Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4807
Revised: June 3, 2024
Accepted: June 13, 2024
Published online: July 26, 2024
Processing time: 80 Days and 4.7 Hours
Paragonimiasis is a typical food-borne zoonotic disease. Hosts acquire Parago
We report a case of liver paragonimiasis that was misdiagnosed as an abscess. The patient presented with fatigue and poor appetite for 2 months, and was diagnosed with liver abscess in the local hospital. After 6 months, the patient visited our hospital because of recurrent abdominal pain and was diagnosed with liver paragonimiasis based on epidemiological history, clinical presentations, and laboratory findings. He was treated with praziquantel (25 mg/kg) three times a day for 3 days; however, the symptoms still presented after treatment. He was treated with oral praziquantel and albendazole for one further course. Follow-up suggested that the treatment was effective and the symptoms improved.
The combination of albendazole and praziquantel may improve the therapeutic efficacy of paragonimiasis.
Core Tip: We report a case of paragonimiasis that was misdiagnosed as liver abscess. The patient was treated with praziq
- Citation: Zheng YQ, Guo GB, Wang MF, Zhu HZ, Zhou C, Li LH, Zhang L, Liu YQ. Paragonimiasis misdiagnosed as liver abscess: A case report. World J Clin Cases 2024; 12(21): 4807-4812
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4807.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4807
Paragonimiasis is a lung fluke disease that is prevalent mainly in Asia, Africa and South America. The morbidity in China is about 1.71%[1]. The occurrence of paragonimiasis in the liver, brain, spinal cord, subcutaneous tissue, muscle and orbi
The patient was admitted to our hospital because of recurrent wandering epigastric.
On November 25, 2021, a 55-year-old male who was admitted to our hospital because of recurrent wandering epigastric pain, with symptoms of fatigue, poor appetite and other symptoms for 6 months. The abdominal pain was located in the subxiphoid and the right epigastric region, which was paroxysmal. The nature of the pain was not clear, and the pain was aggravated by consumption of meat and relieved by exhaustion of gas.
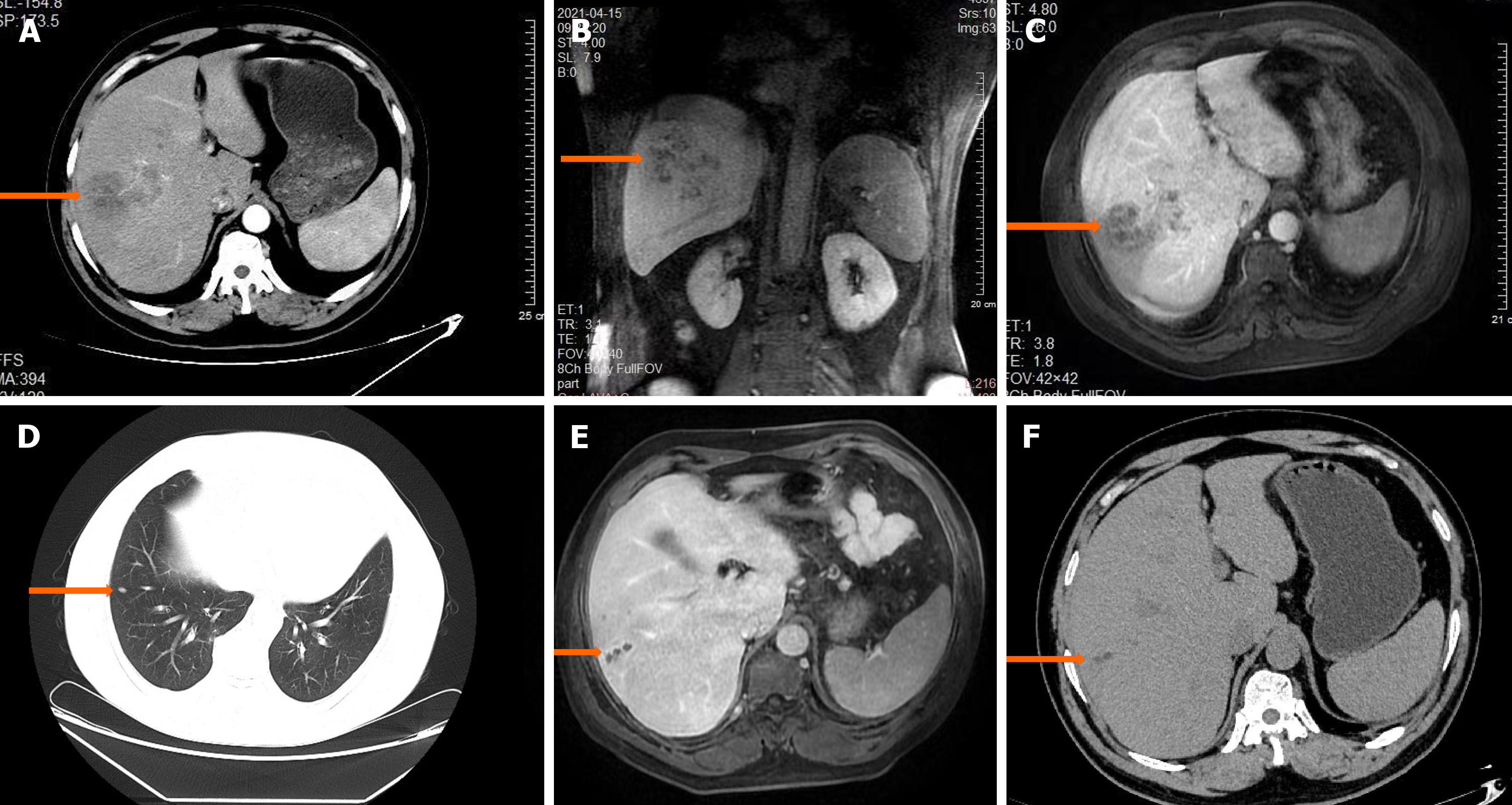
The patient had a history of hypertension and coronary heart disease but denied any other medical history. He was admitted to a local hospital on April 7, 2021, due to fatigue and poor appetite for 2 months. Physical examination showed no abnormality. Routine blood analysis in the local hospital showed an absolute leukocyte count of 10.28 × 109/L, absolute eosinophil count of 2.51 × 109/L, with a percentage of 24.40%, erythrocyte sedimentation rate (ESR) 63mm/h, γ-glutamyltransferase 93.4 U/L, alkaline phosphatase 152.7 U/L, albumin/globulin ratio 1.12. Abdominal ultrasound revealed a space-occupying lesion in the right lobe of the liver. Abdominal contrast-enhanced computed tomography (CT) showed an abscess in the right lobe of the liver (Figure 1A). Contrast-enhanced magnetic resonance imaging (MRI) showed a 6.2 cm × 4.2 cm mass with an abnormal signal in the right lobe of the liver. No enlarged lymph nodes were observed in the abdominal cavity or retroperitoneum (Figure 1B and C). The local hospital considered a diagnosis of liver abscess. Cefoperazone and sulbactam were given as anti-infective treatment for 2 weeks, and the patient was discharged after symptoms such as malaise and poor appetite improved.
The patient had no significant personal or family history.
The findings of the physical examination were within normal limits.
Laboratory analyses revealed admission tests for Mycobacterium tuberculosis IgM antibody and tuberculin were negative. Anti-extractable nuclear antigen peptide profile and anti-neutrophil cytoplasmic antibodies were normal. Routine blood analysis showed a leukocyte count of 13.89 × 109/L, absolute eosinophil count of 8.03 × 109/L, percentage of eosinophils 57.8%, and percentage of neutrophils 32.2%. Routine urinalysis showed weakly-positive proteinuria. Routine stool examination showed no abnormality. ESR was 49 mm/h. Liver function tests showed albumin 32.74 g/L, globulin 43.24 g/L, and albumin/globulin ratio 0.76. Peripheral blood cell morphology demonstrated 51% eosinophils, the rest were normal. Bone marrow biopsy showed active myeloproliferative activity with 25.5% eosinophils. Microscopic fecal analysis showed: no liver fluke, hookworm, tapeworm or other eggs.
Imaging revealed that Chest CT showed a small nodular focus in the middle lobe of the right lung (Figure 1D). Abdomi
The patient's personal history was pressed again, he reported a history of eating raw crab in childhood, so further improved the paragonimus intradermal test suggested strong positivity, which supported the diagnosis of liver paragonimiasis. Definitive clinical diagnosis of liver paragonimiasis was based on recurrent abdominal pain for 6 months, childhood history of eating raw crab, routine blood tests indicating increased eosinophils, bunch of grapes sign on liver MRI, and positive lung fluke intradermal test.
He was treated with praziquantel tablets (25 mg/kg) for 3 days, and discharged with relief of abdominal pain.
On December 27, 2021, the patient was admitted to hospital again with abdominal pain, accompanied by weakness and fatigue, and the symptoms of abdominal pain were the same as before. Admission blood tests showed a white blood cell count of 14.03 × 109/L and an absolute eosinophil value of 6.02 × 109/L. Repeated lung fluke intradermal test still sugge
In China, paragonimiasis is mainly caused by Paragonimus skrjabini and Paragonimus westermani. Adult Paragonimus parasitize human lungs, and the eggs are discharged with sputum through the mouth or digestive tract along with feces. The eggs develop into sporocysts and cercariae. The cercariae enter freshwater crayfish and crab to form metacercariae. People are infected by eating raw or undercooked freshwater crayfish or crab that contain metacercariae. Metacercariae form in the intestinal tract as juvenile worms, which travel through the intestinal tract to abdominal organs, across the diaphragm and into the lungs, where they mature to adults[4]. Pathogenicity is mainly due to the mechanical damage caused by the migration of juvenile worms, and the immunopathological response induced by their metabolites. The disease has been reported in northeastern China, Zhejiang, Sichuan and Guangdong. Similar to the epidemiological trend of other infectious diseases, the prevalence of paragonimiasis has decreased in intensity in traditionally infected areas. New emerging areas of infection continue to appear, which results in decreased alertness of medical personnel in the traditional infected areas. Personnel in the new areas of infection have insufficient knowledge of the clinical characteristics of the disease, which is the reason for the high rate of misdiagnosis. The clinical manifestations of paragonimiasis are not specific, which makes it easier to misdiagnose as liver abscess or cancer, which can lead to delayed treatment or unnecessary surgery, with serious sequelae.
Paragonimiasis be divided into thoracic-pulmonary, liver, cutaneous, cerebrospinal and mixed types. Some patients only show eosinophilia in the peripheral blood and have no obvious clinical symptoms, which is known as cryptic paragonimiasis among which the thoracic–pulmonary type is the most common. However, extrapulmonary paragonimiasis rarely involves the liver[3]. Liver paragonimiasis is clinically characterized by migration of worms and damage to the liver and patients may present with symptoms such as abdominal distension, abdominal pain, nausea, vomiting, fatigue, poor appetite, and fecal blood. The site of abdominal pain is not fixed, and ascites and liver enlargement may also occur, with characteristic imaging manifestations such as a bunch of grapes or tunnel appearance. MRI of liver paragonimiasis has the following characteristics[4-6]: (1) Foci are round, irregular, or strip-shaped, and some foci have a typical a bunch of grapes or tunnel appearance; and (2) Foci are isointense or hypointense in T1WI and hyperintense or hypo
The drug of choice for the treatment of paragonimiasis is praziquantel, and albendazole can also be used[8]. Praziquan
Paragonimiasis is a food-borne parasitic infectious disease with wide distribution and diverse clinical manifestations, which is easily misdiagnosed. On the one hand, health education should be carried out to raise public awareness of the prevention of paragonimiasis, and prevention can be achieved by not eating raw or undercooked crayfish and crab[15]. On the other hand, clinical knowledge of paragonimiasis should be strengthened, especially for liver paragonimiasis, which has a lower incidence, to improve diagnosis and treatment, reduce the rate of misdiagnosis and missed diagnosis, avoid progression of the disease, and reduce complications.
The diagnosis of paragonimiasis should be considered comprehensively. Praziquantel is the first choice for treatment, the combination of albendazole and praziquantel may improve the therapeutic efficacy of paragonimiasis. This provides a new idea for cases with poor treatment effect to praziquantel alone.
We would like to acknowledge all members of the department of General Practice and Pulmonary and Critical Care Medicine, Taihe Hospital, Hubei University of Medicine.
| 1. | Liu Q, Wei F, Liu W, Yang S, Zhang X. Paragonimiasis: an important food-borne zoonosis in China. Trends Parasitol. 2008;24:318-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | Chai JY. Paragonimiasis. Handb Clin Neurol. 2013;114:283-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Ye X, Xiong X, Cheng N, Lu J, Lin Y. Hepatic paragonimiasis: a single-center retrospective analysis of 32 cases in Mainland China. Gastroenterol Rep (Oxf). 2017;5:282-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Donato-R AO, Donato-R JC. Pulmonary, liver and cerebral paragonimiasis: An unusual clinical case in Colombia. Travel Med Infect Dis. 2022;46:102253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Yoshida A, Doanh PN, Maruyama H. Paragonimus and paragonimiasis in Asia: An update. Acta Trop. 2019;199:105074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 6. | Lu CY, Hu YJ, Chen WX. Characteristic MR and CT imaging findings of hepatobiliary paragonimiasis and their pathologic correlations. Acta Radiol. 2012;53:481-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Nagayasu E, Yoshida A, Hombu A, Horii Y, Maruyama H. Paragonimiasis in Japan: a twelve-year retrospective case review (2001-2012). Intern Med. 2015;54:179-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Hu Y, Qian J, Yang D, Zheng X. Pleuropulmonary paragonimiasis with migrated lesions cured by multiple therapies. Indian J Pathol Microbiol. 2016;59:56-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Fürst T, Keiser J, Utzinger J. Global burden of human food-borne trematodiasis: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:210-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 376] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 10. | Oh IJ, Kim YI, Chi SY, Ban HJ, Kwon YS, Kim KS, Kim YC, Kim YH, Seon HJ, Lim SC, Shin HY, Kim SO. Can pleuropulmonary paragonimiasis be cured by only the 1st set of chemotherapy? Treatment outcome and clinical features of recently developed pleuropulmonary paragonimiasis. Intern Med. 2011;50:1365-1370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Lima RM, Ferreira MA, de Jesus Ponte Carvalho TM, Dumêt Fernandes BJ, Takayanagui OM, Garcia HH, Coelho EB, Lanchote VL. Albendazole-praziquantel interaction in healthy volunteers: kinetic disposition, metabolism and enantioselectivity. Br J Clin Pharmacol. 2011;71:528-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Moreno MJ, Urrea-París MA, Casado N, Rodriguez-Caabeiro F. Praziquantel and albendazole in the combined treatment of experimental hydatid disease. Parasitol Res. 2001;87:235-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Garcia HH, Lescano AG, Gonzales I, Bustos JA, Pretell EJ, Horton J, Saavedra H, Gonzalez AE, Gilman RH; Cysticercosis Working Group in Peru. Cysticidal Efficacy of Combined Treatment With Praziquantel and Albendazole for Parenchymal Brain Cysticercosis. Clin Infect Dis. 2016;62:1375-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Petrov K, Ihongbe F, Chang M, Choudhary S, Bhatia D. Combined Albendazole and Praziquantel Therapy in an Adult Female with Neurocysticercosis and Generalized Tonic-clonic Seizures. Cureus. 2018;10:e2996. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Fischer PU, Weil GJ. North American paragonimiasis: epidemiology and diagnostic strategies. Expert Rev Anti Infect Ther. 2015;13:779-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |