Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4794
Revised: May 14, 2024
Accepted: May 27, 2024
Published online: July 26, 2024
Processing time: 86 Days and 5.4 Hours
Ectopic thyroid at the base of the tongue is a rare congenital condition, and it is even rarer to have clinical symptoms and require surgical intervention. This disease is easily misdiagnosed preoperatively. This article reports the diagnosis, surgical treatment, and follow-up of a case of lingual thyroid.
The patient was a 54-year-old woman who presented with laryngeal foreign body sensation and dysphagia for 20 d. The lingual thyroid was considered for general examination, and surgery was performed to transpose the lingual thyroid to the right submaxillary region. Pathological analysis confirmed thyroid tissue. The patient experienced complete remission after surgery, but developed hypo
We report a rare case of lingual thyroid with marked laryngeal foreign body sen
Core Tip: Lingual thyroid with clinical symptoms is rare, and preoperative examination and diagnosis are important. Translocation of lingual thyroid to the submandibular region via the submandibular approach with lateral pharyngotomy can alleviate the pharyngeal symptoms, and this is a surgical approach that can effectively preserve the thyroid function. Post
- Citation: Yin YT, Gui C. Transposition of the lingual thyroid gland to the submandibular region through a submandibular approach: A case report. World J Clin Cases 2024; 12(21): 4794-4801
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4794.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4794
Ectopic thyroid is a rare congenital disorder in which thyroid tissue is located outside the typical location of the thyroid gland in the neck (in front of the second to fourth tracheal rings), with an overall prevalence of 1 in 100000 to 300000 persons[1]. The prevalence is 4- to 8-times higher in females than in males[2]. Ectopic thyroid tissue can be located anywhere along the descending path of the embryo, but 90% of cases of ectopic thyroid tissue are found in the tongue, which is called lingual thyroid tissue[3]. Due to the rarity of lingual thyroid, there is no consensus on its treatment, and options include levothyroxine suppression, radioactive iodine, ablative surgery, lingual thyroidectomy, and lingual thyroid translocation surgery.
Treatment depends on the size, presence or absence of symptoms, age, sex, thyroid function, and complex factors such as ulceration, bleeding, or malignancy[4]. The lingual thyroid may be asymptomatic, or symptoms such as dysphagia, foreign body sensation in the throat, dyspnea, and sleep apnea may occur due to the occupying effect of the lingual thyroid. Asymptomatic and normal thyroid function patients do not require any treatment[5]. Surgical indications include dyspnea, dysphonia, dysphagia, suspected malignancy, hormonal disturbances, failure to respond to medication, or bleeding.
We describe a case of lingual thyroid in a middle-aged woman. She was admitted to the hospital with a foreign body sensation in the larynx and dysphagia, and after a thorough examination a preliminary diagnosis of lingual thyroid was made, and translocation of the lingual thyroid to the submaxillary region was accomplished by lateral pharyngotomy through a submaxillary approach, and the symptoms were completely relieved after the operation.
A 54-year-old female patient presented to the hospital with a 20-d history of throat foreign body sensation and dysphagia.
The patient developed intermittent cough 1 mo ago, and laryngeal foreign body sensation and dysphagia 20 d prior. The patient's symptoms gradually worsened, and she developed sleep apnea syndrome. Computed tomography (CT) and laryngoscopy revealed ectopic thyroid gland at the base of the tongue. The patient had not been treated prior to hospitalization.
The patient had hypertension for 2 years and was controlled by oral lilopril hydrochlorothiazide tablets.
There was no personal or family history of ectopic thyroid or any other disease history.
Physical examination showed a palpable mass at the right base of the tongue with smooth surface mucosa and associated tenderness, no palpable enlarged lymph nodes in the neck, and no palpable mass in the normal thyroid region.
The results of routine complete blood count, kidney function, and liver function tests were normal. Thyroid function tests were normal.
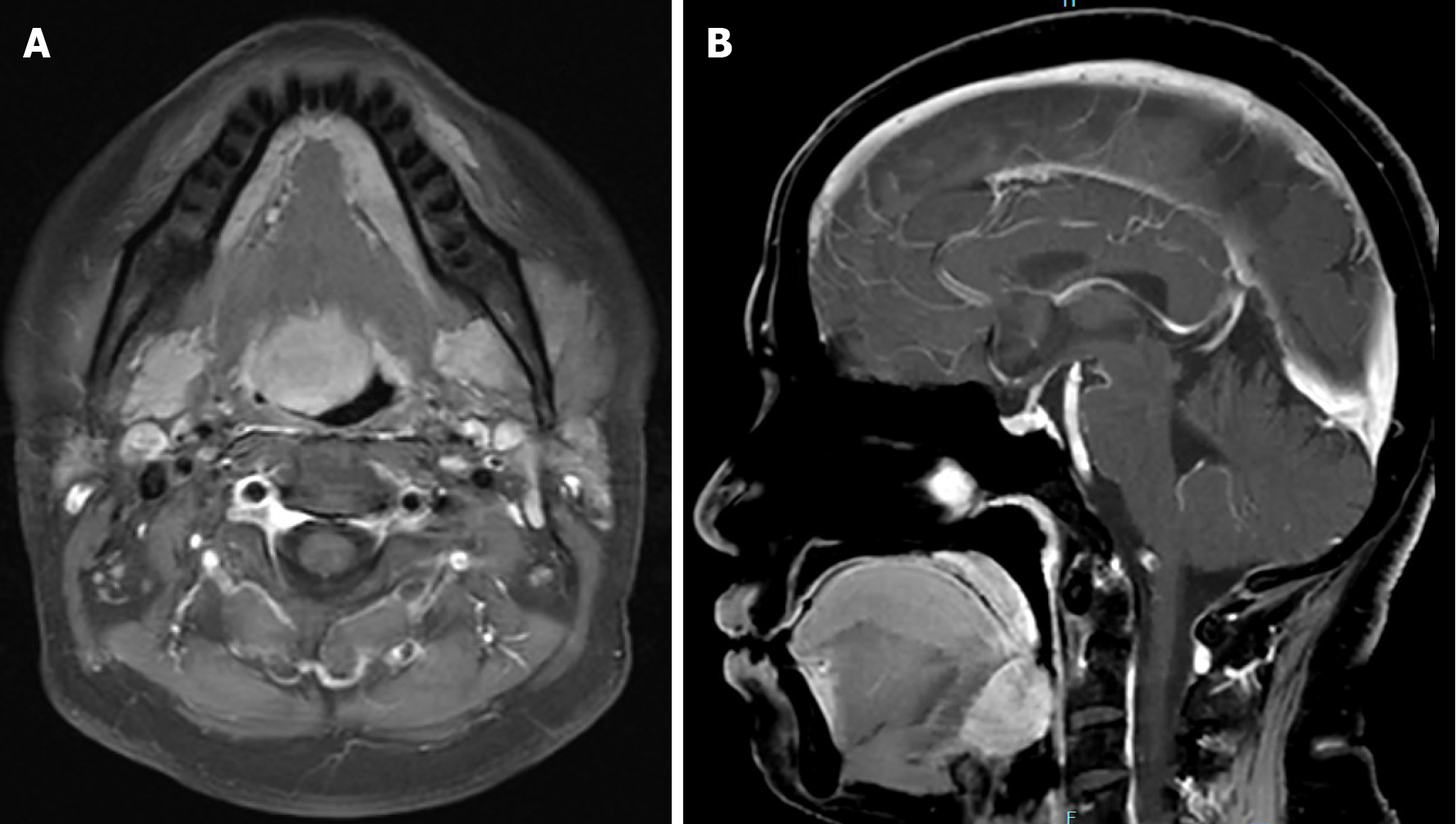
Oral and maxillofacial magnetic resonance imaging (MRI) showed a right-sided nodule at the base of the tongue (size: 2.3 cm × 2.0 cm; Figure 1). Electron nasolaryngoscopy showed a submucosal bulge at the base of the tongue (size: 4 cm × 3 cm; Figure 2), and ultrasonography of the neck showed no thyroid echoes in the normal thyroid region (Figure 3). Tc-99 static imaging showed thyroid tissue visible at the base of the tongue, with no radiological distribution in the normal thyroid location (Figure 4).
After careful consideration of the patient's history, physical examination, laboratory tests, and imaging findings, we made a preliminary diagnosis of lingual thyroid.
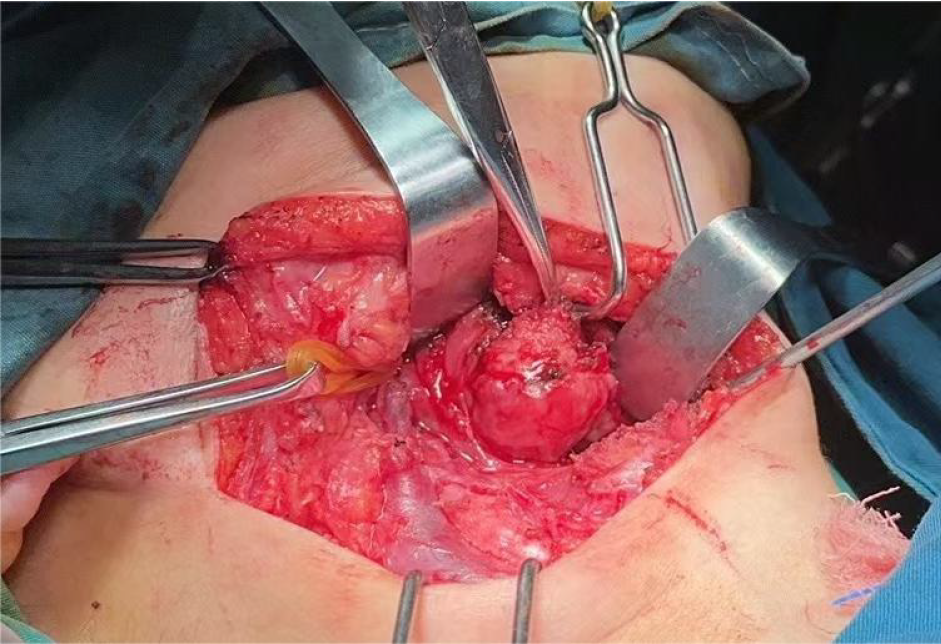
After a thorough preoperative examination and confirmation that there were no contraindications to surgery, the patient underwent lingual thyroid translocation, on October 8, 2023. Intraoperative examination revealed a reddish, bulbous, well-circumscribed mass at the root of the tongue (Figure 5). A small amount of tissue was cut and sent for frozen biopsy to confirm the diagnosis of normal thyroid tissue.
Via the right submandibular approach, the right submandibular gland was excised, the right supraglottic muscle group and the right hyoid bone were dissected so as to enter the laryngeal cavity, and the lingual thyroid was freed from the root of the tongue and then flipped and placed in the right submandibular triangle.
Step one: Tracheotomy was performed under local anesthesia, followed by general anesthesia.
Step two: A long curved incision was made along the right submandibular region, the skin and the vastus cervicis muscle were incised to expose the facial artery and identify the mandibular marginal branch of the facial nerve, the right submandibular gland envelope was loosened and the right submandibular gland was completely resected, revealing the diastasis muscle and sublingual nerve.
Step three: We exposed the right superior thyroid artery, right superior laryngeal nerve and right lingual artery, freed the right lingual artery, dissected the right suprahyoid muscle group and right hyoid bone, accessing to the laryngeal cavity by incising the anterior epiglottic space.
Step four: Entering the laryngeal cavity revealed an lingual thyroid at the base of the right tongue, and the vascularized tip of the right lingual thyroid gland was preserved, the lingual thyroid gland was detached from the root of the tongue, and thyroid tissue was freed with a vascularized tip. It was then turned over and placed in the right submaxillary triangle.
Step five: The mucosa of the laryngeal cavity was sutured, followed by suturing of the right upper and lower hyoid muscle groups, and the incision was closed in layers.
The anterior epiglottic space was incised, the laryngeal cavity was entered, and the lingual thyroid was exposed, the right vascular pedicle of the lingual thyroid was preserved, and the lingual thyroid was detached from the root of the tongue in three directions, along the superior, inferior, and left margins, and the thyroid tissue was freed with a vascular pedicle, which was then flipped and placed in the right submandibular triangle.
First, we completed tracheotomy to facilitate intraoperative and postoperative management of maintaining airway patency. Next, we removed the right submandibular gland to make room for the lingual thyroid transposition. And we protected the mandibular marginal branch of the facial nerve to avoid facial paralysis. The lingual artery was preserved and appropriately freed, and the right vascular pedicle of the lingual thyroid was protected to preserve the blood supply to the thyroid tissue when isolating the lingual thyroid.
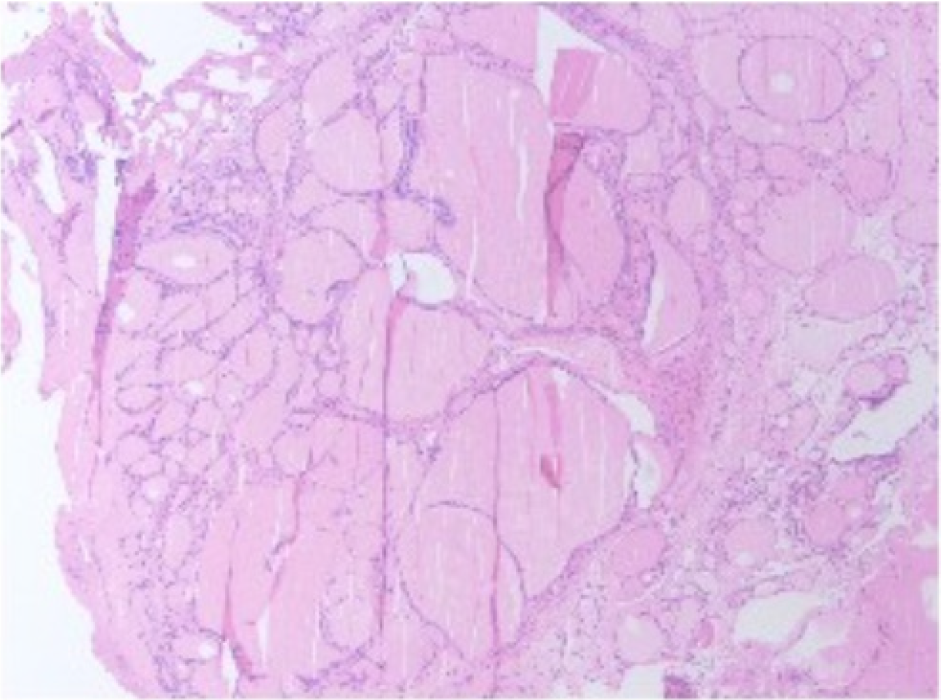
Routine pathological examination in our hospital showed well-differentiated thyroid tissue (Figure 6). The symptoms of foreign body sensation and dysphagia in the throat were completely relieved after surgery. Tracheal and gastric tubes were removed 1 wk after surgery, and wound stitches were removed 10 d after surgery. The wound healed well. At the 3 mo follow-up, the patient had complete remission of symptoms, but thyroid function tests showed hypothyroidism requiring oral thyroid hormone tablet replacement therapy.
Thyroid function test results were thyroid-stimulating hormone (TSH) in the 1st month after surgery was > 100 uIU/mL (reference value 0.27-4.2 uIU/mL), free triiodothyronine (FT3) < 0.6 pmol/L (reference value 3.1-6.8 pmol/L), and free thyroxine (FT4) 1.32 pmol/L (reference value 12-22 pmol/L). We recommended that the patient take oral thyroid hormone tablets 125 μg per day.
In the 2nd postoperative month, TSH was 1.95 uIU/mL, FT3 was 6.45 pmol/L, and FT4 was 26.41 pmol/L. We reco
In the 3rd month after surgery, TSH was 0.0442 uIU/mL, FT3 was 7.80 pmol/L, and FT4 was 28.5 pmol/L, and oral thyroid hormone tablets 75 μg per day were administered.
In the 4th postoperative month, TSH was 0.0399 uIU/mL, FT3 was 4.43 pmol/L, and FT4 was 21.4 pmol/L, and oral thyroid hormone tablets 50 μg per day were administered.
Thyroid function test results indicated that the patient's thyroid function gradually recovered, with a decreasing need for exogenous thyroid hormone medication. Recovery of the patient's thyroid function indicates survival of the trans
Ninety percent of ectopic thyroid glands are located at the base of the tongue, and only 1% are lingual thyroid cancers[6]. Lingual thyroid is an embryological abnormality that occurs during migration of the thyroid gland[7]. The treatment plan is based on the patient's symptoms and complaints. Lingual thyroid is usually asymptomatic but may cause localized symptoms such as dysphagia, dysphonia and upper airway obstruction, due to the occupying effect. Dysphagia and dys
Differential diagnosis of tongue thyroid includes tongue cancer, inflammatory lesions, thyroglossal cyst, hemangioma, and schwannoma. Detailed oropharyngeal and neck examinations are important for preoperative diagnosis and treatment, such as MRI of the oropharynx, ultrasound scanning of the neck, laryngoscopy, technetium scanning tests, and thyroid function tests. Ectopic thyroid usually has no specific clinical symptoms, and an appropriate and thorough workup at the time of initial diagnosis is key to avoiding misdiagnosis[9]. Lingual thyroid is primarily determined initially by complaint, physical examination and imaging. Diagnostic tests of the lingual thyroid include CT, MRI, technetium scanning and fine needle aspiration[10]. Uptake of radiolabeled technetium by the thyroid gland at the base of the tongue is diagnostic of lingual thyroid[11]. Pathology is the gold standard for diagnosis. In our patients, ultrasonography, Tc-99, MRI, and laryngoscopy provided important diagnostic information, where no thyroid tissue was found in the normal thyroid area. Therefore, it was considered to be lingual thyroid.
Surgery is recommended for malignant lesions or when symptoms are severe and seriously affect daily life. In more than 70% of patients with symptomatic lingual thyroid tissue, ectopic glands are their only functional thyroid tissue[12]. In the absence of a cervical thyroid gland, total removal of functional lingual thyroid tissue would result in hypothy
Various approaches have been reported regarding surgery of the lingual thyroid gland. The choice of surgical approach depends on the location and size of the tumor as well as the experience of the surgeon. Symptomatic lingual thyroid can be removed by lateral or midline transcervical approach, transoral resection or robotic surgery[14]. Bao et al[14] reported the transposition of lingual thyroid tissue to the submandibular region by means of lateral pharyngotomy. Wu et al[15] accomplished lingual thyroid transposition using a transoral approach in two cases. Surgical access and extent must be determined by the size and location of the lesion, but total resection is recommended when feasible[16]. The above reported surgical methods have achieved certain therapeutic effects. Some patients may not need long-term oral thyroid hormone replacement therapy. However, robotic surgery requires a high level of equipment, and robotic instruments are not yet fully popularized, so many hospitals are unable to perform robotic surgery. The transoral approach is cosmetically effective; however, this approach provides poor exposure of large masses, and in addition, intraoperative bleeding is sometimes difficult to control. Mandibulotomy and tongue splitting appear to be more damaging to the tissue.
We present a patient with a normal functioning lingual thyroid, which is the patient's only functioning thyroid gland, and therefore, a vascular-preserving transfer procedure may be more appropriate for the patient. The surgical approach we used addressed the patient's dysphagia and pharyngeal foreign body sensation while attempting to preserve the function of the thyroid tissue. The major disadvantages of this approach include aesthetic neck scarring and the need for thyroid hormone replacement therapy due to hypothyroidism resulting from inadequate blood supply to the thyroid gland.
Transmaxillary lateral pharyngotomy allows adequate exposure of the ectopic thyroid gland at the base of the tongue, good visualization reduces the risk of cranial nerve injury and promotes effective hemostasis, and the scar is located submandibularly in a hidden location with less aesthetic imaging. This approach provides good visualization, easy control of bleeding, and a large surgical maneuvering space, and is particularly suitable for surgery of large masses at the base of the tongue. The right submandibular gland is removed to make room for lingual thyroid transposition and the submandibular region does not look bloated. The submandibular region was chosen as the new site for the lingual thyroid. The superficial location allows direct palpation of the transplanted thyroid tissue, which allows timely detection of thyroid abnormalities.
Postoperatively, the patient's tongue functioned normally and all symptoms were relieved, and surgical transposition of the lingual thyroid to the submandibular region with intact vascular supply offers a promising approach to treating this abnormality. Thyroid function was rechecked and drug dosage was adjusted every month after the operation. As thyroid function gradually recovered, the dosage of oral thyroid hormone tablets was gradually reduced.
We reported that a 54-year-old female patient diagnosed with lingual thyroid underwent lingual thyroid transposition via the submandibular approach with complete relief of laryngeal foreign body sensation and dysphagia postoperatively. The patient underwent surgery for diagnosis and indications. At 6 mo postoperatively, the complaints have completely resolved with no signs of recurrence, although hypothyroidism developed early after surgery and required thyroid hormone replacement therapy. Patient’s demand for exogenous thyroid hormone medication was tapering as thyroid function gradually recovered. Although this is a rare case, knowledge of the diagnosis and treatment is necessary. Therefore, the success of this procedure may serve as a reference for the treatment of cases of lingual ectopic thyroid.
| 1. | Noussios G, Anagnostis P, Goulis DG, Lappas D, Natsis K. Ectopic thyroid tissue: anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol. 2011;165:375-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 224] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 2. | Rahbar R, Yoon MJ, Connolly LP, Robson CD, Vargas SO, McGill TJ, Healy GB. Lingual thyroid in children: a rare clinical entity. Laryngoscope. 2008;118:1174-1179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Chiu TT, Su CY, Hwang CF, Chien CY, Eng HL. Massive bleeding from an ectopic lingual thyroid follicular adenoma during pregnancy. Am J Otolaryngol. 2002;23:185-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Arancibia P, Veliz J, Barria M, Pineda G. Lingual thyroid: report of three cases. Thyroid. 1998;8:1055-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Prisman E, Patsias A, Genden EM. Transoral robotic excision of ectopic lingual thyroid: Case series and literature review. Head Neck. 2015;37:E88-E91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Toso A, Colombani F, Averono G, Aluffi P, Pia F. Lingual thyroid causing dysphagia and dyspnoea. Case reports and review of the literature. Acta Otorhinolaryngol Ital. 2009;29:213-217. [PubMed] |
| 7. | Massine RE, Durning SJ, Koroscil TM. Lingual thyroid carcinoma: a case report and review of the literature. Thyroid. 2001;11:1191-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Gallo A, Leonetti F, Torri E, Manciocco V, Simonelli M, DeVincentiis M. Ectopic lingual thyroid as unusual cause of severe dysphagia. Dysphagia. 2001;16:220-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Gao M, He Q, Li L, Ji F, Ding Y, Sun Q, Qiu X. The clinicopathological features, treatment outcomes and follow-up results of 47 ectopic thyroid gland cases: a single-center retrospective study. Front Endocrinol (Lausanne). 2023;14:1278734. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Castro PH, Volpato LE, Tramujas J, Borges AH. Ectopic Thyroid at the Base of the Tongue of a Young Patient. Case Rep Dent. 2016;2016:9174970. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Williams JD, Sclafani AP, Slupchinskij O, Douge C. Evaluation and management of the lingual thyroid gland. Ann Otol Rhinol Laryngol. 1996;105:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 57] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Danner C, Bodenner D, Breau R. Lingual thyroid: iodine 131: a viable treatment modality revisited. Am J Otolaryngol. 2001;22:276-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Nisa L, Morrison S, Levi E. Airway management in patients with lingual thyroid: a case report and review of the literature. Eur Arch Otorhinolaryngol. 2022;279:3289-3295. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Bao T, Wang H, Wei D, Yu D. Transposition of a lingual thyroid to the submandibular space using a modified technique. J Laryngol Otol. 2012;126:1287-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Wu ZX, Zheng LW, Dong YJ, Li ZB, Zhang WF, Zhao YF. Modified approach for lingual thyroid transposition: report of two cases. Thyroid. 2008;18:465-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Sauer AB, Dowling EM, Bauman MMJ, Moore EJ, Carlson ML, Van Abel KM. Does surgical management still play a role in the management of ectopic lingual thyroid: Institutional experience and systematic review of the literature. Am J Otolaryngol. 2022;43:103461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |