Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5051
Revised: May 30, 2024
Accepted: June 20, 2024
Published online: August 6, 2024
Processing time: 91 Days and 19.2 Hours
This work explored the effects of cognitive behavior therapy (CBT)-based comprehensive nursing intervention (CNI) mode in arch expansion to treat patients with orthodontic osteodilated arch (OOA).
To explore the application effect of CBT-based CNI model in orthodontic expan
Using convenient sampling method, 81 patients with OOA were selected and rolled into a control group (Ctrl group, 40 cases) and an observation group (Obs group, 41 cases). During the treatment, patients in the Ctrl group received routine nursing intervention mode, and the those in the Obs group received CBT mode on the basis of this. Before and after intervention, the incidence of oral mucositis, the mastery rate of correct arch expansion method, self-rating anxiety scale score, soft scale index, and plaque index were compared for patients in different groups. In addition, satisfaction and complications were comparatively analyzed.
Incidence of oral mucositis in the Obs group was lower (14.6% vs 38.5%), and the mastery rate of correct arch expansion method was obviously higher (90.2% vs 55.0%) was obviously higher (all P < 0.05). Meanwhile, the soft scale index and plaque index in the Obs group were much lower (P < 0.05). The compliance (90.24%) and satisfaction (95.12%) in the Obs group were greatly higher (P < 0.05).
The CBT-based CNI mode greatly improved the mastery rate of correct arch expansion method during arch expansion in treating patients with OOA and enhanced the therapeutic effect of arch expansion and the oral health of patients, improving the patient compliance.
Core Tip: This article investigated the effectiveness of a comprehensive nursing intervention model based on cognitive behavior therapy (CBT) in the treatment of patients with orthodontic osteodilated arch, which significantly reduced the occurrence of oral mucosal inflammation, improved mastery of appropriate expansion techniques, and improved treatment outcomes compared with the traditional care model. Patient compliance and satisfaction were high, highlighting the potential of CBT-based interventions in orthodontic care.
- Citation: Yang X, Wang ZX, Tian YX, Peng C, Yang HN, Wu Y. Effects of comprehensive nursing with cognitive behavioral therapy in orthodontic osteodilated arch treatment. World J Clin Cases 2024; 12(22): 5051-5058
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5051.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5051
Orthodontic arch expansion treatment is an important technique in the field of dental orthodontics[1], primarily used to address issues of dental crowding and misalignment. However, since this technique involves the remodeling of bone tissue, patients often experience significant pain and discomfort during the treatment process, along with considerable psychological stress[2,3]. These discomforts not only affect the patients' quality of life but may also lead to reduced treatment compliance, thereby impacting the overall effectiveness of the treatment[4]. Therefore, effectively alleviating pain and psychological stress during the treatment process has become a pressing clinical issue.
Cognitive behavioral therapy (CBT), a widely used psychological intervention technique, primarily works by changing patients' cognitive and behavioral patterns to alleviate psychological and physiological symptoms[5,6]. CBT has been proven to be significantly effective in relieving chronic pain, anxiety, and depression[7]. In recent years, researchers have begun exploring the introduction of CBT into orthodontic treatment, with the aim of improving patients' treatment experience and compliance through psychological intervention[8,9]. Compared with traditional therapy, cognitive therapy pays more attention to the correction of bad behaviors, and pays more attention to patients' cognitive style and the harmony between cognition, emotion and behavior[10,11]. CBT is based on a psychologically developed style of care[12]. At present, it is increasingly widely used in the nursing of many chronic diseases. After CBT nursing intervention, patients can distinguish the emotional experience from the symptoms of the real body, build up confidence, re-understand the disease, reduce the adverse experience brought by free death, and enhance the confidence in overcoming the disease[13,14]. CBT can change patients' negative perception of their own pain. In orthodontic osteodilated arch (OOA) treatment, cognitive correction technology or behavioral therapy technology can be adopted, which is characterized by positivity, initiative and short time[15,16].
The comprehensive nursing intervention model combines the advantages of CBT, aiming to provide patients with holistic care and psychological support[17]. This model not only addresses patients' physiological needs but also pays attention to their psychological state. By integrating various nursing measures, it strives to comprehensively enhance treatment outcomes and patient satisfaction. This study applies CBT to the perioperative care of patients undergoing OOA and explores its clinical efficacy. The goal is to provide an effective comprehensive nursing intervention model for patients undergoing orthodontic arch expansion, alleviating their pain and psychological stress, improving treatment outcomes and quality of life, and providing reliable scientific evidence for clinical application.
There are 81 patients with maxillary arch stenosis who received OOA treatment in Orthodontics Department of Stomatology Hospital Affiliated to School of Medicine of Nanjing University from April 2022 to March 2023 were selected by convenient sampling method and randomly rolled into a control group (Ctrl group, 40 cases) and an observation group (Obs group, 41 cases). In the Ctrl group, there were 22 males and 18 females, ranging in age from 31 years to 73 years (49.6 ± 9.6 years in average). Nineteen males and 22 females were enrolled in the Obs group, aged from 33 years to 72 years (50.1 ± 8.4 years in average). General basic information of patients was recorded and collected. Prior to data collection, informed consent was signed according to study requirements; All data were recorded in customized study forms. Analysis on the general data of gender, age, weight, education level, occupation, and disease history of patients in different group exhibited no great difference (P > 0.05), showing that the research objects in various groups were comparable. The vital signs of patients were stable and there were no obvious contraindications. In this work, patients who fully met the inclusion criteria accepted the experimental regulations and signed experimental informed consent, and the study was approved by the Ethics committee of Nanjing Stomatological Hospital.
Criteria based on which the patients were enrolled could be described as follows: (1) Patients who were treated in XX hospital for a long time without obvious root or alveolar bone resorption on imaging; (2) Inpatients receiving detailed clinical treatment (including age, gender, and past drug use history); (3) Patients with no history of surgery or other treatments; (4) Patients with no other mental disorders; (5) Those with good understanding and communication skills; (6) Those with no systemic disease, drug allergy, or trauma history; and (7) Those with no congenital alveolar dysplasia or bone fenestration.
The patients were excluded according to the following criteria: (1) Patients disagreeing to participate in this study; (2) Patients with incomplete case data; (3) Patients with bimaxillary protrusion; (4) Patients with maxillary mass or cyst; (5) Patients with temporomandibular joint disorders; (6) Patients with congenital tooth loss; and (7) Patients with a history of orthodontic or maxillofacial surgery.
During the arch expansion for treatment, patients in the Ctrl group adopted routine nursing intervention mode, while those in the Obs group were guided to correctly master the personalized arch expansion program, and standardized the use of improved douches and improved floss mucosa preconditioning devices. It meant that the CBT-based comprehensive nursing intervention (CNI) mode was implemented.
CBT was introduced as follows. Specialized care of patients must have rich experience, high professionalism, high enthusiasm for work, enough care and patience, and be able to take the initiative to communicate with patients. Firstly, the patient was comprehensively evaluated, cognitive reconstruction was carried out according to the different psychological conditions of the patient, and corresponding measures were actively taken. It should explain the related knowledge of arch expansion treatment to patients, the effect after treatment, and actively eliminate the anxiety of patients. Then, the patients were given relaxation therapy, including breathing relaxation training and deep breathing by listening to slow music, twice a day for 30 minutes. Secondly, the self-rating anxiety scale (SAS) was employed to assess the mental state, blood pressure, heart rate, diagnosis of patients with different anxiety emotions actively psychological counseling to promote their good mental state and help them generate positive confidence to overcome the disease. For patients with great ideological pressure according to the serious emotions produced by the condition changes, they should be helped to eliminate the anxiety and fear of patients as far as possible, thus enhancing their confidence in the success of treatment.
Firstly, the incidence of oral mucositis and the degree of response, the mastery rate of correct arch expansion method, the degree of soft scale formation around the arch expansion abutment, and the degree of oral mucosa proliferation were compared between patients in different groups before and after intervention expansion. The soft scale index (SCI) was evaluated as no soft scale, the area covered by soft scale was less than 1/3, 1/3-2/3, and more than 2/3 of the tooth face neck, which were scaled as 0-3 points, respectively. The plaque index was calculated by 0 points based on no plaque on the tooth surface, 1 point based on dotted plaque, 2 points based on banded plaque (width ≤ 1 mm), 3 points based on plaque staining band exceeding 1 mm but covering area below 1/3 crown neck, 4 points based on plaque covering 1/3-2/3 crown, and 5 points based on plaque covering crown exceeding 2/3.
Secondly, the psychological status of the patients was evaluated by SAS. The SAS scale included items such as dyspnea, palpitation, frequency of urination, fear, panic, sedentary inability, and sleep disorder. There were 20 entries in total. Each entry included no/occasionally, sometimes, often, and always. Twenty items were graded at four levels. The scores added up to a rough score. The integral part of the score multiplied by 1.25 was the standard score. The total standard score of domestic SAS was (37.23 ± 0.46) points[18]. The questionnaire was filled out in the morning of the first day of treatment, and the patients were reminded to read the instructions on the questionnaire carefully to ensure that the questionnaire was completed within half an hour. The questionnaire recovery rate was 100%, and the questionnaire was filled in the form of anonymous recovery. The decomposition value of SAS standard score was 50 points, and the severe, moderate, and mild anxiety were scored as 70 or above, 60-69, and 50-59 points, respectively.
Thirdly, the visual analogue scale (VAS) was administered by the same nurse for both groups. The VAS was measured by a line of 10 cm, with “0” indicating no pain and “10” indicating the most unbearable pain. Patients were marked according to their own degree of feeling, and the measurement results showed 0-2 points as excellent, 3-5 points as good, 6-8 points as medium, and 8-10 points as poor. Postoperative VAS score of the patients was 0-3. Nursing effects of the two groups were observed and compared, namely, compliance (rehabilitation plan formulated by medical staff) and satisfaction (satisfaction to nursing staff).
The changes of angle indexes were compared before and after treatment. The measurements included the buccal inclination of the first molar on the right (RMA°) and the buccal inclination of the first molar on the left (LMA°). The extension of the long axis of the first molar was added to the plane of the palate to measure the internal angle.
SPSS20.0 was utilized for statistical processing of data. Count data were expressed as n (%). Normality test and variance test were performed on the measurement data. Data conforming to normal distribution and homogeneity of variance were represented by mean ± SD, and χ2 test was employed for comparison between counting data groups. Binary Logistic regression analysis was adopted to screen the factors affecting tumorigenesis. P < 0.05 was statistically significant.
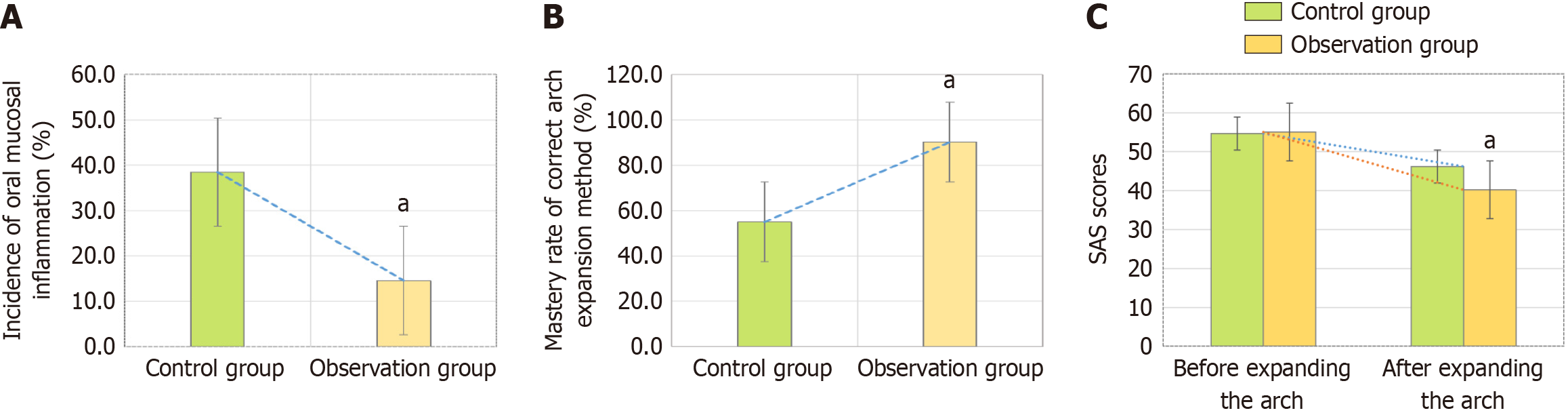
Incidence of oral mucositis and the mastery rate of correct arch expansion method and SAS score.
As illustrated in Figure 1A, the incidence of oral mucositis in the Obs group was 14.6 percent, while that in the Ctrl group was 38.5%, showing a great difference (P < 0.05). This suggested that the CBT-based CNI could greatly reduce the incidence of oral mucositis.
As demonstrated in Figure 1B, the mastery rate of correct arch expansion method of patients in the Obs group was 90.2%, which was greatly higher than that in the Ctrl group (55.0%), with an obvious significance (P < 0.05). This indicated that the CBT-based CNI could promote the mastery rate of correct arch expansion method in patients.
The SAS score in the Obs group before arch expansion was (55.02 ± 2.21), which was higher based on that in the Ctrl group (54.67 ± 2.35), showing a remarkable difference (P > 0.05). After arch expansion, the SAS scores of patients in the Obs group and Ctrl group were (40.02 ± 2.16) and (46.19 ± 2.11), respectively, suggesting that the patients receiving the CBT-based CNI showed a higher SAS score and exhibited a great difference with those in the Ctrl group (P < 0.05). This indicated that the anxiety of patients with arch expansion after CBT-based CNI was reduced, which can promote the recovery of the disease. The above results were specified in Figure 1C below.
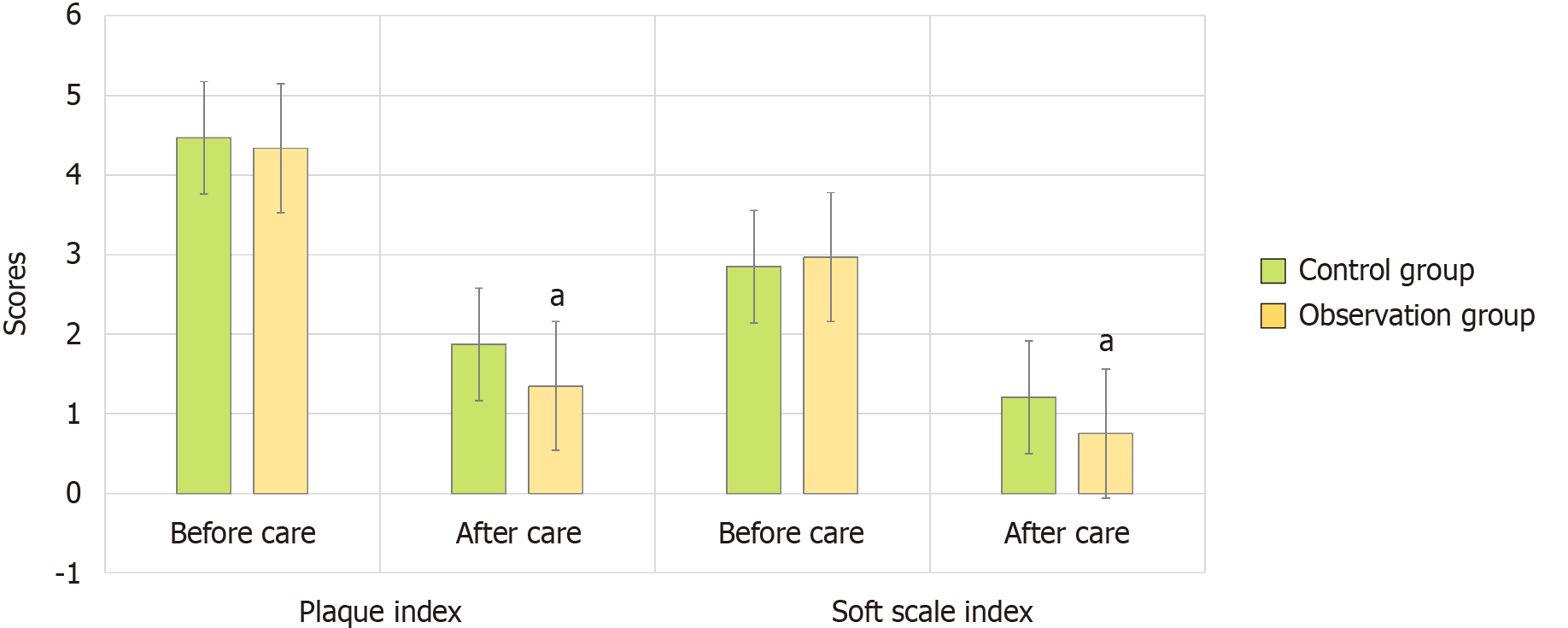
The plaque index and SCI of patients before and after they received different nursing modes were compared, as displayed in Figure 2 below.
Before nursing, the plaque index was 4.34 ± 0.63 in the Obs group and was 4.47 ± 0.34 in the Ctrl group. After nursing, the plaque indexes in the Obs and Ctrl groups were 1.35 ± 0.36 and 1.87 ± 0.41, respectively. It meant that the plaque index in patients receiving the CBT-based CNI was greatly decreased to that of patients intervened with the RBI (P < 0.05).
The SCI values in the Obs group before and after the patients were nursed were 2.97 ± 0.56 and 0.75 ± 0.31, respectively; while those in the Ctrl group were 2.85 ± 0.41 and 1.21 ± 0.35, respectively. In addition, the SCI value in the Obs group after nursing was greatly lower and possessed an obvious difference with P < 0.05 based on that in the Ctrl group.
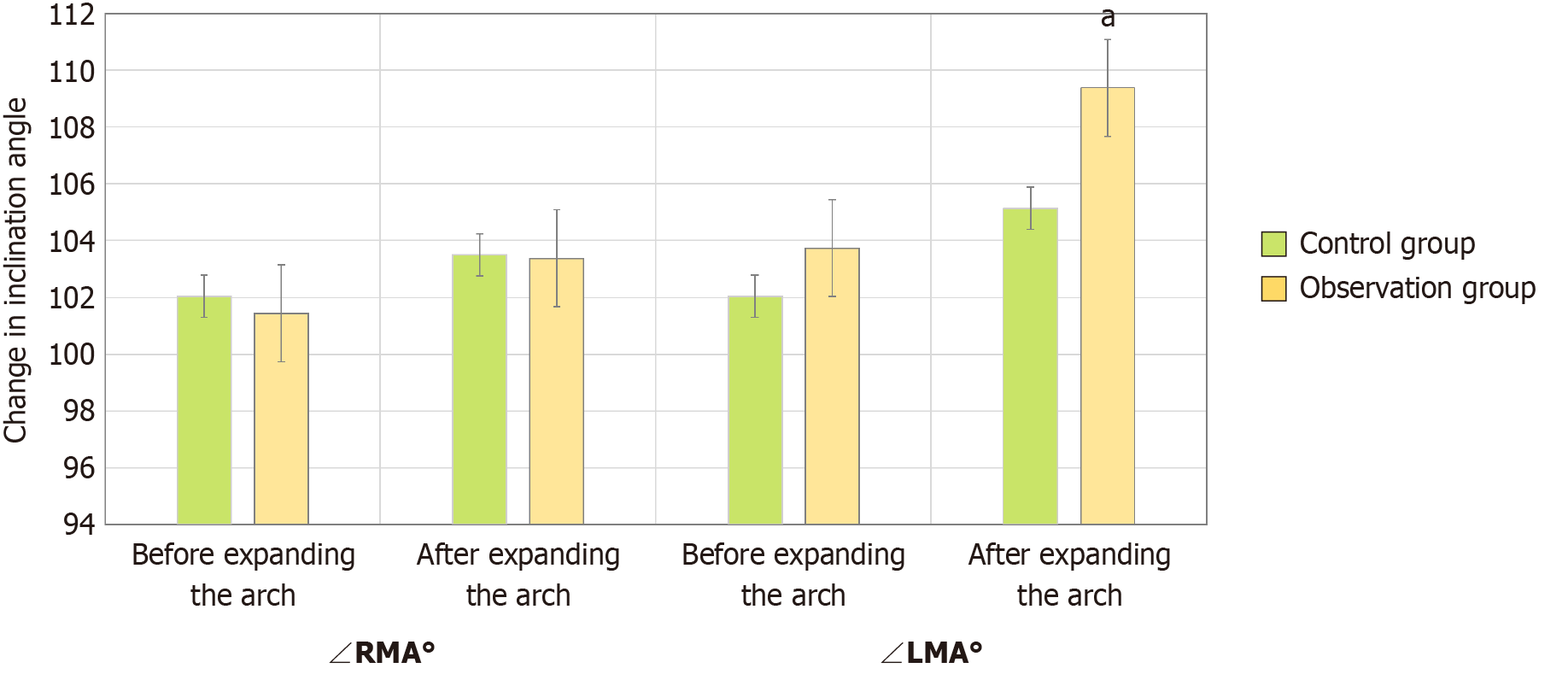
After different degrees of nursing, the change of buccal inclination angle of upper molars before and after arch expansion was compared for patients in different groups, as revealed in Figure 3 below. Before arch expansion, the RMA° was 101.43 ± 1.62 in the Obs group and 102.04 ± 0.34 in the Ctrl group. After arch expansion, the RMA° was 103.38 ± 1.81 in the Obs group and was 103.5 ± 0.34 in the Ctrl group, exhibiting no obvious difference (P > 0.05). Before arch expansion, the LMA° values were 103.74 ± 2.29 and 102.04 ± 2.53 in the Obs group and the Ctrl group, respectively. After arch expansion, they were 109.38 ± 2.19 and 105.14 ± 2.65, respectively, which exhibited great differences based on those before the arch expansion (P < 0.05).
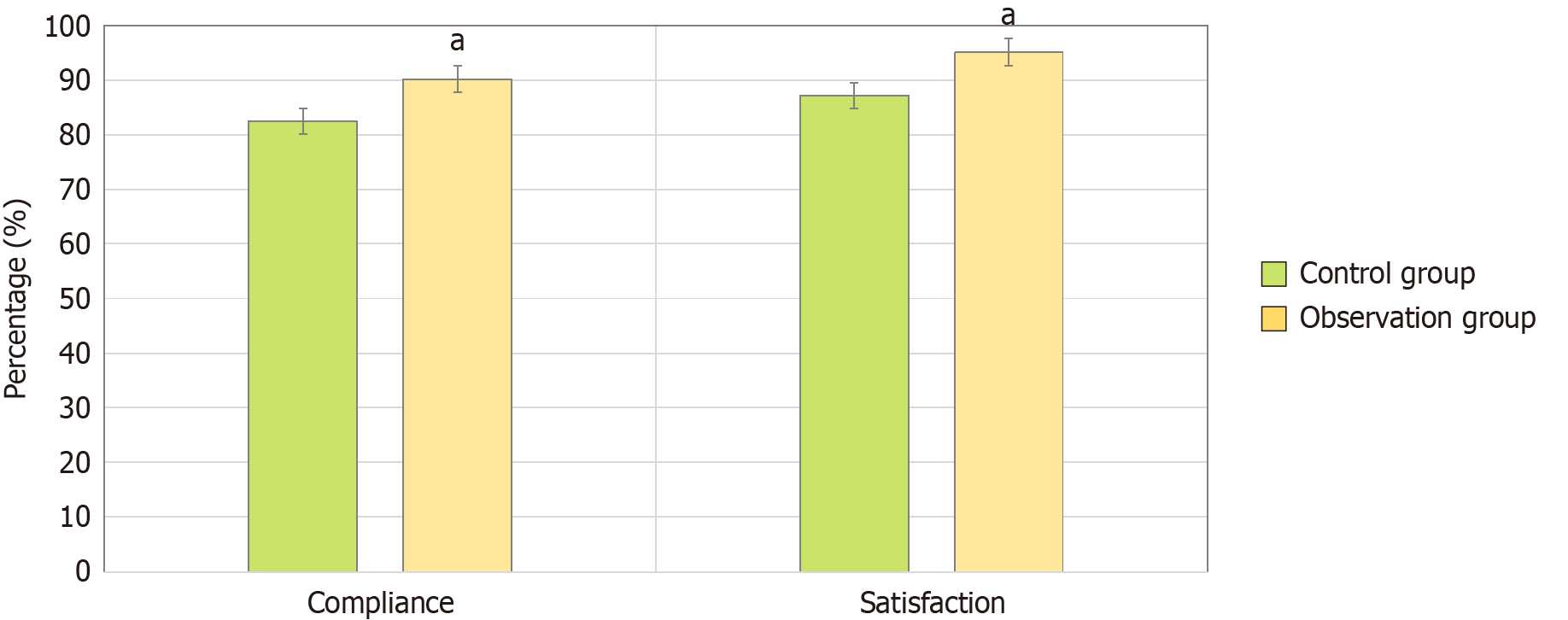
As explicated in Figure 4, in the Obs group, the numbers of patients with compliance and satisfaction were 37 (90.24%) and 39 (95.12%), respectively; while those were 33 (82.5%) and 34 (87.18%) in the Ctrl group. Therefore, the percentages of patients with compliance and satisfaction in the Obs group were much higher to those in the Ctrl group (P < 0.05).
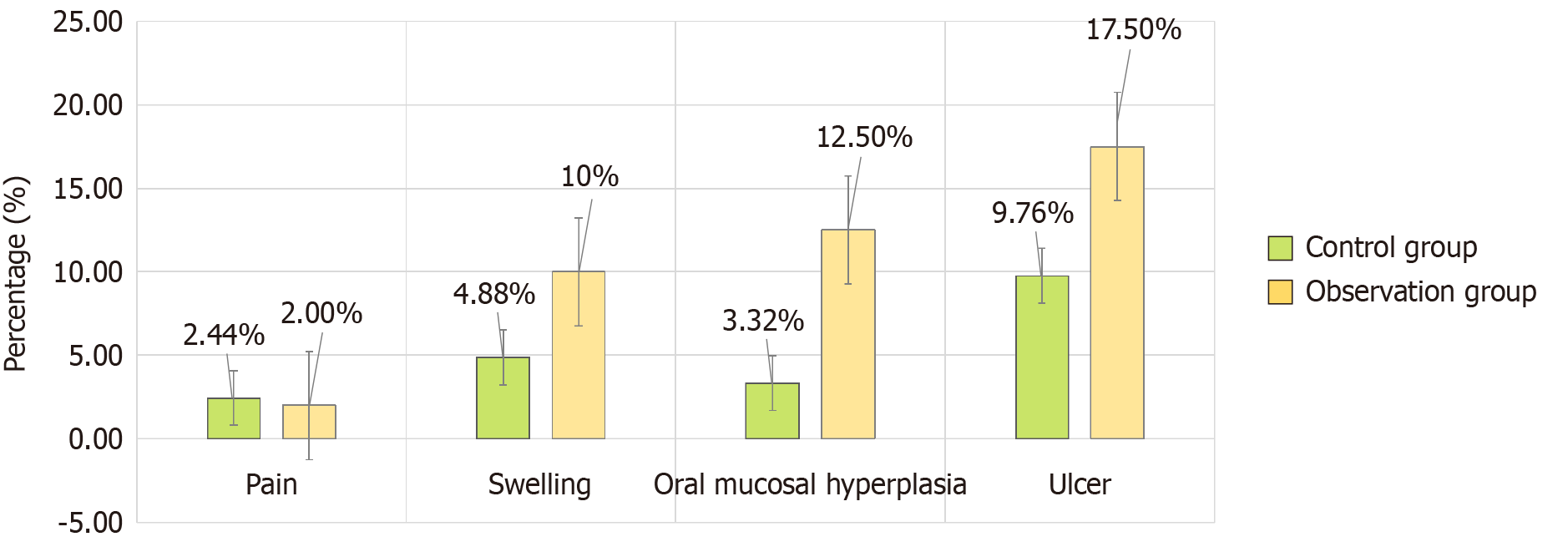
Figure 5 compared the complications in patients after they were intervened with different modes. In Obs group, there were 1 (2.44%) case with pain, 2 (4.88%) cases with swelling, 3 (3.32%) cases with oral mucosa hyperplasia, and 4 (9.76%) cases with ulcer. There were 2 (5.00%), 4 (10.00%), 5 (12.5%), and 7 (17.5%) cases with pain, swelling, oral mucosa hyperplasia, and ulcer, respectively. It suggested that fewer complications were observed in patients receiving CBT-based CNI after cognitive therapy care.
The biological basis of arch expansion treatment involves bone deposition at the mid-palatal suture, the high plasticity of the alveolar bone, and the compensatory effect of buccal tilting of the posterior teeth. The ideal conditions for arch expansion treatment are to maximize skeletal effects while avoiding buccal tipping of the posterior teeth[19]. The CNI model includes cognitive education, psychological counseling, behavior training, and emotional support for patients, helping them better cope with the various discomforts and psychological challenges during the treatment process. This study explores the application effects of CNI and CBT in patients undergoing orthodontic arch expansion. The results show that the combination of CNI and CBT in comprehensive nursing intervention significantly improves treatment outcomes, patient satisfaction, and quality of life. In this study, patients receiving comprehensive nursing intervention demonstrated higher compliance and enthusiasm during the treatment process. CNI, through personalized care plans, psychological support, and health education, effectively helped patients understand and accept the treatment, enhancing their trust and involvement. This is consistent with previous studies[20,21], proving the importance of comprehensive nursing intervention in improving overall treatment outcomes for patients. CBT was used in this study to help patients adjust their cognitive and emotional responses to orthodontic arch expansion treatment. CBT alleviated their anxiety and stress by changing their perceptions of the treatment process and outcomes, enhancing psychological preparedness and adaptability. The study found[22] that patients who received CBT showed fewer symptoms of anxiety and depression during treatment, consistent with the documented effectiveness of CBT in various medical interventions. A significant finding of this study is that the combined intervention of CNI and CBT has a notable synergistic effect on overall treatment efficacy for patients. Compared to using CNI or CBT alone, the combined intervention showed more significant improvements in patients' psychological state, treatment compliance, and satisfaction. This finding suggests that the comprehensive application of multiple intervention methods better meets the holistic needs of patients, optimizing treatment outcomes in orthodontic arch expansion.
Chesak et al[22] showed that CBT could improve patients' sleep quality and quality of life. Yang et al[23] showed that mindfulness-based psychological care could relieve patients' anxiety. Moradi et al[24] showed that CBT could signi
The CBT-based nursing model can relieve the anxiety of patients, assess their psychological status by means of conversation, eliminate the adverse effects of patients’ anxiety on the disease in the atmosphere of laughter, and thus promoting the recovery of the disease. After treatment with arch expansion, OOA patients will inevitably have psychological burden due to the existence of orthotics. The use of CBT nursing model in patients with relatively stable mood to give health guidance, can improve the compliance of patients. Satisfaction is not only the most direct standard to reflect the quality of nursing work, but also the highest standard of nursing. In this work, the patient satisfaction after the CBT-based CNI (95.12%) was much higher than to that after the RBI (87.18%) (P < 0.05). These results indicated that patients had higher CNI satisfaction with cognitive therapy. Park et al[25] suggested that CBT could relieve depression. Rajabi et al[17] can alleviate the sleep disorders of patients. In this work, CBT could improve compliance, because the compliance of patients with CBT-based CNI was higher to that of patients receiving the RBI, showing an obvious difference (P < 0.05). After CBT care, the plaque index and SCI of patients in the Obs group were much better than those in the Ctrl group (P < 0.05), which promotes a better oral hygiene environment. In conclusion, the CBT-based CNI comprehensive nursing has better disease rehabilitation effect, worthy of clinical promotion.
CBT-based CNI model is very necessary during treatment with arch expansion for OOA patients, and can improve the mastery rate of correct arch expansion method, better the therapeutic effect of arch expansion, effectively enhance the oral health of patients, prevent the occurrence of oral mucositis, and reduce the severity of oral mucositis. The sample size herein was relatively small, which had certain limitations. The follow-up research can be combined with more samples for in-depth exploration, and it is believed that there will be more breakthroughs.
| 1. | Cui Y, Zhang F, Zhu C, Geng L, Tian T, Liu H. Upregulated lncRNA SNHG1 contributes to progression of non-small cell lung cancer through inhibition of miR-101-3p and activation of Wnt/β-catenin signaling pathway. Oncotarget. 2017;8:17785-17794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 185] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 2. | Alves ACM, Janson G, Mcnamara JA Jr, Lauris JRP, Garib DG. Maxillary expander with differential opening vs Hyrax expander: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2020;157:7-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Massaro C, Janson G, Miranda F, Aliaga-Del Castillo A, Pugliese F, Lauris JRP, Garib D. Dental arch changes comparison between expander with differential opening and fan-type expander: a randomized controlled trial. Eur J Orthod. 2021;43:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Kapetanović A, Theodorou CI, Bergé SJ, Schols JGJH, Xi T. Efficacy of Miniscrew-Assisted Rapid Palatal Expansion (MARPE) in late adolescents and adults: a systematic review and meta-analysis. Eur J Orthod. 2021;43:313-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 5. | Elnagar MH, Elshourbagy E, Ghobashy S, Khedr M, Evans CA. Dentoalveolar and arch dimension changes in patients treated with miniplate-anchored maxillary protraction. Am J Orthod Dentofacial Orthop. 2017;151:1092-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Garib D, Lauris RC, Calil LR, Alves AC, Janson G, De Almeida AM, Cevidanes LH, Lauris JR. Dentoskeletal outcomes of a rapid maxillary expander with differential opening in patients with bilateral cleft lip and palate: A prospective clinical trial. Am J Orthod Dentofacial Orthop. 2016;150:564-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | de Almeida AM, Ozawa TO, Alves ACM, Janson G, Lauris JRP, Ioshida MSY, Garib DG. Slow versus rapid maxillary expansion in bilateral cleft lip and palate: a CBCT randomized clinical trial. Clin Oral Investig. 2017;21:1789-1799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Nagrik AP, Bhad WA, Chavan SJ, Doshi UH. A randomized clinical trial to assess the sagittal effects of Transforce transverse appliance (TTA) and NiTi palatal expander (NPE) on skeletal class II malocclusion in growing patients during retention phase - A cephalometric study using a historical control group. Int Orthod. 2020;18:722-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | de Medeiros Alves AC, Garib DG, Janson G, de Almeida AM, Calil LR. Analysis of the dentoalveolar effects of slow and rapid maxillary expansion in complete bilateral cleft lip and palate patients: a randomized clinical trial. Clin Oral Investig. 2016;20:1837-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Ganal-Vonarburg SC, Duerr CU. The interaction of intestinal microbiota and innate lymphoid cells in health and disease throughout life. Immunology. 2020;159:39-51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 63] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 11. | Stefan S, Cristea IA, Szentagotai Tatar A, David D. Cognitive-behavioral therapy (CBT) for generalized anxiety disorder: Contrasting various CBT approaches in a randomized clinical trial. J Clin Psychol. 2019;75:1188-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Pan MR, Huang F, Zhao MJ, Wang YF, Wang YF, Qian QJ. A comparison of efficacy between cognitive behavioral therapy (CBT) and CBT combined with medication in adults with attention-deficit/hyperactivity disorder (ADHD). Psychiatry Res. 2019;279:23-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Meng FP, Zhou LN. Positive role of cognitive-behavioral therapy on sexual dysfunction and behavioral problems in prostate cancer-treated patients. J Biol Regul Homeost Agents. 2020;34:1049-1052. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Serrat M, Sanabria-Mazo JP, Almirall M, Musté M, Feliu-Soler A, Méndez-Ulrich JL, Sanz A, Luciano JV. Effectiveness of a Multicomponent Treatment Based on Pain Neuroscience Education, Therapeutic Exercise, Cognitive Behavioral Therapy, and Mindfulness in Patients With Fibromyalgia (FIBROWALK Study): A Randomized Controlled Trial. Phys Ther. 2021;101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 15. | Pinhas-Hamiel O, Hamiel D. Cognitive Behavioral Therapy and Mindfulness-Based Cognitive Therapy in Children and Adolescents with Type 2 Diabetes. Curr Diab Rep. 2020;20:55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Moberg C, Niles A, Beermann D. Guided Self-Help Works: Randomized Waitlist Controlled Trial of Pacifica, a Mobile App Integrating Cognitive Behavioral Therapy and Mindfulness for Stress, Anxiety, and Depression. J Med Internet Res. 2019;21:e12556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 17. | Rajabi Majd N, Broström A, Ulander M, Lin CY, Griffiths MD, Imani V, Ahorsu DK, Ohayon MM, Pakpour AH. Efficacy of a Theory-Based Cognitive Behavioral Technique App-Based Intervention for Patients With Insomnia: Randomized Controlled Trial. J Med Internet Res. 2020;22:e15841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 18. | Heckler CE, Garland SN, Peoples AR, Perlis ML, Shayne M, Morrow GR, Kamen C, Hoefler J, Roscoe JA. Cognitive behavioral therapy for insomnia, but not armodafinil, improves fatigue in cancer survivors with insomnia: a randomized placebo-controlled trial. Support Care Cancer. 2016;24:2059-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Peoples AR, Garland SN, Pigeon WR, Perlis ML, Wolf JR, Heffner KL, Mustian KM, Heckler CE, Peppone LJ, Kamen CS, Morrow GR, Roscoe JA. Cognitive Behavioral Therapy for Insomnia Reduces Depression in Cancer Survivors. J Clin Sleep Med. 2019;15:129-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | van Manen AS, Aarts S, Metzelthin SF, Verbeek H, Hamers JPH, Zwakhalen SMG. A communication model for nursing staff working in dementia care: Results of a scoping review. Int J Nurs Stud. 2021;113:103776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 21. | Nes AAG, Steindal SA, Larsen MH, Heer HC, Lærum-Onsager E, Gjevjon ER. Technological literacy in nursing education: A scoping review. J Prof Nurs. 2021;37:320-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 22. | Chesak SS, Rhudy LM, Tofthagen C, Chlan LL. A practice-based model to guide nursing science and improve the health and well-being of patients and caregivers. J Clin Nurs. 2022;31:445-453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 23. | Yang J, Tang S, Zhou W. Effect of Mindfulness-Based Stress Reduction Therapy on Work Stress and Mental Health of Psychiatric Nurses. Psychiatr Danub. 2018;30:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Moradi M, Akbari M, Alavi M. The effect of cognitive-behavioral therapy on death anxiety and depression in patients with heart failure: A quasi-experimental study. Perspect Psychiatr Care. 2022;58:2791-2799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Park S, Sato Y, Takita Y, Tamura N, Ninomiya A, Kosugi T, Sado M, Nakagawa A, Takahashi M, Hayashida T, Fujisawa D. Mindfulness-Based Cognitive Therapy for Psychological Distress, Fear of Cancer Recurrence, Fatigue, Spiritual Well-Being, and Quality of Life in Patients With Breast Cancer-A Randomized Controlled Trial. J Pain Symptom Manage. 2020;60:381-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 111] [Article Influence: 22.2] [Reference Citation Analysis (0)] |