Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.4956
Revised: May 22, 2024
Accepted: June 5, 2024
Published online: August 6, 2024
Processing time: 91 Days and 18.8 Hours
In patients with liver failure (LF), the high rate of secondary infections, which are associated with poor prognosis, highlights the clinical significance of understanding the underlying risk factors and implementing targeted intervention programs.
To investigate risk factors for secondary infections in patients with LF and evaluate the effectiveness of comprehensive nursing interventions.
This retrospective study included 64 patients with LF, including 32 with and 32 without secondary infections. A questionnaire was used to collect data on age; laboratory parameters, including total and direct bilirubin, prothrombin time, blood ammonia, and other biochemical parameters; invasive procedures; and complications. Patients with secondary infections received comprehensive nursing intervention in addition to routine nursing care, whereas those without secondary infections received only routine nursing care to compare the effect of nursing intervention on outcomes.
The infection rate, which was not associated with age or complications, was significantly associated with biochemical parameters and invasive procedures (P < 0.05). The infection rate was 61.6% in patients who had undergone invasive procedures and 32.1% in those who had not undergone invasive procedures during the hospital stay. The infection rate was also significantly associated with the type of LF (P < 0.05), with the lowest rate observed in patients with acute LF and the highest rate observed in those with subacute LF. The nursing satisfaction rate was 58.3% in the uninfected group and 91.7% in the infected group, indicating significantly higher satisfaction in the infected group (P < 0.05).
In patients with LF, the rate of secondary infections was high and associated with biochemical parameters and type of LF. Comprehensive nursing intervention can improve patient satisfaction.
Core Tip: This study focused on approaches for early and effective prevention of infections, improvement of outcomes in patients with liver failure, and comprehensive disease assessment to improve understanding of the disease. Our findings revealed that comprehensive nursing intervention improves the curative effect and patient satisfaction.
- Citation: Zhang WW, Chen L, Wu YF. Risk factors for secondary infection after liver failure and effect of comprehensive nursing intervention. World J Clin Cases 2024; 12(22): 4956-4964
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/4956.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.4956
Infections secondary to liver failure (LF) usually exacerbate the clinical condition of patients with LF and are associated with a poor prognosis. Patients with LF have severe hepatocellular damage, reduced neutrophil and macrophage function, impaired immune response, and reduced hepatic complement, which greatly increase susceptibility to bacterial and other microbial infections[1]. Previous national and international studies have shown that ~79% of patients with LF have concurrent bacterial and fungal infections. In these patients, intestinal bacteria are the primary pathogens associated with secondary infections, and common sites of infection include lungs and abdominal cavity, followed by the biliary tract and intestines. Bacteremia may occur, with studies reporting Gram-positive bacteria as the most common cause, accounting for ~72% of all confirmed blood-borne infections in patients with LF[2,3]. Intriguingly, Gram-negative bacteremia has been reported as the most common etiology of secondary infections in recent years. Some patients with LF may develop concurrent infections at multiple sites or multiple infections with different pathogens, significantly increasing the mortality rate. Studies have shown that the mortality rate can reach 73.5% within 2 wk after a secondary infection in patients with LF. The mortality rate also depends on the site of infection, i.e., the mortality rate is as high as 80% in patients with usual pulmonary infections and ~65.3% in those with abdominal infections. The high mortality rate due to secondary infections hinders the clinical diagnosis and treatment of patients with LF[4]. Therefore, in patients with LF, understanding the characteristics and risk factors for secondary infections is important for the implementation of targeted preventive measures and treatment approaches.
In China, hepatitis virus infection, especially that due to hepatitis B virus (HBV), is the main cause of LF, followed by drugs, and hepatotoxic substances, such as alcohol and chemicals. Acute or chronic LF is the most common type of LF due to chronic HBV infection in China[5]. In chronic liver disease, extensive hepatocyte injury and necrosis as well as the failure of regeneration lead to the loss of hepatocyte function. Altered immune response significantly increases susceptibility to spontaneous bacterial, nosocomial and other unexplained infections. In patients with secondary infections, the levels of proinflammatory cytokines are increased, hemodynamics are altered, and LF continues to worsen, increasing the risk for septic shock, multiorgan failure, other complications and death[6]. In patients with LF, common types of secondary infections include spontaneous bacterial peritonitis and pulmonary infection bacteremia, whereas meningitis and bacterial endocarditis are less common. The site of infection, pathogenesis and clinical features also differ depending on the etiology of LF. Infection is a significant concern that interferes with the prognosis of patients with LF. Patients with LF and infections are at higher risk of acute kidney injury and septic shock, which may lead to serious complications, such as gastrointestinal bleeding and aggravated LF, causing further adverse consequences[7]. Previous studies have shown that patients with LF tend to develop multipathogen infections and suffer from higher mortality rates[8,9]. Studies evaluating potential risk factors for complications and mortality in patients with LF report that the rate of coinfections is 69.7%. Among patients with LF, the mortality rate was 62.1% in those with infections and 30.4% in those without infections. In addition, the reported rate of improvement was 27.5% in patients with secondary infections and 54.2% in those without secondary infections, indicating poor prognosis in patients with secondary infections. Therefore, accumulating evidence highlights the importance of early diagnosis and effective treatment approaches in improving prognosis in these patients[10]. Domestic epidemiological survey reports also revealed that secondary infections are a major factor impacting prognosis in patients with LF[11]. Thus, addressing the causes of disease has clinical importance. In patients with LF, immunological alterations and overactivation of proinflammatory cytokines can lead to the translocation of intestinal bacteria from the intestinal lumen to mesenteric lymph nodes and portal vein. Bacterial translocation has a significant impact on damage in LF and its consequences. In patients with LF, prophylactic antibiotic use, which usually indicates disease severity at admission, remains controversial[12]. Studies indicate that prophylactic antibiotic use may not reduce the rate of secondary infections or mortality in patients with LF. In healthy individuals, the intestinal flora and the external environment in the body are in a dynamic balance, whereas the translocation risk of intestinal flora is higher in patients with LF[13]. Prophylactic antibiotic administration disrupts the normal balance, significantly increasing the risk of endogenous infections. Liver parenchyma and metabolic function are impaired in patients with LF, and infection is a major cause of multiorgan failure during LF[14].
Approaches to prevent infections as early as possible and improve prognosis are primary focuses in the treatment of patients with LF, who suffer from higher rates of secondary infections with poor prognosis and potential harm. The high morbidity and mortality rates of patients with LF have led to numerous lines of investigation, improving our understanding of the disease and revealing that early detection, active prevention and timely standardized treatments are critical to reduce mortality in patients with LF and secondary infections. LF is complicated with complex clinical symptoms and high mortality, severely impacting the quality of life of patients. Therefore, effective treatment approaches and nursing care based on scientific evidence are critical. The present study aimed to evaluate risk factors for secondary infections in patients with LF and determine the impact of comprehensive nursing intervention.
This was a retrospective study. The study included 64 patients with LF, including those with and without secondary infections, who were admitted to The First Affiliated Hospital of Soochow University Hospital between January 2019 and December 2021. Patients with secondary infections (infected group) received comprehensive nursing intervention in addition to routine nursing care, whereas those without secondary infections (uninfected group) received routine nursing care.
The inclusion criteria were as follows: (1) Fulfillment of the diagnostic criteria for LF as outlined in the 2018 version of the Guidelines for Diagnosis and Treatment of LF; and (2) diagnosis of infection based on the clinical assessment of symptoms, physical examination, and laboratory tests for those with secondary infections. The exclusion criteria were as follows: (1) Diagnosis of chronic LF; (2) history of liver transplantation; (3) diagnosis of primary liver cancer or other malignant tumors; (4) history of other severe organic diseases; and (5) comorbid diseases which can cause immune system dysfunction.
During overall medication intervention, the nursing staff asked the patients regarding contraindications before administering medication and observed physiological indicators in real time throughout treatment. In addition, the nursing staff provided information regarding treatments, including contraindications, dosage and time. If the patient’s condition worsened during treatment, the physician was notified without delay.
Regarding dietary intervention, the nursing staff provided a diet appropriate for the clinical situation of the patients, instructing them to primarily consume foods that were easily digestible, high in protein content, and contained multivitamins; the patients were also instructed to consume more frequent meals with smaller amounts of food. The nursing staff also encouraged the patients to eat more fresh vegetables and fruits. Spicy food, tobacco, and alcohol were strictly prohibited.
The nursing staff provided psychological intervention to understand the life and family situation of the patients; conducted counseling according to their psychological changes; patiently responded to patients' questions; used an understandable manner to inform the disease theory, such as small lectures, multimedia and so on; popularized relevant cases with successful treatment outcomes; Set up a weChat group to promote communication and encouragement between patients. To improve patients' enthusiasm and compliance with treatment by showing successful treatment cases. Improved the patients’ confidence in cooperating with medical treatment; and eliminated negative emotions.
In terms of exercise intervention, the nursing staff prepared scientific and reasonable exercise plans for patients according to the actual situation; ensured proper sleep; expressed no feeling of painstaking during treatment; formulated appropriate exercise plans, primarily aerobic exercises such as tai chi and walking; and maintained a reasonable schedule.
Patient age was retrospectively determined using a questionnaire. The laboratory parameters used in the present study included several biochemical parameters on liver function, such as total bilirubin (TBIL), direct bilirubin (DBIL), prothrombin time (PT), and blood ammonia (NH3). To assess conditions associated with infections, data were collected on the details of invasive procedures and complications until hospital discharge or in-hospital death. Nursing satisfaction and complication rates were determined, and questionnaires were used to evaluate nursing satisfaction using the following scoring system: 100, full satisfaction; > 80, high satisfaction; 60–80, satisfaction; and < 60, dissatisfaction.
All statistical analyses were performed using SPSS version 21. Numerical data were presented as frequencies or percentages (%), and measurement data were expressed as mean ± SD. Student’s t and Wilcoxon rank-sum tests were used to compare general data, and a logistic regression model was used to evaluate potential risk factors for secondary infections. P < 0.05 was considered statistically significant.
In total, 64 patients, including 32 males and 32 females, were included in the present study. These patients were aged 18–85 years (49.23 ± 7.11 years), and their average hospital stay was 13.15 ± 9.14 d. No significant difference was observed between the infected and uninfected groups in terms of basic information, such as physical condition, sex and age. In terms of the disease type, 22 patients suffered acute LF, 10 subacute LF, and 32 chronic and subacute LF.
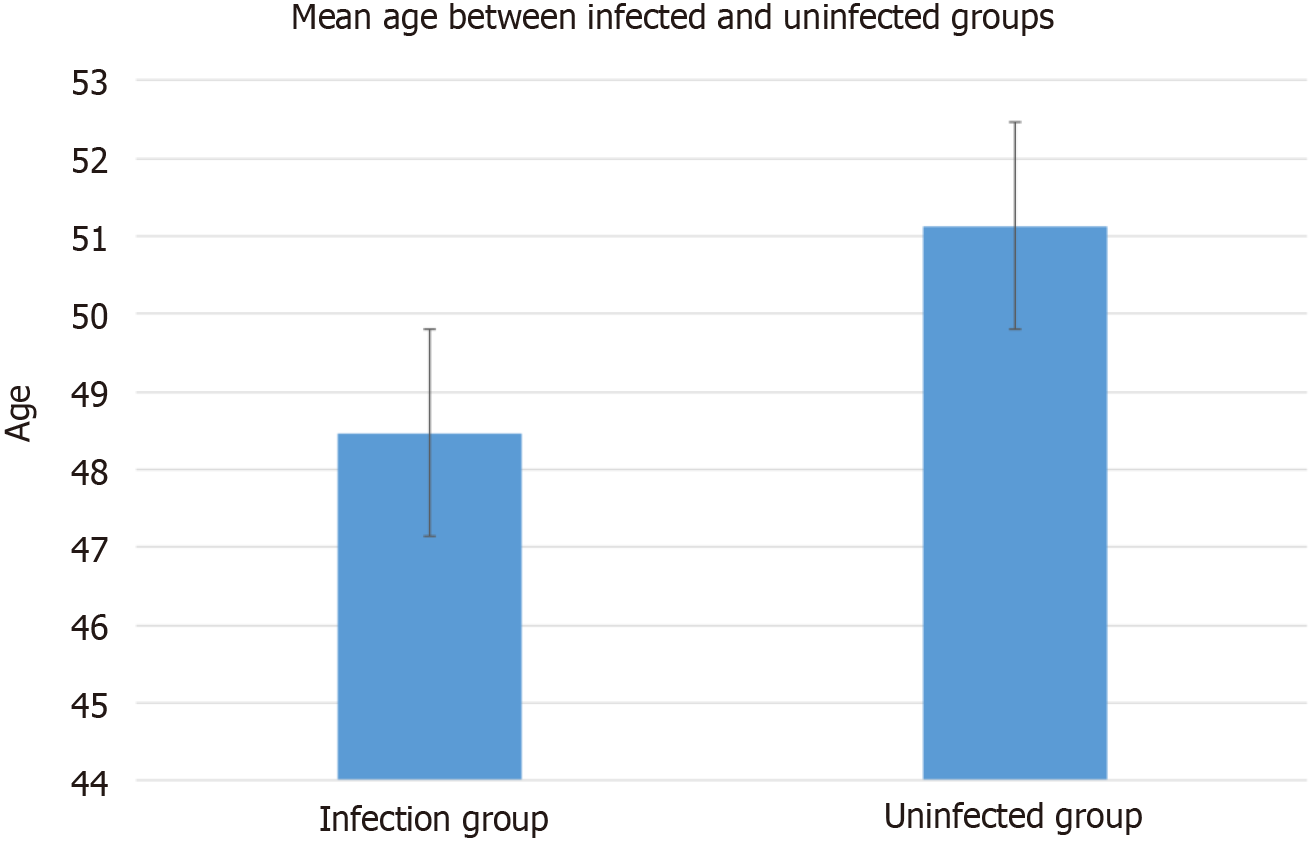
The mean age of the infected group was 48.47 ± 17.17 years, and that of the uninfected group was 51.13 ± 16.88 years. No significant difference in the average age of the patients was observed between the infected and uninfected groups (P > 0.05) (Figure 1).
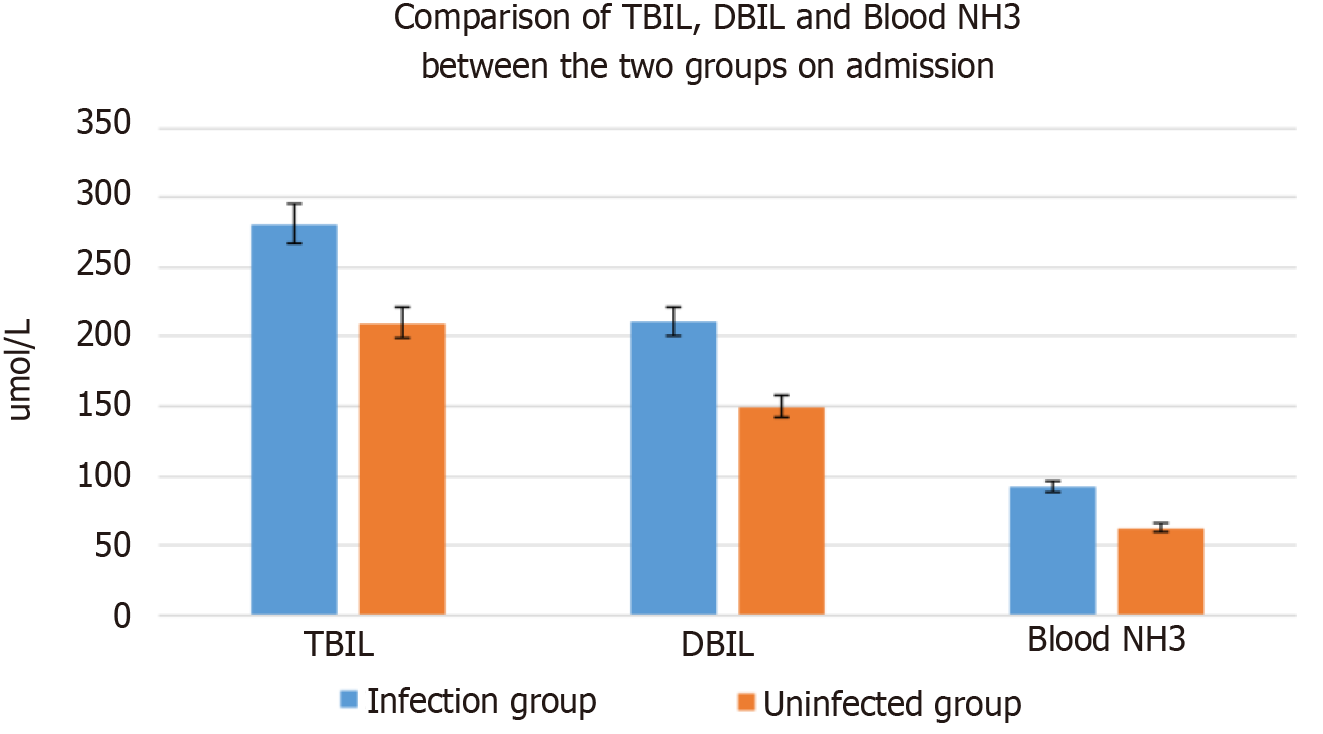
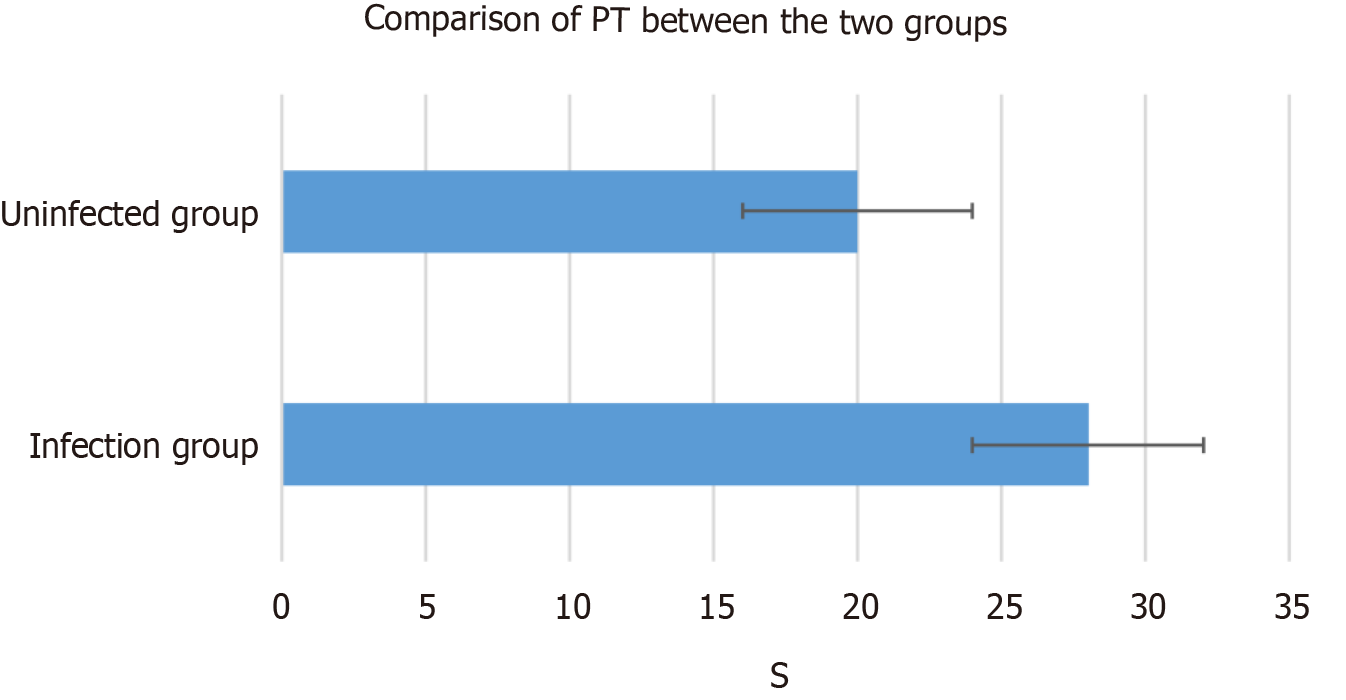
TBIL was 281.23 mol/L for the infected group and 210.04 mol/L for the uninfected group. DBIL was 210.62 mol/L for the infected group and 150.16 mol/L for the uninfected group. PT was 28 s for the infected group and 20 s for the uninfected group. Blood NH3 was 92.4 mol/L for the infected group and 63.12 mol/L for the uninfected group. TBIL, DBIL, PT and blood NH3, and other biochemical indexes of the infected and uninfected groups at admission were statistically analyzed, and statistical differences between the two groups (P < 0.05) are shown in Figures 2 and 3.
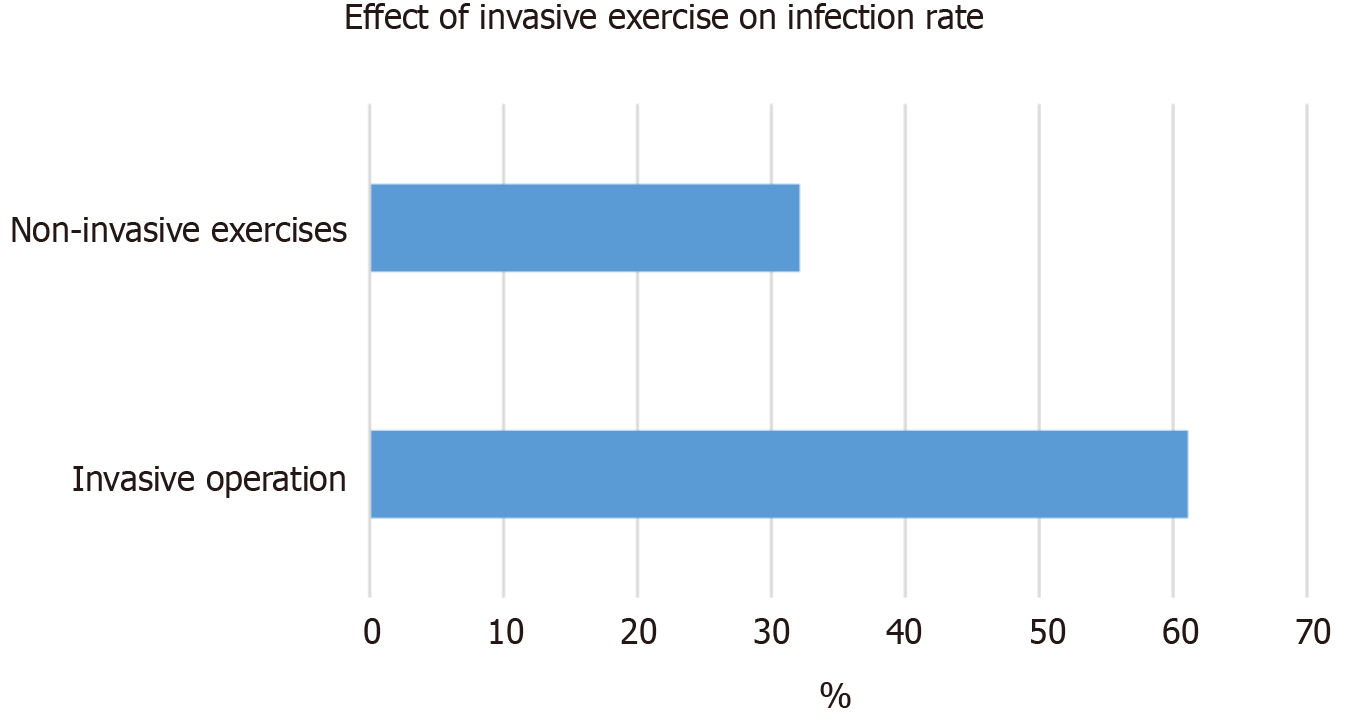
Among the enrolled patients, 36, including 22 with infection and 14 without, underwent invasive operations, and their infection rate was 61.1%. Among 28 patients, including nine with infection and 19 without, who did not undergo invasive operations, the infection rate was 32.1%. Patients undergoing invasive procedures had a higher infection rate, with a statistically significant difference (P < 0.05) (Figure 4).
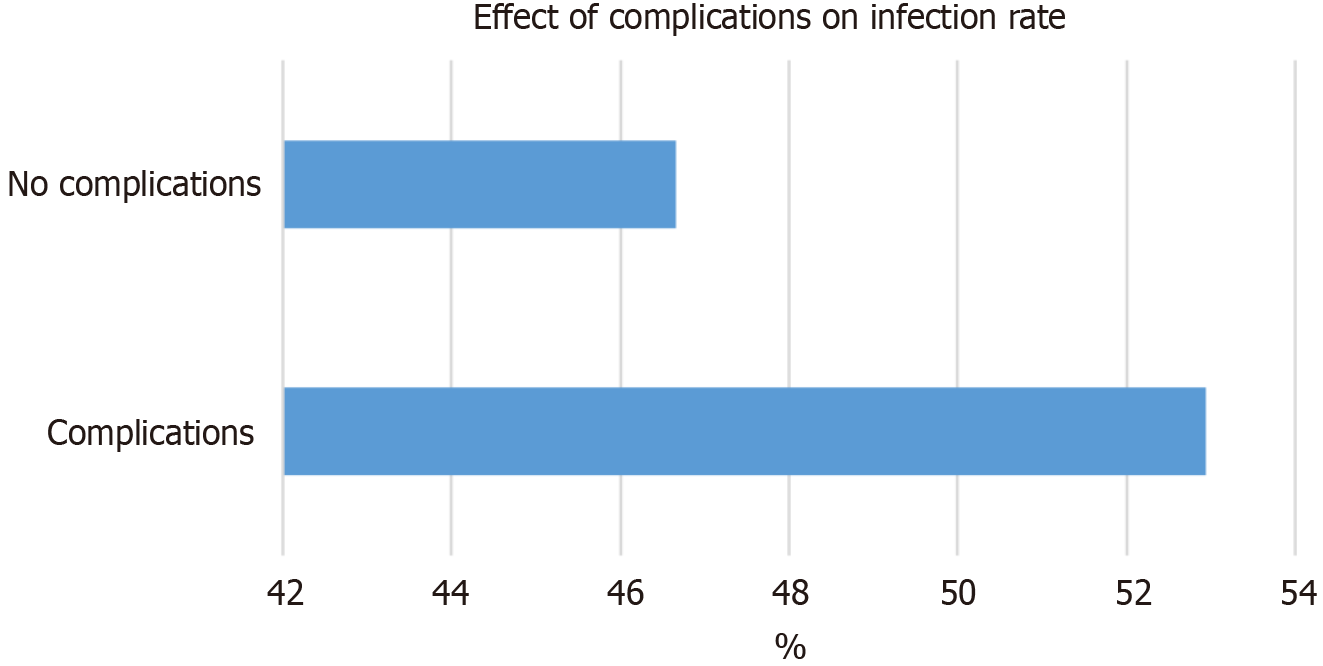
Among the 64 patients enrolled, 35 had complications of LF and 29 had none. There were 18 patients (52.94%) with complications in the infected group, 16 (47.06%) with complications in the uninfected group, 14 (46.66%) without complications in the infected group, and 16 (53.34%) without complications in the uninfected group. Figure 5 shows great difference in complications in different groups (P < 0.05).
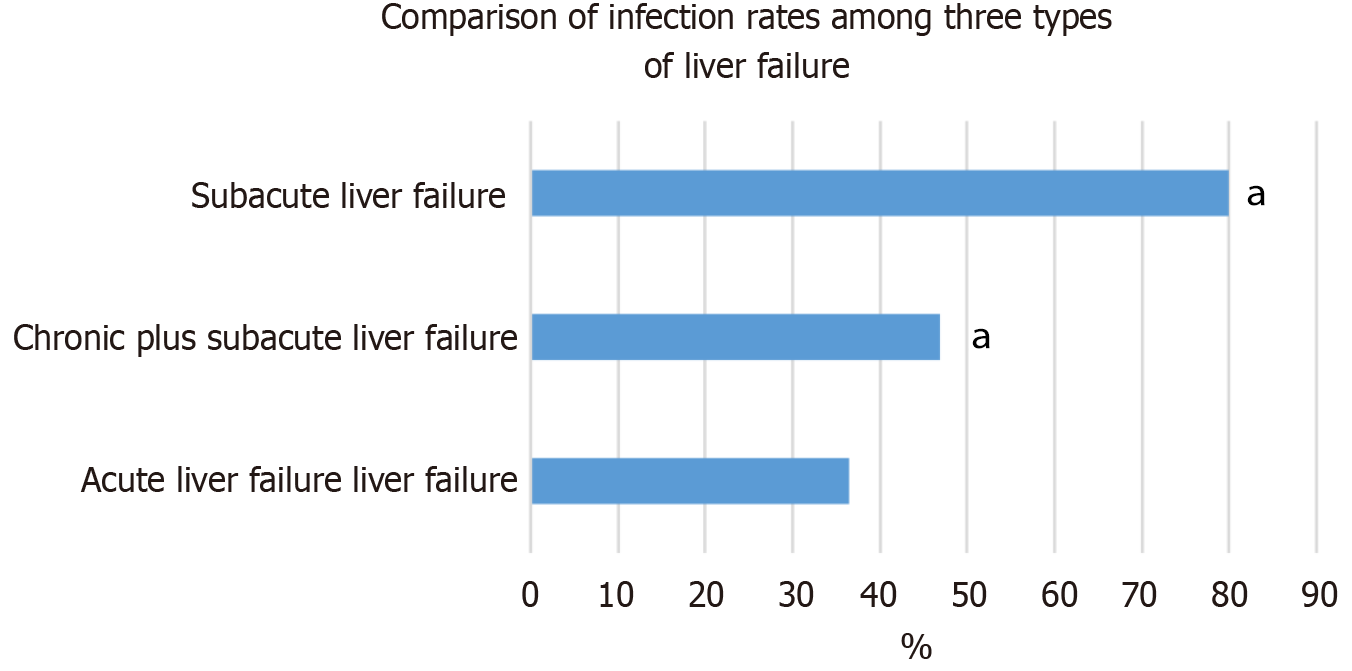
Among all 22 patients with acute LF, eight were infected and 14 were not, with a total infection rate of 36.4%. Among the 32 patients with chronic and subacute LF, 15 were infected and 19 were not, with a total infection rate of 46.9%. Among the 10 patients with subacute LF, eight were infected and two were not, with a total infection rate of 80%. A significant difference in the total infection rate was observed among patients with three types of LF (χ2 = 5.980, P = 0.041); patients with acute LF had the lowest total infection rate, and those with subacute LF showed the highest total infection rate (Figure 6).
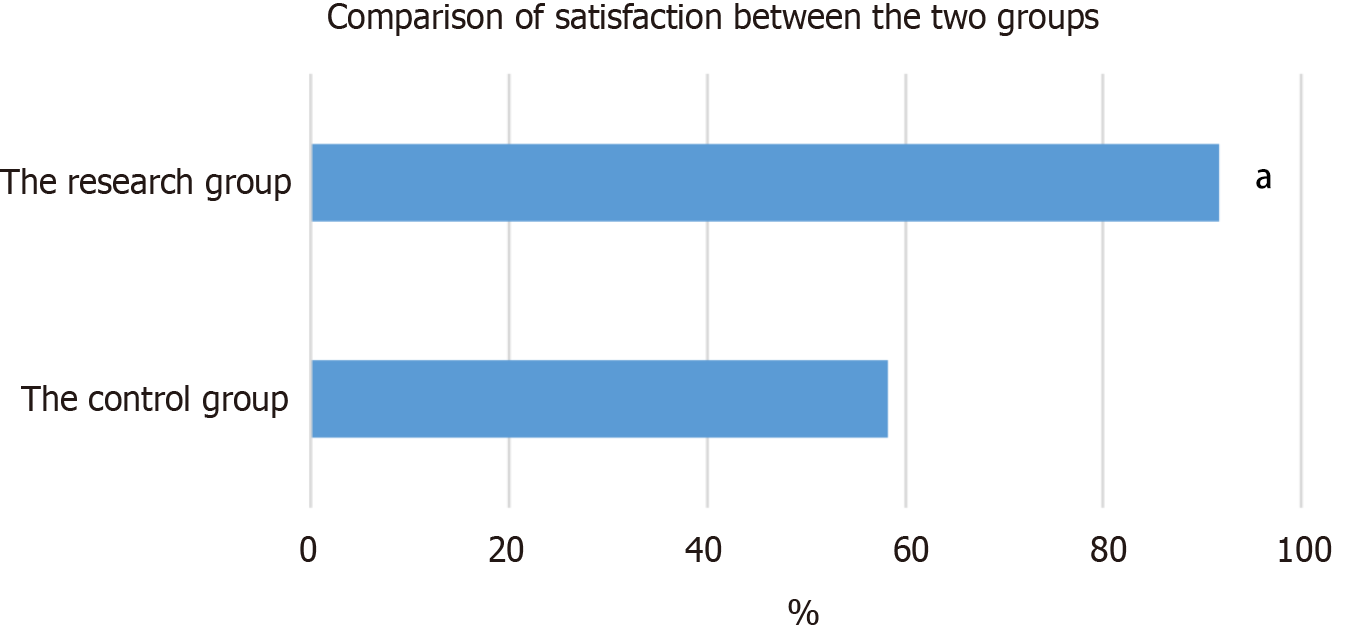
Among the 12 patients in the uninfected group, five were dissatisfied, three were satisfied, and four were very satisfied; therefore, in total, seven patients (58.3%) were satisfied. Among the 12 patients in the infected group, one was dissatisfied, three were satisfied, and eight were very satisfied; therefore, in total, 11 patients (91.7%) were satisfied. The nursing satisfaction of the infected group was higher than that of the uninfected group (P < 0.05) (Figure 7).
Infection is the most common complication of LF. Impaired immune function in patients with LF markedly increases susceptibility to secondary bacterial infections. The most common infections are spontaneous bacterial peritonitis, urinary tract infection, and bacteremia, whereas meningitis and others are less common. Infections may arise at different sites, with different pathogenic mechanisms and clinical characteristics. Elevated levels of proinflammatory cytokines, disrupted hemodynamics and worsening LF lead to complications such as septic shock, sequential organ failure and death[15]. One study reported that 69.7% of patients with LF had infections as a complication[16]. In the present study, the rate of infection in patients with LF was 50%, slightly lower than that reported previously, which might be due to the short cutoff time. A previous study reported hepatic encephalopathy as a crucial cause of intervention in patients with acute LF[17]. Infection, granulocyte ratio and coagulation function can be used to predict mortality, and secondary infection was an independent predictor of 30-day mortality and led to sepsis in 31% of patients with LF[18]. Identification of risk factors can aid in reducing mortality and improving prognosis in these patients[19]. HBV is a key cause of LF[20]. In the present study, the cause of LF was HBV infection in 50% of the patients. No study to date has evaluated whether the rate of infection is associated with the etiology of LF. There is no clear association between the rate of infection and the etiology of LF, which should be investigated in future studies[21]. In addition, the number of complications has been reported to be associated with higher coinfection risk[22], which is likely related to their impact on shared pathways and the relationship among various complications that eventually leads to multiorgan failure, LF and infection. It is also related to invasive procedures, such as indwelling catheter placement and abdominal puncture. Strict adherence to aseptic technique during such procedures is strongly associated with infection, consistent with the present study[23].
In the present study, the infection rate differed among the patients with different types of LF, in agreement with previous studies[24], indicating that the infection rate was significantly higher in patients with hospitalization duration > 30 d than in those with a < 30 d hospitalization. Studies suggest that patients with LF should be treated clinically to improve treatment efficacy and that the length of hospital stay should be controlled to prevent cross-infection[25]. The average length of hospital stay in the current study was < 30 d, and the association between the length of hospital stay and the infection rate was not analyzed.
In patients with LF and no infection, prophylactic antibiotic use, which remains a focus of clinical interest, is controversial. In the early stages, researchers believe that antibiotic prophylaxis should be immediately initiated to prevent infection and LF exacerbation. Previous studies have demonstrated that prophylactic antibiotic use can reduce infection rate in patients with LF, although it does not significantly improve survival rate[26]. There is no research on the use of prophylactic antibiotics currently. Some studies have suggested that prophylactic or nonstandard antibiotic treatment causes an imbalance in the composition of the gut flora, thereby leading to immune dysfunction and secondary infections[27,28]. This is an important factor in secondary infection and superinfection. In one study, the incidence of new infections did not significantly differ between patients with LF who received prophylactic antibiotic treatment and those who received nonprophylactic antibiotic treatment. Therefore, in patients with LF, routine prophylactic antibiotic treatment after admission is not recommended; however, prophylactic antibiotics may have some clinical significance in patients with subacute LF who are undergoing invasive surgery[29]. Given that infection significantly impacts the prognosis of patients with LF, careful surveillance for infection and prompt initiation of antimicrobial therapy are crucial[30]. Comprehensive hospital assessment should be implemented in patients with LF. For high-risk patients who are prone to infection, antibiotics should be used in a timely manner at the first sign of opportunistic infections in accordance with aseptic procedures, and the selection of targeted antibiotics with low resistance is necessary to improve outcomes after secondary infections and reduce mortality in patients with LF. The clinical symptoms include extreme fatigue, severe coagulation dysfunction and severe gastrointestinal symptoms. Secondary infections are difficult to treat and are associated with a high mortality rate. Therefore, attention should be paid to reasonable treatment and nursing[31,32].
In the present study, the comprehensive nursing intervention model included medication, dietary, psychological and exercise interventions, which can provide patients with more comprehensive and systematic nursing services. A reasonable diet can alleviate drug reactions and enhance immunity, and appropriate exercise can promote physical recovery. The patient’s knowledge on disease-related issues can also be expanded[33,34]. In the present study, the significantly better patient satisfaction rate after nursing observed in the infected group compared with the uninfected group (91.7% vs 58.3%) reflects the effectiveness of the comprehensive nursing intervention used in patients with LF, and it was worthy of widespread application.
The rate of secondary infection, which was high in patients with LF, was not associated with age or comorbidity. However, the rate of infections was associated with biochemical parameters of LF and the type of LF. The rate of secondary infection was lowest in patients with acute LF and highest in those with subacute LF. Our analyses also revealed that invasive procedures were associated with secondary infection in patients with LF. Clinically, comprehensive nursing intervention can improve the satisfaction of patients with LF and secondary infection. The major study limitations included short study period and small sample size. Further comprehensive studies should include multiple centers with large cohorts.
| 1. | Olson JJ, Entezari V, Vallier HA. Risk factors for nonunion after traumatic humeral shaft fractures in adults. JSES Int. 2020;4:734-738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Bin Arif T, Khalid S, Siddiqui MS, Hussain H, Sohail H. Incidence, patterns, risk factors, and histopathological findings of liver injury in coronavirus disease 2019 (COVID-19): a scoping review. Hong Kong Med J. 2021;27:198-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Shumbusho F, Liu AF, Kateera F, Kabahizi J, Nsanzaimana S, Serumondo J, Damascene Makuza J, Grant PM, Musabeyezu E, Muvunyi C, Gupta N. Risk factors for difficult-to-treat hepatitis C virus genotype 4r in Rwanda and implications for elimination in sub-Saharan Africa. J Viral Hepat. 2021;28:682-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Lin SL, Lin MH, Wang XM, Chen XM, Ye HH, Ma HX, Zhang DQ, Wu WJ, Lin JH, Liao ZY, Zheng RD, Gao HB. [Energy metabolism characteristic with risk of secondary bacterial infection in patients with hepatitis B virus-related chronic liver disease]. Zhonghua Gan Zang Bing Za Zhi. 2021;29:558-564. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Quinonez SC, Thoene JG. Dihydrolipoamide Dehydrogenase Deficiency. 2014 Jul 17. In: GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–. [PubMed] |
| 6. | Zhang AR, Wang Q, Zhou CE, Zhang JG, Wang XJ, Zhao JK, Lu BH, Yang CX, Gu L, Ma LY, Su JR, Cao B, Wang H. [Risk factors and clinical prognosis analysis of carbapenem-resistant Enterobacterales bacteria nosocomial infection]. Zhonghua Yi Xue Za Zhi. 2021;101:1572-1582. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Rosenblatt R, Atteberry P, Tafesh Z, Ravikumar A, Crawford CV, Lucero C, Jesudian AB, Brown RS Jr, Kumar S, Fortune BE. Uncontrolled diabetes mellitus increases risk of infection in patients with advanced cirrhosis. Dig Liver Dis. 2021;53:445-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Zheng S, Zou Q, Wang X, Bao J, Yu F, Guo F, Liu P, Shen Y, Wang Y, Yang S, Wu W, Sheng J, Vijaykrishna D, Gao H, Chen Y. Factors Associated With Fatality Due to Avian Influenza A(H7N9) Infection in China. Clin Infect Dis. 2020;71:128-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Kanda T, Sasaki R, Masuzaki R, Takahashi H, Mizutani T, Matsumoto N, Nirei K, Moriyama M. Co-Occurrence of Hepatitis A Infection and Chronic Liver Disease. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Yaghobi R, Kazemi MJ, Geramizadeh B, Malek Hosseini SA, Moayedi J. Significance of Occult Hepatitis C Virus Infection in Liver Transplant Patients With Cryptogenic Cirrhosis. Exp Clin Transplant. 2020;18:206-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Llaneras J, Riveiro-Barciela M, Rando-Segura A, Marcos-Fosch C, Roade L, Velázquez F, Rodríguez-Frías F, Esteban R, Buti M. Etiologies and Features of Acute Viral Hepatitis in Spain. Clin Gastroenterol Hepatol. 2021;19:1030-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Nguyen Thi Thu P, Ngo Thi Quynh M, Pham Van L, Nguyen Van H, Nguyen Thanh H. Determination of Risk Factors Associated with the Failure of 12 Weeks of Direct-Acting Antiviral Therapy in Patients with Hepatitis C: A Prospective Study. Biomed Res Int. 2022;2022:6054677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 13. | Fan YN, Ji TT, Liang RY, Yu YY, Xu JH. [Retrospective analysis of risk factors of liver cirrhosis combined with overt hepatic encephalopathy: a single -center case-control study]. Zhonghua Gan Zang Bing Za Zhi. 2021;29:133-136. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Salih OAMM, Nail AM, Modawe GA, Swar MO, Ahmed MH, Khalil A, Satti AB, Abuzeid N. Risk Factors of Inpatients Mortality of Visceral Leishmaniasis, Khartoum State, Sudan. J Glob Infect Dis. 2020;12:135-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Casulleras M, Zhang IW, López-Vicario C, Clària J. Leukocytes, Systemic Inflammation and Immunopathology in Acute-on-Chronic Liver Failure. Cells. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 16. | Bartoletti M, Baldassarre M, Domenicali M, Lewis RE, Giannella M, Antognoli A, Rinaldi M, Zaccherini G, Verucchi G, Marconi L, Tamè M, Berardi S, Napoli L, Siniscalchi A, Fabbri A, Biselli M, Tufoni M, Pavarin RM, Trevisani F, Viale P, Bernardi M, Caraceni P. Prognostic Role of Bacterial and Fungal Infections in Patients With Liver Cirrhosis With and Without Acute-on-Chronic Liver Failure: A Prospective 2-Center Study. Open Forum Infect Dis. 2020;7:ofaa453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Tao Y, Sun ZJ, Zhu L, Lang JH. [Clinical analysis of 68 cases of sepsis during pregnancy and the postpartum period]. Zhonghua Fu Chan Ke Za Zhi. 2020;55:770-777. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Hong Y, Dufendach K, Wang Y, Thoma F, Kilic A. Impact of hepatic steatosis on outcomes after left ventricular assist device implantation. J Card Surg. 2021;36:2277-2283. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Elahi W, Syed AZ, Nasim F, Anwar A, Hashmi AA. Hepatitis B and C Infections in Patients With Prolonged Hemodialysis Secondary to Chronic Renal Failure. Cureus. 2020;12:e10905. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Egawa H. Challenge to ABO blood type barrier in living donor liver transplantation. Hepatobiliary Pancreat Dis Int. 2020;19:342-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Ullah K, Dogar AW, Uddin S, Hasnain S, Ahmad B, Ghaffar A. Frequency and Outcome of Hepatic Arterial Thrombosis in Recipients of Living Donor Liver Transplantation. J Coll Physicians Surg Pak. 2021;31:897-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 22. | Cheung A, Kwo P. Viral Hepatitis Other than A, B, and C: Evaluation and Management. Clin Liver Dis. 2020;24:405-419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (3)] |
| 23. | Wong GL, Wong VW, Yuen BW, Tse YK, Yip TC, Luk HW, Lui GC, Chan HL. Risk of hepatitis B surface antigen seroreversion after corticosteroid treatment in patients with previous hepatitis B virus exposure. J Hepatol. 2020;72:57-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 24. | Liao X, Zhao S, Yin J, Liu L, Liang J, Jiang Y, Yu N, Fan R, Zhong C. Sexual Dysfunction in Patients with Chronic Hepatitis B: Prevalence and Risk Factors. J Sex Med. 2022;19:207-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Shi J, Zhou Y, Wang F, Wang C, Miao H, Sun T, Shan Y, Cui Y, Zhang Y. A case series of children with adenovirus pneumonia: three-year experiences in a tertiary PICU. BMC Pediatr. 2020;20:375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Kang WW, Duan LP, Xu MM, Kong M, Cao YY, Liu F, Han T, Duan ZP, Chen Y; China Network for Severe Liver Diseases(CNSLD). [Comparison of clinical features between patients with acute-on-chronic liver failure and decompensated liver cirrhosis combined with acute kidney injury]. Zhonghua Gan Zang Bing Za Zhi. 2020;28:391-396. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Namiki T, Takayama S, Arita R, Ishii T, Kainuma M, Makino T, Mimura M, Yoshino T, Nogami T, Arai M, Sato J, Tanaka K, Nakae H, Igari H, Ozawa Y, Shiko Y, Kawasaki Y, Nezu M, Ito T. A structured summary of a study protocol for a multi-center, randomized controlled trial (RCT) of COVID-19 prevention with Kampo medicines (Integrative Management in Japan for Epidemic Disease by prophylactic study: IMJEDI P1 study). Trials. 2021;22:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Sahra S, Jahangir A, Iqbal QZ, Mobarakai N, Glaser A, Jahangir A. Co-infection of hepatitis E virus and Plasmodium falciparum malaria: A genuine risk in sub-Saharan Africa. Parasit Vectors. 2021;14:215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 29. | Peng Q, Zhang L, Ai M, Huang L, Ai Y. Clinical values of cerebral oxygen saturation monitoring in patients with septic shock. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2021;46:1212-1219. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 30. | Iriyama H, Abe T, Kushimoto S, Fujishima S, Ogura H, Shiraishi A, Saitoh D, Mayumi T, Naito T, Komori A, Hifumi T, Shiino Y, Nakada TA, Tarui T, Otomo Y, Okamoto K, Umemura Y, Kotani J, Sakamoto Y, Sasaki J, Shiraishi SI, Takuma K, Tsuruta R, Hagiwara A, Yamakawa K, Masuno T, Takeyama N, Yamashita N, Ikeda H, Ueyama M, Fujimi S, Gando S; JAAM FORECAST group. Risk modifiers of acute respiratory distress syndrome in patients with non-pulmonary sepsis: a retrospective analysis of the FORECAST study. J Intensive Care. 2020;8:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Lutfi R, Abulebda K, Nitu ME, Molleston JP, Bozic MA, Subbarao G. Intensive Care Management of Pediatric Acute Liver Failure. J Pediatr Gastroenterol Nutr. 2017;64:660-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 32. | Søreide JA, Deshpande R. Post hepatectomy liver failure (PHLF) - Recent advances in prevention and clinical management. Eur J Surg Oncol. 2021;47:216-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 139] [Article Influence: 27.8] [Reference Citation Analysis (1)] |
| 33. | Yeh ML, Huang CF, Huang CI, Holmes JA, Hsieh MH, Tsai YS, Liang PC, Tsai PC, Hsieh MY, Lin ZY, Chen SC, Huang JF, Dai CY, Chuang WL, Chung RT, Yu ML. Hepatitis B-related outcomes following direct-acting antiviral therapy in Taiwanese patients with chronic HBV/HCV co-infection. J Hepatol. 2020;73:62-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 34. | Hsu JT, Hsu PI, Shie CB, Chuah SK, Wu IT, Huang WW, Tang SY, Tsai KF, Kuo LF, Ghose S, Hsu JC, Shih CA. Comparison of the Efficacies of Direct-Acting Antiviral Treatment for HCV Infection in People Who Inject Drugs and Non-Drug Users. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |