Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.4973
Revised: June 5, 2024
Accepted: June 17, 2024
Published online: August 6, 2024
Processing time: 62 Days and 22 Hours
Nasolabial fold (NLF) depression can affect the facial appearance of patients to some extent and increase their psychological burdens. In recent years, autologous fat grafting (AFG) combined with botulinum toxin A (BTX-A) injection (AFG + BTX-A injection) has been gradually applied in the treatment of patients with NLF depression. Although studies have been conducted on the efficacy and safety of AFG + BTX-A injection in treating NLF depression, the experimental design, observational indicators, and sample enrollment criteria vary remarkably, making it difficult to draw convincing and consistent conclusions. Thus, further relevant research is warranted.
To assess the esthetic improvement, efficacy, and safety of AFG + BTX-A injec
This study included 60 patients with NLF depression who were treated in our hospital from February 2019 to April 2021. These patients were categorized into control (n = 30) and observation (n = 30) groups. The observation group received AFG + BTX-A injection, whereas the control group underwent AFG only. All patients were evaluated using the wrinkle severity rating scale (WSRS) and global aesthetic improvement scale. The compactness of facial contours, skin evaluation indexes, adverse reactions, and satisfaction of the two groups were evaluated 3 months postoperatively.
The WSRS scores of the observation group at 1, 3, and 6 months postoperatively were lower than those of the control group (P < 0.05). Three months postoperatively, facial fine lines and pores showed obvious improvement and the skin index score was higher in the observation group than in the control group (P < 0.05). The compactness of facial contours was better in the observation group than in the control group (P < 0.05). In addition, no remarkable differences were noted in the incidence of postoperative adverse reactions such as facial stiffness, facial asymmetry, facial bruising, and facial concavity inequality (P > 0.05).
AFG + BTX-A injection is a highly safe, cost-effective, effective, and long-lasting treatment for NLF depression with high esthetic value, which should be promoted in the future.
Core Tip: The nasolabial fold (NLF) is not only the most prominent feature of midface aging but also a challenging treatment area for plastic surgeons. The combination therapy of botulinum toxin A (BTX-A) injection and autologous fat grafting (AFG) is becoming increasingly popular in the treatment of NLF depression. Although this protocol has certain clinical advantages, the conclusions of previous studies are somewhat controversial. This study revealed that AFG + BTX-A injection is a highly safe, economical, effective, and long-lasting treatment for NLF depression with high esthetic value. Further cross-regional, multicenter, and large-sample studies are warranted to obtain more accurate evidence in clinical practice.
- Citation: Wang RJ, Wang Y, Wu JF, Si TT. Clinical effect of botulinum toxin type A combined with autologous fat grafting in patients with nasolabial fold depression. World J Clin Cases 2024; 12(22): 4973-4982
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/4973.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.4973
The nasolabial fold (NLF) is the dividing line between the cheek and nasal alar and upper lip[1]. Factors influencing NLF depression can be categorized into dynamic and nondynamic factors. Dynamic factors refer to factors related to changes in facial expression, particularly when smiling, and contractions of the perioral muscles, including levator labialis alar muscle, levator labialis muscle, zygomatic major muscle, zygomatic minor muscle, and transverse part of the nasal muscle. These muscles are closely connected to the skin and soft tissues on their surfaces. Upon contraction, these muscles pull the skin and soft tissues on their surfaces outward, resulting in NLF depression. Nondynamic factors refer to factors related to aging. The less elastic fibers in the outer skin of the NLF lead to skin relaxation, the subcutaneous fat content on the outside of the NLF is higher than that on the inside, and the sagging of the zygomatic fat pad of the NLF leads to NLF depression. The lateral area of the NLF has many fibrous septa and is rich in adipose tissue[2]. The NLF is the most prominent feature of midfacial aging. The structure of the NLF is extremely complex, making it a challenging treatment area for plastic surgeons. Traditional facelift surgery is associated with trauma, high risk, and uncertain curative effects[3]. The number of patients seeking improvement of NLF depression is also increasing, thus broadening the treatment options[4].
Currently, autologous fat particles are used as natural autologous soft tissue fillers. Autologous fat particles are abundant in the tissue source, do not induce foreign body rejection reaction, have a texture similar to that of the normal tissue, and appear natural. However, according to a previous study, the fat absorption rate after autologous fat grafting (AFG) is high (25%-80%)[5]. Many factors affect the survival of fat cells after AFG, such as revascularization of grafts, fat cell injury, narcotic drugs, material purification methods, fat filling, amount of fat transplanted, and infection. With the advancement of surgical methods, the damage to fat cells during material purification and fat filling has been greatly reduced, improving the survival rate of fat cells after AFG[6]. In recent years, restoration of the blood circulation of adipocytes, promotion of the differentiation of preadipocytes, and enhancement of the survival rate of fat cells after AFG have become research hotspots[7].
Botulinum toxin A (BTX-A) is secreted by an anaerobic gram-positive bacterium — Clostridium tumefaciens — which is mainly composed of proteins and induces strong neurotoxicity. BTX-A primarily acts at the neuromuscular junction, cleaves the prominent associated proteins, inhibits the release of acetylcholine from the presynaptic membrane of the nerve endings, and blocks the conduction of nerve impulses to the muscles. Moreover, it blocks the transmission of neuromuscular excitations to the pathway, which prevents excitatory contractions of perioral muscles (such as labialis externa and turbinatus) and fibrillatory muscles, and solves the kinetic factor for NLF depression.
AFG combined with BTX-A injection (AFG + BTX-A) can act on both nondynamic and dynamic factors of NLF depression. Thus, AFG + BTX-A can block oral angular muscles, maintain the stable fixation of the transplanted adipose tissue during the early stage, and accelerate revascularization, thus improving the survival rate of the transplanted adipose tissue[8].
Currently, hyaluronic acid fillers are the main skin fillers used clinically; however, they have short-term efficacy and are associated with embolism, allergy, and other adverse reactions[9]. In recent decades, AFG + BTX-A has become more popular in the treatment of NLF depression, which has the advantages of less trauma, rapid recovery, lower malpractice rate, higher safety, fewer adverse reactions, and being convenient and economical. However, previous studies greatly differed in experimental design, observational indexes, and sample enrollment criteria, preventing the drawing of consistent conclusions. Therefore, further relevant research is warranted. This study aimed to determine the clinical effect of AFG + BTX-A in patients with NLF depression.
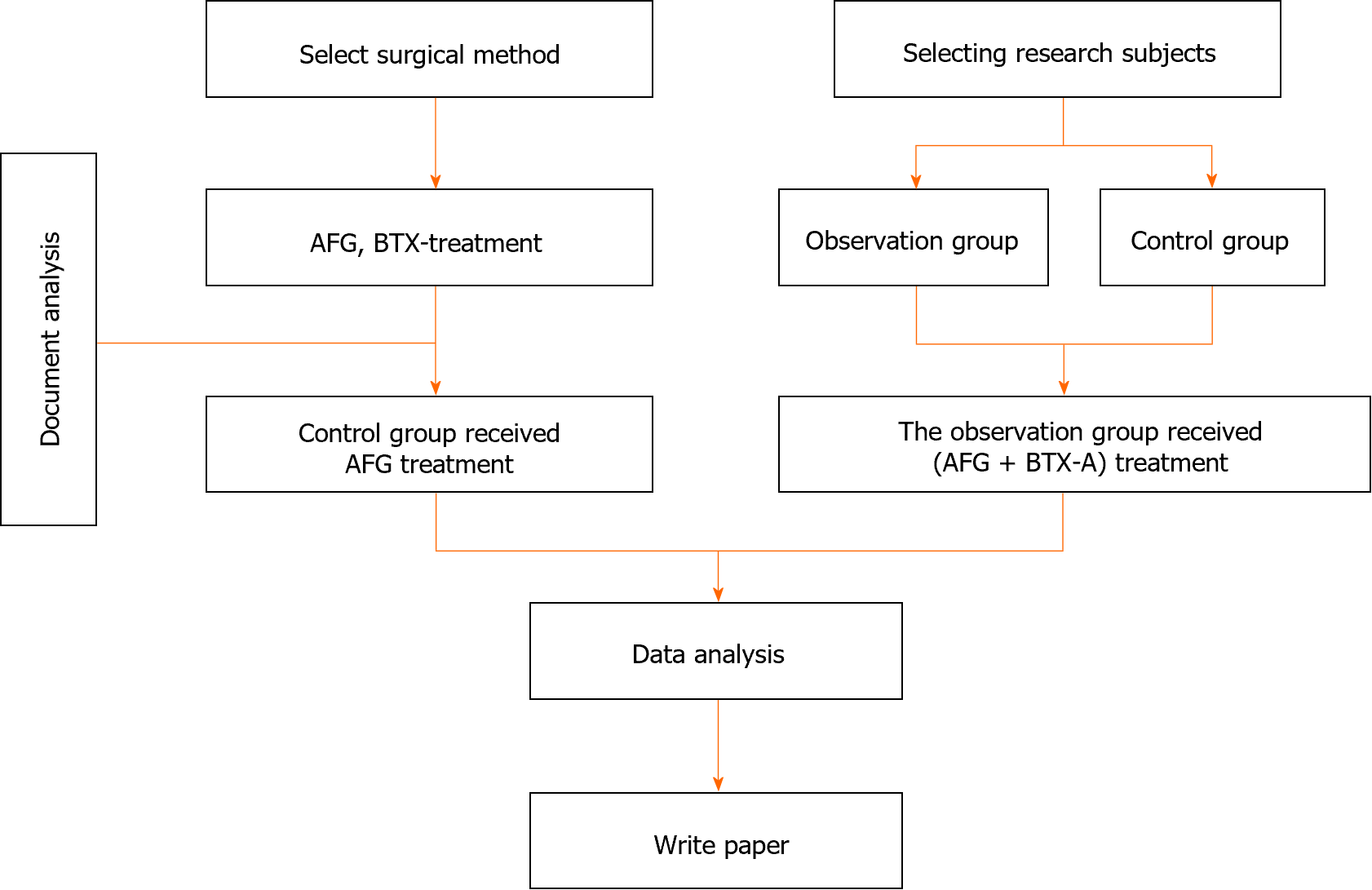
The research flow chart is shown in Figure 1.
This study included 60 patients with NLF depression who were treated in the 903rd Hospital of PLA from February 2019 to April 2021. These patients were classified into control (n = 30) and observation (n = 30) groups. No remarkable differences in general data were noted (P > 0.05, Table 1).
| Group | Sample size (n) | Age (years) | BMI (kg/m2) | Number of years of education (years) |
| Observation group | 30 | 50.96 ± 3.58 | 23.14 ± 2.24 | 9.55 ± 1.20 |
| Control group | 30 | 50.91 ± 3.63 | 23.08 ± 2.28 | 9.60 ± 1.24 |
| t | 0.053 | 0.103 | 0.159 | |
| P value | > 0.05 | > 0.05 | > 0.05 |
The inclusion criteria were as follows: (1) Patients aged ≥ 18 years; (2) Those who had no cognitive, language, or intellectual impairment and had basic reading and writing ability; (3) Those who met the diagnostic criteria for NLF depression[10] and had wrinkle severity rating scale (WSRS) score[10] of 2-5; (4) Those who had no surgical contraindications and severe cardiovascular and pulmonary diseases; (5) Those who had no history of allergy to BTX-A drug-related components; and (6) Those who had no obvious abnormalities in blood routine and coagulation function.
The exclusion criteria were as follows: (1) Patients who had severe heart, liver, or kidney insufficiency; malignant tumors; or other diseases; (2) Those who received facial rejuvenation-related treatment for facial aging in the past 6 months; (3) Those who were allergic to any components of BTX-A drugs; (4) Those with infection or ulcers in the injection area; (5) Those with blood system diseases or poor blood coagulation function or those with bleeding tendencies who received anticoagulation therapy; (6) Those with poor wound healing or history of keloid; (7) Those who had a recent intake of drugs that affect the neuromuscular junction, such as quinine, aminoglycoside, and morphine, or those with systemic neuromyopathy, such as myasthenia gravis, Lambert-Eaton syndrome, and motor neuron disease; (8) Those with major life-threatening diseases; (9) those with fever or acute infectious diseases; (10) Children, older adults, pregnant and lactating women, and menstruating women; or (11) Those with obvious psychological disorders, such as depression, physical disorders, or unrealistic expectations of postoperative results and more than correct understanding of their facial aging.
Sample size: Bilateral α was 0.05 and β was 0.20. The clinical effect (total effective rate) was considered the effect index, with P1 of 0.95 and P2 of 0.75. According to the calculation, each group should include 27 samples. Considering a shedding rate of 10%, each group included 30 patients, with a total sample size of 60.
The observation group received AFG + BTX-A injection, whereas the control group underwent AFG only.
AFG: Based on the site of subcutaneous fat accumulation as well as the requirements of the patients, the abdomen and anterior medial thigh are usually selected for liposuction. Methylene blue was used to mark the liposuction area and facial filling area.
Local anesthesia and local swelling anesthesia were used during incision. A 3.0-mm incision was made in the medial thigh and the concealed part of the Yin. The swelling fluid (20 mL of 2% lidocaine, 1 mL of 0.1% epinephrine, and 1000 mL of normal saline) was injected slowly and evenly from the deep to shallow part and from the edge to the center of the operation area. As the tissue was pale and hard, the local area could be massaged appropriately. Liposuction was performed after an interval of 15 min. The liposuction tube with a diameter of 3.0 mm was connected to a negative-pressure liposuction machine or a 20-mL syringe to pump the fluid evenly and slowly. The thickness of subcutaneous fat was approximately 1 cm; thus, the amount of fat extracted was three times the amount to be filled. The fat mixture was filtered with an aseptic gauze and cotton pad to remove fibrous tissues.
Some fat particles were selected from the syringe. A 1-mm blunt-tipped liposuction cannula was attached to a 2-mL syringe containing autologous fat particles, and the needle was inserted into the distal corner of the mouth in the direction of the medial NLF. The injection levels included the subcutaneous layer and supraperiosteal space, and the injection followed the principle of multiple points and multiple planes. The injection volume can be appropriately increased in areas with obvious wrinkles owing to the characteristics of the adipose tissue, and the adipose tissue should be optimally distributed in the operation area. The amount of single-point injection should not exceed 0.1 mL to avoid clumping of the adipose tissue, which may affect its blood circulation and absorption. The filling area should be anesthetized with the swelling solution, and an optimal amount of injection volume should cover the filling area evenly. The filling doses were as follows: Forehead, 5.0-15.0 mL; temple, 5.0-10.0 mL/side; eyebrow arch, 1.0-2.0 mL/side; brow center, 1.0-2.0 mL/side; tear trough, 0.3-1.0 mL/side; NLF, 3.0-5.0 mL/side; zygomatic cheek, 6.0-15.0 mL/side; and chin, 4.0-8.0 mL/side. After pressing and shaping, the patient was asked to make a smiling expression repeatedly to observe whether the NLF on both sides were symmetrical and whether the transition with the cheeks was smooth and natural. Depending on the patient’s specific situation, a small amount of supplemental injections can be added.
BTX-A injection: Immediately after fat filling, patients in the observation group were injected with BTX-A (100 U/branch; Lanzhou Institute of Biological Products Co., Ltd.) mixed with 2 mL of saline at a concentration of 50 U/mL. In this study, 25 UA botulinum toxin was diluted with normal saline to 2.5 mL and fully mixed, and the mixture was connected to an electronic syringe (DermaShine Company, South Korea). Five-needle treatment head was selected at a dose of 0.0179-0.0208 mL, and the needle depth was 1.0-1.2 mm. Before injection, the patient was asked to make a dynamic smiling expression to determine the most obvious muscle protrusions on both sides of the NLF, which were marked with methylene blue, and the corresponding auxiliary points were marked according to the patient’s specific situation.
The distance between the marked points was approximately 1 cm, the injection area was routinely sterilized, and the needle was inserted vertically into the superficial subcutaneous layer to start the injection process. The injection depth reached up to the superficial layer of facial muscles; therefore, BTX-A can be evenly distributed in the injection area. BTX-A spreads and penetrates into the deeper expression muscles. The BTX-A dose was 1-2 U per injection site, and the injection site and dose must be the same on both sides. Epinephrine must be prepared to avoid allergic reactions.
WSRS: The WSRS[11] has been clinically verified, and items are scored 1-5. The scores positively correlated with the severity of wrinkles. Patients were evaluated before and 1, 3, and 6 months after the operation. The evaluation criteria are shown in Table 2.
| Scoring | Degree | Description |
| 5 | Extremely heavy | The wrinkles are extremely deep and long, stretching inch folded 2-4 mm |
| 4 | Heavy weight | The folds are deep, long, and obvious, and the folds stretch 2 mm in the middle |
| 3 | Moderate | The folds are deep and clear, but the folds disappear when they are stretched |
| 2 | Mild | There are shallow wrinkles, slight dents, and fine folds |
| 1 | None | There are no visible folds, showing the presence of only continuous skin lines |
Skin index score: The skin health status of the patients was evaluated 3 months postoperatively. The skin color, texture, pores, wrinkles, and grease were evaluated using the self-designed skin index score scale of our hospital. The full score was 10, with 0 indicating ineffective; 1-3, slight improvement; 4-6, remarkable improvement; and 7-10, remarkable improvement.
The compactness of facial contours was evaluated by comparing photos before and 3 months after the operation, and facial improvement was categorized as obviously effective, effective, and ineffective (based on our hospital’s self-designed evaluation standard).
Obviously effective: The facial outline is extremely smooth and relaxed; atrophy and depression are obviously improved to achieve the desired results.
Effective: The facial outline is generally smooth and relaxed; atrophy and depression are improved. There exists a gap with expectations, but the gap is acceptable.
Ineffective: The improvement of the facial contour, relaxation, atrophy, and depression is not obvious, and the treatment effect is not satisfactory.
Efficiency = (effective + effective)/total number of instances × 100%.
The esthetic improvement of patients with NLF depression was evaluated using the global aesthetic improvement scale (GAIS) score[11], which was calculated once before and 1, 3, and 6 months after the operation. The evaluation criteria are shown in Table 3.
| Grading | Description | |
| 1 | Remarkable improvement | Good improvement effect |
| 2 | Great improvement | The appearance is obviously improved, but it is not the best |
| 3 | Limited improvement | The appearance is obviously improved compared with the initial state, but supplementary treatment is recommended |
| 4 | No improvement | Basically no change |
| 5 | Worsen | The appearance is even worse than that before the operation |
The incidence of adverse reactions (including facial stiffness, facial asymmetry, facial bruising, and facial concavity inequality) in the two groups within 3 months after the operation were recorded. It was determined that the lower the incidence of adverse reactions, the higher the safety of treatment.
Data analysis and processing were performed using IBM SPSS Statistics for Windows version 21.0. Initially, the normal distribution and variance homogeneity of the measurement data were evaluated. Mean ± SD was used to indicate measurements with a normal distribution or almost normal distribution. The two groups were compared using paired t-tests, whereas a separate comparison of the two groups was performed using independent samples t-tests. Counting data were presented as n (%), and the χ2 test was employed. P value of < 0.05 were considered to indicate statistical significance.
The observation group had the following characteristics: Age, 40-58 (mean, 50.96 ± 3.58) years and body mass index (BMI), 17.55-27.88 (mean, 23.14 ± 2.24) kg/m2. This group included 30 women. The years of education ranged from 6 to 16 (mean, 9.55 ± 1.20) years.
The control group had the following characteristics: Age, 41-59 (mean, 0.91 ± 3.63) years and BMI, 17.46-27.90 (mean, 23.08 ± 2.28) kg/m2. This group included 30 women. No remarkable difference was noted in sex, age, BMI, and years of education (P > 0.05), as shown in Table 1.
No remarkable difference was noted in the WSRS scores before the operation (P > 0.05). After the operation, the WSRS scores of the patients decreased. The WSRS scores of the observation group at 1, 3, and 6 months postoperatively were lower than those of the control group (P < 0.05) (Table 4).
Three months postoperatively, the facial fine lines and pores in the observation group were remarkably improved, and the patients felt that their skin was delicate and shiny. The score was significantly higher in the observation group than in the control group (P < 0.05) (Table 5).
| Group | n | Color and luster | Texture | Pore | Wrinkles | Fat |
| Observation group | 30 | 5.60 ± 1.77 | 6.03 ± 1.86 | 4.87 ± 1.40 | 6.13 ± 1.80 | 6.07 ± 1.76 |
| Control group | 30 | 4.70 ± 1.36 | 5.10 ± 1.39 | 2.10 ± 1.34 | 5.03 ± 1.79 | 3.13 ± 1.65 |
| t | 2.201 | 2.192 | 7.773 | 2.382 | 6.654 | |
| P value | < 0.05 | < 0.05 | < 0.05 | < 0.05 | < 0.05 |
Three months postoperatively, the compactness of facial contours was better in the observation group than in the control group (P < 0.05) (Table 6).
| Group | n | Obvious effect | Effective | Invalid | Effectiveness rate |
| Observation group | 30 | 15 (50.00) | 10 (33.33) | 5 (16.67) | 25 (83.33) |
| Control group | 30 | 6 (20.00) | 12 (40.00) | 12 (40.00) | 18 (60.00) |
| χ2 | 4.022 | ||||
| P value | < 0.05 |
No remarkable difference was noted in GAIS scores before the operation (P > 0.05). After the operation, the GAIS scores of both groups decreased. The GAIS scores before and 1, 3, and 6 months after the operation were lower and the esthetic degree was higher in the observation group than in the control group (P < 0.05) (Table 7).
The incidences of facial stiffness, facial asymmetry, facial bruising, and facial concavity inequality between the two groups during treatment and follow-up were collected and analyzed, and the difference was not statistically significant (P > 0.05) (Table 8).
| Group | n | Facial stiffness | Facial asymmetry | Surgical area bruising | Facial unneveness |
| Observation group | 30 | 10 (33.33) | 1 (3.33) | 7 (23.33) | 6 (20.00) |
| Control group | 30 | 12 (40.00) | 2 (6.66) | 8 (26.67) | 8 (26.67) |
| χ2 | 0.287 | 0.351 | 0.889 | 0.373 | |
| P value | > 0.05 | > 0.05 | > 0.05 | > 0.05 |
The NLF is a depressed area of the midface extending from the lateral side of the nasal alar to the corner of the mouth, indicating the dividing line between the cheek and nasolabial region. Gradual deepening of the NLF is a prominent feature of midfacial aging. The mechanism underlying NLF depression is complex[12-14], which may be due to the loss of deep fat and atrophy of midfacial muscles; however, the specific tissue structure related to NLF depression remains unknown. The NLF is composed of the superficial fat layer of the superficial fascia[15]. Currently, NLF depressions are mainly categorized into dermatologic, fat pad, muscular, and skeletal types. Filler injections are indicated for the cutaneous and skeletal types. Fat pad-type depressions can be corrected via liposuction or surgery, and muscular-type depressions can be treated with botulinum toxin.
Currently, commonly used treatments include various types of filling and laser alone or combined application, dioxanone monomer line (pmurdioxanone) line combined filling, radiofrequency combined filling, and surgery. For the safety of patients, it is important to correctly understand and master the facial anatomical structure and critical areas[16-20]. By combining laser, radiofrequency, injection, and plastic surgery to enhance the shape of the nasolabial groove from an anatomical perspective, NLF depression can be improved, and the long-term therapeutic effect can be maintained. In recent years, the emergence of various new materials has provided new ideas and tools for the treatment of NLF depression. Plastic surgeons must treat NLF depression innovatively on the premise of ensuring patient safety[21-25].
BTX-A is a bacterial exotoxin secreted by anaerobic Clostridium species. According to immunoantigenicity, BTX-A can be divided into eight subtypes: A, B, C1, C2, D, E, F, and G. Except for C2, all of the subtypes are neurotoxins. Among them, type A is the most common subtype, with strong toxicity and stability, and it was the first subtype purified and applied in clinical settings[26]. BTX-A mainly acts on the presynaptic membrane at the nerve–muscle junction, rupturing the membrane contact/transmembrane proteins of the presynaptic membrane-associated proteins and fusion proteins on the membrane of acetylcholine vesicles in the nerve endings, and inhibiting the release of neurotransmitter acetylcholine from the nerve endings. This blocks the transmission of nerve impulses to the muscle, preventing the muscle from receiving neurotransmitters to produce excitatory contractions, resulting in abnormal muscle contractions[27-30]. BTX-A increases the density of blood vessels and mature adipocytes, improves the histologic characteristics of fat grafts, and enhances the retention of fat grafts transplanted into muscles[31]. The current study results showed that the WSRS and GAIS scores 1, 3, and 6 months after the operation were lower, the facial fine lines and pores were remarkably improved, the skin index score was higher, and the compactness of facial contours was better in the observation group. BTX-A injection is widely used in wrinkle removal, masseter hypertrophy, leg muscular hypertrophy, armpit odor, scar, skin quality improvement, and other plastic and cosmetic procedures, achieving good results, and its safety and effectiveness have been fully validated[32]. Furthermore, the proportion of patients receiving nonoperative medical cosmetic treatment is increasing annually. BTX-A injection plays an important role in nonoperative cosmetic surgery. The wide application of BTX-A has completely changed the traditional cosmetic methods of medical plastic surgery, and injection microsurgery has become one of the most popular cosmetic methods[33-35]. BTX-A treatment of NLF depression particularly acts on the block of the oral angle muscles and can improve the dynamic factors of NLF depression, which cannot be cured by alone. In this study, the observation group was treated with AFG + BTX-A, which act on both dynamic and nondynamic factors to improve NLF depression.
However, BTX-A treatment of NLF depression is associated with a certain risk, and the main complications include asymmetry of bilateral nasolabial sulci and lengthening or prolapse of the upper lip, especially when smiling. Owing to anatomical factors such as the presence of more muscles around the mouth, unclear boundaries, and other anatomical factors, local drug concentrations in the nasolabial groove injection site and injection levels may vary. Therefore, to avoid the corresponding complications caused by uneven diffusion and different concentrations of BTX-A, this study followed the principles of fewer but better, shallower but not deeper lines, with fewer adverse reactions. The results showed no remarkable difference in the incidence of postoperative adverse reactions such as facial stiffness, facial asymmetry, facial bruise, and facial concavity inequality between the two groups.
As a natural soft tissue filler, autologous fat particles have been widely used in plastic and cosmetic surgery and are accepted by most patients because of their natural advantages. However, the fat absorption rate after AFG is relatively high. Therefore, reducing postoperative absorption and improving the survival rate of fat cells remain challenging. Currently, many factors are considered to affect the survival of fat cells postoperatively, but the mechanism remains unclear. The problem of postoperative absorption rate has always been the research focus in fat particle transplantation. In recent years, the survival rate of fat cells has been greatly improved through the enhancement of surgical methods and application of various auxiliary technologies. The thigh should be preferred as the fat donor area, which is rich in lipoprotein lipase. The fat particles obtained via suction in this area are easier to purify and less fibrous, which do not easily block the needle[36,37]. Because the amount of fat needed to correct NLF depressions is small, a low negative-pressure syringe can be used to suction the fat, thereby preventing damage to deep blood vessels and nerves. In general, the suction volume is approximately three times the estimated volume, which ensures that the amount of fat particles obtained after purification can meet the filling needs.
In addition, autologous fat injections are generally performed using a retrograde injection method, with continuous linear injections administered upward along the NLF. This method involves multiple flat superimposed layers, which include the subcutaneous, fascial, and periosteal surfaces. In general, injection concentrations should exceed 20%-30%, resulting in a slight elevation of the NLF. The NLF area, as part of facial movements, has a high fat resorption rate; therefore, a second autologous fat injection should be performed 3-6 months postoperatively. When botulinum toxin acts on the muscle tissue, it can effectively inhibit muscle contraction and relax the muscles. This effect is widely used in the field of medical beauty, such as facial wrinkle removal and facelifting. Moreover, the effect of botulinum toxin can affect fat cells. Studies have revealed that botulinum toxin can improve the survival rate of fat cells after inhibiting muscle activity. This is because muscle activity will exert a certain pressure on fat cells, and inhibiting muscle activity can alleviate this pressure, which is conducive to the survival of fat cells.
The survival rate of fat cells after AFG is the main focus of this experiment. Blood supply is the key factor affecting the survival of fat cells after transplantation, and the reformation of local blood supply directly affects the postoperative effect. Adipose stem cells can be purified to assist adipose transplantation via two approaches: (1) Adipose stem cells can differentiate into various tissues; and (2) Adipose stem cells can secrete various cytokines, including vascular endothelial growth factor and basic fibroblast growth factor, and this secretion is conducive to wound recovery and microcirculation establishment. The progress in this field is also reflected in new injection fillers prepared from adipose tissue for enriching and concentrating adipose-derived stem cells (ADSCs). In 2013, Tonnard developed a new filtrate via mechanical emulsification and nylon gauze filtration and named it nanofat, which contained broken fat cells and ADSCs. Nanofat is more suitable for the elimination of shallow lines; however, the support effect after filling was poor. Some scholars used simple and rapid mechanical methods to destroy and isolate most mature adipocytes in the adipose tissue and obtained a colloidal product with an original volume of only 15%; however, the degree of stromal vascular fraction (SVF) was enriched by > 4.5 times and the ADSC content was enriched by 6.3 times[38]. As mature adipocytes in the SVF gel are removed, there is a large space for inflammatory cells to enter the transplantation site to engulf wastes and facilitate the entry of blood vessels. Simultaneously, the adipose tissue is almost completely regenerated, with characteristics closer to those of the normal tissue, a longer-term volume retention rate, and a more stable therapeutic effect[39,40]. Therefore, SVF gels have a good application prospect in facial and neck rejuvenation, including NLF depression filling.
Taken together, AFG filling has the following advantages: Wide source of raw materials, absence of tissue rejection, lack of differences between the filling site and surrounding normal tissues, and good repeatability.
| 1. | Stefura T, Kacprzyk A, Droś J, Krzysztofik M, Skomarovska O, Fijałkowska M, Koziej M. Tissue Fillers for the Nasolabial Fold Area: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Aesthetic Plast Surg. 2021;45:2300-2316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 2. | Kwon HJ, O J, Cho TH, Choi YJ, Yang HM. The Nasolabial Fold: A Micro-Computed Tomography Study. Plast Reconstr Surg. 2020;145:71-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Dayal A, Bhatia A, Hsu JT. Fat grafting in aesthetics. Clin Dermatol. 2022;40:35-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 4. | Dusseldorp JR, Faraway J, Razavi L, Hadlock TA, Trotman CA. Nasolabial fold dynamics: Implications for facial paralysis and facial reanimation surgery. Orthod Craniofac Res. 2021;24:62-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Tanaka OM, Cavassin LD, Gasparello GG, Meira TM, Miyoshi CS, Hartmann GC. The Esthetics of the Nasolabial Fold and Age in the Elderly Via Eye-Tracking. Contemp Clin Dent. 2023;14:18-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Delay E. Commentary on: Autologous Fat Transplantation for Aesthetic Breast Augmentation: A Systematic Review and Meta-Analysis. Aesthet Surg J. 2021;41:NP430-NP432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Magnusson MR. Commentary on: Three-Dimensional Description of the Angular Artery in the Nasolabial Fold. Aesthet Surg J. 2021;41:705-706. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | El-Mesidy MS, Alaklouk WT, Azzam OA. Nasolabial fold correction through cheek volume loss restoration versus thread lifting: a comparative study. Arch Dermatol Res. 2020;312:473-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Ueberreiter CS, Ueberreiter K, Mohrmann C, Herm J, Herold C. [Long-term evaluation after autologous fat transplantation for breast augmentation]. Handchir Mikrochir Plast Chir. 2021;53:149-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Day DJ, Littler CM, Swift RW, Gottlieb S. The wrinkle severity rating scale: a validation study. Am J Clin Dermatol. 2004;5:49-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 175] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 11. | Qiao J, Li F, Jin HZ, Yang XM, Fang H, Li L, Zhang W, Wu XF, Zheng M, Jia QN. The efficacy and safety of Dermalax(TM) DEEP in the correction of moderate to severe nasolabial folds: a multicenter, randomized, double-blind clinical study. J Dermatolog Treat. 2021;32:548-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Pruettijarai U, Meephansan J, Prapapan O, Pureesrisak P, Sirithanabadeekul P, Tantisantisom K, Thongma S, Rayanasukha Y, Adulyaritthikul P, Khanchaitit P. Efficacy of a novel microneedle patch for rejuvenation of the nasolabial fold. Skin Res Technol. 2022;28:786-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Gelezhe P, Gombolevskiy V, Morozov S, Melnikov DV, Korb TA, Aleshina OO, Frank K, Gotkin RH, Green JB, Cotofana S. Three-Dimensional Description of the Angular Artery in the Nasolabial Fold. Aesthet Surg J. 2021;41:697-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Kim MJ, Oh TS. A nasolabial fold reset technique for enhancing midface lifts in facial reanimation: Three-dimensional volumetric analysis. J Craniomaxillofac Surg. 2020;48:162-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Peng T, Hong WJ, Fang JR, Luo SK. The selection of hyaluronic acid when treating with the nasolabial fold: A meta-analysis. J Cosmet Dermatol. 2022;21:571-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 16. | Turin SY, Gosain AK. New Insights into the Three-Dimensional Anatomy of the Facial Mimetic Muscles Related to the Nasolabial Fold: An Iodine Staining Technique Based on Nano-computed Tomography (Discussion). Aesthetic Plast Surg. 2020;44:87-88. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Deptula P, Fox P. Autologous Fat Grafting in Hand Surgery. J Hand Surg Am. 2021;46:594-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Lee W, Kim JS, Moon HJ, Yang EJ. A Safe Doppler Ultrasound-Guided Method for Nasolabial Fold Correction With Hyaluronic Acid Filler. Aesthet Surg J. 2021;41:NP486-NP492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Al Soueidy A, Yoon MK. Re: "Paradoxical Prominence of Nasolabial Fold as a Sign of Aberrant Facial Nerve Regeneration:. Ophthalmic Plast Reconstr Surg. 2020;36:315-316. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Tarantino IS, Whitsitt J, Pflederer RT, Aires DJ. Retraction of the cheek to enhance visualization of the nasolabial fold region. J Am Acad Dermatol. 2023;88:e293-e294. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Solish N, Carruthers J, Kaufman J, Rubio RG, Gross TM, Gallagher CJ. Overview of DaxibotulinumtoxinA for Injection: A Novel Formulation of Botulinum Toxin Type A. Drugs. 2021;81:2091-2101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 22. | Borba A, Matayoshi S, Rodrigues M. Avoiding Complications on the Upper Face Treatment With Botulinum Toxin: A Practical Guide. Aesthetic Plast Surg. 2022;46:385-394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 23. | Shim YJ, Lee HJ, Park KJ, Kim HT, Hong IH, Kim ST. Botulinum Toxin Therapy for Managing Sleep Bruxism: A Randomized and Placebo-Controlled Trial. Toxins (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | Wollmer MA, Magid M, Kruger THC, Finzi E. Treatment of Depression with Botulinum Toxin. Toxins (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 25. | Moreau C, Kervarrec T. sQuiz your knowledge! Slow-growing papule on the nasolabial fold of a 61-year-old man. Eur J Dermatol. 2021;31:681-682. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Nestor MS, Han H, Gade A, Fischer D, Saban Y, Polselli R. Botulinum toxin-induced blepharoptosis: Anatomy, etiology, prevention, and therapeutic options. J Cosmet Dermatol. 2021;20:3133-3146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 27. | Dressler D, Adib Saberi F, Rosales RL. Botulinum toxin therapy of dystonia. J Neural Transm (Vienna). 2021;128:531-537. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 28. | Kassir M, Gupta M, Galadari H, Kroumpouzos G, Katsambas A, Lotti T, Vojvodic A, Grabbe S, Juchems E, Goldust M. Complications of botulinum toxin and fillers: A narrative review. J Cosmet Dermatol. 2020;19:570-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 29. | Hanna E, Xing L, Taylor JH, Bertucci V. Role of botulinum toxin A in improving facial erythema and skin quality. Arch Dermatol Res. 2022;314:729-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 30. | Tavares H, Oliveira M, Costa R, Amorim H. Botulinum Toxin Type A Injection in the Treatment of Postparetic Facial Synkinesis: An Integrative Review. Am J Phys Med Rehabil. 2022;101:284-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 31. | Alam MS. Paradoxical Prominence of Nasolabial Fold as a Sign of Aberrant Facial Nerve Regeneration: The Alam's Sign. Ophthalmic Plast Reconstr Surg. 2019;35:408-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | de Sanctis Pecora C, Shitara D. Botulinum Toxin Type A to Improve Facial Symmetry in Facial Palsy: A Practical Guideline and Clinical Experience. Toxins (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 33. | Cervantes JA, Deen S, Shimizu I. Combination repair of nasal ala and nasolabial fold defects following Mohs micrographic surgery. Int J Dermatol. 2023;62:106-107. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 34. | Abramo AC, Scartozzoni M, Sgarbi R. Histological and Quantitative Appraisal of the Intradermal and Subcutaneous Distribution of the Hyaluronic Acid Injected into the Nasolabial Fold. Aesthetic Plast Surg. 2021;45:710-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Kane MAC. Invited Discussion on: A Single Center, Randomized, Double-blind Clinical Trial to Compare the Efficacy and Safety of a New Monophasic Hyaluronic Acid Filler and Biphasic Filler in Correcting Nasolabial Fold. Aesthetic Plast Surg. 2021;45:2909-2911. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 36. | Dadkhahfar S, Robati RM, Gheisari M, Moravvej H. Subcision: Indications, adverse reactions, and pearls. J Cosmet Dermatol. 2020;19:1029-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 37. | Abramo AC, Sgarbi R, Kim CY, Bastos PA. Effectiveness and Long-Acting of the Hyaluronic Acid Injected into the Nasolabial Fold Measured Through Magnetic Resonance Imaging. Aesthetic Plast Surg. 2021;45:1221-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 38. | Moers-Carpi M, Christen MO, Delmar H, Brun P, Bodokh I, Kestemont P. European Multicenter Prospective Study Evaluating Long-Term Safety and Efficacy of the Polycaprolactone-Based Dermal Filler in Nasolabial Fold Correction. Dermatol Surg. 2021;47:960-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Mesa-Álvarez L, Peón Currás G, Flórez Á. Widespread Erythematous and Bullous Plaques Associated With Nasolabial Fold Ulceration: Answer. Am J Dermatopathol. 2019;41:237-238. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 40. | Solomon P, Ng CL, Kerzner J, Rival R. Facial Soft Tissue Augmentation With Bellafill: A Review of 4 Years of Clinical Experience in 212 Patients. Plast Surg (Oakv). 2021;29:98-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |