Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4802
Revised: June 6, 2024
Accepted: June 17, 2024
Published online: July 26, 2024
Processing time: 68 Days and 3 Hours
Norwegian scabies (NS) is a serious parasitic skin condition. Although NS is one of the causes of erythroderma, it is frequently overlooked. Therefore, it is essential to raise awareness regarding NS presenting as erythroderma.
We present a case of NS that persisted for more than 3 years. After following nonstandard treatment, the patient’s rash worsened and gradually progressed into erythroderma. Finally, NS was diagnosed by skin microscopy and pathology.
When patients with pruritic dermatosis have high-risk factors such as prolonged bed rest and immunodeficiency, clinicians need to enhance their awareness of NS and ensure prompt diagnosis and treatment.
Core Tip: In this study, we have described an elderly patient with Norwegian scabies for over 3 years. The patient developed multiple erythema, papules, and scales throughout the body. After repeated irregular treatments, his condition worsened for 2 months, and the rash advanced to diffuse infiltrating dark erythema with keratinized papules, pustu
- Citation: Chen HJ, Lu CY, Huang GM, Tang LL. Norwegian scabies presenting as erythroderma: A case report. World J Clin Cases 2024; 12(21): 4802-4806
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4802.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4802
Scabies is a parasitic skin disease caused by human scabies mites. Norwegian scabies (NS) is one of the most severe types of scabies. It is more frequent in patients who are physically weak, have weakened immune function, and have extremely poor personal hygiene. Unlike classic scabies, it is characterized by an excessive number of mites on the skin surface, which can affect the scalp, face, back, and nail wrinkles[1]. Erythroderma is often secondary to conditions such as derma
A 74-year-old man was admitted to the intensive care unit with a 1-day history of altered consciousness.
He had a history of generalized rash observed 3 years before admission and worsened 2 months before admission. Over 3 years ago, the patient developed scattered erythema and papules all over the body, accompanied by mild pruritus. The patient had been diagnosed with eczema and scabies, and was treated topically with corticosteroids and sulfur cream. However, the rash recurred and worsened 2 months ago, leading to severe erythroderma covering more than 90% of the body surface. Erythroderma due to eczema or psoriasis was considered as the first diagnosis. Although treatments such as anti-allergy, immune regulation, and external medicines were administered to repair the skin barrier, there was no significant improvement in his condition.
His medical history included hypertension, Parkinson’s disease, and left-sided hemiparesis resulting from cerebral infarction.
We observed that two family members of the patient had a similar history of skin itching.
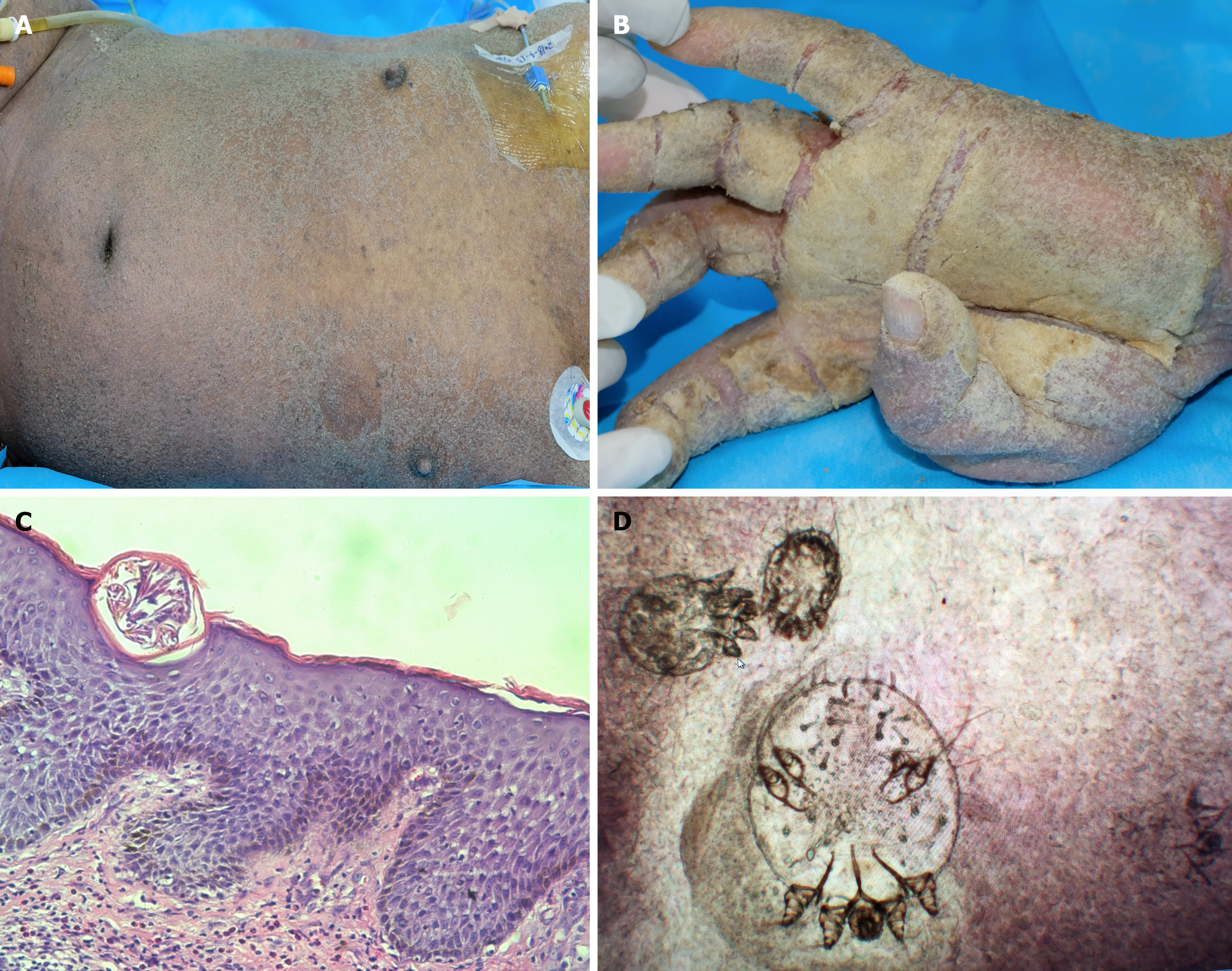
Generalized scaly erythema, papules-pustules over the whole body, and crusted hyperkeratotic lesions on the arms and hands, particularly the thick yellow scab on the palm (Figure 1A and B).
Laboratory tests revealed an increase in eosinophils. Skin biopsy of the lesion was performed, and pathological examination showed a foreign body with encapsulated structures below the cuticle. Significant eosinophil infiltration in the superficial dermis, as well as moderate lymphocyte and neutrophil infiltration was noted (Figure 1C). Direct microscopy of skin scrapings revealed live scabies mites and eggs (Figure 1D).
The occurrence of NS was confirmed.
After diagnosis, the patient was treated using 20% sulfur cream, resulting in an improvement in the rash.
Because of the patient’s primary disease and various complications, he eventually died of septic shock. Therefore, the prognosis and follow-up could not be conducted.
NS, also known as crusted scabies (CS), is a serious parasitic skin infection. The differential diagnosis of NS includes psoriasis, eczema, contact dermatitis, insect bites, seborrheic dermatitis, lichen planus, systemic infection, palmoplantar keratoderma, and cutaneous lymphoma[2]. Compared with conventional scabies, NS is typically characterized by generalized erythroderma and significant hyperkeratosis, which is easily misdiagnosed as erythrodermic psoriasis[3].
In this case, the patient had been experiencing a systemic rash for 3 years. Initially, “scabies” was considered, and the treatment provided temporary relief. However, he stayed in bed for a long time due to hemiplegia, and the rash progressed to generalized erythema, papules, pustules, scales, and scabs, and obvious thick scales and scabs could be observed at the fusion of trunk and hand and foot skin lesions. Therefore, after the first consultation in our department, the patient was misdiagnosed with eczema, psoriasis, and other skin diseases, which is similar to the previous studies. This underscores the common occurrence of misdiagnosis of NS in clinical practice. Due to the unsatisfactory treatment outcomes, a thorough review of the patient’s medical history was conducted, revealing that two family members had experienced rash and itching symptoms. This prompted the consideration of NS as a potential diagnosis. Factors for NS diagnosis are listed below: (1) The elderly patient who has been bedridden for an extended period, has multiple underlying diseases, and malnutrition. He has lived in a hot and humid place in southern China for a long time, providing favorable conditions for the parasites to thrive; (2) Two members of the patient’s family exhibit similar rash and itching symptoms; (3) The special rash all over the body; and (4) Itching, particularly at night, is prominent, and despite long-term use of anti-allergic medications and external application of glucocorticoid patches, there was no significant improvement.
The treatment of scabies typically involves the use of external medicine (chlorpyrifos, sulfur ointment, and lindane) and oral medicine (ivermectin). Although external sulfur ointment is no longer the primary treatment choice in deve
The patient’s hypoesthesia and lax treatment may have contributed to the treatment failure. Mechanical removal of mites and eggs by scratching is an effective host mechanism that can help limit their proliferation. Therefore, patients with cognitive impairment, physical disability, or neuropathy who cannot feel or interpret the itch or are unable to scratch effectively are at increased risk of developing CS[5]. Eventually, the condition progressed to erythrodermic scabies.
A previous study has revealed a significant delay in the diagnosis of NS[6]. Early identification enables appropriate management and treatment, thereby reducing the risk of infection and community-wide scabies outbreaks[7]. A delay in diagnosis and treatment results in the dissemination of the infestation with an increasing risk of sepsis and death, and scabies nosocomial outbreaks[8].
A patient with CS may host more than a million mites; therefore, scraping any affected site is highly likely to yield a definitive diagnosis[4]. As a result, the challenge of diagnosis is not the lack of evidence, but confirmation regarding the occurrence of NS. Awareness of this rare form of scabies should be raised among dermatologists, and when patients present with atypical psoriasis, atypical morbiliform eruptions, or erythroderma, NS should be considered[6].
Dermatologists should enhance their understanding of NS, perform thorough medical history inquiries, combine existing advanced diagnostic and treatment techniques for pathogen testing, clarify the diagnosis, and isolate and treat as early as possible to achieve early and precise treatment and effectively prevent epidemics within families or medical facilities.
| 1. | Bassi A, Arunachalam M, Galeone M, Scarfì F, Difonzo EM. Norwegian scabies. QJM. 2014;107:225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Siegfried EC, Hebert AA. Diagnosis of Atopic Dermatitis: Mimics, Overlaps, and Complications. J Clin Med. 2015;4:884-917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Hengge UR, Currie BJ, Jäger G, Lupi O, Schwartz RA. Scabies: a ubiquitous neglected skin disease. Lancet Infect Dis. 2006;6:769-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 211] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 4. | Fonseca V, Price HN, Jeffries M, Alder SL, Hansen RC. Crusted scabies misdiagnosed as erythrodermic psoriasis in a 3-year-old girl with down syndrome. Pediatr Dermatol. 2014;31:753-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Lee K, Heresi G, Al Hammoud R. Norwegian Scabies in a Patient with Down Syndrome. J Pediatr. 2019;209:253-253.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Yélamos O, Mir-Bonafé JF, López-Ferrer A, Garcia-Muret MP, Alegre M, Puig L. Crusted (Norwegian) scabies: an under-recognized infestation characterized by an atypical presentation and delayed diagnosis. J Eur Acad Dermatol Venereol. 2016;30:483-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Matsuura H, Senoo A, Saito M, Fujimoto Y. Norwegian scabies. Cleve Clin J Med. 2019;86:163-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Del Borgo C, Belvisi V, Tieghi T, Mastroianni CM. Atypical presentation of crusted (Norwegian) scabies. Infection. 2015;43:623-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |