Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.4897
Revised: May 28, 2024
Accepted: June 21, 2024
Published online: August 6, 2024
Processing time: 130 Days and 19.8 Hours
It has been confirmed that the increased posterior tibial slope over 12 degrees is a risk factor for anterior cruciate ligament injury, and varus deformity can agg
To evaluate the efficacy of modified high tibial osteotomy (HTO) and anterior cruciate ligament reconstruction (ACLR) in the treatment of anterior cruciate ligament (ACL) injuries with varus deformities and increased posterior tibial slope (PTS) based on clinical and imaging data.
The patient data in this retrospective study were collected from 2019 to 2021. A total of 6 patients were diagnosed with ACL injury combined with varus defor
All 6 patients (6 knee joints) were followed up for an average of 20.8 ± 3.7 months. The average age at surgery was 29.5 ± 3.8 years. At the last follow-up, all patients resumed competitive sports. The International Knee Documentation Committee score increased from 50.3 ± 3.1 to 87.0 ± 2.8, the Lysholm score increased from 43.8 ± 4.9 to 86 ± 3.1, and the Tegner activity level increased from 2.2 ± 0.7 to 7.0 ± 0.6. The average movement distance of the tibia anterior translation was 4.8 ± 1.1 mm, medial proximal tibial angle (MPTA) was 88.9 ± 1.3° at the last follow-up, and the PTS was 8.4 ± 1.4°, both of which were significantly higher than those before surgery (P < 0.05).
Modified open wedge HTO combined with ACLR can effectively treat patients with ACL ruptures with an associated increased PTS and varus deformity. The short-term effect is significant, but the long-term effect requires further follow-up.
Core Tip: Some patients anterior cruciate ligament injury have sagittal varus deformity and coronal increased posterior tibial slope. We can correct the biplanar deformity simultaneously with a modified osteotomy.
- Citation: Deng FY, Liu JC, Li Z. Osteotomy combined with anterior cruciate ligament reconstruction for anterior cruciate ligament injury and biplanar deformity. World J Clin Cases 2024; 12(22): 4897-4904
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/4897.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.4897
At present, high tibial osteotomy (HTO) is widely used in varus deformity accompanied by osteoarthritis and has achieved good results. It is especially appropriate for some young patients with high athletic ability requirements, which can preserve the function of the knee joint to a greater extent and delay bone arthritis progression[1]. Anterior cruciate ligament reconstruction (ACLR) can effectively restore stability of the knee joint and help patients improve their athletic ability. For patients with medial knee osteoarthritis and varus deformity caused by anterior cruciate ligament (ACL) injury, HTO and ACLR have significant advantages, which have been reported in the relevant literature[2-5].
In addition, there have been literature reports and biomechanical experiments proving that a posterior tibial slope (PTS) of more than 12° will increase the probability of ACLR failure to a large extent[6-8]. Therefore, some surgeons have used different osteotomies to correct the PTS in order to reduce the risk of ligament failure after reconstruction[9,10]. We have found that some patients with ACL injury have sagittal varus deformity and coronal increased PTS. Therefore, when we reconstruct the ACL, combined osteotomy corrects the patient's sagittal and coronal deformity. We hypothesize that this procedure could effectively delay knee degeneration and reduce the probability of ACLR revision.
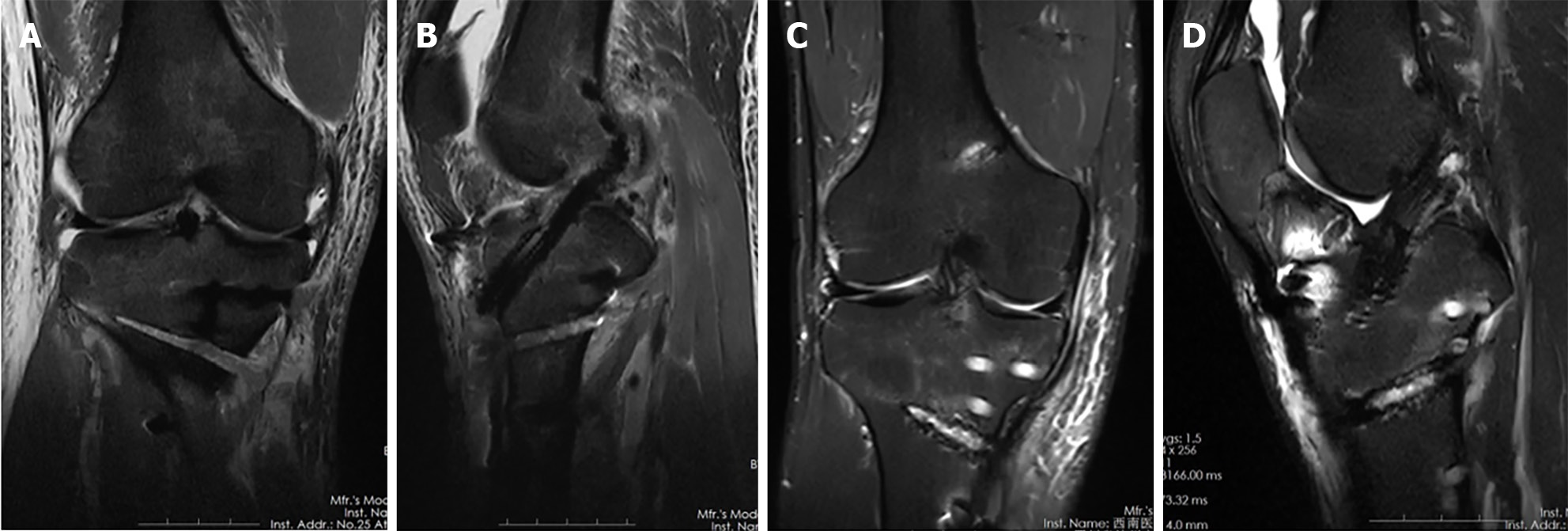
We reviewed a total of 6 patients diagnosed with ACL injury combined with varus deformities and increased PTS from 2019 to 2021. All 6 patients underwent modified open wedge HTO and arthroscopic ACLR. The inclusion criteria for this study were: (1) Magnetic resonance imaging (MRI) to confirm ACL rupture; (2) Full-length imaging of lower limbs to confirm varus deformity (over 5 degrees); (3) MRI or arthroscopy to confirm medial meniscus injury or medial cartilage injury; and (4) The follow-up time was at least 1 year. Exclusion criteria were: patients had a combination of other ligament injuries, lateral meniscus tear, and inflammatory knee arthritis.
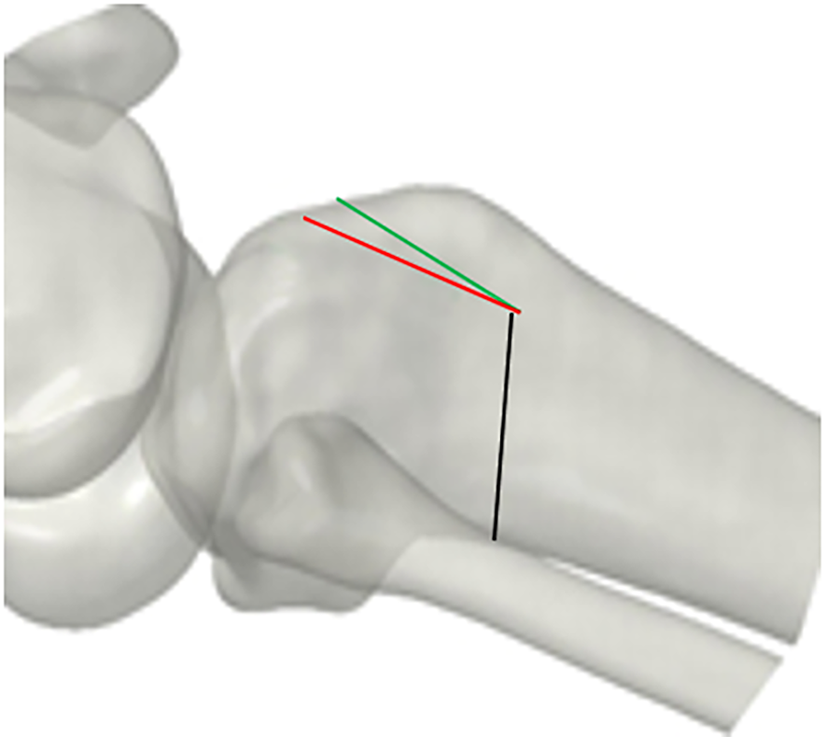
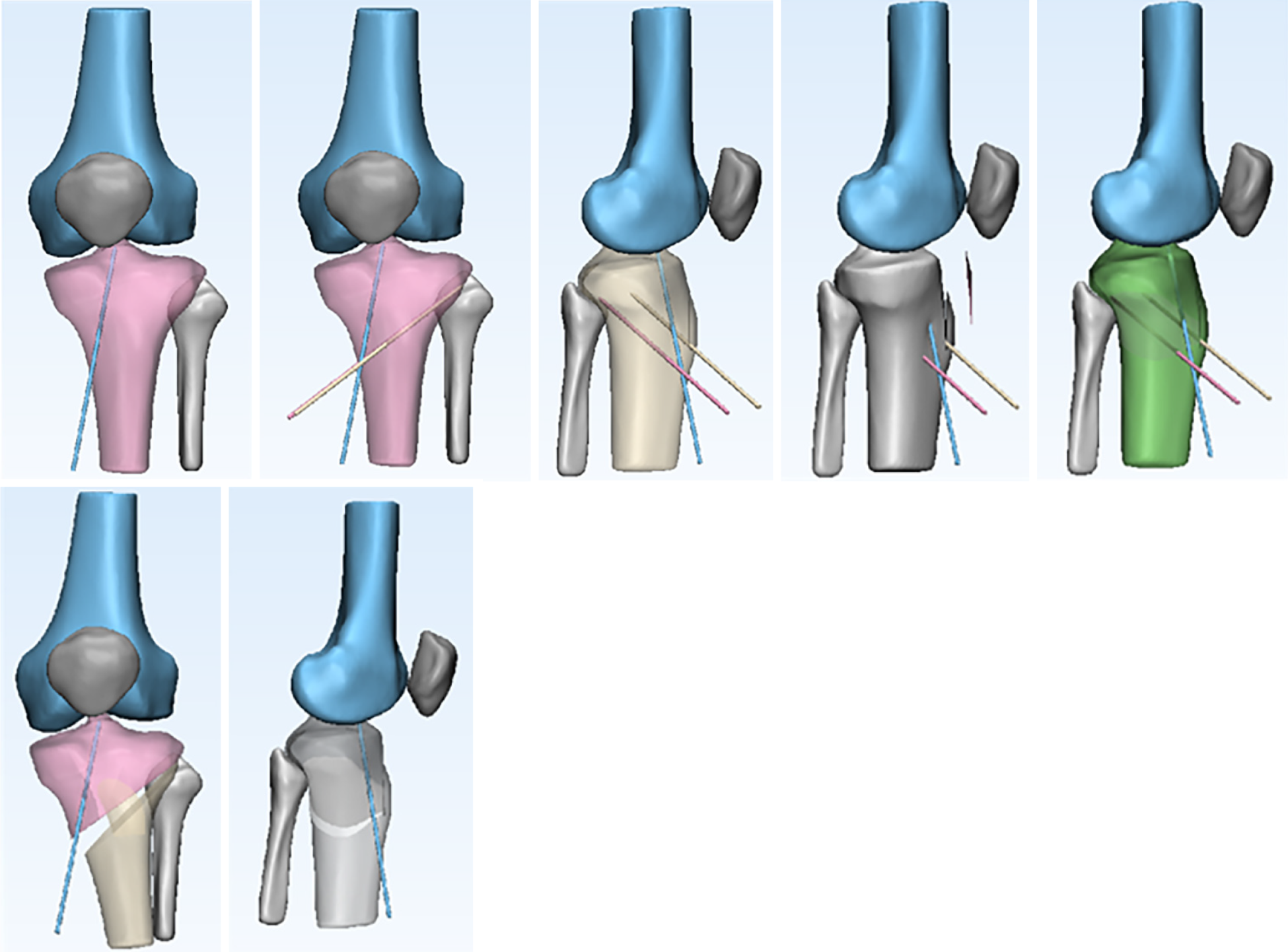
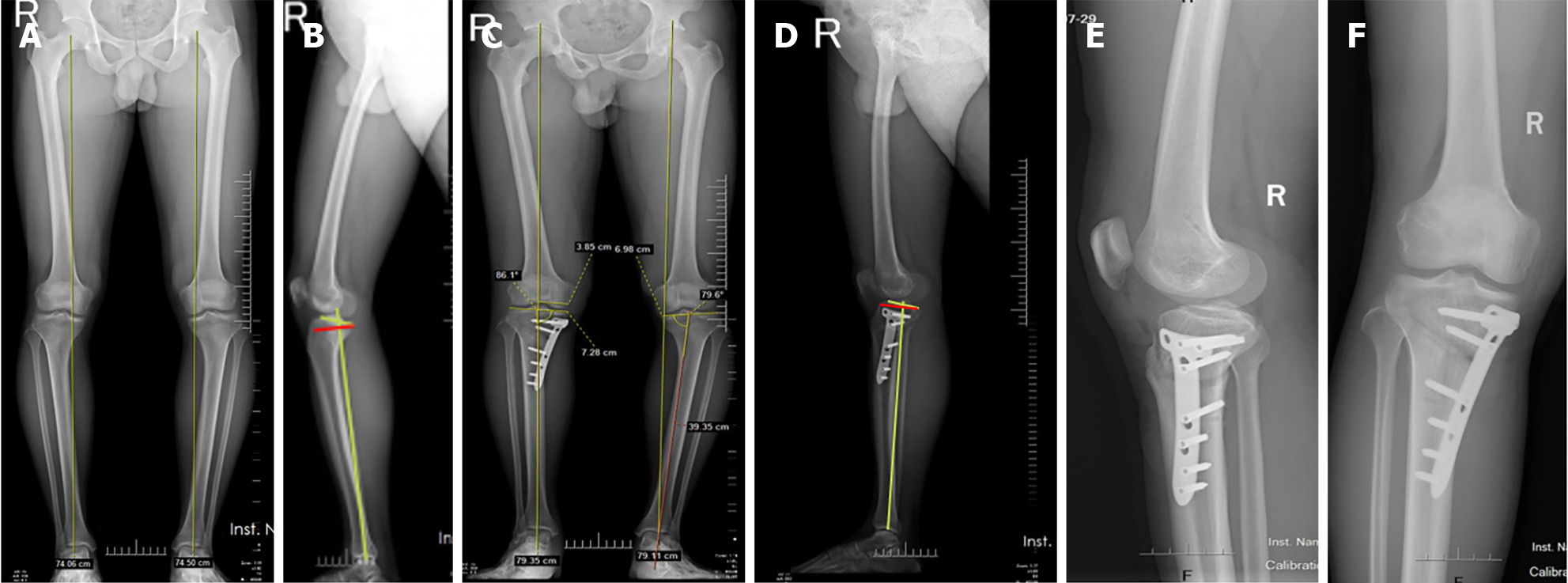
Two senior surgeons performed the operations on all patients. All cases underwent diagnostic arthroscopy before ACLR and osteotomy. All 6 cases had different degrees of cartilage damage and medial meniscus tear. Among them, 4 cases had degree I cartilage injury, 2 cases had degree II cartilage injury, 3 cases had a longitudinal tear of the medial meniscus, 1 case had an oblique tear of the posterior angle, and 1 case had a compound tear. In all cases, four-strand hamstring tendon grafts were obtained from the same side. The target force line for osteotomy correction was 50%, and the PTS was corrected by 5 degrees. Under arthroscopic monitoring and C-arm fluoroscopy, the femoral tunnel was firstly located, and after confirming the tibial tunnel, a Kirschner wire was inserted. Two Kirschner wires were placed 3.5 cm distal to the medial tibial plateau, and the position was confirmed to be consistent with the plan under C-arm fluoroscopy. Osteotomy was performed twice with a swing saw at 1.5 cm behind the tibial tubercle, as shown in Figure 1. The green line is the ascending osteotomy line behind the tibial tubercle, and the red line is the increased wedge osteotomy line. The wedge osteotomy between the two lines was about 5 mm, and the PTS can be corrected by closing the area between the two lines. A swing saw was used to cut the tibia along the direction of two Kirschner wires, and the varus deformity is corrected by opening the gap with an instrument. The osteotomy area behind the tibial tubercle was then closed by applying pressure to the knee in front of the tibia and then the tibia was fixed with a plate and screw. Finally, the femur and tibia were drilled and the bone tunnel was made, and the tendon was inserted. The autologous hamstring tendon was fixed by RigidFix in the femur and the tibia was fixed with an extrusion screw and the tendon suture was fixed on the plate. Detailed surgical procedures are shown in Figure 2.
All data were collected by an independent orthopedic researcher who was not directly involved in patient mana
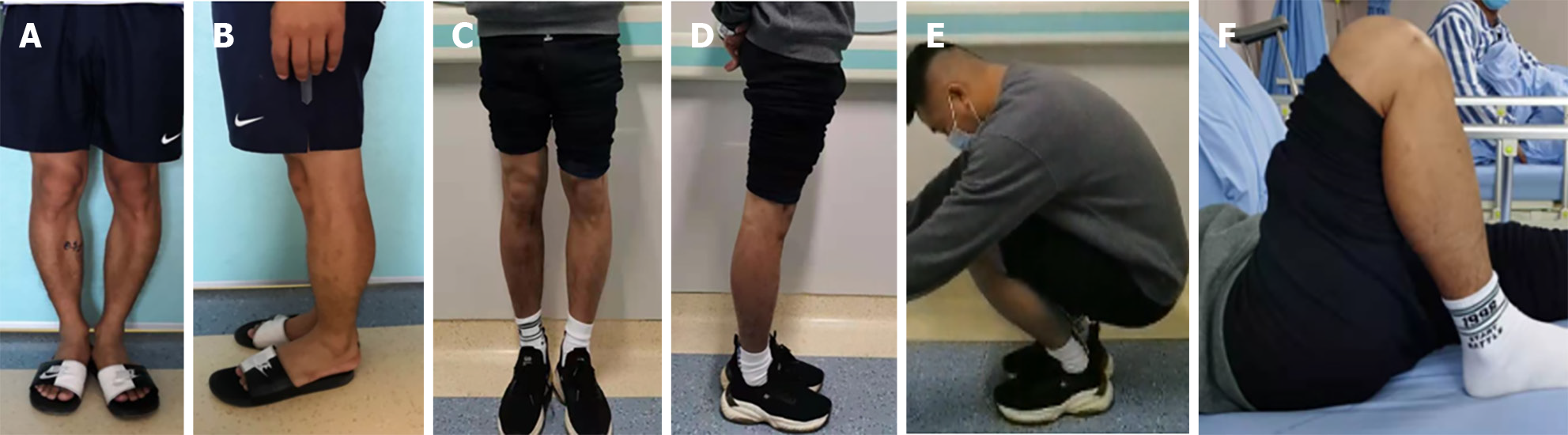
Six patients (6 knees) were followed up for an average of 20.8 ± 3.7 months. The average age of the patients was 29.5 ± 3.7 years. At the last follow-up, all patients resumed competitive sports. Comparing the preoperative and last follow-up findings, the medial proximal tibial angle was 83.0 ± 0.9° before the operation and was 88.5 ± 1.1° at the last follow-up, with an average improvement of 5.6 ± 1.3°; preoperative PTS was 14.4 ± 0.8° and at the last follow-up was 8.8 ± 1.2°, an average improvement of 5.6 ± 0.6°; the preoperative translation distance of the tibia was 8.6 ± 1.0 mm and at the last follow-up was 3.9 ± 0.6 mm, an average improvement of 4.7 ± 1.0 mm; the IKDC score was 50.3 ± 3.1 points before the operation, and at the last follow-up was 87.0 ± 2.8 points; the Lysholm score before the operation was 43.8 ± 4.9 points and at the last follow-up was 86.6 ± 3.4 points; the Tegner activity level was 2.2 ± 0.7 before the operation and was 7.0 ± 0.6 at last follow-up; the last follow-up results were significantly higher than those before the operation, and the difference was statistically significant (P < 0.05, Tables 1 and 2). At the last follow-up, all patients were negative for the Lachman test and pivot-shift test. All wounds healed at stage I, and no ligament rupture, poor functional activity, wound infection, deep vein thrombosis of the lower limbs, bone nonunion, or delayed healing were found during the last follow-up (Figure 6).
| Preoperative | Final follow-up | P value | |
| IKDC | 50.3 ± 3.1 | 87.0 ± 2.8 | < 0.05 |
| Tegner | 2.2 ± 0.7 | 7.0 ± 0.6 | < 0.05 |
| Lysholm | 43.8 ± 4.9 | 86.6 ± 3.4 | < 0.05 |
| Preoperative | Final follow-up | Difference | P value | |
| MPTA | 83.0 ± 0.9 | 88.5 ± 1.1 | 5.6 ± 1.3 | < 0.05 |
| PTS | 14.4 ± 0.8 | 8.8 ± 1.2 | 5.6 ± 0.6 | < 0.05 |
| Side-to-side difference (mm) | 8.7 ± 1.0 | 3.9 ± 0.6 | 4.8 ± 1.1 | < 0.05 |
Anterior cruciate ligament injury is usually accompanied by medial meniscus injury, medial cartilage injury, etc[11,12], especially in young people. The aforementioned accompanying injuries will accelerate degeneration of the medial tibiofemoral joint. This means that in the foreseeable future, the risk of joint replacement for young patients will be greatly increased, which will significantly reduce the patient's exercise level. In particular, when combined with varus deformity, this risk will greatly increase. Knee varus deformity is prone to damage the medial meniscus and cartilage, and this injury can further aggravate the knee varus deformity. Therefore, for the medial meniscus injury accompanied by knee varus deformity, it is difficult to obtain satisfactory clinical effects by simply treating the meniscus injury. Osteotomy should also be used to improve the force line of the lower limbs and the mechanical environment in the knee joint.
Current relevant research opinions confirm that HTO can increase the viability of the joints, improve the patient's exercise level, and reduce the probability of joint replacement[13,14]. In recent years, HTO has also been used in patients with ACL combined with varus deformity, aiming to improve the patient's exercise capacity and delay the occurrence of medial osteoarthritis. Some surgeons have performed ACLR combined with HTO in patients with an ACL injury and varus deformity. The results have shown that this operation can improve the patient's exercise ability. Schneider et al[15] performed ACLR and medial open wedge-shaped HTO in 35 patients. After 10 years of follow-up, it was found that approximately 80% of patients resumed exercise, with a low recurrence rate and good control of anterior lateral relaxation. There was no rapid progression of osteoarthritis. Khan et al[16] also published a review in 2019 which showed that the complications, re-rupture, and revision rates after HTO and ACLR were lower. Jin et al[17] performed ACLR and medial open wedge-shaped HTO in 24 patients. These patients were followed up for 5 years and were found to have satisfactory function and the level of postoperative activity was significantly improved.
Relevant literature has confirmed that PTS is an independent risk factor for the failure of ACLR[18,19]. Biomechanical experiments have confirmed that proximal tibial anterior closing wedge osteotomy can reduce the pressure on the ACL and displacement of the tibia. Webb et al[6] showed that the PTS is an independent risk factor for ACL injury after ALCR, especially when it is greater than 12°. To reduce the failure rate after ACLR, different osteotomies are used to reduce the PTS. Sonnery-Cottet et al[10] measured a significant increase in the PTS of 5 patients who had rupture after ACLR. The surgeon performed ACL revision combined with anterior closing wedge proximal tibial osteotomy in all patients. The stability and function of the knee joint recovered after the operation, and satisfactory clinical results were obtained. Dejour et al[9] also performed an anterior closing wedge proximal tibial osteotomy in 9 patients with excessively large PTS who suffered a rupture after the initial ACLR, and the postoperative results were satisfactory. DePhillipo et al[20] described in detail the technique of adjusting the PTS through the anterior closing wedge proximal tibial osteotomy. The advantage is that the adjustment angle is more accurate. The existence of the rear hinge can ensure the stability of the tibia, and the proximal closed osteotomy area is easier to heal. The disadvantage lies in the need for tibial tuberosity displacement, which may lead to bone nonunion. When the correction degree is too large, the posterior hinge may break, and the position of the patella may shift, resulting in a low or high patella.
Previous related literature reported that the anterior closing wedge proximal tibial osteotomy combined with ACLR was mainly used in revision of the ACL. The operation to reduce the PTS can reduce the chance of failure of ACLR[10]. However, related literature has confirmed that the clinical outcome of ACL revision surgery is worse than that of the initial ligament reconstruction. For some patients with a rupture of the ACL with a PTS greater than 12°, an anterior closing wedge proximal tibial osteotomy can be considered for the first reconstruction. In particular, for combined meniscus damage or cartilage damage, the surgical indications are more obvious, which is also more consistent with the results of Dejour et al[9].
In summary, for patients with simple sagittal deformity and PTS greater than 12°, the anterior closing wedge proximal tibial osteotomy is required to reduce PTS to reduce ligament tension and the possibility of its failure, especially when accompanied by meniscus injury or cartilage damage. However, for some patients with varus deformity, a simple closed anterior tibial osteotomy cannot correct the coronal deformity, and HTO alone cannot solve the sagittal deformity. Therefore, by partially adjusting the HTO, we cut a piece of bone backward during horizontal osteotomy. After placing a spreader to correct the varus deformity, we slowly close the anterior osteotomy area backward to correct the PTS. The biggest advantage of this procedure is that it can correct biplanar deformity at the same time. According to relevant literature reports, the simple open wedge HTO will slightly increase the PTS, and we can reduce the PTS at the same time through this improvement, and avoid tibial tubercle displacement. The disadvantage is that excessive correction may cause the hinge to break, but the Tomofix steel plate can provide strong fixation and ensure the stability of the tibia. We conducted postoperative follow-up and imaging in 6 patients, their functional recovery was good, and all patients significantly improved compared with preoperative levels, and recovered high-intensity exercise ability. The final MRI showed that the ACL was stable after reconstruction, and there was no tearing of the meniscus. The postoperative full-length film showed that the varus deformity was significantly corrected, the correction angle was not significantly lost, and there was no significant progress in osteoarthritis.
There are limitations in this study. Firstly, it was a retrospective study, with a small sample size and short follow-up time, and long-term follow-up is needed to determine patient outcomes. Secondly, there was no control group and no secondary arthroscopy. Although the follow-up results of the 6 patients showed that there was no rupture or failure of the anterior cruciate ligament, and the osteotomy area had healed well, further follow-up is required to evaluate the long-term curative effect.
The results show that the modified open wedge HTO and ACLR under arthroscopy can effectively treat patients with ACL injury combined with varus deformities and increased PTS. The short-term effect is significant, but the long-term effect requires further follow-up.
| 1. | Jeon YS, Ahn CH, Kim MK. Comparison of HTO with articular cartilage surgery and UKA in unicompartmental OA. J Orthop Surg (Hong Kong). 2017;25:2309499016684092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Marriott K, Birmingham TB, Kean CO, Hui C, Jenkyn TR, Giffin JR. Five-year changes in gait biomechanics after concomitant high tibial osteotomy and ACL reconstruction in patients with medial knee osteoarthritis. Am J Sports Med. 2015;43:2277-2285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Schuster P, Schulz M, Richter J. Combined Biplanar High Tibial Osteotomy, Anterior Cruciate Ligament Reconstruction, and Abrasion/Microfracture in Severe Medial Osteoarthritis of Unstable Varus Knees. Arthroscopy. 2016;32:283-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Rossi MJ. Editorial Commentary: Combined High Tibial Osteotomy and Anterior Cruciate Ligament Reconstruction Yield Good Results With Unknown Effect of the Cartilage Restoration Procedure. Arthroscopy. 2016;32:293-294. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Crawford MD, Diehl LH, Amendola A. Surgical Management and Treatment of the Anterior Cruciate Ligament-Deficient Knee with Malalignment. Clin Sports Med. 2017;36:119-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41:2800-2804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 270] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 7. | Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC Jr, Dabezies E, Beynnon BD. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 289] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 8. | Khan MS, Seon JK, Song EK. Risk factors for anterior cruciate ligament injury: assessment of tibial plateau anatomic variables on conventional MRI using a new combined method. Int Orthop. 2011;35:1251-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23:2846-2852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 209] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 10. | Sonnery-Cottet B, Mogos S, Thaunat M, Archbold P, Fayard JM, Freychet B, Clechet J, Chambat P. Proximal Tibial Anterior Closing Wedge Osteotomy in Repeat Revision of Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2014;42:1873-1880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 180] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 11. | Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230-2235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 292] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 12. | Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Intraoperative findings and procedures in culturally and geographically different patient and surgeon populations: an anterior cruciate ligament reconstruction registry comparison between Norway and the USA. Acta Orthop. 2012;83:577-582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Kfuri M, Lobenhoffer P. High Tibial Osteotomy for the Correction of Varus Knee Deformity. J Knee Surg. 2017;30:409-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Ferruzzi A, Buda R, Cavallo M, Timoncini A, Natali S, Giannini S. Cartilage repair procedures associated with high tibial osteotomy in varus knees: clinical results at 11 years' follow-up. Knee. 2014;21:445-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Schneider A, Gaillard R, Gunst S, Batailler C, Neyret P, Lustig S, Servien E. Combined ACL reconstruction and opening wedge high tibial osteotomy at 10-year follow-up: excellent laxity control but uncertain return to high level sport. Knee Surg Sports Traumatol Arthrosc. 2020;28:960-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | Stride D, Wang J, Horner NS, Alolabi B, Khanna V, Khan M. Indications and outcomes of simultaneous high tibial osteotomy and ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:1320-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Jin C, Song EK, Jin QH, Lee NH, Seon JK. Outcomes of simultaneous high tibial osteotomy and anterior cruciate ligament reconstruction in anterior cruciate ligament deficient knee with osteoarthritis. BMC Musculoskelet Disord. 2018;19:228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Shultz SJ, Schmitz RJ. Tibial plateau geometry influences lower extremity biomechanics during landing. Am J Sports Med. 2012;40:2029-2036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Ristić V, Maljanović MC, Pericin B, Harhaji V, Milankov M. The relationship between posterior tibial slope and anterior cruciate ligament injury. Med Pregl. 2014;67:216-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | DePhillipo NN, Kennedy MI, Dekker TJ, Aman ZS, Grantham WJ, LaPrade RF. Anterior Closing Wedge Proximal Tibial Osteotomy for Slope Correction in Failed ACL Reconstructions. Arthrosc Tech. 2019;8:e451-e457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |