation disorder caused by abnormal neuroendocrine regulation of the hypothalamic-pituitary-ovarian axis (HPO). The current treatment for ovulatory disorder infertility (ODI) primarily involves induction of ovulation to increase the chances of pregnancy[4].
Clomiphene citrate (CC) is a first-line ovulation induction drug, and it often leads to high output and low pregnancy in clinical application[5]. Long-term oral administration can result in side effects such as ovarian hyperstimulation syndrome (OHSS) and luteinized unruptured follicle syndrome as well as an increased risk of multiple pregnancies, birth defects, and abnormal epigenetic modifications. Moreover, using CC orally for more than 6 mo raises the risk of ovarian cancer[6]. This brings trouble and challenge to the clinical application of CC in the treatment of infertility through ovulation induction. Therefore, identifying effective assisted reproductive techniques to enhance the pregnancy success rate for ODI patients becomes crucial and urgent.
Acupuncture (AT) has garnered attention as a potential treatment for ODI. A 2010 study conducted in the United States revealed that 29% of 428 infertile couples chose complementary and alternative therapies to address their fertility issues. Among these therapies, AT was utilized by 23% and emerged as the most popular alternative approach[7]. Recent clinical randomized trials (RCTs) have demonstrated that AT can stimulate ovulation and enhance reproductive function[8-10]. The potential mechanisms underlying the effectiveness of AT in treating ODI include regulation of the HPO, reduction of inflammation-induced inhibition on follicular development, modulation of Kisspeptin expression levels, improvement of endometrial receptivity, and increased pregnancy rate[11-13].
The limited evidence from a previous meta-analysis compared AT alone or combined with CC for ODI showed no significant improvement in the rate of pregnancy and ovulation, without any observed reduction in miscarriage rate. Notably, this meta-analysis neither analyzed the impact of AT on sex hormone levels nor included an adequate number of studies with satisfactory methodological quality[13]. Therefore, this study aimed to conduct a more comprehensive meta-analysis by combining recently published RCTs to explore the feasibility and effectiveness of using AT for ODI.
This review was performed following PRISMA guidelines[14] and was registered with INPLASY (registration number: INPLASY202340088, https://inplasy.com/inplasy-2023-4-0088/).
Cochrane Library, Embase, PubMed, VIP, China National Knowledge Infrastructure, WanFang Data, and Chinese biomedical literature databases were searched from inception to January 20, 2024. The retrieval strategy was determined after several preliminary searches using a combination of subject terms and free words. The search terms used were “acupuncture,” “ovulation disorders,” and “infertility.” Table 1 summarizes the search strategy for PubMed, with adjustments made for other electronic databases based on their specifications. The search strategies were shown in the supplementary material.
| Search | Terms |
| 1 | “Infertility” (MeSH Terms) |
| 2 | “Infertility” (Title/Abstract) OR “Infertile” (Title/Abstract) OR “Sterility” (Title/Abstract) OR “Sterile” (Title/Abstract) |
| 3 | 1 OR 2 |
| 4 | “Anovulation” (MeSH Terms) |
| 5 | “Ovulatory dysfunction” (Title/Abstract) OR “Anovulation” (Title/Abstract) OR “Anovulatory” (Title/Abstract) OR “Ovulatory disorders” (Title/Abstract) OR “Ovulation failure” (Title/Abstract) OR “Ovarian stimulation” (Title/Abstract) OR “Ovarian induction” (Title/Abstract) |
| 6 | 4 OR 5 |
| 7 | “Acupuncture” (MeSH Terms) |
| 8 | “Acupuncture” (Title/Abstract) OR “Acupuncture Therapy” (Title/Abstract) OR “Auricular Points” (Title/Abstract) OR “Ear acupuncture” (Title/Abstract) OR “Electroacupuncture” (Title/Abstract) OR “Electro-acupuncture” (Title/Abstract) OR “Meridians” (Title/Abstract) OR “Acupuncture Points” (Title/Abstract) OR “Acupressure” (Title/Abstract) OR “Auricular” (Title/Abstract) OR “Acusector” (Title/Abstract) OR “Needle” (Title/Abstract) OR “Fire Needle” (Title/Abstract) “Acupoint catgut embedding” (Title/Abstract) OR “Moxibustion” (Title/Abstract) OR “Scalp acupuncture points” (Title/Abstract) OR “Bleeding” (Title/Abstract) OR “Acupoint injection” (Title/Abstract) OR “Needle knife” (Title/Abstract) |
| 9 | 7 OR 8 |
| 10 | (“Randomized controlled trial” (Publication Type) OR “Controlled clinical trial” (Publication Type) OR “Randomized” (Title/Abstract) OR “Placebo” (Title/Abstract) OR “Clinical trials as topic” (MeSH Terms) OR “Randomly” (Title/Abstract) OR “Trial” (Title)) NOT “Animals” (MeSH Terms) NOT “Humans” (MeSH Terms) |
| 11 | 3 AND 6 AND 9 AND 10 |
The inclusion criteria were: (1) Participants (P). Patients diagnosed with ODI. The diagnostic criteria were followed by the Obstetrics and Gynecology, published by the People’s Medical Publishing House in 2013[15] and Guiding Principles for Clinical Research on New Chinese Medicines, published by the China Pharmaceutical Science and Technology Press in 2002[16]; (2) Intervention (I). Intervention groups received AT alone or combined with CC; (3) Control (C). Control groups should be CC; (4) Outcome (O). Outcomes included ovulation rate, pregnancy rate, miscarriage rate, follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), progesterone (P), thickness of endometrium, and adverse events; and (5) Study (S). RCTs.
Exclusion criteria: (1) Not RCTs, including animal studies, review articles, and case reports; (2) Repeat published studies; (3) Patients who do not meet the diagnostic criteria for ODI; (4) Use of other drugs that may affect ovulation; and (5) Studies with no reported relevant data.
Two researchers (Chen YQ and Shen T) independently reviewed the titles and abstracts of identified trials and excluded irrelevant literature. Any uncertainties were resolved through a detailed examination of the full text, followed by data extraction and cross-verification. Potential conflicts were addressed through discussion with a third researcher (Lv Y). The extracted information included details such as first author, publication date, sex distribution, sample size, age range, intervention measures, outcomes, etc. The Cochrane Collaboration tool was used to evaluate the quality of the included studies. The content included the random sequence, allocation concealment, blinding (including blinding of researchers and participants, and blind evaluation of study results), the integrity of the results, selective reporting of study results, and other bias. Each item was judged by low risk, high risk, and unclear.
The Revman 5.4 software was used for meta-analysis. Relative risk (RR) was employed as the effect indicator for binary variables, and mean difference (MD) was utilized as the effect indicator for continuous variables. For each effect size, its point estimate and a 95% confidence interval (CI) were presented. A heterogeneity test was performed by χ2 test, and the test level was P = 0.05. The studies showed no statistical heterogeneity (P > 0.10, I2 < 50%), thus the fixed-effect model was applied for analysis; otherwise, the random-effects model was used instead. If more than ten trials were included, publication bias was analyzed by funnel plot. To determine whether the type of experimental intervention (AT plus CC vs CC or AT vs CC) affected the efficacy of AT, we planned to perform a subgroup meta-analysis. The grade guideline was performed to summarize the quality of evidence for the outcomes of the meta-analysis.
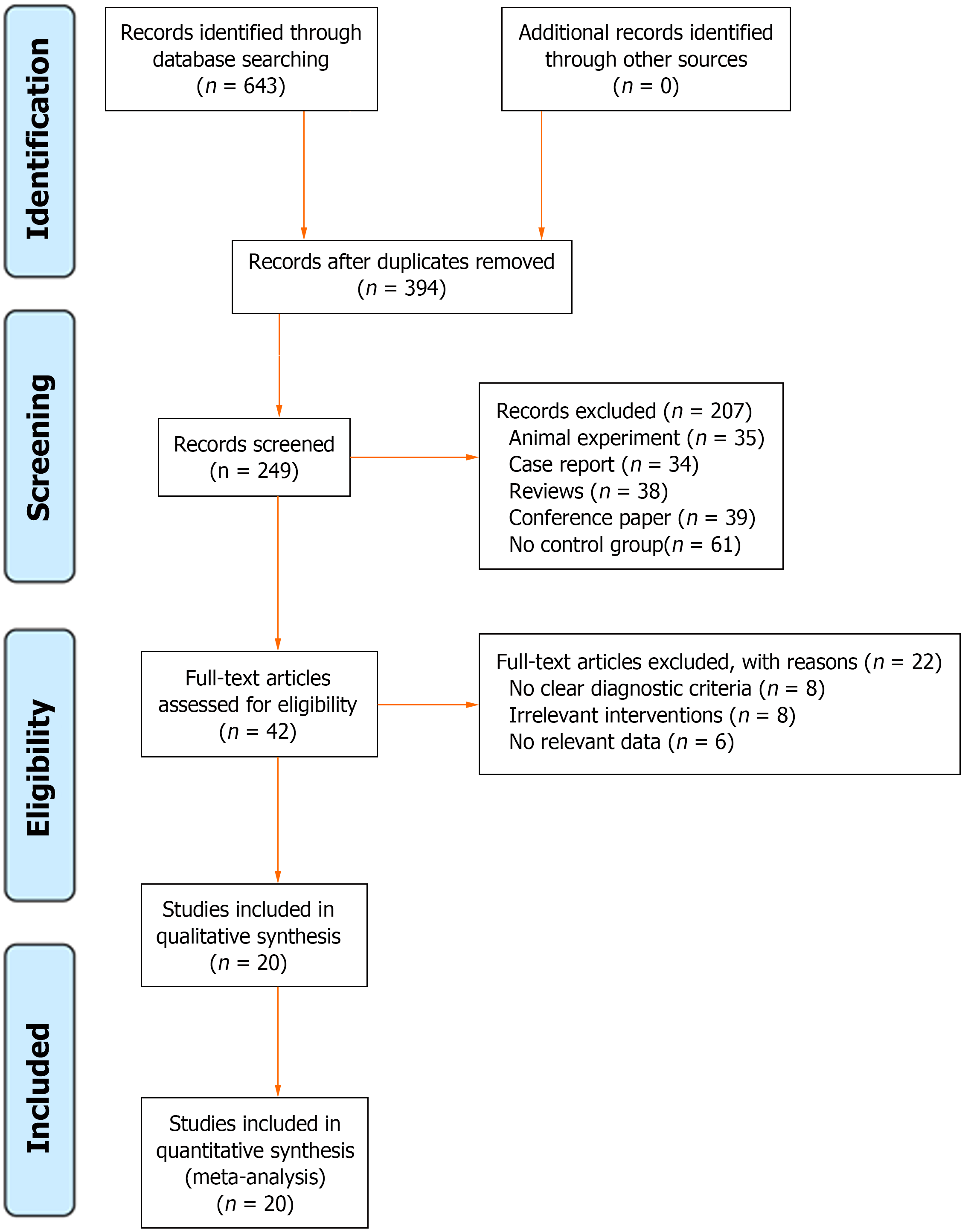
A total of 643 potentially eligible studies were collected, and 249 duplicate studies were removed by Endnote 20. According to the inclusion and exclusion criteria, 207 studies were removed after screening by title and abstract. After reading the full text, 42 studies were deleted, and 20 studies were finally included[17-36]. The literature screening process is shown in Figure 1.
Twenty trials with 1677 patients were included. There were 840 patients in the treatment group and 827 patients in the control group. The minimum sample size was 52 and the maximum was 179. The included trials varied in terms of outcomes, including pregnancy rate[17,18,20-23,25-36], ovulation rate[19,21-23,25,26,28,30-33,35], miscarriage rate[20,21,23,26,28-30,32,34-36], FSH levels[17-19,22,24,25,28,33], LH levels[17-19,22,24,25,28,33], E2 levels[18,19,22,24,25,28,33], P levels[17-19,25], thickness of endometrium[22,24,25,27,28,32-34,36], and adverse events[25-28,33,34]. Detailed characteristics of the studies are shown in Table 2.
| Ref. | Sample size | Mean age in yr | Course of disease in yr | Intervention | Details of AT | Acupoint | Comparison | Duration | Outcomes |
| Su et al[17], 2022 | T: 30, C: 30 | T: 29.50 ± 2.50, C: 28.45 ± 2.50 | NR | AT plus CC | Every other day, 5 consecutive times/starting on day 5 after the end of menstruation | RN4, RN6, Zigong, BL23, BL31, BL32, BL33, BL34, SP6 | CC, 50 mg/tid, for 5 d, starting on day 5 after the end of menstruation | 4 MC | 1,4,5,7 |
| Zhu and Xiang[18], 2022 | T: 47, C: 51 | T: 30 ± 3, C: 29 ± 3 | T: 2.41 ± 1.37, C: 2.39 ± 1.42 | AT plus CC | 30 min, each day/until 1 wk before the next MC | RN4, Zigong, SP10, GV4, BL23, BL32, ST36, SP6, KI1, KI3, PC8 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1,4,5-7 |
| Cui et al[19], 2022 | T: 28, C: 28 | T: 26.53 ± 3.11, C: 26.25 ± 3.01 | T: 2.09 ± 0.29, C: 2.05 ± 0.27 | AT plus CC | Starting on day 4 after the end of menstruation | BL31, BL32, BL33, BL34 | CC, 50 mg/qd, for 5 d, starting on day 4 after the end of menstruation | 3 MC | 2,4-7 |
| Li[20], 2015 | T: 51, C: 51 | T: 23.2 ± 0.5, C: 2.0 ± 0.6 | T: 23.4 ± 0.6, C: 2.2 ± 0.9 | AT | 30 min, each day, for 10 d/starting on day 5 after the end of menstruation | RN3, RN4, RN8, ST36, Zigong, SP6 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1,3 |
| Song et al[21], 2008 | T: 60, C: 60 | T: 28.60 ± 3.74, C: 28.30 ± 3.67 | T: 3.75 ± 1.94, C: 3.69 ± 1.83 | AT | 30 min, each day, for 10 d/starting on day 5 after the end of menstruation | RN3, RN4, RN8, Zigong, ST36, SP6 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1-3 |
| Zhang[22], 2019 | T: 53, C: 53 | T: 29 ± 4, C: 29 ± 4 | T: 3.50 ± 0.43, C: 3.47 ± 0.41 | AT plus CC | Starting on day 5 after the end of menstruation, every other day/until the next MC | BL23, GV4, RN3, RN4, ST25, ST29, SP6 | CC, 50 mg/tid, for 5 d, starting on day 2-5 after the end of menstruation or day 6 of withdrawal bleeding | 3 MC | 1,2,4-6,8 |
| Amina·and Yang[23], 2011 | T: 66, C: 66 | NR | NR | AT | 30 min, each day, for 10 d/starting on day 5 after the end of menstruation | RN3, RN4, Zigong, ST36, SP6 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1-3 |
| Zhong and Chen[24], 2017 | T: 38, C: 38 | T: 30.84 ± 1.64, C: 31.02 ± 1.56 | T: 7.30 ± 1.27, C: 7.23 ± 1. 31 | AT plus CC | 30 min, each day, for 10 d/starting on day 5 after the end of menstruation | RN3, RN4, RN8, SP6, Zigong, ST36, LR3, KI3 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 2 MC | 4-6,8 |
| Yuan[25], 2022 | T: 36, C: 36 | T: 27.19 ± 2.58, C: 27.67 ± 2.74 | T: 3.33 ± 1.88, C: 3.19 ± 1.26 | AT | 30 min, 6 times per week /starting on day 5 after the end of menstruation | RN4, RN5, BL20, BL23, SP6 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1,2,4-9 |
| Zheng[26], 2019 | T: 35, C: 35 | T: 30.24 ± 3.05, C: 29.25 ± 3.53 | T: 27.59 ± 12.20 m, C: 27.03 ± 11.34 m | AT plus CC | 30 min, every other day/starting on day 5 after the end of menstruation | ST25, ST36, RN3, RN4, RN5, SP6, K13, BL20, BL23, LR03 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1-3,9 |
| Zhu[27], 2017 | T: 30, C: 30 | T: 32.17 ± 3.23, C: 33.07 ± 3.13 | T: 5.23 ± 3.21, C: 5.73 ± 2.10 | AT plus CC | 30 min, each day/starting on day 5 after the end of menstruation | ST25, ST28, ST36, SP6, RN7, RN9 | CC, 50 mg/qd, for 3 d, starting on day 5 after the end of menstruation | 3 MC | 1,8,9 |
| Su[28], 2016 | T: 33, C: 33 | T: 31.00 ± 4.57, C: 29.83 ± 4.99 | NR | AT | 20-30 min, once every 3 d/starting on day 5 after the end of menstruation | RN10, RN12, RN4, RN5, ST28, Zigong | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1-6,8,9 |
| Liu[29], 2018 | T: 26, C: 26 | T: 32.1 ± 5.5,C: 31.5 ± 5.8 | T: 3.4 ± 1.1, C: 3.2 ± 1.2 | AT plus CC | 30 min, each day, for 7 d/starting on day 5 after the end of menstruation | RN8, Zigong, RN4, RN3, SP6, ST36 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1,3 |
| Wang[30], 2014 | T: 50, C: 50 | T: 28.70 ± 3.75, C: 28.40 ± 3.68 | T: 3.76 ± 1.95, C: 3.70 ± 1.85 | AT | 30 min, each day, for 10 d/starting on day 6 after the end of menstruation | RN4, RN8, SP6, Zigong, RN3 | CC, 50 mg/qd, for 5 d, starting on day 6 after the end of menstruation | 3 MC | 1-3 |
| Danniyaer[31], 2023 | T: 32, C: 32 | T: 33.93 ± 3.59, C: 34.14 ± 3.51 | T: 3.44 ± 1.12, C: 3.25 ± 1.17 | AT plus CC | Starting on day 5 after the end of menstruation | RN4, RN3, Zigong, ST36 | CC, 50 mg/qd, for 5 d, starting on day 5 after the end of menstruation | 3 MC | 1,2 |
| Zhai[32], 2016 | T: 30, C: 30 | T: 28.26 ± 3.96, C: 28.45 ± 3.87 | T: 3.37 ± 1.36, C: 3.52 ± 1.57 | AT plus CC | 20 min, each day, for 5 d/starting on day 5 after the end of menstruation | LI4, SP9, ST36, SP6 | CC, 50 mg/qd, for 5 d, starting on 5 after the end of menstruation | 3 MC | 1-3,8,9 |
| Wei et al[33], 2010 | T: 93, C: 86 | T: 33.0 ± 2.4, C: 31.0 ± 3.8 | T: 7.0 ± 1.5, C: 7.0 ± 1.1 | AT plus CC | 40 min, every other day/starting on day 5 after the end of menstruation | RN4, Zigong, SP10, SP6, KI3, ST36, LI4, LR3 | CC, 50 mg/qd, for 5 d, starting on 5 after the end of menstruation | 3 MC | 1,2,4-6,8,9 |
| Zhou[34], 2019 | T: 32, C: 32 | T: 26.97 ± 3.85, C: 27.50 ± 2.58 | T: 2.00 ± 1.58, C: 1.37 ± 0.81 | AT plus CC | 30 min, 3 times per week/starting on day 5 after the end of menstruation | RN4, RN3, Zigong, SP6 | CC, 50 mg/qd, for 5 d, starting on 5 after the end of menstruation | 3 MC | 1,3,8,9 |
| Zheng et al[35], 2007 | T: 40, C: 40 | T: 27.6 ± 7.6, C: 28.1 ± 7.4 | T: 3.7 ± 4.1, C: 3.8 ± 4.1 | AT | 30 min, starting on day 5 after the end of menstruation | RN8, RN3, RN4, Zigong, ST36, SP6 | CC, 50 mg/qd, for 5 d, starting on 5 after the end of menstruation | 3 MC | 1-3 |
| Zhou et al[36], 2018 | T: 30, C: 30 | T: 29.3, C: 29.3 | NR | AT | Each day, for 10 d/starting on day 5 after the end of menstruation | SP6, K17, BL23 | CC, 50-100 mg/qd, for 5 d, starting on 5 after the end of menstruation | 1 MC | 1,3,8 |
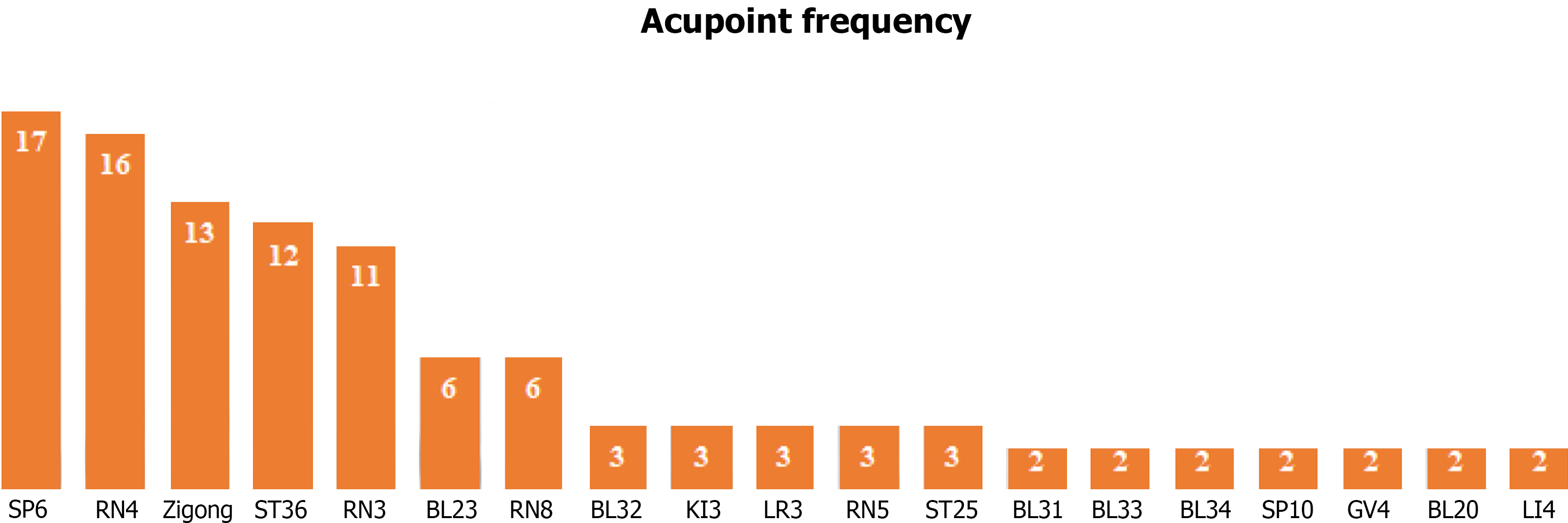
A total of 12 trials[17-19,22,24,26,27,29,31-34] used AT plus CC, and 8 trials[20,21,23,25,28,30,35,36] used AT. All included trials described acupoint selection. As shown in Figure 2, the top five acupoints with the highest frequency were Sanyinjiao (SP 6), Guanyuan (RN 4), Zigong, Zusanli (ST36), and Zhongji (RN 3). The residence time of the needle ranged from 20-40 min. The frequency of treatment was each day[18,20,21,23,24,27,29-32,35,36], every other day[17,22,26,33], once every 3 d[28], 3 times per week[34], and 6 times per week[25]. The duration of treatment was 2 to 4 menstrual cycles. A total of 20 trials highlighted Deqi, a unique AT sensation that is critical for clinical efficacy.
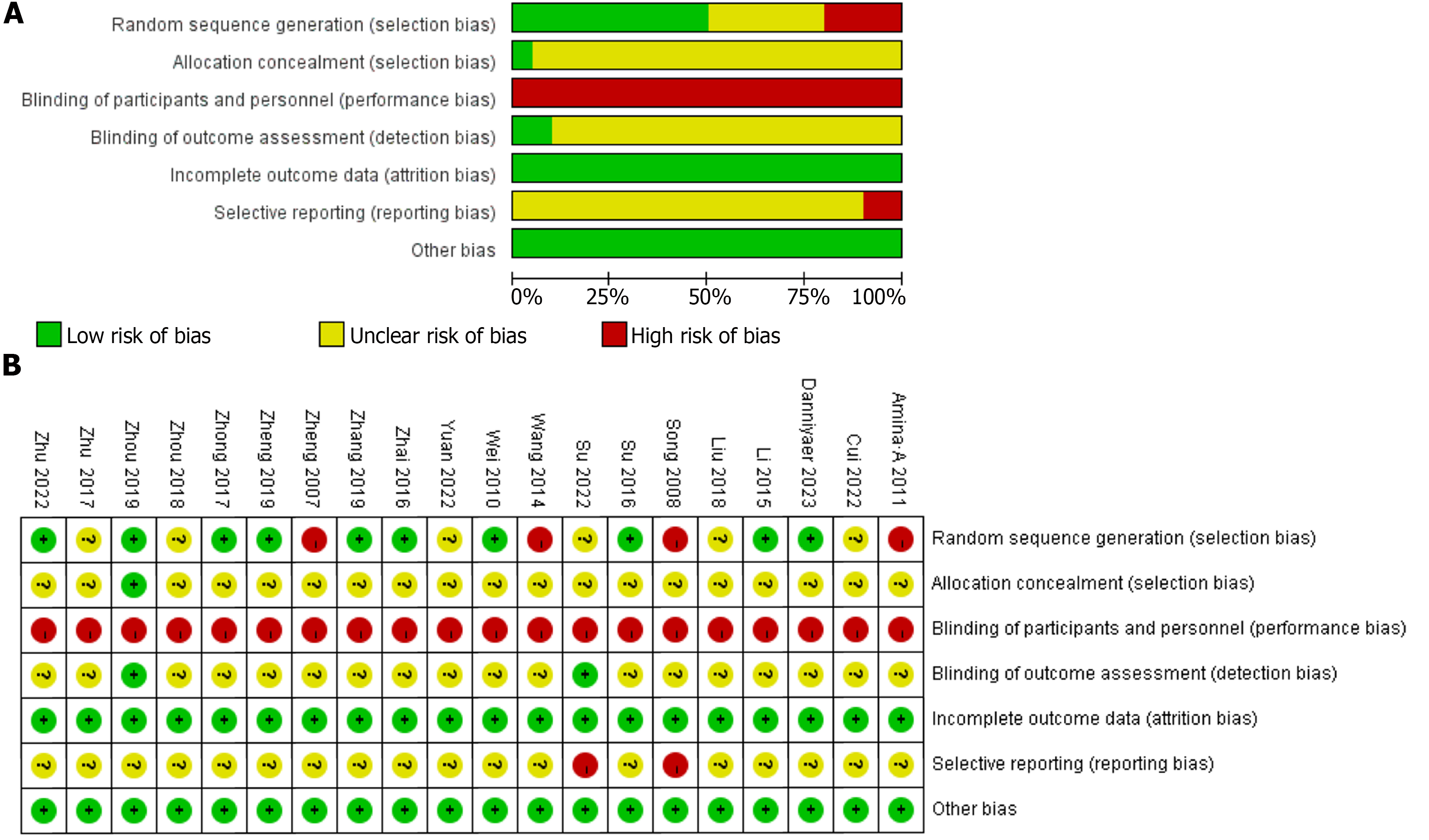
Among the included 20 trials, 10 trials[18,20,22,24,26,28,31-34] used the random number table method, 6 trials[17,19,25,27,29,36] only mentioned randomization without describing the specific randomization method, and 4 trials[21,23,30,35] used the order randomization method. Allocation concealment was mentioned in only one trial[34]. Blinding was reported in only two trials[17,34]. Two trials[17,21] reported selective reporting. Figure 3 illustrates the risk of bias in included trials.
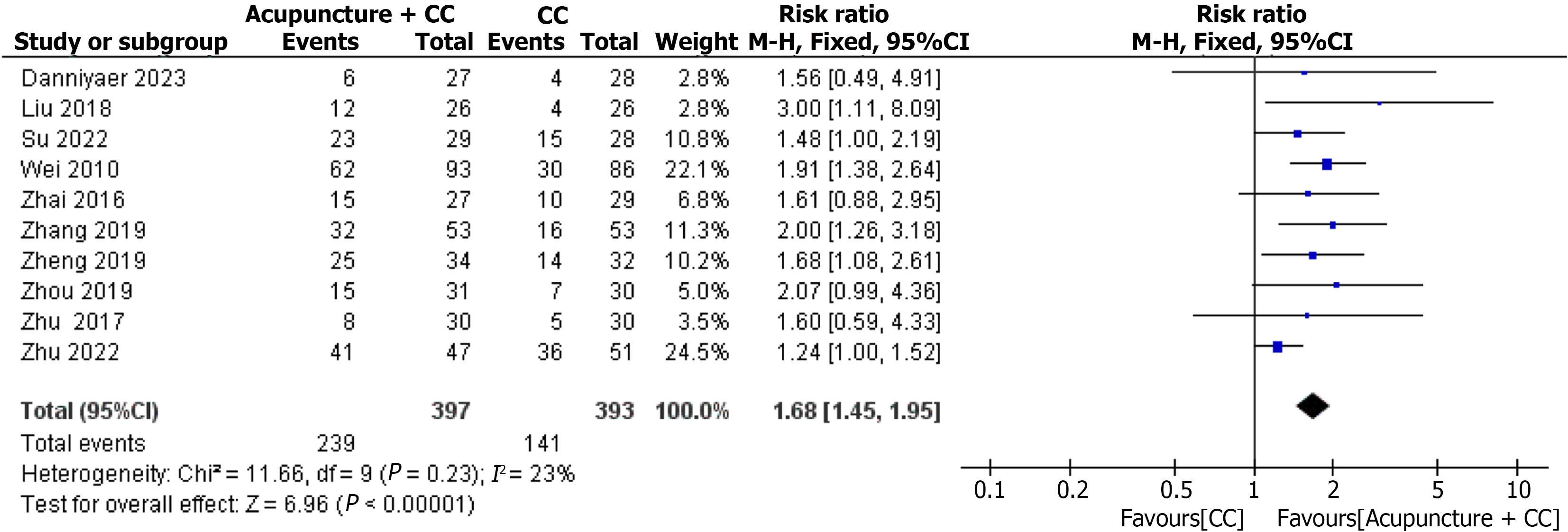
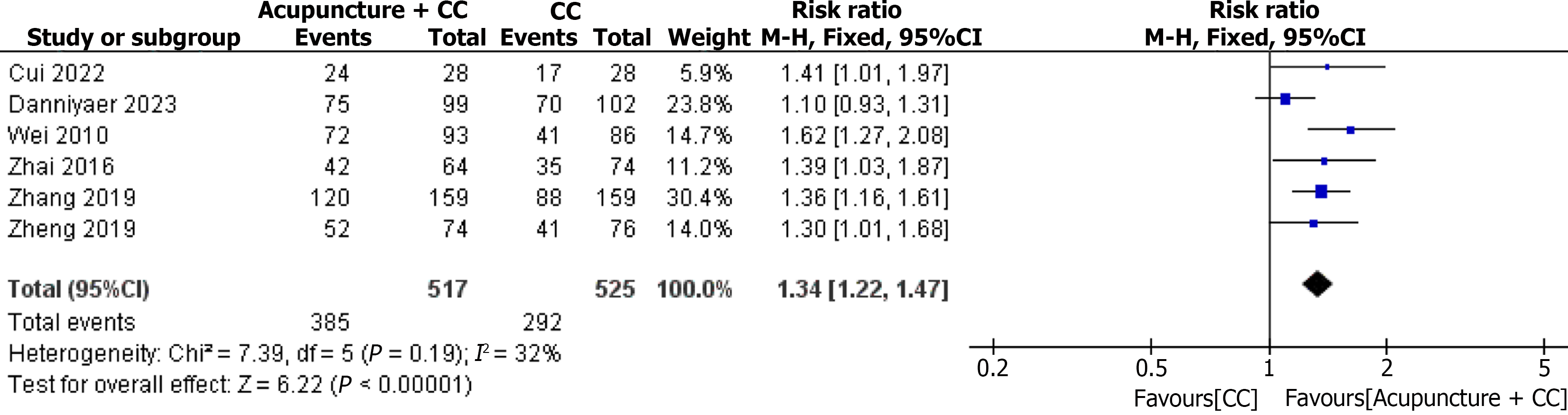
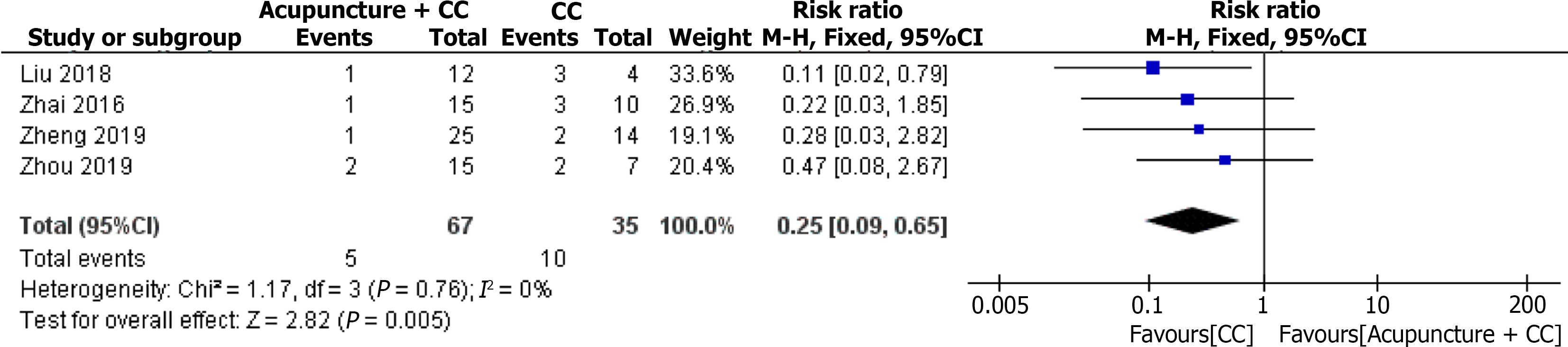
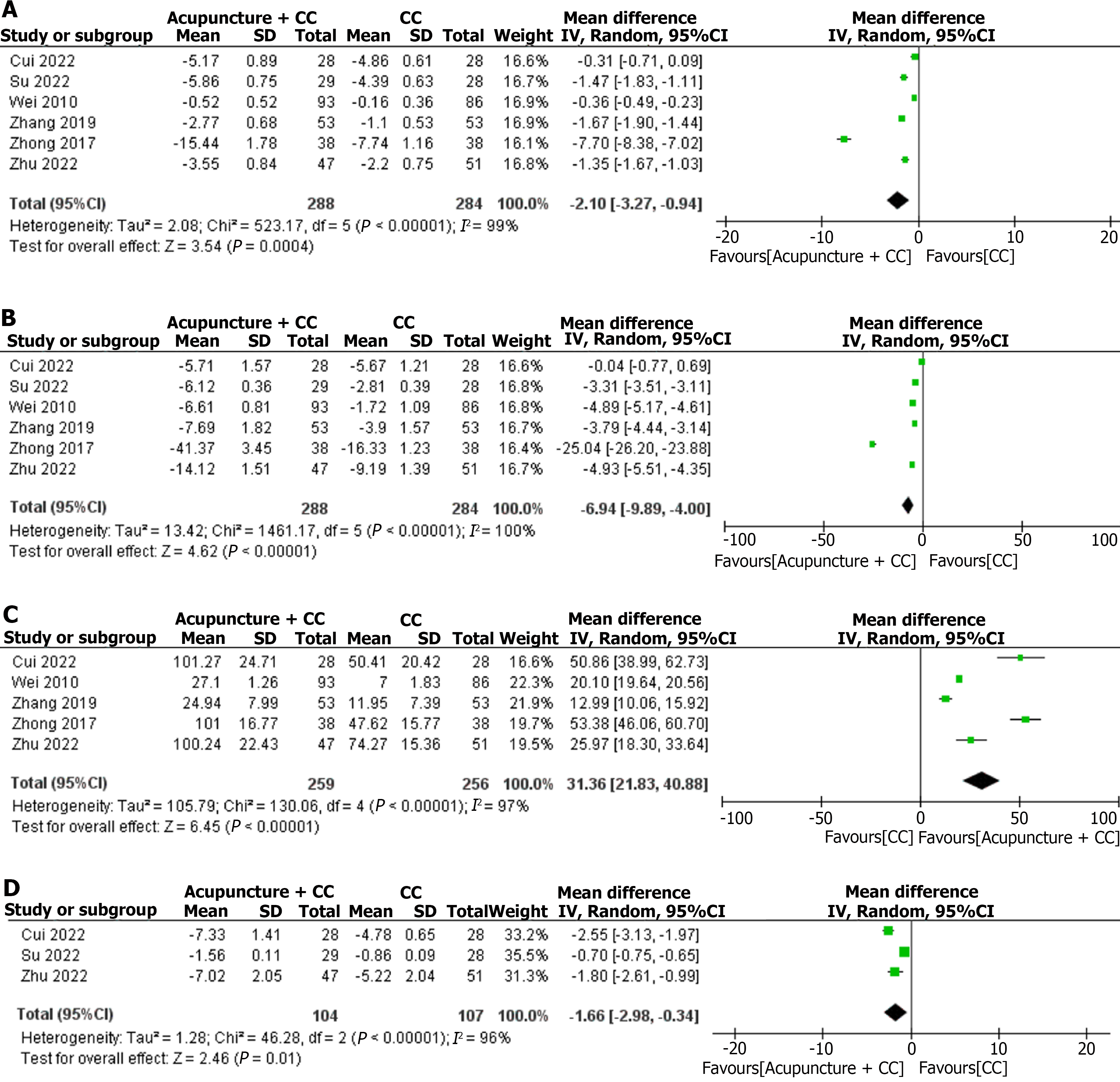
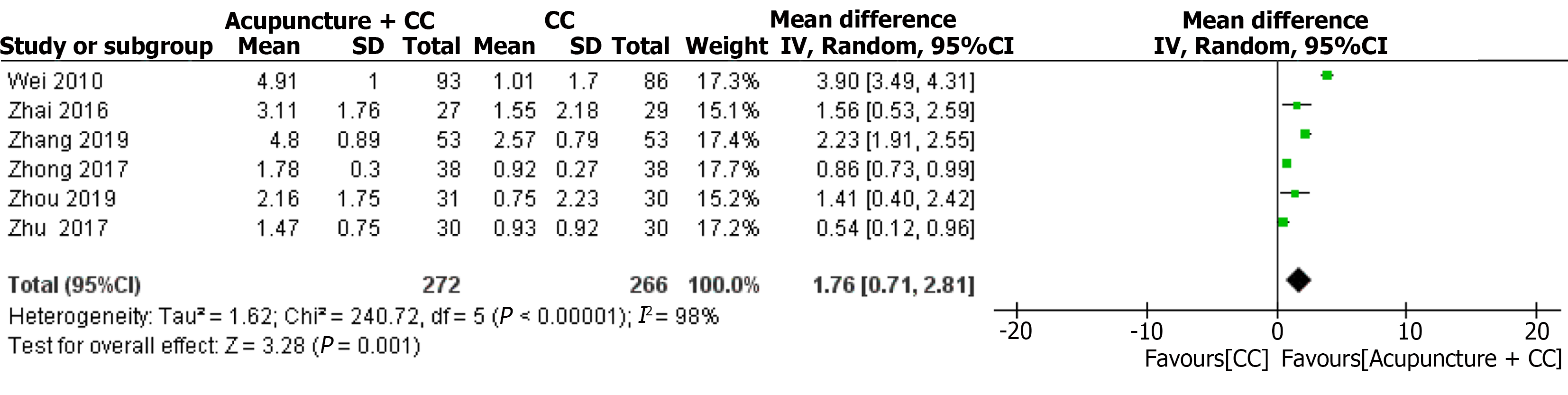
AT plus CC vs CC: (1) Pregnancy rate. Ten trials involving 790 ODI patients compared the pregnancy rate between AT plus CC and CC. The fixed-effect model indicated that the pregnancy rate of AT plus CC was significantly higher than CC (RR = 1.68, 95%CI:1.45-1.95, P < 0.00001), and heterogeneity in the pregnancy rate was low (I2 = 23%, P = 0.23) (Figure 4); (2) Ovulation rate. Six trials involving 1042 ODI patients compared the ovulation rate between AT plus CC and CC. The fixed-effect model indicated that the ovulation rate of AT plus CC was significantly higher than CC (RR = 1.34, 95%CI: 1.22-1.47, P < 0.00001), and heterogeneity in the ovulation rate was low (I2 = 32%, P = 0.19) (Figure 5); (3) Miscarriage rate. Four trials involving 102 ODI patients compared the miscarriage rate between AT plus CC and CC. The fixed-effect model indicated that the miscarriage rate of AT plus CC was superior to CC (RR = 0.25, 95%CI: 0.09-0.65, P = 0.005), and heterogeneity in the miscarriage rate was low (I2 = 0%, P = 0.76) (Figure 6); (4) FSH. Six trials involving 572 ODI patients compared the serum FSH level between AT plus CC and CC. The random-effect model indicated that the serum FSH level of AT plus CC was significantly lower than CC (MD = -2.10, 95%CI: -3.27 to -0.94, P = 0.0004), and heterogeneity in the serum FSH level was significant (I2 = 99%, P < 0.00001) (Figure 7A); (5) LH. Six trials involving 572 ODI patients compared the serum LH level between AT plus CC and CC. The random-effect model indicated that the serum LH level of AT plus CC was noticeably lower than CC (MD = -6.94, 95%CI: -9.89 to -4.00, P < 0.00001), and heterogeneity in the serum LH level was significant (I2 = 100%, P < 0.00001) (Figure 7B); (6) E2. Five trials involving 515 ODI patients compared the serum E2 level between AT plus CC and CC. The random-effect model indicated that the serum E2 level of AT plus CC was significantly higher than CC (MD = 31.36, 95%CI: 21.83-40.88, P < 0.00001), and heterogeneity in the serum E2 level was significant (I2 = 97%, P < 0.00001) (Figure 7C); (7) P. Three trials involving 211 ODI patients compared the serum P level between AT plus CC and CC. The random-effect model indicated that the serum P level of AT plus CC was significantly lower than CC (MD = -1.66, 95%CI: -2.98 to -0.34, P = 0.01), and heterogeneity in the serum P level was significant (I2 = 96%, P < 0.00001) (Figure 7D); and (8) Thickness of endometrium. Six trials involving 538 ODI patients compared the thickness of endometrium between AT plus CC and CC. The random-effect model indicated that the thickness of endometrium of AT plus CC was significantly higher than CC (MD = 1.76, 95%CI: 0.71-2.81, P = 0.001), and heterogeneity in the thickness of endometrium was significant (I2 = 98%, P < 0.00001) (Figure 8).
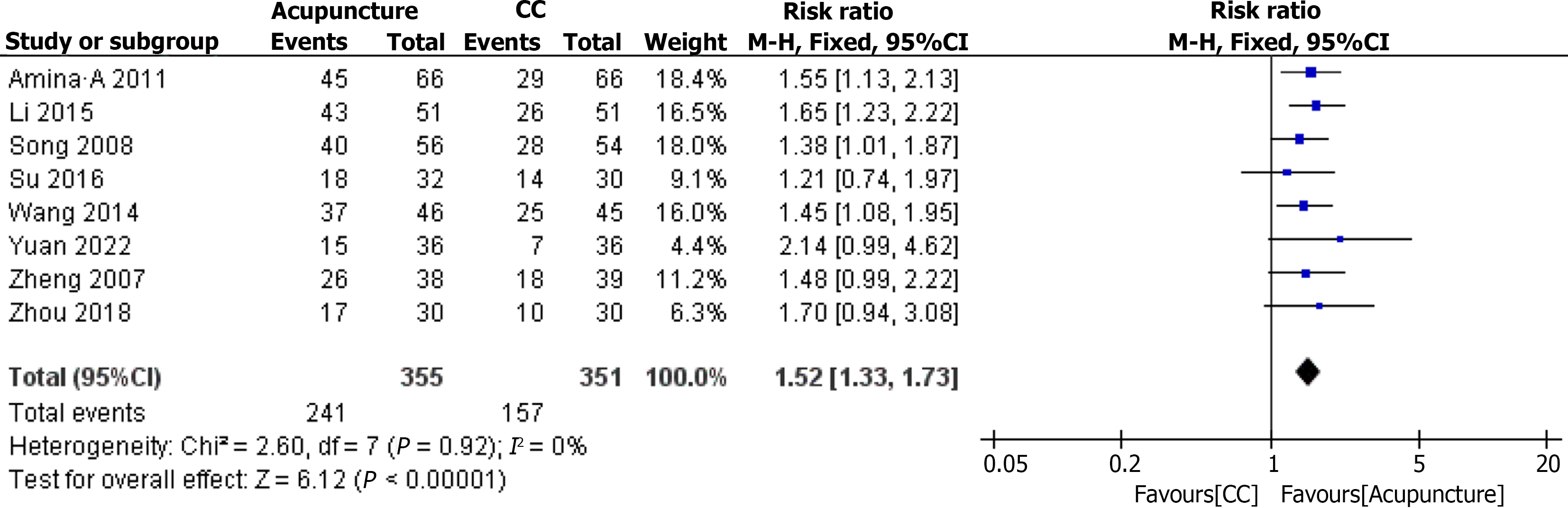
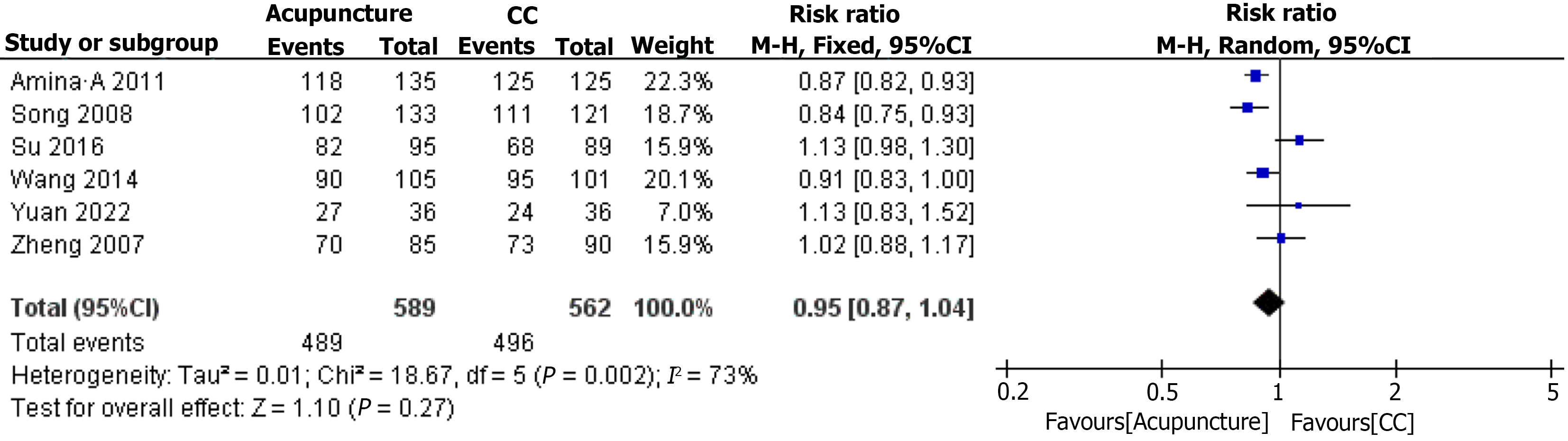
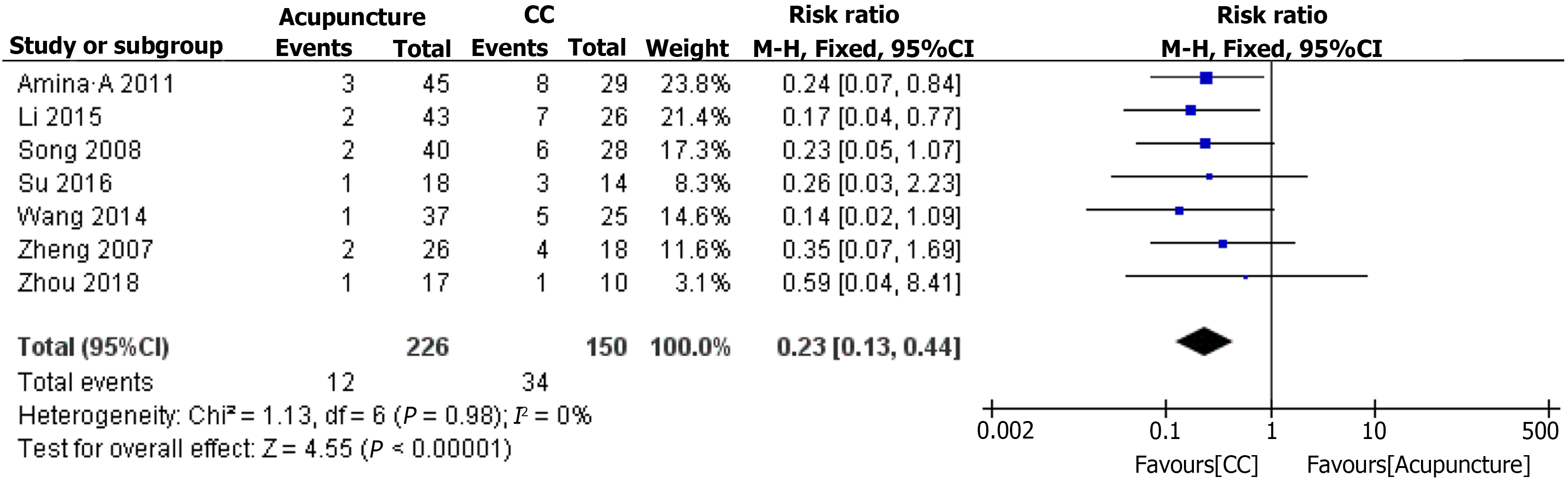
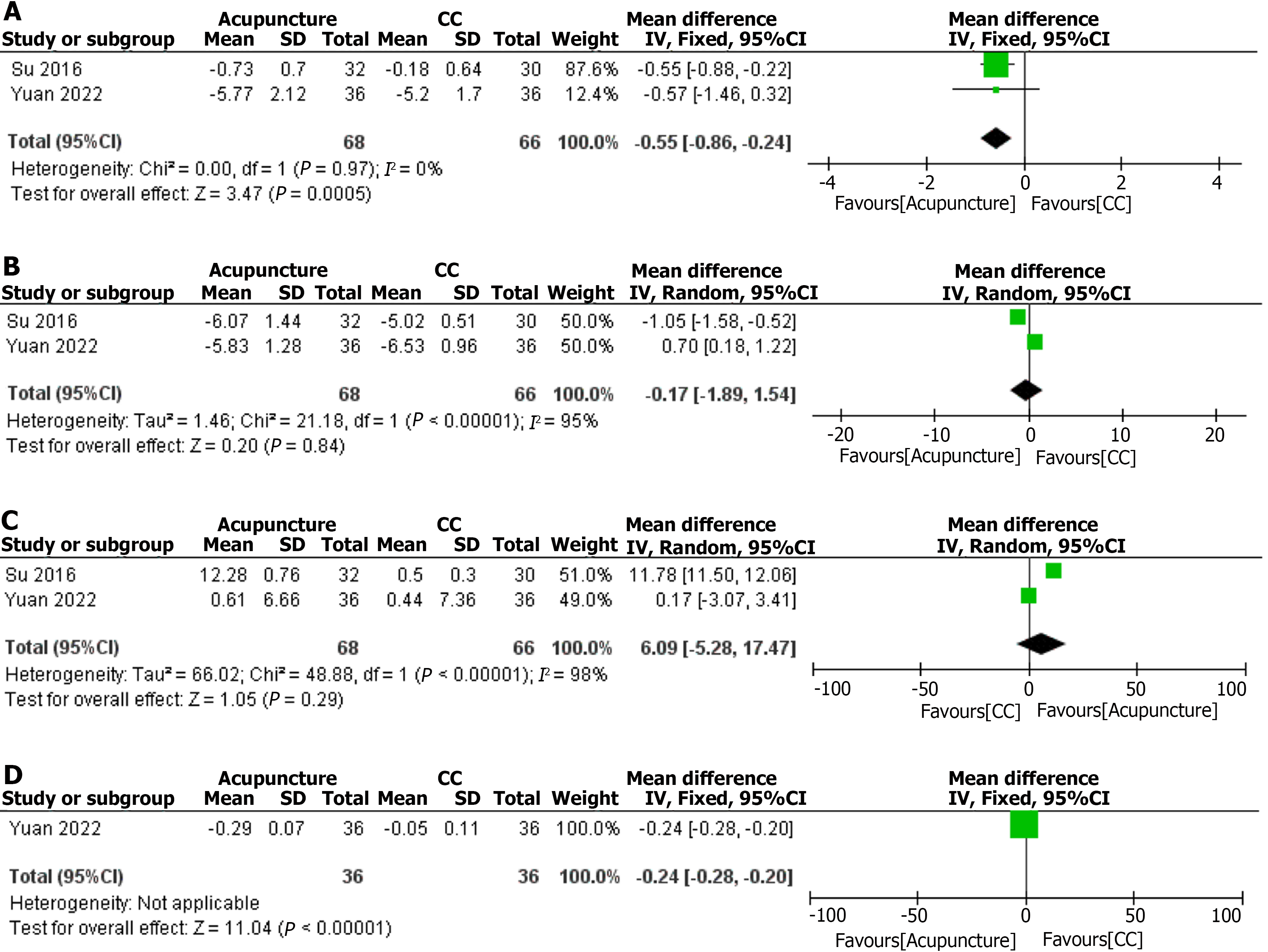
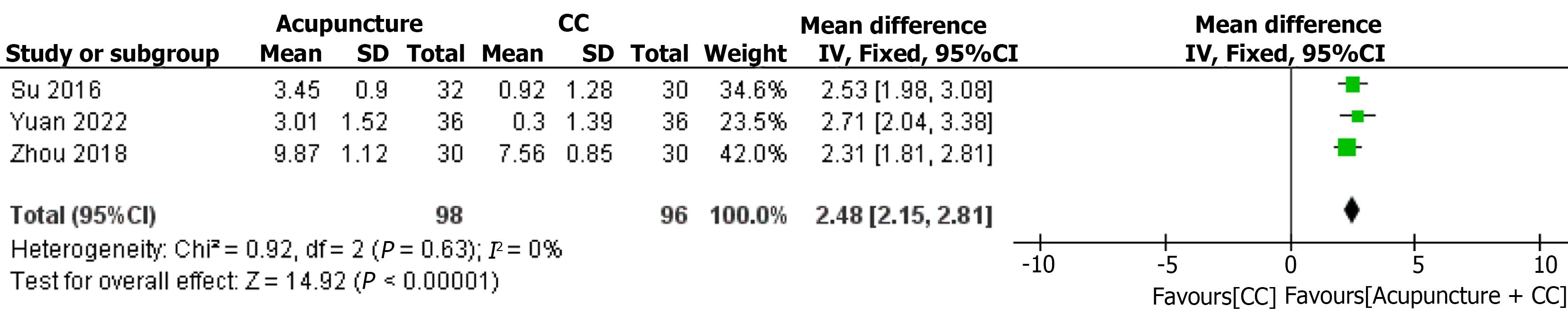
AT vs CC: (1) Pregnancy rate. Eight trials involving 706 ODI patients compared the pregnancy rate between AT and CC. The fixed-effect model indicated that the pregnancy rate of AT was significantly higher than CC (RR = 1.52, 95%CI: 1.33-1.73, P < 0.00001), and heterogeneity in the pregnancy rate was low (I2 = 0%, P = 0.92) (Figure 9); (2) Ovulation rate. Six trials involving 1151 ODI patients compared the ovulation rate between AT and CC. The random-effect model indicated that the ovulation rate of AT was not significantly different than CC (RR = 0.95, 95%CI: 0.87-1.04, P = 0.27), and heterogeneity in the ovulation rate was significant (I2 = 73%, P = 0.002) (Figure 10); (3) Miscarriage rate. Seven trials involving 376 ODI patients compared the miscarriage rate between AT and CC. The fixed-effect model indicated that the miscarriage rate of AT was superior to CC (RR = 0.23, 95%CI: 0.13-0.44, P < 0.00001), and heterogeneity in the miscarriage rate was low (I2 = 0%, P = 0.98) (Figure 11); (4) FSH. Two trials involving 134 ODI patients compared the serum FSH level between AT and CC. The fixed-effect model indicated that the serum FSH level of AT was significantly lower than CC (MD = -0.55, 95%CI: -0.86 to -0.24, P = 0.0005), and heterogeneity in the serum FSH level was low (I2 = 0%, P = 97) (Figure ); (5) LH. Two trials involving 134 ODI patients compared the serum LH level between AT and CC. The random-effect model indicated that the serum LH level of AT was not significantly different than CC (MD = -0.17, 95%CI: -1.891.54, P = 0.84), and heterogeneity in the serum LH level was significant (I2 = 95%, P < 0.00001) (Figure ); (6) E2. Two trials involving 134 ODI patients compared the serum E2 level between AT and CC. The random-effect model indicated that the serum E2 level of AT was not significantly different than CC (MD = 6.09, 95%CI: -5.28-17.47, P = 0.29), and heterogeneity in the serum E2 level was significant (I2 = 98%, P < 0.00001) (Figure ); (7) P. One study involving 72 ODI patients compared the serum P level between AT and CC. The fixed-effect model indicated that the serum P level of AT was significantly lower than CC (MD = -0.24, 95%CI: -0.28 to -0.20, P < 0.00001) (Figure ); and (8) Thickness of endometrium. Three trials involving 194 ODI patients compared the thickness of endometrium between AT and CC. The fixed-effect model indicated that the thickness of endometrium of AT was significantly higher than CC (MD = 2.48, 95%CI: 2.15, 2.81, P < 0.00001), and heterogeneity in the thickness of endometrium was low (I2 = 0%, P = 0.63) (Figure 13).
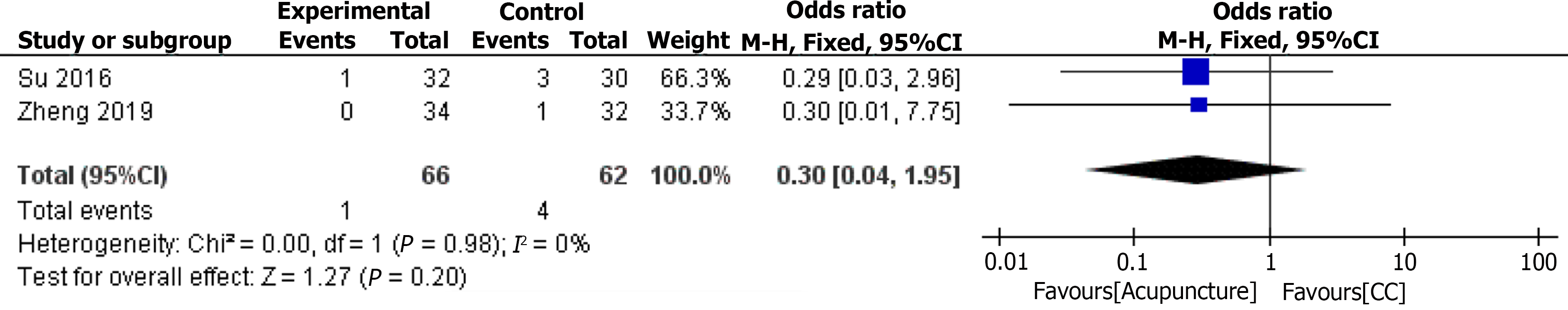
Six trials including 511 ODI patients reported adverse events[25-28,33,34]. Four trials did not describe the occurrence of adverse events. Two trials observed the occurrence of OHSS. There was no statistically significant difference in the incidence of OHSS between the two groups (Odds ratio = 0.30, 95%CI: 0.04 -1.95, P = 0.20) (Figure 14).
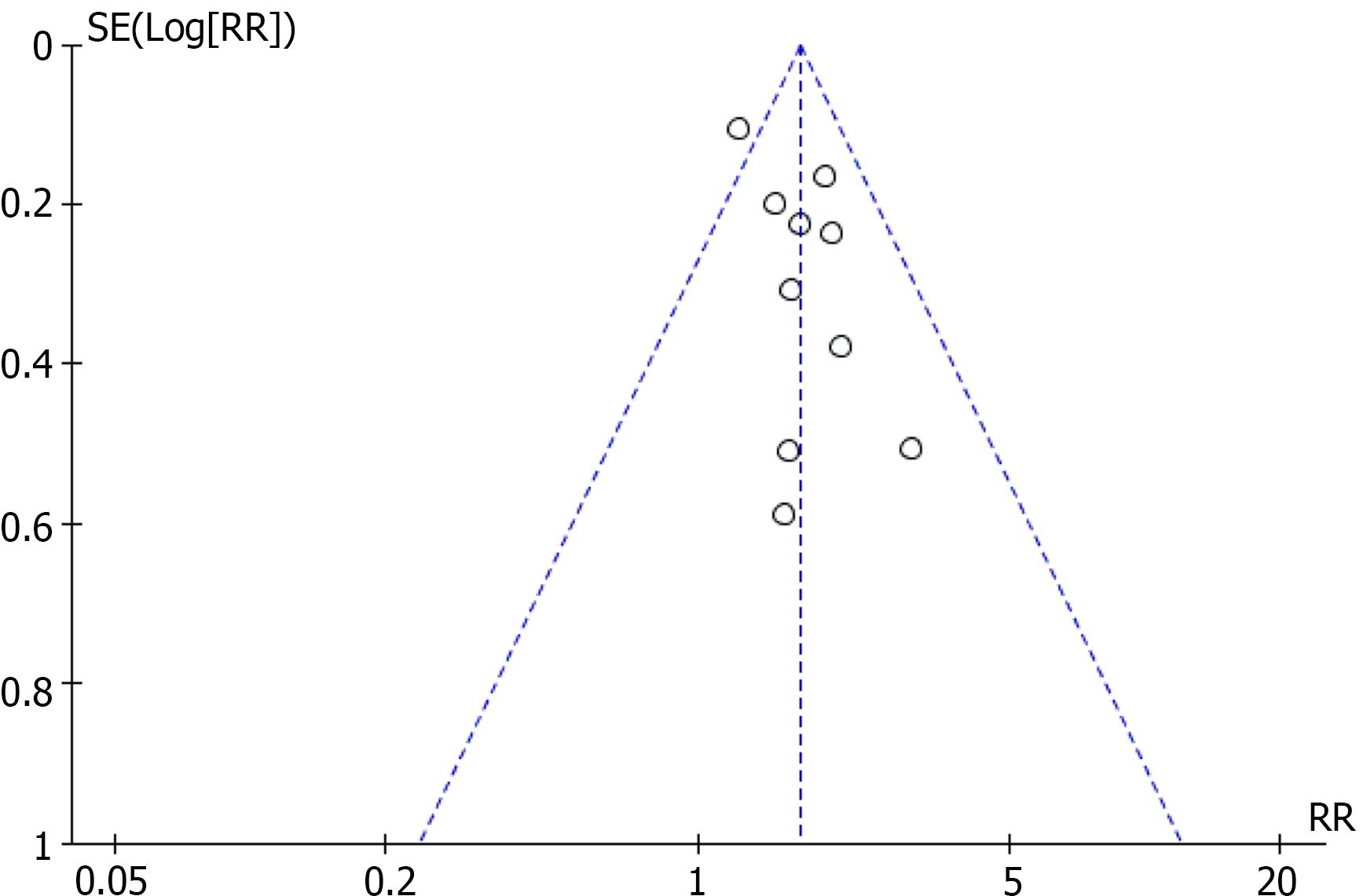
The publication bias of pregnancy rate outcome was evaluated by funnel plots of AT plus CC vs CC based on the analysis of 10 trials. Funnel plot asymmetry was observed, indicating no significant evidence of publication bias (Figure 15). Due to the limited inclusion of studies, other outcomes were not evaluated for publication bias.
Table 3 summarizes the detailed ratings and reasons for the downgrade. The overall certainty of the quality of evidence was categorized as very low to moderate.
| Outcomes | Certainty assessment | Effect sizes | Certainty | Importance | |||||
| Number of trials (patients) | Risk of bias1 | Inconsistency2 | Indirectness3 | Imprecision4 | Publication bias5 | RR or MD (95%CI) | |||
| AT plus CC vs CC | |||||||||
| Pregnancy | 10 (790) | Serious | No serious | No serious | No serious | Likelihood | RR 1.68 (1.45-1.95) | Moderate6 | Critical |
| Ovulation | 6 (1042) | Serious | No serious | No serious | No serious | Undetected | RR 1.34 (1.22-1.47) | Moderate6 | Critical |
| Miscarriage rate | 4 (102) | Serious | No serious | No serious | Serious | Undetected | RR 0.25 (0.09-0.65) | Low7 | Critical |
| FSH | 6 (572) | Serious | Serious | No serious | No serious | Undetected | MD -2.10 (-3.27 to -0.94) | Low7 | Important |
| LH | 6 (572) | Serious | Serious | No serious | No serious | Undetected | MD -6.94 (-9.89 to -4.00) | Low7 | Important |
| E2 | 5 (515) | Serious | Serious | No serious | No serious | Undetected | MD 31.36 (21.83-40.88) | Low7 | Important |
| P | 3 (211) | Serious | Serious | No serious | Serious | Undetected | MD -1.66 (-2.98 to -0.34) | Very low8 | Important |
| Thickness of endometrium | 6 (538) | Serious | Serious | No serious | No serious | Undetected | MD 1.76 (0.71-2.81) | Low7 | Important |
| AT vs CC | |||||||||
| Pregnancy | 8 (706) | Serious | No serious | No serious | No serious | Undetected | RR 1.52 (1.33-1.73) | Moderate | Important |
| Ovulation | 6 (1151) | Serious | Serious | No serious | No serious | Undetected | RR 0.95 (0.87-1.04) | Low7 | Important |
| Miscarriage rate | 7 (376) | Serious | No serious | No serious | Serious | Undetected | RR 0.23 (0.13-1.04) | Low7 | Important |
| FSH | 2 (134) | Serious | Serious | No serious | Serious | Undetected | MD -0.55 (-0.86 to -0.24) | Very low8 | Important |
| LH | 2 (134) | Serious | Serious | No serious | Serious | Undetected | MD 3.27 (1.55-4.99) | Very low8 | Important |
| E2 | 2 (134) | Serious | Serious | No serious | Serious | Undetected | MD 2.19 (1.10-3.28) | Very low8 | Important |
| P | 1 (72) | Serious | Undetected | No serious | Serious | Undetected | MD 3.02 (1.33-4.71) | Low7 | Important |
| Thickness of endometrium | 3 (194) | Serious | Serious | No serious | Serious | Undetected | MD 2.06 (1.23-2.89) | Very low8 | Important |
This review evaluated the possibilities and advantages of AT for ODI, including 20 studies with 1677 patients. The results of this review demonstrating the effect of AT in improving pregnancy outcomes in patients with ODI are consistent with the previous review[13]. Unlike the previous review[13], studies that used other Teding dianci bopu traditional Chinese medicine interventions in the intervention group were excluded from this review because the potential harms and benefits of these interventions are not known. Ten recently published studies were added to this review to provide important evidence updates. In addition, we further analyzed the improvement effect of AT on sex hormone levels and ovarian function. Compared to CC alone, AT as an adjunctive treatment can significantly increase the pregnancy rate and ovulation rate by approximately 68% and 34%, respectively, while also improving serum E2 levels and endometrial thickness. In addition, adjuvant AT also significantly reduced serum FSH, LH, and P levels and 25% miscarriage rate. In the comparison of AT with CC, AT could significantly improve endometrial thickness and pregnancy rate by 52%. It was more beneficial in reducing serum FSH and P levels and 23% miscarriage rate. There was no significant difference between AT and CC in reducing the incidence of adverse effects.
For a long time, AT has been widely used to treat infertility, and several potential mechanisms have been demonstrated to explain its effects. AT in the treatment of ODI can regulate the endocrine level of patients, significantly increase the level of β-endorphin, improve the blood supply of the ovarian artery, promote endometrial development, promote blastocyst implantation, and achieve the purpose of increasing the pregnancy rate and reducing the early abortion rate[37,38].
Chen et al[39] found that AT regulated ovarian granulosa cell autophagy by downregulating LncMEG3 expression and inhibiting the PI3K/AKT/mTOR pathway, thereby improving ovarian development and sex hormone levels and possibly treating ovulation dysfunction. Zhang et al[40] found that electroacupuncture regulated serum E2, FSH, and LH levels and improved ovarian function by activating the PI3K/AKT/mTOR signaling pathway.
Fu et al[41] found that AT reduced the increase in serum E2 levels and increased the decreased pituitary estrogen receptor expression in the superovulatory rat model, enhanced the function of the HPO axis, and prevented and reduced the occurrence of OHSS. Studies have shown that AT can promote follicle growth, rupture, and excretion and improve endometrial receptivity. AT treatment of ODI is closely related to its regulation of the reproductive axis and increase of the endometrial blood supply[42].
In addition, this review found that SP 6, RN 4, Zigong, ST 36, and RN 3 seemed to be the most commonly used acupoints for AT treatment of ODI. The most common treatment number was each day (65%), and the duration was 30 min (80%). It is suggested that in future studies, priority should be given to the above acupoints and the number and duration of treatment.
SP6 is the essential point of the spleen meridian of foot-taiyin, which is the intersection point with the kidney, liver and spleen three Yin meridians. It can invigorate the spleen and regulate blood, soothe the liver and nourish the kidney, and regulate and replenish the thoroughgoing conception vessel. Studies have confirmed that the SP6 and RN4 acupoints of AT ovariectomy rats can regulate the disorder of serum endocrine hormones and improve the dysfunction of the HPO axis[43].
RN4 is the intersection point between conception vessel and kidney, liver, spleen, three Yin meridians, and the thoroughgoing vessel, which can regulate qi and blood of all meridians, strengthen the yuan, strengthen the root, and replenish the lower jiao. The RN4 acupoint can regulate the pituitary and gonadal functions by affecting the secretion of gonadotropin-releasing hormone from the hypothalamus in female AT rats[44].
The Zigong point is a special extrameridian point, which is not only located near the uterus in the lower abdomen but also closely related to the uterus in its neuroanatomical structure. It is an important point for the treatment of gynecological and obstetrical diseases and has a significant clinical effect on infertility and other uterine diseases[45].
ST36 can warm up the innate and acquired vitality, and SP6 matches and can supplement the liver and kidney, promote blood circulation, and regulate menstruation. The results showed that AT in ST36 reduced the serum levels of interleukin-6 and tumor necrosis factor α in animals, which may be related to the ability of AT to inhibit inflammation and oxidative stress[46].
RN3 is the intersection point of conception vessel and kidney, liver and spleen three Yin meridians, which affects the uterus and sperm chamber, and can lead to human reproductive diseases. It has been shown that continuous electroacupuncture stimulation of RN4 and RN3 can reduce the expression of P450c17α in the theca cell layer and downregulate the levels of testosterone, androstenedione, and LH, thereby improving follicular development and ovulation[47].
Although from a clinical perspective, the results of this meta-analysis support the use of AT in patients with ODI, there were some limitations: (1) Few studies discussed how to estimate the sample size, and most studies involved small sample sizes leading to low accuracy; (2) The quality of most of the literatures was low, and no specific randomization method was defined; (3) Some studies did not adequately report allocation concealment. Failure to fully implement allocation concealment may overstate any treatment effect observed; (4) The search scope was not wide enough, the clinical trial platform was not searched, the grey literature was not collected, and the results of the included literature were all positive, which may affect the results of the meta-analysis; and (5) Lack of follow-up. For example, 18 studies reported the pregnancy rate but did not report the live birth rate and neonatal health status.
AT can improve the pregnancy outcomes and sex hormone levels for patients with ODI. However, further studies are needed to confirm these findings.
| 1. | Petykó Z, Lénád L, Sümegi B, Hajnal A, Csete B, Faludi B, Jandó G. Learning disturbances in offsprings of zidovudine (AZT) treated rats. Neurobiology (Bp). 1997;5:83-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 603] [Article Influence: 150.8] [Reference Citation Analysis (0)] |
| 2. | Vander Borght M, Wyns C. Fertility and infertility: Definition and epidemiology. Clin Biochem. 2018;62:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 516] [Cited by in RCA: 1135] [Article Influence: 162.1] [Reference Citation Analysis (0)] |
| 3. | Zhou Z, Zheng D, Wu H, Li R, Xu S, Kang Y, Cao Y, Chen X, Zhu Y, Xu S, Chen ZJ, Mol BW, Qiao J. Epidemiology of infertility in China: a population-based study. BJOG. 2018;125:432-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 252] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 4. | Zhang J, Tang L, Kong L, Wu T, Xu L, Pan X, Liu GJ. Ultrasound-guided transvaginal ovarian needle drilling for clomiphene-resistant polycystic ovarian syndrome in subfertile women. Cochrane Database Syst Rev. 2021;11:CD008583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ; International PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33:1602-1618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 619] [Cited by in RCA: 957] [Article Influence: 159.5] [Reference Citation Analysis (0)] |
| 6. | Althuis MD, Moghissi KS, Westhoff CL, Scoccia B, Lamb EJ, Lubin JH, Brinton LA. Uterine cancer after use of clomiphene citrate to induce ovulation. Am J Epidemiol. 2005;161:607-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 76] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Smith JF, Eisenberg ML, Millstein SG, Nachtigall RD, Shindel AW, Wing H, Cedars M, Pasch L, Katz PP; Infertility Outcomes Program Project Group. The use of complementary and alternative fertility treatment in couples seeking fertility care: data from a prospective cohort in the United States. Fertil Steril. 2010;93:2169-2174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 8. | Pastore LM, Williams CD, Jenkins J, Patrie JT. True and sham acupuncture produced similar frequency of ovulation and improved LH to FSH ratios in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011;96:3143-3150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Johansson J, Redman L, Veldhuis PP, Sazonova A, Labrie F, Holm G, Johannsson G, Stener-Victorin E. Acupuncture for ovulation induction in polycystic ovary syndrome: a randomized controlled trial. Am J Physiol Endocrinol Metab. 2013;304:E934-E943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 10. | Jedel E, Labrie F, Odén A, Holm G, Nilsson L, Janson PO, Lind AK, Ohlsson C, Stener-Victorin E. Impact of electro-acupuncture and physical exercise on hyperandrogenism and oligo/amenorrhea in women with polycystic ovary syndrome: a randomized controlled trial. Am J Physiol Endocrinol Metab. 2011;300:E37-E45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 11. | Xu JY, Fan YH, Geng JZ, Gao N, Yu FH, Xia T. Application progress of acupuncture in treatment of ovarian hypofunction. TMR Non-Drug Ther. 2021;4:16. [DOI] [Full Text] |
| 12. | Shi Y, Li L, Zhou J, Sun J, Chen L, Zhao J, Wu L, Cui Y, Wu L, Wu H. Efficacy of electroacupuncture in regulating the imbalance of AMH and FSH to improve follicle development and hyperandrogenism in PCOS rats. Biomed Pharmacother. 2019;113:108687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Gao R, Guo B, Bai J, Wu Y, Wu K. Acupuncture and clomiphene citrate for anovulatory infertility: a systematic review and meta-analysis. Acupunct Med. 2020;38:25-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, McKenzie JE. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4127] [Cited by in RCA: 4658] [Article Influence: 1164.5] [Reference Citation Analysis (0)] |
| 15. | Hua KQ, Feng YJ. Obstetrics and Gynecology. 3rd ed. Beijing: People’s Medical Publishing House, 2013: 257-268. |
| 16. | Zheng XY. Guiding Principles for Clinical Research on New Chinese Medicines. 3rd ed. Beijing: China Pharmaceutical Science and Technology Press, 2002: 293-295. |
| 17. | Su QD, Yang YP, Wu HQ. [Observation on the Curative Effect of Fire Needling Acupuncture in the Treatment of Kidney Qi Deficiency Type Ovulatory Disorder Infertility]. Shenzhen Zhongxiyi Jiehe Zazhi. 2022;32:25-28. |
| 18. | Zhu JY, Xiang HM. [Efficacy Observation of Shui Huo Ji Needling Combined with Western Medication for Anovulatory Infertility and Its Effects on Serum VEGF, CTGF, and HGF Levels]. Shanghai Zhenjiu Zazhi. 2022;41:1089-1094. |
| 19. |
Cui DW, Mi JP, Yu ZS.
[Effects of acupuncture New Baliao acupoints on ovulation and quantitative scoring of TCM evidence in patients with PCOS ovulation disorder infertility] |
| 20. | Li F. [Clinical observation on the treatment of ovulatory infertility with acupuncture]. Shenzhen Zhongxiyi Jiehe Zazhi. 2015;25:76-77. |
| 21. | Song FJ, Zheng SL, Ma DZ. [Cinical observation on acupuncture for treatment of infertility of ovulatory disturbance]. Zhonghguo Zhenjiu. 2008;1:21-23. |
| 22. | Zhang YH. [Effect of Tong Yuan Needling on Pregnancy Rate in Anovulatory Infertility Patients]. Shanghai Zhenjiu Zazhi. 2019;38:520-524. |
| 23. | Amina A, Yang JY. [Clinical observation on the treatment of 66 ovulatory infertile patients use acupuncture]. Zhongguo Shiyong Yiyao. 2011;6:124-125. |
| 24. | Zhong WH, Chen QP. [Curative Efficacy of Feizhen Acupuncture Combined with Ovulation Stimulants in Treatment of Anovulatory Infertility and its effects on Sex Hormone and Endometrium]. Hebei Yixue. 2017;23:1715-1718. |
| 25. | Yuan SX. [Clinical study of acupuncture combined with through moxibustion in the treatment of ovulation disorder infertility of spleen and kidney deficiency]. M.Sc. Henan Zhongyiyao Daxue. 2022;1-56. |
| 26. | Zheng SZ. [Effect of Tongyuan Acupuncture on Ovarian Induction Period with Clomiphene Citrate: A Randomized Clinical Trial]. M.Sc. Guangzhou Zhongyiyao Daxue. 2019;1-66. |
| 27. | Zhu JJ. [To four points around navel acupuncture curative effect observation of its effect on promoting ovulation]. M.Sc. Guangzhou Zhongyiyao Daxue. 2018;1-43. |
| 28. | Su BY. [The clinical research of abdominal acupuncture combined with moxibustion in treating ovulation obstructive infertility (insufficiency of kidney-YANG)]. M.Sc. Guangzhou Zhongyiyao Daxue. 2017;. |
| 29. | Liu YE. [To analyze the clinical effect of acupuncture and moxibustion in the treatment of ovulatory infertility and its influence on abortion rate]. Shiyong Fuke Neifenmi Zazhi. 2018;5:67-68. |
| 30. | Wang MH. [To observe the clinical effect of acupuncture and moxibustion in the treatment of ovulatory infertility]. Zhingguo Yiyao Zhinan. 2014;12: 119-120. |
| 31. | Danniyaer H. [Clinical study of warming acupuncture and moxibustion in the treatment of infertility with ovulation disorder of kidney Yang deficiency]. M.Sc. Xinjiang Yike Daxue. 2024;1-35. |
| 32. | Zhai WP. [Clinical study on the treatment of polycystic ovary syndrome ovulation disorder by supplementing qi and ovulation acupuncture combined with clomiphene]. M.Sc. Guangxi Zhongyiyao Daxue. 2017;1-64. |
| 33. | Wei LX, Zhou JP, Xu S, Shao XM, Liang RF. [Clinical observation on therapeutic effect of acupuncture at Guanyuan with the methods of Cuobing and Ticha on anovulation infertility]. Zhongguo Zhongyi Yaobao. 2010;25:1705-1707. |
| 34. | Zhou MQ. [Clinical observation on the treatment of infertility caused by polycystic ovary syndrome by acupuncture]. M.Sc. Chengdu Zhongyiyao Daxue. 2020;1-83. |
| 35. | Zheng SL, Song FJ, Ma DZ. [To evaluate the clinical efficacy of acupuncture and moxibustion in the treatment of ovulatory infertility]. Zhenjiu Linchuang Zazhi. 2007;1:9-10+14. |
| 36. | Zhou JH, Pang QH. [The clinical view of acupuncture and moxibustion of Zhuang medicine in the treatment of ovulatory infertility with kidney deficiency]. Zhongguo Ziran Liaofa. 2018;26:8-9. |
| 37. | Ciechanowska M, Lapot M, Mateusiak K, Przekop F. Neuroendocrine regulation of GnRH release and expression of GnRH and GnRH receptor genes in the hypothalamus-pituitary unit in different physiological states. Reprod Biol. 2010;10:85-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 38. | Zhong Y, Zeng F, Liu W, Ma J, Guan Y, Song Y. Acupuncture in improving endometrial receptivity: a systematic review and meta-analysis. BMC Complement Altern Med. 2019;19:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 39. | Chen X, Tang H, Liang Y, Wu P, Xie L, Ding Y, Yang P, Long B, Lin J. Acupuncture regulates the autophagy of ovarian granulosa cells in polycystic ovarian syndrome ovulation disorder by inhibiting the PI3K/AKT/mTOR pathway through LncMEG3. Biomed Pharmacother. 2021;144:112288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 40. | Zhang H, Qin F, Liu A, Sun Q, Wang Q, Xie S, Lu S, Zhang D, Lu Z. Electro-acupuncture attenuates the mice premature ovarian failure via mediating PI3K/AKT/mTOR pathway. Life Sci. 2019;217:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 41. | Fu H, Sun J, Tan Y, Zhou H, Xu W, Zhou J, Chen D, Zhang C, Zhu X, Zhang Y, Wu X, Xi Z. Effects of acupuncture on the levels of serum estradiol and pituitary estrogen receptor beta in a rat model of induced super ovulation. Life Sci. 2018;197:109-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 42. | Xi J, Cheng J, Jin CC, Liu JY, Shen ZR, Xia LJ, Li Q, Shen J, Xia YB, Xu B. Electroacupuncture Improves Pregnancy Outcomes in Rats with Thin Endometrium by Promoting the Expression of Pinopode-Related Molecules. Biomed Res Int. 2021;2021:6658321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 43. | Seo SY, Moon JY, Kang SY, Kwon OS, Kwon S, Bang SK, Kim SP, Choi KH, Ryu Y. An estradiol-independent BDNF-NPY cascade is involved in the antidepressant effect of mechanical acupuncture instruments in ovariectomized rats. Sci Rep. 2018;8:5849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 44. | Zhai ZJ, Liu JE, Lei LL, Wang SY. Effects of Transcutaneous Electrical Acupoint Stimulation on Ovarian Responses and Pregnancy Outcomes in Patients Undergoing IVF-ET: A Randomized Controlled Trial. Chin J Integr Med. 2022;28:434-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 45. | Wang SC, Jiang YM, Qiu LR, Su M. Efficacy of needling acupoints of Guanyuan (CV4), Sanyinjiao (SP6), Zusanli (ST36), Pishu (BL20), Shenshu (BL23), Zigong (EX-CA1) on expression of p38 mitogen-activated protein kinase in ovarian tissue in rats with premature ovarian failure induced by cyclophosphamide. J Tradit Chin Med. 2021;41:953-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 46. | Hu R, Huang Y, Song Y, Wu X, Song K, Huang G, Zhang M, Dong H. Effect of acupuncture on the opening time of implantation window and endometrial receptivity in controlled ovarian hyperstimulation rats during peri-implantation period. Front Endocrinol (Lausanne). 2023;14:1110266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 47. | Sun J, Jin C, Wu H, Zhao J, Cui Y, Liu H, Wu L, Shi Y, Zhu B. Effects of electro-acupuncture on ovarian P450arom, P450c17α and mRNA expression induced by letrozole in PCOS rats. PLoS One. 2013;8:e79382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |