Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5083
Revised: May 24, 2024
Accepted: June 11, 2024
Published online: August 6, 2024
Processing time: 82 Days and 20.4 Hours
In this randomized controlled trial (RCT) comparing current acupuncture with carbamazepine for trigeminal neuralgia, meta- and sequential analyses were utilized.
To guide clinical decision making regarding the treatment of trigeminal neuralgia with carbamazepine.
The RCT literature on needle comparison was searched in various Chinese biomedical databases including Chinese Biomedical Literature Database, Wan
This study analyzed 16 RCTs with a total of 1231 participants. The meta-analysis revealed a statistically significant difference in pain reduction between acupuncture and carbamazepine [standardized mean difference (SMD) = 1.47; 95% confidence interval (CI): 0.99-1.95], although the quality of evidence was deemed to be of extremely low quality. Cumulative meta-analysis based on the year of publication indicated that carbamazepine treatment first demonstrated a statistically significant difference in pain reduction in 2014 and remained relatively stable over time [SMD = 1.84; 95%CI: 0.22-3.47]. Additionally, the number of adverse events associated with acupuncture was significantly lower compared to carbamazepine.
Acupuncture for trigeminal neuralgia is better than analgesia and safer than carbamazepine; however, firm conclusions still require a high-quality, multicenter, large-sample RCT to confirm these findings.
Core Tip: Randomized controlled trial studies have confirmed that both acupuncture and carbamazepine have significant therapeutic effects on primary trigeminal neuralgia. Our meta-analysis results showed that acupuncture treatment for trigeminal neuralgia is superior to analgesics and safer than carbamazepine.
- Citation: Wei L, Han H, Meng J, Li X, Yao QP. Meta-analysis and sequential analysis of acupuncture compared to carbamazepine in the treatment of trigeminal neuralgia. World J Clin Cases 2024; 12(22): 5083-5093
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5083.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5083
Pain, recognized as the fifth vital sign of the human body, serves as a crucial indicator of potential harm or existing damage. Trigeminal neuralgia, a prominent type of pain, typically affects individuals aged 50-60 years, with a higher incidence in women than in men[1,2]. Research indicates that approximately 27 out of 100000 individuals suffer from trigeminal neuralgia[3], with an annual incidence rate of approximately 12.6 per 100000[4,5]. Furthermore, trigeminal nerve pain is often described as unbearable, significantly impacting both the physical and mental wellbeing of patients. However, treating this condition poses considerable challenges due to the unclear specific cause[6].
Carbamazepine is commonly used in modern medicine as the primary medication to treat trigeminal neuralgia[7]. While it can significantly reduce pain associated with the trigeminal nerve and extend the time between attacks[8], it does have various side effects such as vertigo, diplopia, nausea, and ataxia[9]. Furthermore, there is a high recurrence rate and a risk of developing drug resistance. Acupuncture and moxibustion, valued in Chinese medicine, provide simple, convenient, effective, and cost-efficient alternatives. Our research team has conducted multiple randomized controlled trials (RCTs) on acupuncture for pain-related conditions, which have offered initial evidence supporting the efficacy and safety of acupuncture in pain management. Several studies[10-17] currently indicate that acupuncture therapy is both effective and safe for treating trigeminal neuralgia, leading to increased acceptance of this treatment among healthcare professionals.
Early publication of systematic evaluations and meta-analyses can lead to a more subjective selection of indicators. While meta-analyses often include acupuncture and other treatments, previous studies have not compared individual acupuncture therapy with carbamazepine for efficacy and safety. This lack of comparison, along with the absence of sample size estimation and sequential analysis, may introduce bias and lead to false positive results. To address these issues, our study was registered to prevent publication bias. We employed cumulative meta-analysis to combine our results and estimated the necessary sample size. Furthermore, we utilized the GRADE tool to evaluate the current quality of evidence, offering valuable insights for clinical application and serving as a reference for future clinical studies.
This system evaluation/meta-analysis was conducted in the Open Science framework register and strictly followed the PRISMA checklist.
Research design: RCT for acupuncture treatment of trigeminal neuralgia, limited to the following languages for publication: Chinese and English.
Research population: Patients with clear diagnosis of trigeminal neuralgia, specific diagnostic criteria, no restrictions on sex, age, etc.
Intervention measures: The experimental group received simple acupuncture therapy; Control group: conventional Western medicine (Cama) Xiping treatment.
Outcome indicators: Main outcome measure: degree of change in pain intensity (using visual analog scale) as a measurement indicator; secondary outcome measure: incidence of adverse events.
Literature retrieval methods: The search terms used in this study covered a range of Chinese and English terms related to acupuncture, including warm needle, electric needle, scalp needle, ear needle, fire needle, abdominal needle, floating needle, percutaneous electrical stimulation, wrist and ankle needle, moxibustion, and trigeminal neuralgia. The search was conducted in various databases such as China Biology Medicine disc, China National Knowledge Infrastructure, Wanfang Data, VIP Database, Cochrane Library, Excerpt Medica Database, PubMed, Web of Science, and clinical trial registration platforms (WHO ICTRP, ChiCTR, Clinical Trials). The search also included major acupuncture journals and conference papers, with the search date up to 1 April 2020. The retrieval strategies focused on disease type (trigeminal neuralgia), treatment methods (acupuncture, warm needle, electric needle, etc), and trial type (RCT).
We excluded repeated RCT studies, non-RCT research, and literature not found.
Literature searches, screening, and data extraction were independently conducted by two individuals. Duplicate literature was initially excluded using NoteExpress. Subsequently, a preliminary screening was carried out, with two researchers independently reviewing the titles, key points, key words, and abstracts of the literature to exclude experiments that clearly did not meet the inclusion criteria. The full text of studies that potentially met the inclusion criteria was then downloaded and thoroughly read to ensure accuracy, finalizing the selection of literature that fully met the inclusion criteria. In cases of disagreement, an arbitrator was consulted to assist in making judgments, and any missing information was communicated to the author for supplementation. Data collection for this study was performed using Excel 2016, focusing on basic research information, research characteristics, intervention measures, research methods, risk of bias, and outcome measures.
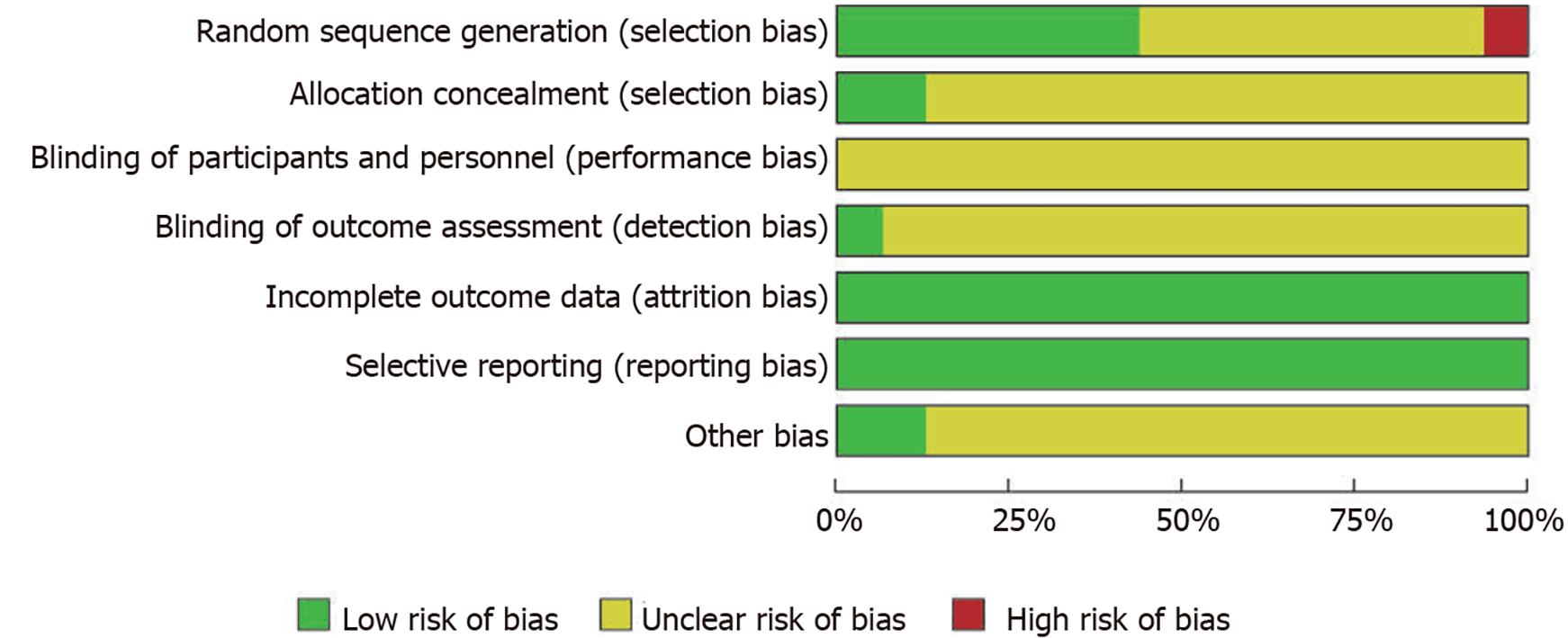
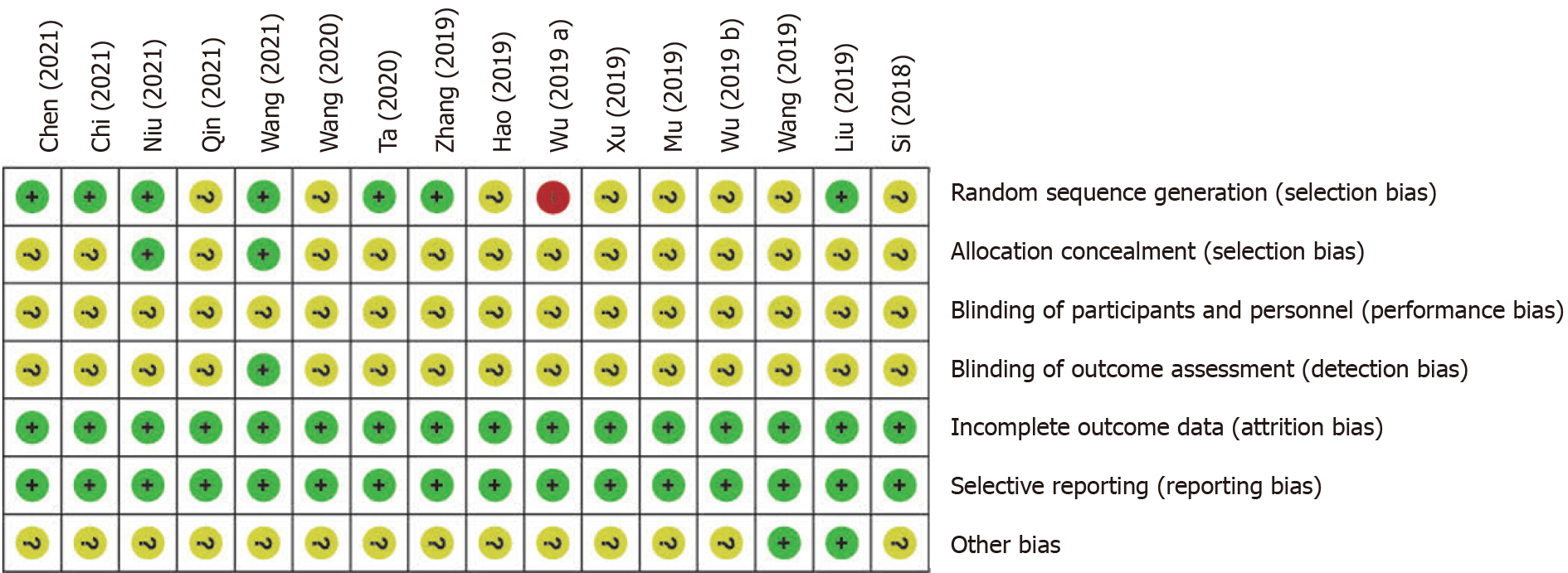
The bias risk assessment tool outlined in the Cochrane manual[18] was employed to methodologically evaluate the literature entries. This tool consists of seven items: (1) Objective (randomization correctness, allocation concealment, and referencing); (2) Participant blinding; (3) Evaluator blinding; (4) Completeness of result data; (5) Selective reporting; and (6) Other biases. Each item is categorized into three levels: Low risk, high risk, and uncertain. Subsequently, a risk map was generated utilizing RevMan 5.3 software.
Both traditional and cumulative meta-analyses were performed using STATA software (StataCorp, College Station, TX, United States). When analyzing binary variables, the effect scale chosen was relative risk with a 95% confidence interval (CI). For continuous variables, the standardized mean difference (SMD) and 95%CI were utilized. If the P value exceeds 0.05 and I2 is below 50%, it indicates low heterogeneity among studies, leading to the application of a fixed effects model. Conversely, if the P value is below 0.05 and I2 is 50% or higher, suggesting high heterogeneity, a random effects model is employed. In instances of significant heterogeneity, a descriptive analysis was be carried out.
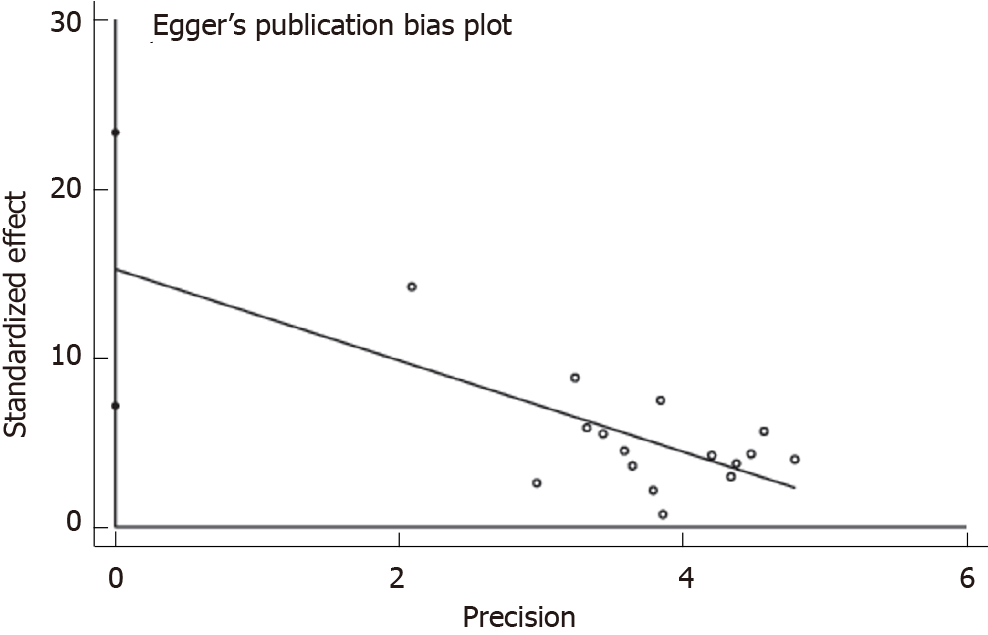
We analyzed potential publication bias using an Egger test. When P > 0.05, it indicates a lower risk of publication bias. If heterogeneity is high, a sensitivity analysis was used for analysis.
Traditional and cumulative meta-analyses do not address the issue of sample size estimation. Trial sequential analysis (TSA) integrates the group sequential analysis design principle to address random errors in meta-analysis and determine the required sample size to reduce the risk of inflated type I errors from multiple statistical tests. The researchers in this study employed the TSA 0.9.5.10 Beta software from the Copenhagen Clinical Trial Center to conduct a sequential analysis on the degree of pain reduction.
To address the research question, a mixed-methods approach combining quantitative and qualitative data collection methods will be utilized. The study aims to provide a comprehensive understanding of the topic by analyzing both numerical data and in-depth interviews with participants. This approach will allow for a more nuanced exploration of the research problem and provide a well-rounded perspective on the issue at hand.
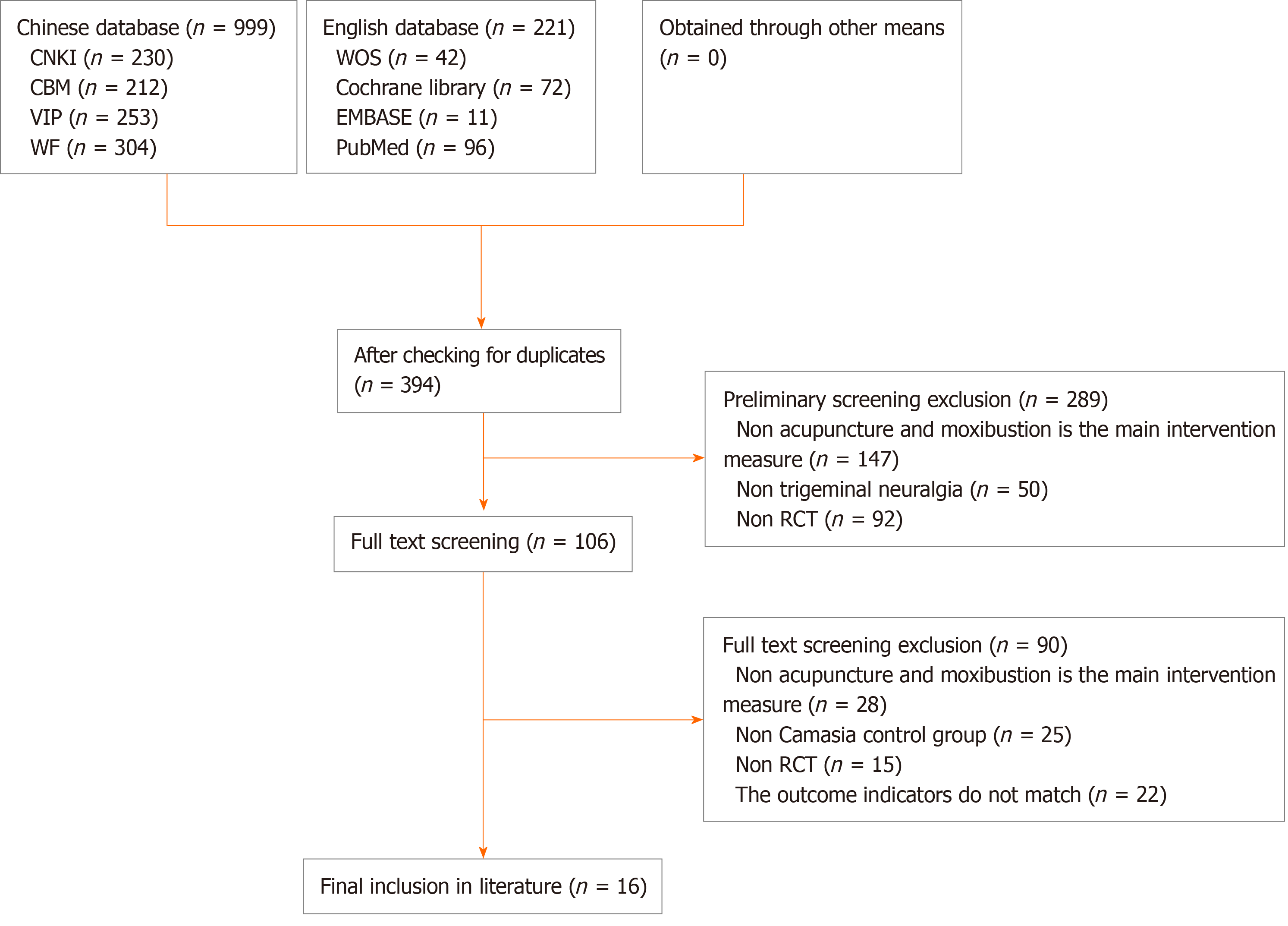
A total of 999 documents in Chinese and 221 in English were identified initially. After removing duplicates, 394 unique documents remained. During primary screening, 147 articles unrelated to acupuncture interventions, 50 not related to trigeminal neuralgia, and 92 non-RCT articles were excluded, resulting in 106 articles for further evaluation. Subsequent full-text screening led to the exclusion of 15 non-RCT articles, 28 articles with non-acupuncture treatment groups, 25 articles with non-carbamazepine control groups, and 22 articles with outcome measures that did not meet inclusion criteria. Ultimately, 16 RCT studies on acupuncture for trigeminal neuralgia were included[19-34]. The detailed process of literature screening is depicted in Figure 1.
The analysis of 16 articles, conducted in China between 2010 and 2019, focused on acupuncture and electroacupuncture therapy, as well as carbamazepine as interventions in the treatment group[19-34]. A total of 1231 participants were included in the treatment groups across the studies. The baseline comparability of the study subjects was deemed satisfactory, with the main outcome indicators being visual analog scale scores and adverse event occurrences. Most studies concluded that acupuncture and carbamazepine were effective in pain management, although one earlier study indicated no significant difference between carbamazepine and acupuncture in terms of analgesia[33-37].
As shown in Table 1[38-53], the basic characteristics of acupuncture and moxibustion are different, the stay time is mainly 30 min, and the treatment time is ≥ 4 wk.
| Ref. | Sample | Literature type | Random ratio | Intervention measures | Main outcome measures | Needle retention time | Treatment frequency | Course of treatment | Main conclusion | |
| Chen and He[38] (2021) | 90 | RCT | 1:1 | Treatment group | Control group | VAS | 30 min | Once a day | 4 wk | + |
| Chi et al[39] (2021) | 88 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS/adverse event | 20 min | Once a day | 1 mo | + |
| Niu[40] (2021) | 63 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS/adverse event | 30 min | Once a day | 30 d | + |
| Qin[41] (2021) | 62 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 20 min | Once a day | 1 mo | + |
| Wang and Zeng[42] (2021) | 100 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 30 min | Once a day | 30 d | + |
| Wang[43] (2020) | 60 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 20 min | Once a day | 3 mo | + |
| Ta[44] (2020) | 82 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 30 min | Once a day | 30 wk | + |
| Zhang et al[45] (2019) | 62 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 30 min | Once a day | 90 d | + |
| Hao et al[46] (2019) | 80 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS/adverse event | - | Once a day | - | + |
| Wu et al[47] (2019) | 100 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS/adverse event | 40 min | Once a day | 4 wk | + |
| Xu and Wang[48] (2019) | 84 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS/adverse event | 20 min | Once a day | 4 wk | + |
| Mu[49] (2019) | 80 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 20 min | Once a day | 30 d | + |
| Wu and Sun[50] (2019) | 60 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 30 min | Once a day | 4 wk | + |
| Liu and Liu[51] (2019) | 40 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 30 min | Once a day | 30 d | + |
| Wang[52] (2019) | 60 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 30 min | Once a day | 30 d | - |
| Si[53] (2018) | 120 | RCT | 1:1 | Acupuncture | Carbamazepine | VAS | 30 min | Once a day | 30 d | + |
All 16 studies were RCTs, with seven RCTs[19,21,22,28,29,32,34] providing detailed descriptions of the random sequence generation. One study[23] assigned participants randomly based on the order of visits, whereas the remaining studies did not provide detailed information on random sequence generation. Only two studies[39,40] used allocation concealment, and only one study[50] mentioned blinding of the evaluators. Overall, the data integrity of all studies was good, with no reported abnormalities in selective reporting. Only two studies[43] had a low risk of other biases. The methodological quality of the included studies was deemed to be of moderate quality, as shown in Figures 2 and 3.
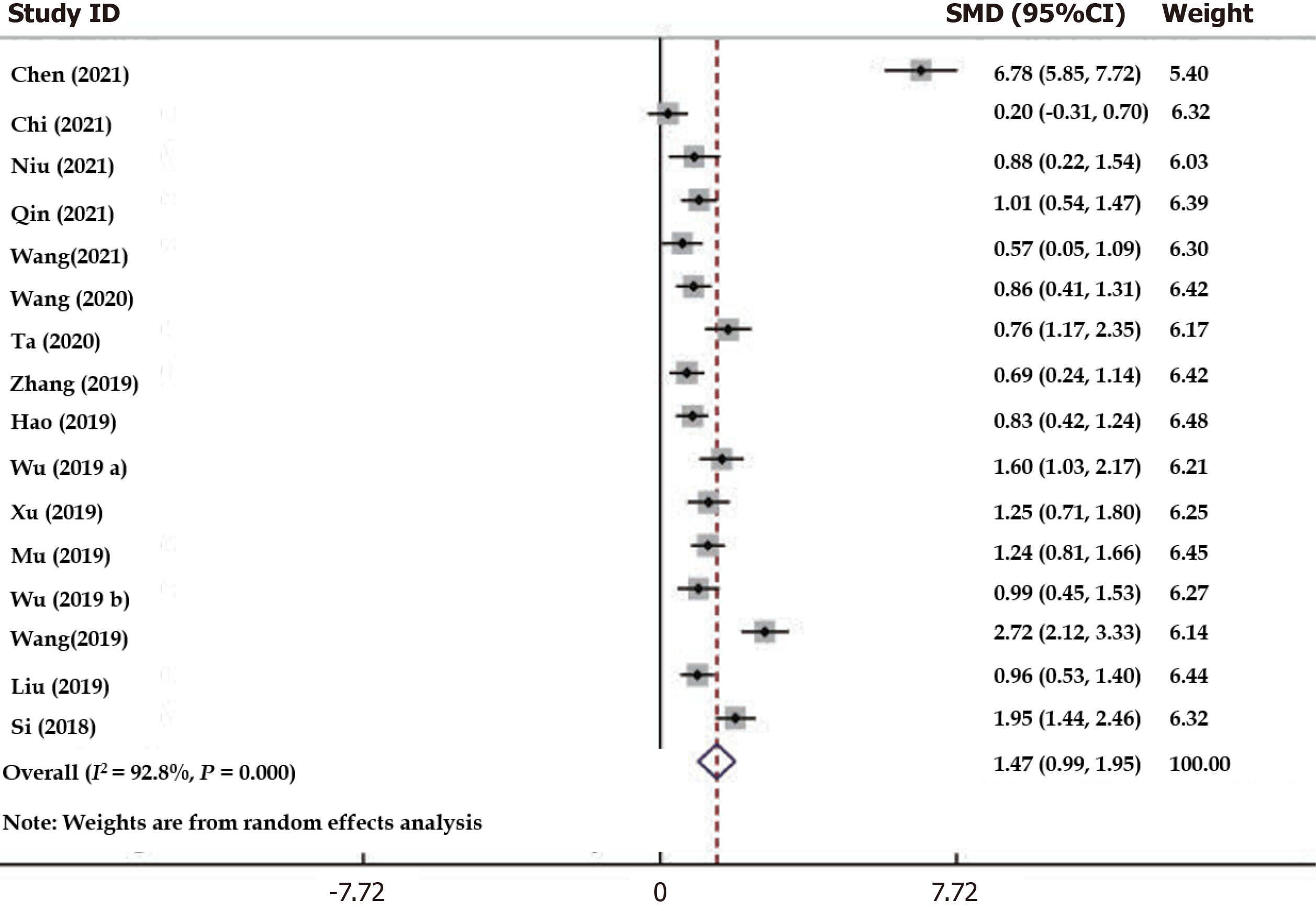
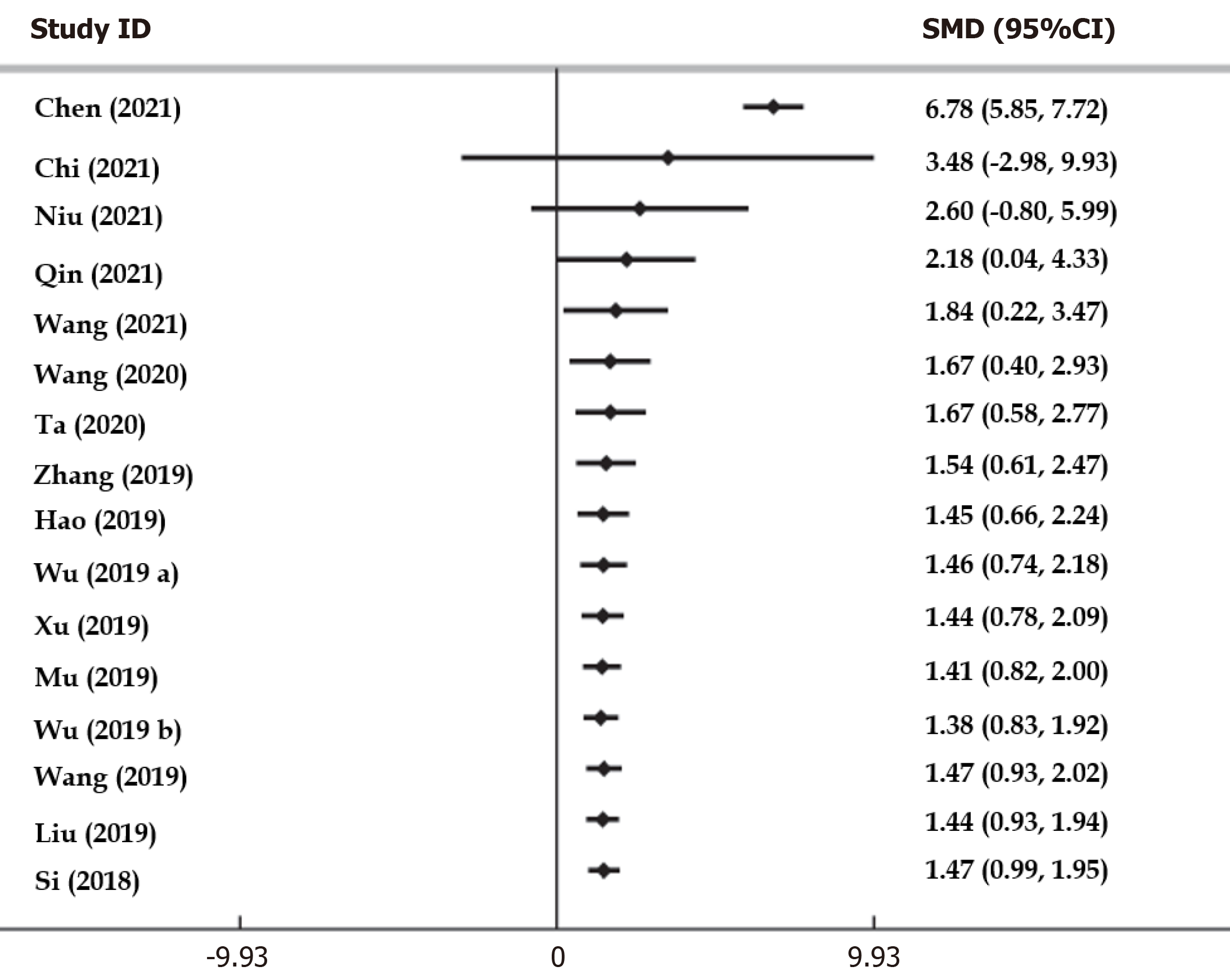
Traditional meta-analysis: The results were assessed for heterogeneity using conventional paired meta-analysis (χ2 = 208.84, P = 0.0001, I2 = 92.8% > 50%), which revealed high heterogeneity. Therefore, a random effect model was applied (Figure 4). Additionally, with a test value of Z = 5.99, P < 0.05, it was found that acupuncture provided better analgesia compared to carbamazepine, showing a statistically significant difference [SMD = 1.47; 95%CI: 0.99-1.95].
Analysis of publication bias: Publication bias analysis using Egger test, P = 0.001 < 0.05, suggesting a possible publication bias (Figure 5).
Sensitivity analysis: Through sensitivity analysis, it was discovered that, even after excluding one article[44] which stood out from the rest, there was still notable heterogeneity present. This suggests that the potential heterogeneity in our analysis stemmed from the overall study design rather than being attributed to a single trial.
Cumulative meta-analysis by year of publication: A cumulative meta-analysis based on publication years compared the effects of acupuncture and carbamazepine treatment. Initially, in 2014, the SMD was found to be 1.84 with a 95%CI of 0.22-3.47. Subsequent longitudinal comparisons revealed a trend of stabilization in the SMD value post-2014, with a narrowing 95%CI indicating increased accuracy over time. The final SMD value settled at 1.47 with a 95%CI of 9.99-1.95, suggesting that pain reduction in the acupuncture group surpassed that of the carbamazepine group, showing a tendency toward stability over time (Figure 6).
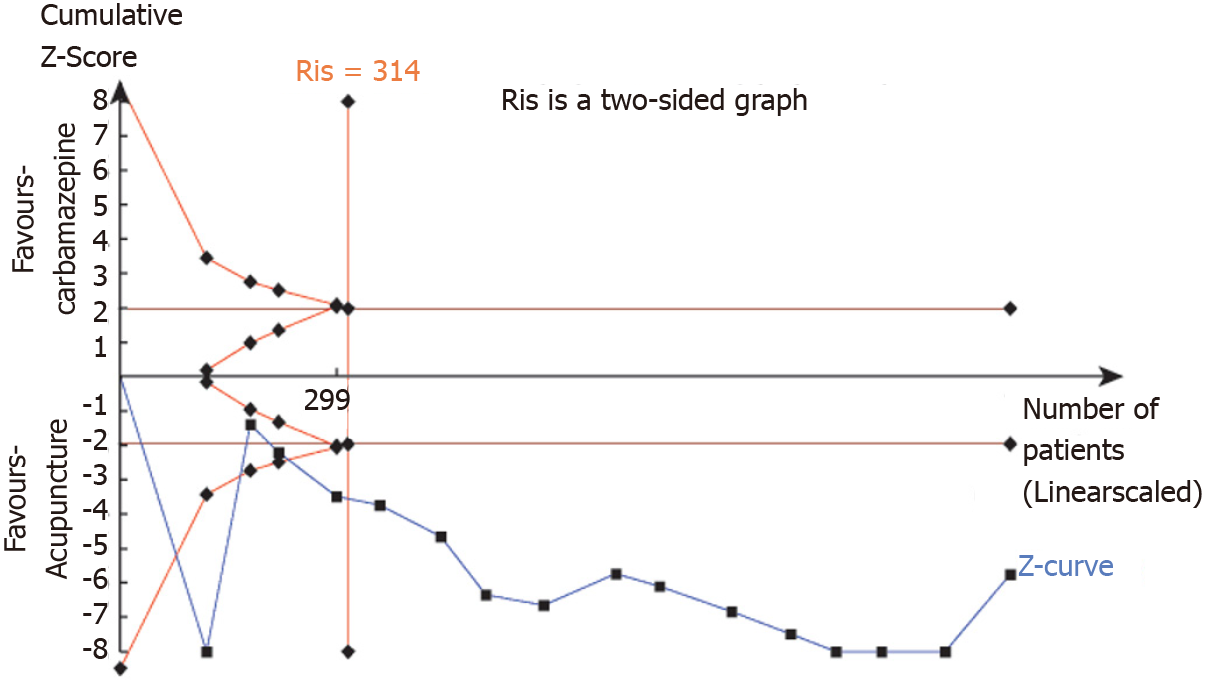
Sequential analysis of the TSA test: TSA was conducted using TSA 0.9.5.10 Beta software. The meta-analysis requires an expected sample size of 314. The estimation of RIS was determined using the two-sided test method with a probability of class I error α set at 0.05 and a statistical test power value of 0.8. The TSA analysis results indicate that the cumulative Z value (blue curve) has surpassed the traditional bound and the boundary curve set by TSA, suggesting that the sample information volume from the current included studies has met and exceeded the RIS value (Figure 7). Therefore, based on the data, it can be concluded that acupuncture is more effective than carbamazepine in reducing trigeminal nerve pain.
GRADE evidence analysis: Using the GRADE evaluation tool to rate the above outcome measures, we found that the quality of evidence for the reduction in pain compared with carbamazepine for trigeminal neuralgia was extremely low (Table 2).
Acupuncture comparison: Safety analysis of carbamazepine in the treatment of trigeminal neuralgia involved a total of five RCTs of 415 subjects[20,21,46-47] and provided information on adverse events related to acupuncture and carbamazepine (Table 3). The needle thorn group involved the number of adverse events was much lower than that caused by carbamazepine, but no serious adverse events occurred. At the same time, acupuncture easily leads to pigmentation, dizziness, drowsiness; carbamazepine easily causes dizziness, exfoliative dermatitis, digestive system issues, and other adverse reactions.
| Ref. | Treatment group as A | Control group as B | Sample size as A/B | Adverse event |
| Si[53] | Acupuncture | Carbamazepine | 44/44 | A: 1 case |
| B: 6 cases | ||||
| Wu and Sun[50] | Acupuncture | Carbamazepine | 32/31 | A: 1 case of pigmentation |
| B: 5 cases of dizziness and 1 case of exfoliative dermatitis | ||||
| Hao et al[46] | Acupuncture | Carbamazepine | 40/40 | A: 2 cases of pigmentation |
| B: 6 cases of dizziness and 1 case of exfoliative dermatitis | ||||
| Zhang et al[45] | Acupuncture | Carbamazepine | 50/50 | A: 1 case of dizziness caused by acupuncture |
| B: Mild digestive system adverse reactions, 4 cases with mild liver dysfunction, and 2 cases with rash | ||||
| Wang[52] | Acupuncture | Carbamazepine | 42/42 | A: 3 cases of drowsiness |
| B: 3 cases of dizziness, 5 cases of drowsiness, and 3 cases of vomiting |
In recent years, there have been reports of adverse events of acupuncture and moxibustion at different levels in China, from which experience has been learned; acupuncture treatment has been carried out in strict accordance with acupuncture operation specifications; and avoiding the influence of human factors on the reputation of acupuncture and moxibustion, which is of positive significance for the promotion and development of acupuncture and moxibustion. The causes of adverse events caused by acupuncture are mostly concentrated in improper operation, ignoring acupuncture contraindications, and so on. The most common adverse events are a series of acupuncture consequences that affect treatment, including pain, hematoma, infection, dizziness, pneumothorax, and organ rupture caused by acupuncture.
This study found through meta-analysis that the incidence of adverse events in the acupuncture group was much lower than that caused by carbamazepine, but no serious adverse events occurred. Therefore, it is believed that simple acupuncture therapy has certain therapeutic advantages and is safer than Western medicine (carbamazepine) in the treatment of trigeminal neuralgia in terms of pain relief. The methodological quality of the included literature was found to be moderate, with the GRADE evaluation tool indicating extremely low quality[48]. While acupuncture shows better effectiveness and safety for trigeminal neuralgia, the current evidence quality is not high, leading to highly uncertain results.
Limitations of this study: (1) Only published articles in Chinese and English were considered, excluding databases in other languages; (2) the treatment group used carbamazepine as compared to the control group, with variations in dose, dosage form, and timing; and (3) the reviewed literature had a small sample size, resulting in low-quality evidence and uncertainty in the conclusion.
This study compares acupuncture to carbamazepine to treat trigeminal neuralgia, suggesting that acupuncture may be more effective in pain relief. However, the analysis reveals that most of the literature has a moderate risk of bias and potential publication bias, resulting in very low-quality evidence. While previous studies have shown significant differences and stability in treating trigeminal neuralgia with carbamazepine before 2014, the conclusion is subject to change and requires further validation through high-quality, multicenter, large-sample RCTs.
This study offers several suggestions for future research in the field. Firstly, it notes that, while 16 RCTs demonstrated the effectiveness of acupuncture and carbamazepine in treating trigeminal neuralgia, most of these studies had small sample sizes and were conducted at single centers, lacking high-quality RCT support. Secondly, the study highlights that none of the RCTs mentioned clinical study registration, only indicating that they had undergone ethical review[49]. Therefore, it recommends that clinical trials should be registered and reported to minimize publication bias in RCTs. Thirdly, the study suggests using high-quality clinical trials tools such as the Cochrane risk assessment tool, CONSORT, and STRICTA to ensure the quality of RCTs and guide clinical practice[50,51]. Lastly, the study calls for the establishment of more standardized clinical studies on acupuncture techniques, acupoint selection, treatment duration, and clear guidelines for drug use. It is important to note that there are no conflicts of interest involved in this study.
Acupuncture for trigeminal neuralgia is better than analgesia and safer than carbamazepine. However, firm conclusions still require a high-quality, multicenter, large-sample RCT to confirm these findings.
| 1. | Bendtsen L, Zakrzewska JM, Abbott J, Braschinsky M, Di Stefano G, Donnet A, Eide PK, Leal PRL, Maarbjerg S, May A, Nurmikko T, Obermann M, Jensen TS, Cruccu G. European Academy of Neurology guideline on trigeminal neuralgia. Eur J Neurol. 2019;26:831-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 191] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 2. | Maarbjerg S, Di Stefano G, Bendtsen L, Cruccu G. Trigeminal neuralgia - diagnosis and treatment. Cephalalgia. 2017;37:648-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 312] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 3. | Hu H, Chen L, Ma R, Gao H, Fang J. Acupuncture for primary trigeminal neuralgia: A systematic review and PRISMA-compliant meta-analysis. Complement Ther Clin Pract. 2019;34:254-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Tölle T, Dukes E, Sadosky A. Patient burden of trigeminal neuralgia: results from a cross-sectional survey of health state impairment and treatment patterns in six European countries. Pain Pract. 2006;6:153-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 123] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Al-Quliti KW. Update on neuropathic pain treatment for trigeminal neuralgia. The pharmacological and surgical options. Neurosciences (Riyadh). 2015;20:107-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 6. | Koopman JS, Dieleman JP, Huygen FJ, de Mos M, Martin CG, Sturkenboom MC. Incidence of facial pain in the general population. Pain. 2009;147:122-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 305] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 7. | Maarbjerg S, Gozalov A, Olesen J, Bendtsen L. Trigeminal neuralgia--a prospective systematic study of clinical characteristics in 158 patients. Headache. 2014;54:1574-1582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 198] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 8. | Asplund P, Blomstedt P, Bergenheim AT. Percutaneous Balloon Compression vs Percutaneous Retrogasserian Glycerol Rhizotomy for the Primary Treatment of Trigeminal Neuralgia. Neurosurgery. 2016;78:421-8; discussion 428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Araya EI, Claudino RF, Piovesan EJ, Chichorro JG. Trigeminal Neuralgia: Basic and Clinical Aspects. Curr Neuropharmacol. 2020;18:109-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 89] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 10. | Chen B, Choi H, Hirsch LJ, Katz A, Legge A, Buchsbaum R, Detyniecki K. Psychiatric and behavioral side effects of antiepileptic drugs in adults with epilepsy. Epilepsy Behav. 2017;76:24-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 260] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 11. | Huang Z, Huo J, Zhao J. Efficacy on primary trigeminal neuralgia treated with triple puncture technique and electroacupuncture at trigger points. Zhongguo Zhenjiu. 2017;37:31-34. |
| 12. | Fu Y, Zhang HF, Li F, Xiong J, Zhang B, Li L, Chen RX. Comparative research of moxibustion and infrared method in testing heat-sensitive state at Xiaguan (ST 7) in primary trigeminal neuralgia. Zhongguo Zhenjiu. 2013;33:411-414. |
| 13. | Fu Y, Zhang HF, Li F, Xiong J, Zhang B, Li L, Chen RX. Observation on the distribution of heat-sensitized acupoints in patients with primary trigeminal neuralgia. Zhongguo Zhenjiu. 2013;33:325-327. |
| 14. | He L, Zhou WY, Zhang XM. Trigeminal neuralgia of hyperactive of liver yang type treated with acupuncture at Xiaguan (ST 7) at different depth: a randomized controlled trial. Zhongguo Zhenjiu. 2012;32:107-110. |
| 15. | Zhu X. Electro-acupuncture combined with the trigger point needle-embedding for treatment of primary trigeminal neuralgia in 31 cases. J Tradit Chin Med. 2008;28:13-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Ichida MC, Zemuner M, Hosomi J, Pai HJ, Teixeira MJ, de Siqueira JTT, de Siqueira SRDT. Acupuncture treatment for idiopathic trigeminal neuralgia: A longitudinal case-control double blinded study. Chin J Integr Med. 2017;23:829-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Gao J, Zhao C, Jiang W, Zheng B, He Y. Effect of Acupuncture on Cognitive Function and Quality of Life in Patients With Idiopathic Trigeminal Neuralgia. J Nerv Ment Dis. 2019;207:171-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Lee IS, Cheon S, Park JY. Central and Peripheral Mechanism of Acupuncture Analgesia on Visceral Pain: A Systematic Review. Evid Based Complement Alternat Med. 2019;2019:1304152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 19. | Acar HV. Acupuncture and related techniques during perioperative period: A literature review. Complement Ther Med. 2016;29:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 20. | Qiao L, Guo M, Qian J, Xu B, Gu C, Yang Y. Research Advances on Acupuncture Analgesia. Am J Chin Med. 2020;48:245-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Chen T, Zhang WW, Chu YX, Wang YQ. Acupuncture for Pain Management: Molecular Mechanisms of Action. Am J Chin Med. 2020;48:793-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 22. | Tonin FS, Rotta I, Mendes AM, Pontarolo R. Network meta-analysis: a technique to gather evidence from direct and indirect comparisons. Pharm Pract (Granada). 2017;15:943. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 171] [Cited by in RCA: 256] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 23. | Dai YK, Wu YB, Li RL, Chen WJ, Tang CZ, Lu LM, Hu L. Efficacy and safety of non-pharmacological interventions for irritable bowel syndrome in adults. World J Gastroenterol. 2020;26:6488-6509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Yin Z, Geng G, Xu G, Zhao L, Liang F. Acupuncture methods for allergic rhinitis: a systematic review and bayesian meta-analysis of randomized controlled trials. Chin Med. 2020;15:109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Debray TP, Schuit E, Efthimiou O, Reitsma JB, Ioannidis JP, Salanti G, Moons KG; GetReal Workpackage. An overview of methods for network meta-analysis using individual participant data: when do benefits arise? Stat Methods Med Res. 2018;27:1351-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 26. | Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catalá-López F, Gøtzsche PC, Dickersin K, Boutron I, Altman DG, Moher D. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4165] [Cited by in RCA: 5279] [Article Influence: 527.9] [Reference Citation Analysis (1)] |
| 27. | MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, Moher D; STRICTA Revision Group. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. 2010;7:e1000261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 695] [Cited by in RCA: 626] [Article Influence: 41.7] [Reference Citation Analysis (0)] |
| 28. | Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, Fainsinger R, Aass N, Kaasa S; European Palliative Care Research Collaborative (EPCRC). Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41:1073-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1913] [Cited by in RCA: 1733] [Article Influence: 123.8] [Reference Citation Analysis (0)] |
| 29. | Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6581] [Cited by in RCA: 15191] [Article Influence: 2531.8] [Reference Citation Analysis (0)] |
| 30. | Mu J, Furlan AD, Lam WY, Hsu MY, Ning Z, Lao L. Acupuncture for chronic nonspecific low back pain. Cochrane Database Syst Rev. 2020;12:CD013814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 31. | Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med. 2013;159:130-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 611] [Cited by in RCA: 777] [Article Influence: 64.8] [Reference Citation Analysis (0)] |
| 32. | Sutton A, Ades AE, Cooper N, Abrams K. Use of indirect and mixed treatment comparisons for technology assessment. Pharmacoeconomics. 2008;26:753-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 276] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 33. | Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 584] [Cited by in RCA: 1106] [Article Influence: 110.6] [Reference Citation Analysis (0)] |
| 34. | Baek E, Ferron JM. Bayesian Analysis for Multiple-baseline Studies Where the Variance Differs across Cases in OpenBUGS. Dev Neurorehabil. 2021;24:130-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1540] [Cited by in RCA: 2092] [Article Influence: 139.5] [Reference Citation Analysis (0)] |
| 36. | Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, Kessels AG, Guyatt GH; GRADE Working Group. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 903] [Cited by in RCA: 1238] [Article Influence: 112.5] [Reference Citation Analysis (0)] |
| 37. | Mehta S, Bastero-Caballero RF, Sun Y, Zhu R, Murphy DK, Hardas B, Koch G. Performance of intraclass correlation coefficient (ICC) as a reliability index under various distributions in scale reliability studies. Stat Med. 2018;37:2734-2752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 38. | Chen H, He K. Clinical Observation on Acupuncture and Moxibustion in Treatment of Primary Trigeminal Neuralgia. Shiyong Zhongyiyao Zazhi. 2021;37: 468-469. |
| 39. | Chi Y, Barth J, Wang M, Robinson N, Li ZH, Liu JP. Eye acupuncture for pain conditions: a scoping review of clinical studies. BMC Complement Med Ther. 2021;21:101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 40. | Niu Q. Experience in acupuncture treatment of primary trigeminal neuralgia. Zhongwai Nvxing Jiankang Yanjiu. 2021;5:115-116. |
| 41. | Qin LM. Clinical observation of 66 cases of primary trigeminal neuralgia treated with acupuncture. Zhongyi Linchuang Zazhi. 2021;13:78-79. [DOI] [Full Text] |
| 42. | Wang Y, Zeng Q. Effects of acupuncture combined with carbamazepine on quality of life in patients with primary trigeminal neuralgia. Dangdai Yixue Luncong. 2021;19:173-174. |
| 43. | Wang GR. Clinical effect of acupuncture on primary trigeminal neuralgia. Shijie Zuixin Yixue Xinxi Wenzhai. 2020;39:2. [DOI] [Full Text] |
| 44. | Ta YQ. Clinical Observation of Acupuncture Combined with Carbamazepine in the Treatment of Primary Trigeminal Neuralgia. Changchun, China: Changchun University of Chinese Medicine. 2020. [DOI] [Full Text] |
| 45. | Zhang YP, Wang Y, Xia WG, Song AQ. Triple Puncture for Primary Trigeminal Neuralgia: A Randomized Clinical Trial. Curr Med Sci. 2019;39:638-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 46. | Hao WB, Li YF, Gong SY. Clinical observation on treatment of primary trigeminal neuralgia with carbamazepine combined with acupuncture. Shiyong Zhongyiyao Zazhi. 2019;35:209-210. [DOI] [Full Text] |
| 47. | Wu JL, Yang H, Mi Y, Song Y, Wang Y. Clinical Study on Treatment of Primary Trigeminal Neuralgia with Warming Acupuncture at Xiaguan Acupoint. Xinjiang Zhongyiyao. 2019;37:34-36. |
| 48. | Xu JW, Wang HY. Clinical effect of acupuncture and moxibustion on primary trigeminal neuralgia. Neimenggu Zhongyiyao. 2019;38:137-138. |
| 49. | Mu DN. Effect analysis of acupuncture on primary trigeminal neuralgia. Zhongguo Xiandai Yaowu Yingyong. 2019;13:118-120. |
| 50. | Wu HD, Sun Y. Clinical observation of treating primary trigeminal neuralgia with warm acupuncture and moxibustion in Xiaguan acupoint. Zhongguo Zhongyi Jizheng. 2019;28:1457-1459. [DOI] [Full Text] |
| 51. | Liu YM, Liu CX. Clinical effect of acupuncture on patients with primary trigeminal neuralgia. Yiliao Shebei. 2019;32: 63-64. [DOI] [Full Text] |
| 52. | Wang Y. Therapeutic effect of acupuncture on 30 cases of primary trigeminal neuralgia. Yunan Zhongyi Zhongyao Zazhi. 2019;40:94-54. [DOI] [Full Text] |
| 53. | Si SX. Efficacy of carbamazepine combined with high frequency electroacupuncture in the treatment of primary trigeminal neuralgia. Neimengbu Yixue Zazhi. 2018;50:731-733. |