Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.4905
Revised: May 12, 2024
Accepted: June 13, 2024
Published online: August 6, 2024
Processing time: 128 Days and 21 Hours
Spastic pelvic floor syndrome (SPFS) is a refractory pelvic floor disease characterized by abnormal (uncoordinated) contractions of the external anal sphincter and puborectalis muscle during defecation, resulting in rectal emptation and obstructive constipation. The clinical manifestations of SPFS are mainly characterized by difficult defecation, often accompanied by a sense of anal blockage and drooping. Manual defecation is usually needed during defecation. From physical examination, it is commonly observed that the patient's anal muscle tension is high, and it is difficult or even impossible to enter with his fingers.
To investigate the characteristics of anorectal pressure and botulinum toxin A injection combined with biofeedback in treating pelvic floor muscle spasm syndrome.
Retrospective analysis of 50 patients diagnosed with pelvic floor spasm syn
After the botulinum toxin A injection combined with two cycles of biofeedback therapy, the patient's postoperative resting and systolic blood pressure were significantly lower than before surgery (P < 0.05). Moreover, the electromy
Botulinum toxin A injection combined with biofeedback can significantly reduce pelvic floor muscle tension in treating pelvic floor muscle spasm syndrome. Anorectal manometry is an effective method to evaluate the efficacy of treatment objectively. However, randomized controlled trials are needed.
Core Tip: In this study, a retrospective analysis was conducted on 50 patients diagnosed with pelvic floor spasm syndrome who received injections of type A botulinum toxin and underwent two cycles of biofeedback therapy. After treatment, the patients' postoperative resting pressure and systolic pressure were significantly lower than those before surgery, and the electromyogram index during resting and after resting was significantly lower than before surgery. Type A botulinum toxin injection combined with biofeedback therapy can significantly reduce the tension of the pelvic floor muscles in treating pelvic floor muscle spasm syndrome.
- Citation: Sun FF, Chen YQ, Jiang ZL, Ma L. Botulinum toxin type A injection combined with biofeedback in the treatment of spastic pelvic floor syndrome. World J Clin Cases 2024; 12(22): 4905-4912
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/4905.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.4905
Spastic pelvic floor syndrome (SPFS) is a refractory pelvic floor disease characterized by abnormal (uncoordinated) contractions of the external anal sphincter and puborectalis muscle during defecation, resulting in rectal emptation and obstructive constipation. The clinical manifestations of SPFS are mainly characterized by difficult defecation, often accompanied by a sense of anal blockage and drooping. Manual defecation is usually needed during defecation. From physical examination, it is commonly observed that the patient's anal muscle tension is high, and it is difficult or even impossible to enter with his fingers. It is also generally believed that abnormal pelvic floor muscle spasms mainly characterize pelvic floor muscle spasm syndrome. Although injection of botulinum toxin A can relax and paralyze muscles and reduce muscle tension, contradictory contractions still exist in the defecation process.
Thus, this study evaluated the treatment of pelvic floor muscle spasm syndrome by injection of botulinum toxin A combined with biofeedback through an objective evaluation method.
General data: A retrospective observational study was used. Patients with severe defecation disorder or suspected pelvic floor spasm syndrome admitted to the Department of Anorectal Surgery of Qingdao Eighth People's Hospital from 2020 to 2023 were retrospectively assessed. We included patients who underwent anorectal physiological examination in Qingdao No. 8 People's Hospital (Qingdao, China). The participants had no major systemic disease or anorectal inflammation, and 54 patients met the inclusion criteria. Exclusion criteria included a history of pelvic floor surgery and incomplete medical history. As such, a total of 4 patients were excluded. Information about medical history was collected from electronic patient records. The hospital ethics committee approved this study.
Surgical methods: Patients were forbidden to eat for 6 h before surgery and were given a clean enema for 1 h before surgery. The patient was placed in the supine knife position, and topical anesthesia was applied locally around the anus. The sonographer positioned the puborectalis muscle under ultrasound, and 100 U of botulinum toxin A was diluted to 10 mL before surgery. Following the injection, fingers were locally massaged in the rectal cavity to promote the complete absorption and dispersion of the drug solution. A postoperative observation was made for bleeding, infection, and other complications.
Physical therapy: Biofeedback stimulation was done using a pelvic floor rehabilitation instrument (SA980X; Nanjing Weisi Medical Technology Co., Ltd., Nanjing, China). This technology is the advanced version of the biofeedback therapy instrument, which can carry out biofeedback therapy and provide pelvic floor muscle electrical stimulation therapy. During the treatment process, the electrical activity signals of the surface muscle before rest, fast muscle (class II muscle), slow muscle (class I muscle), and post-rest stage were recorded before and after rest.
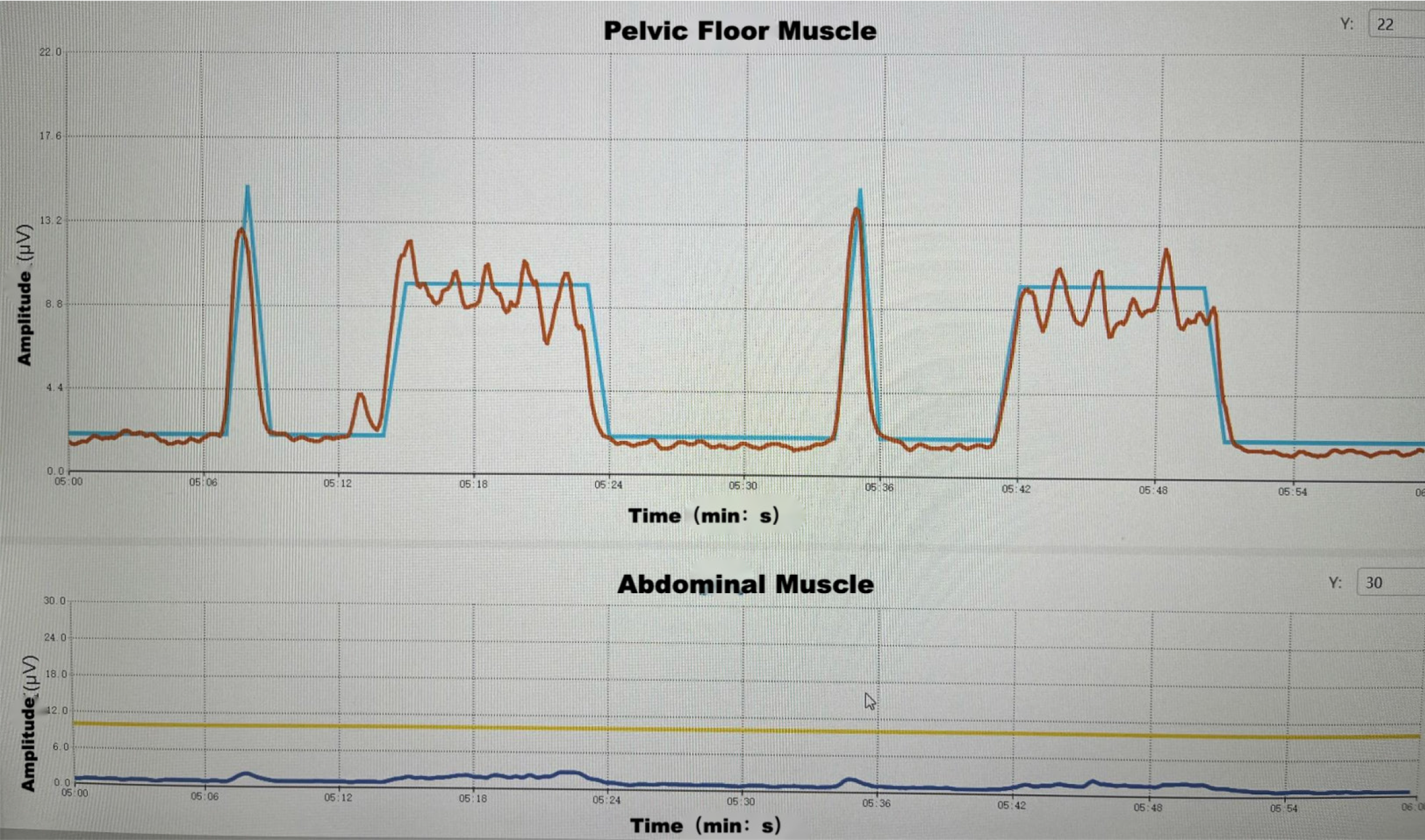
Specific treatment process: The patient was first placed in the left decubitus position. The therapist slowly inserted a rectal electrode into the patient's rectum, and then the patient was placed in a supine position. Each patient was evaluated for 3 min at first and instructed to cooperate with the training according to the computer voice and screen prompt line (Figure 1). Furthermore, parameters were adjusted according to the personal test results, and the degree of painlessness was optimal. According to the comprehensive evaluation results of patients, biofeedback stimulation treatment was divided into three modules; each module lasted 15 min. The first module was given electrical stimulation for 5 s each time and relaxation for 5 s. The second module provides biofeedback training. In the third module, relaxation training was given for two courses of treatment (six times per week for a total of 2 wk).
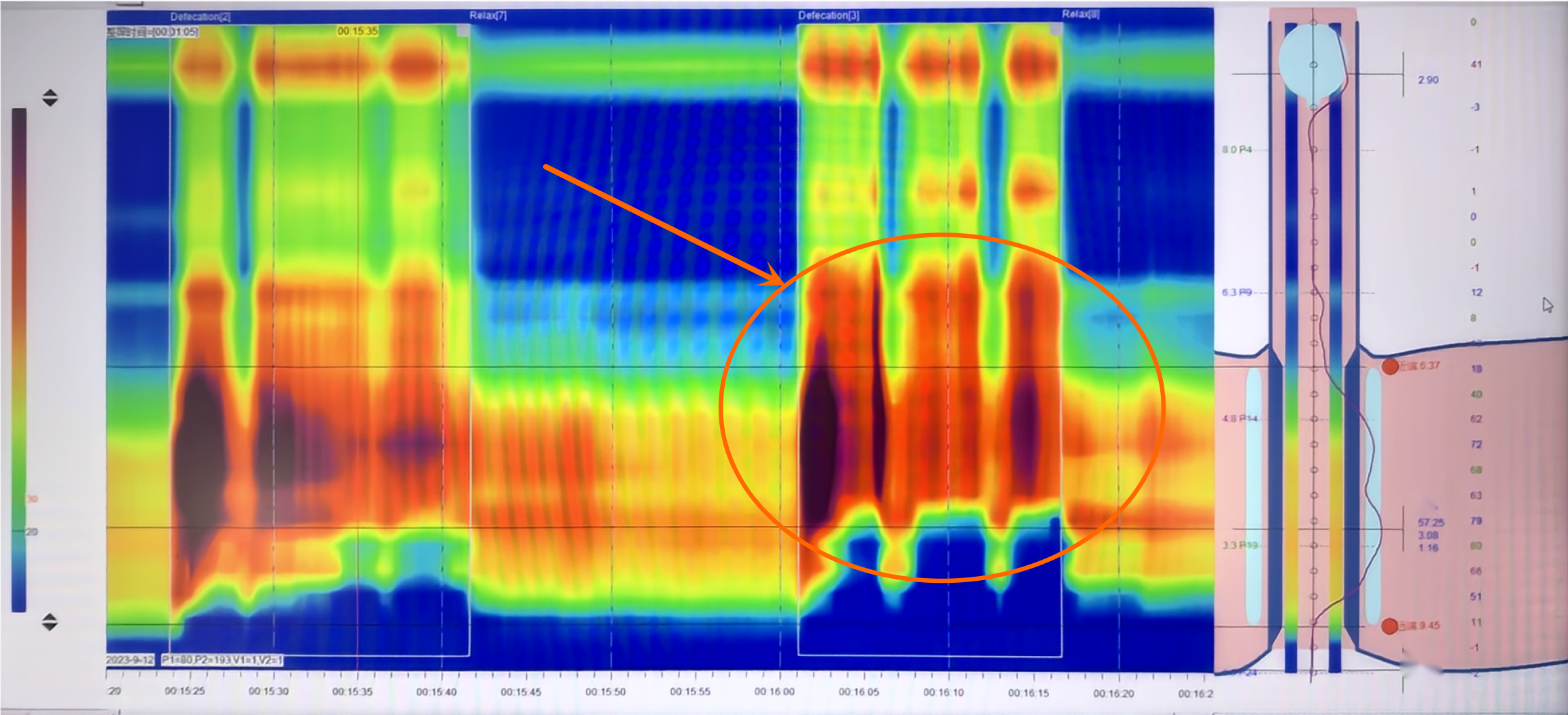
Anorectal dynamic examination: Anorectal physiological tests were performed using the Medkinetic digestive tract dynamic examination system (GAP-24A; Medkinetic; 167-8, Lushan West Road, Bonded South District, Beilun District, Ningbo, Zhejiang, China), as previously described. The patient did not take any medication prior to the test, which might affect the results. The patient was placed in the left decubitus position. Then a 12-channel pressure catheter was inserted into the rectum, with a total length of 10 cm in the anus and rectum, which was fixed on the patient's buttocks. The pressure of the anus and rectum in the patient's resting state was measured, and the pressure of the anal canal contraction was measured, 5 s for each contraction and 10 s for three consecutive times. Simulated defecation was measured; each defecation was 15 s and the interval was 10 s. Continuous measurement was conducted three times. Moreover, patients were assessed preoperatively and postoperatively.
Pelvic floor muscle strength assessment: The SA980X pelvic floor rehabilitation instrument (Nanjing Weiss Medical Technology Co., Ltd.) was used for biofeedback stimulation therapy, and the electrical activity signals of the surface muscle of patients before and after resting, fast muscle (class II muscle), slow muscle (class I muscle) and post-resting stage were recorded. Patients were assessed preoperatively and postoperatively.
Fifty enrolled patients completed a questionnaire before manometry. The questionnaire assessed defecation-related symptoms, including constipation and their severity. The Agachan constipation score determined the severity of constipation.
SPSS 20.0 software (IBM Corp., Armonk, NY, United States) was used for statistical analyses. Measurement data are expressed as the mean ± standard deviation, and a t-test comparison between groups was performed. The statistical data are expressed as the number of cases and percentage (%), and the χ2 test was used to compare groups. P < 0.05 was considered statistically significant.
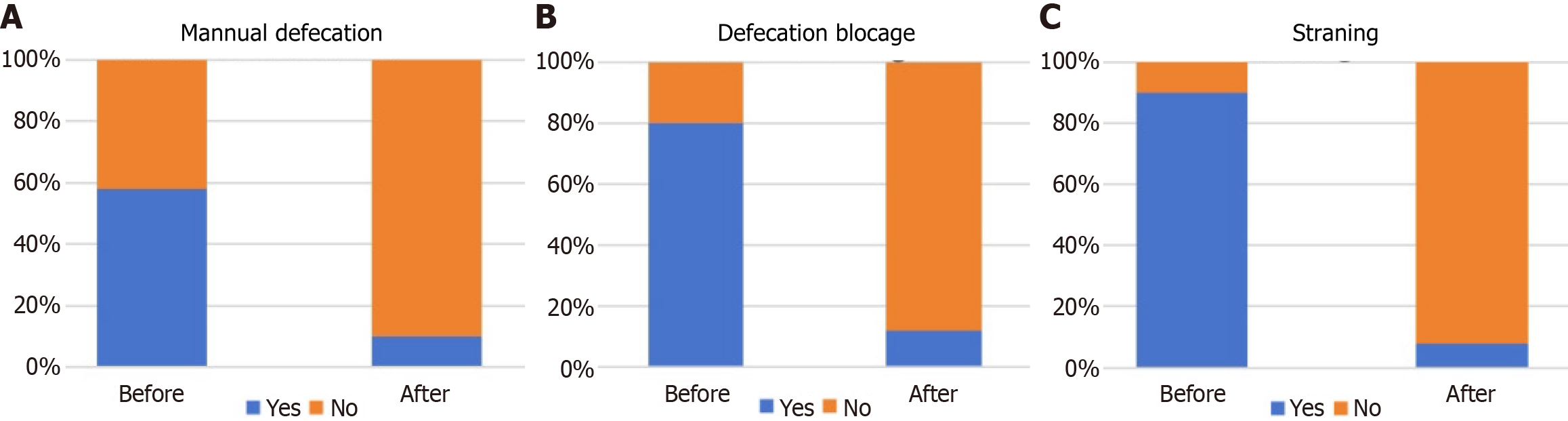
A total of 50 patients who did not respond to conservative treatments and who met the inclusion criteria were included in the study. The data of 50 patients (8 females [16%] and 42 males [84%]) was evaluated (Table 1). Rectal pressure before and after treatment was measured. The resting pressure was reduced by 18.84%, and the systolic blood pressure was reduced by 29.11% (Table 2). Among the 50 patients, most can significantly reduce the tension in the resting and post-resting stages after biofeedback therapy. There is no significant change in the muscle strength of type I and type II muscle tonic contraction variability before and after treatment. The gap between the two becomes smaller, and the activity coordination increases (Table 3). The mean Agachan constipation score was 13.68 ± 5.14. Patients in the current study mainly reported straining (90%), defecation blockage (80%), and manual defecation (60%) (Figure 2).
| Group | Age in yr | BMI | Sex | |
| Males | Female | |||
| Result | 42.1 (9.1) | 25 (4.4) | 42/50 (84) | 8/50 (16) |
| Pressure | Before | After | P value |
| Resting | 92.27 ± 20.38 | 74.89 ± 14.68 | < 0.05 |
| Squeeze | 159.93 ± 40.23 | 113.37 ± 16.97 | < 0.05 |
| Pressure type | Before | After | P value |
| Resting stage | 6.14 ± 3.34 | 3.97 ± 1.87 | < 0.05 |
| Type I muscle tonic contraction variability | 34.37 ± 17.94 | 32.71 ± 12.23 | > 0.05 |
| Type II muscle tonic contraction variability | 19.84 ± 9.76 | 22.76 ± 5.81 | > 0.05 |
| Post-resting stage | 6.01 ± 3.24 | 3.71 ± 1.31 | < 0.05 |
Under normal circumstances, when a patient tries to defecate, the rectal pressure increases, the abdominal wall dilates, and the perineum drops to coordinate movement. Then the anus relaxes, and the rectum empties. One study suggests that insufficient rectal propulsion force, changes in the structure of the rectoanal canal, and damaged anal canal relaxation will affect normal defecation[1]. Pelvic floor muscle spasm syndrome is a refractory pelvic floor disease caused by abnormal contraction of the external anal sphincter and puborectalis muscle during defecation (i.e. uncoordinated contraction) (Figure 3). By measuring the anorectal pressure, we know that the pelvic floor muscles of such patients are spastic in the resting state, and the patient's muscle tension level is high and cannot be completely relaxed. Following the simulated defecation, the anorectal muscle spasm continues, the pressure level increases and the rectal pressure is lower than the anal pressure, presenting a reverse gradient. However, the muscles cannot completely relax after defecation, and the rectal pressure spasms. By contrast, the rectal pressure is significantly higher than the anal pressure during normal defecation.
The aim of our treatment is not only to reduce sphincter tension but also to coordinate defecation movement. One study has confirmed that local injection of botulinum toxin can significantly reduce anal resting tension[2] and relieve pelvic floor muscle spasms. The results of this study showed that postoperative resting pressure (74.89 ± 14.68) was significantly lower than preoperative pressure (92.27 ± 20.38) after botulinum toxin A injection, and postoperative systolic pressure (113.37 ± 16.97) was lower than preoperative pressure (159.93 ± 40.23), with statistically significant differences. Thus, the patient's anal tract tension was significantly relaxed. Botulinum toxin is a protein produced by the anaerobic gram-positive bacterium Clostridium botulinum, which can affect smooth and striated muscles, inhibit acetylcholine release by presynaptic means, and stimulate temporary chemical innervation[3]. Relevant studies have confirmed that injection of botulinum toxin can reduce the pressure of the anal sphincter while avoiding permanent damage to the anal sphincter[4,5]. Meanwhile, botulinum toxin is believed to have a dual mechanism of action, as it relaxes muscles and reduces central sensitization[6]. This was confirmed in a study by Brisinda et al[7] who used botulinum toxin injections to treat anal fissure, in which 780 patients (77.7%) showed apparent complete healing, and anal resting tension was significantly lower than baseline. Notably, this finding confirms that the toxin dose was significantly associated with healing, and the higher the dose, the faster and more significant the decline in resting anal tension.
Although botox injection can reduce anal sphincter pressure, patients still suffer from defecation disorders (conflicting contractions). Additionally, pelvic floor biofeedback therapy has been recommended as a first-line treatment by multiple discipline guidelines[8-11]. Chiarioni et al[12] studied 109 constipation patients who had failed conservative treatment and showed that biofeedback was more effective than laxatives in the treatment of pelvic floor dysfunction constipation. After two stages of treatment, the constipation scores of the patients in this study were significantly lower than those before treatment, and the scores of the patients' feeling of obstructed defecation and hand-assisted defecation were significantly lower than those before treatment and had clinical significance (Table 4). Likewise, their clinical symptoms of difficulty in defecation and blockage improved.
| Parameter | Before | After | P value |
| Straining | 2.76 ± 1.17 | 0.14 ± 0.50 | < 0.01 |
| Defecation blockage | 2.86 ± 1.53 | 0.20 ± 0.57 | < 0.01 |
| Manual defecation | 0.82 ± 0.80 | 0.10 ± 0.30 | < 0.01 |
Patients' muscle strength and stability can be improved considerably. During the training process, breathing relaxation can also reduce the electromyography level of muscles after exercise. At the same time, abdominal muscles can be significantly more relaxed in the resting state. The significance of biofeedback therapy is that it helps patients rebuild the conditioned reflex process, accurately locate the trained muscles, exercise muscle functions, master the key points of action in continuous learning, and control pelvic floor muscles freely[13]. In this study, the electromyography index of patients in the postoperative resting and postoperative resting stages was significantly lower than before surgery, and the patient's pelvic floor muscles were more relaxed. There was no statistically significant difference between the patients' fast and slow muscles before and after surgery (P > 0.05). It was suggested that botulinum toxin injection could locally disperse and relax the pelvic floor muscles, and the patient's ability to control the muscles was decreased. Still, the pelvic floor muscles were no longer in a state of tension because the patients accurately positioned the trained muscles and controlled the pelvic floor muscles.
In this study, patients were only under local infiltration anesthesia, and botulinum toxin injection was performed by palpation. Under non-anesthesia, patients can cooperate with doctors to perform pelvic floor muscle contraction, which is helpful for doctors to master the injection site better. However, due to patients' nervousness and the fact that an unskilled operator may cause injection-related acupuncture injury rate, the palpation-guided injection has certain risks[14]. However, some studies have used electromyography or intravenous ultrasound[15-17]. Notably, ultrasound or electro
In our study, we found two interesting situations. First, several patients with rectal mucosa prolapse after defecation. Thus, we also speculated that this concern with patients with pelvic floor muscle spasms, long hard defecation, and rectal mucosa relaxation occurs due to the spasm of the muscle contraction of the outlet. Additionally, the relaxation of the tissue in the rectum stimulates the mucosal receptors caused by the blockage. As time goes by, the blockage continues to encourage the patient to defecate. Consequently, the patient's defecation time increases, and efforts to defecate aggravate mucosal accumulation and the vicious cycle. Second, we found that most of the patients had a history of pelvic floor spasm syndrome before the occurrence of adverse events in life. Thus, we also consider that after psychological trauma, abnormal secretion of brain-gut peptide, resulting in abnormal gastrointestinal function regulation of the nervous system, led to a decrease in rectal sensitivity, an increase in anorectal contraction rate, an increase in pelvic floor muscle tension causing somatic reaction, that patients cannot self-soothe. With the development of time, patients appear to have pelvic floor muscle spasm syndrome. Thus, our subsequent research topic will explore the relationship between psychological factors and pelvic floor muscle spasm syndrome.
This study provides evidence on the efficacy of botulinum toxin injection and biofeedback in treating pelvic floor muscle spasm syndrome. However, some limitations have been noted in our research. First, the sample size we screened was small and the inclusion criteria were more stringent, but we still thought it necessary. Second, this study is retrospective. Patients were only compared before and after treatment; no controlled study was carried out in the blank group. Thirdly, the dose of botulinum toxin injection is uniform, and there is no individual difference in choosing different doses. Of course, our next research will study the dose of botulinum toxin. Fourth, in our study, there were only two courses of pelvic floor biofeedback therapy (six times per week, 2 wk in total), which was short. Likewise, the long-term efficacy of botox injection combined with biofeedback in the treatment of pelvic floor muscle spasm syndrome needs further improvement. In future studies, we will design a large sample randomized controlled trial and conduct a multicenter study.
Botulinum toxin A injection combined with biofeedback can significantly reduce pelvic floor muscle tension in treating pelvic floor muscle spasm syndrome. Anorectal manometry is an effective method to evaluate the efficacy of treatment objectively. However, added randomized controlled trials are needed.
| 1. | Deb B, Sharma M, Fletcher JG, Srinivasan SG, Chronopoulou A, Chen J, Bailey KR, Feuerhak KJ, Bharucha AE. Inadequate Rectal Pressure and Insufficient Relaxation and Abdominopelvic Coordination in Defecatory Disorders. Gastroenterology. 2022;162:1111-1122.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Brisinda G, Maria G, Bentivoglio AR, Cassetta E, Gui D, Albanese A. A comparison of injections of botulinum toxin and topical nitroglycerin ointment for the treatment of chronic anal fissure. N Engl J Med. 1999;341:65-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 229] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 3. | El-Khawand D, Wehbe S, Whitmore K. Botulinum toxin for conditions of the female pelvis. Int Urogynecol J. 2013;24:1073-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Maria G, Brisinda G, Bentivoglio AR, Cassetta E, Gui D, Albanese A. Botulinum toxin injections in the internal anal sphincter for the treatment of chronic anal fissure: long-term results after two different dosage regimens. Ann Surg. 1998;228:664-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 109] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Maria G, Cassetta E, Gui D, Brisinda G, Bentivoglio AR, Albanese A. A comparison of botulinum toxin and saline for the treatment of chronic anal fissure. N Engl J Med. 1998;338:217-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 210] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 6. | Karp BI, Tandon H, Vigil D, Stratton P. Methodological approaches to botulinum toxin for the treatment of chronic pelvic pain, vaginismus, and vulvar pain disorders. Int Urogynecol J. 2019;30:1071-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Brisinda G, Chiarello MM, Crocco A, Bentivoglio AR, Cariati M, Vanella S. Botulinum toxin injection for the treatment of chronic anal fissure: uni- and multivariate analysis of the factors that promote healing. Int J Colorectal Dis. 2022;37:693-700. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Skardoon GR, Khera AJ, Emmanuel AV, Burgell RE. Review article: dyssynergic defaecation and biofeedback therapy in the pathophysiology and management of functional constipation. Aliment Pharmacol Ther. 2017;46:410-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Paquette IM, Varma MG, Kaiser AM, Steele SR, Rafferty JF. The American Society of Colon and Rectal Surgeons' Clinical Practice Guideline for the Treatment of Fecal Incontinence. Dis Colon Rectum. 2015;58:623-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 121] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 10. | Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Nonsurgical management of urinary incontinence in women: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2014;161:429-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 11. | Narayanan SP, Bharucha AE. A Practical Guide to Biofeedback Therapy for Pelvic Floor Disorders. Curr Gastroenterol Rep. 2019;21:21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 12. | Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006;130:657-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 297] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 13. | Ding SQ. Application of pelvic floor biofeedback therapy in the treatment of pelvic disease. Zhonghua Weichang Waike Zazhi. 2017;20:4. [DOI] [Full Text] |
| 14. | Brueseke TJ, Lane FL. Ischiorectal fossa abscess after pelvic floor injection of botulinum toxin. Am J Obstet Gynecol. 2012;206:e7-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Zhang Y, Wang ZN, He L, Gao G, Zhai Q, Yin ZT, Zeng XD. Botulinum toxin type-A injection to treat patients with intractable anismus unresponsive to simple biofeedback training. World J Gastroenterol. 2014;20:12602-12607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Ron Y, Avni Y, Lukovetski A, Wardi J, Geva D, Birkenfeld S, Halpern Z. Botulinum toxin type-A in therapy of patients with anismus. Dis Colon Rectum. 2001;44:1821-1826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Nesbitt-Hawes EM, Dietz HP, Abbott JA. Four-dimensional ultrasound guidance for pelvic floor Botulinum toxin-A injection in chronic pelvic pain: a novel technique. Ultrasound Obstet Gynecol. 2018;51:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Yiannakopoulos CK, Megaloikonomos PD, Foufa K, Gliatis J. Ultrasound-guided versus palpation-guided corticosteroid injections for tendinosis of the long head of the biceps: A randomized comparative study. Skeletal Radiol. 2020;49:585-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Wu C, Xue F, Chang W, Lian Y, Zheng Y, Xie N, Zhang L, Chen C. Botulinum toxin type A with or without needle electromyographic guidance in patients with cervical dystonia. Springerplus. 2016;5:1292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |