Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4789
Revised: May 21, 2024
Accepted: June 11, 2024
Published online: July 26, 2024
Processing time: 86 Days and 4.8 Hours
Peritoneal dialysis (PD) is an important renal replacement therapy in patients with end-stage renal disease. PD catheters remain the lifeline for patients under
The PD catheter spontaneously dislodged in a patient undergoing PD during regular fluid exchange without pain. Abdominal computed tomography showed a tunnel infection. A double-cuff straight Tenckhoff catheter had been inserted using the Seldinger technique. Before this incident, the patient had a history of tunnel infections. We speculate that recurrent tunnel infections and catheter insertion using the Seldinger technique may have led to catheter dislodgement.
The present case suggests that clinicians should more rigorously assess the persistence of catheter-related infections concerning the potential complications arising from catheter dislodgement associated with the Seldinger technique.
Core Tip: This study reports a unique case of spontaneous dislodgement of a peritoneal dialysis catheter, probably attributed to recurrent tunnel infections and the Seldinger insertion technique. This highlights the necessity for rigorous assessment of catheter-related infections to prevent the severe complication of catheter dislodgement. This case suggests that complications may arise from catheter placement using the Seldinger technique.
- Citation: Wu RY, Tan Y, Li H, Zou YR, Chen XL, Chen J. Spontaneous dislodgment of a peritoneal dialysis catheter inserted using the Seldinger technique: A case report. World J Clin Cases 2024; 12(21): 4789-4793
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4789.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4789
Peritoneal dialysis (PD) is an important renal replacement therapy that offers patients with end-stage renal disease an alternative to hemodialysis and provides greater flexibility and autonomy. PD catheters remain the lifeline for patients undergoing PD. The catheter technique survival rate is considered a core domain in reports of PD outcomes, as important as the patient survival rate and cardiovascular disease[1]. Catheter displacement and obstruction are common mechanical complications. Few reports have described PD catheter extrusion with a superficial cuff due to weight loss or infection[2,3] rather than the entire catheter. We report a rare case of spontaneous dislodgement of a PD catheter during therapy.
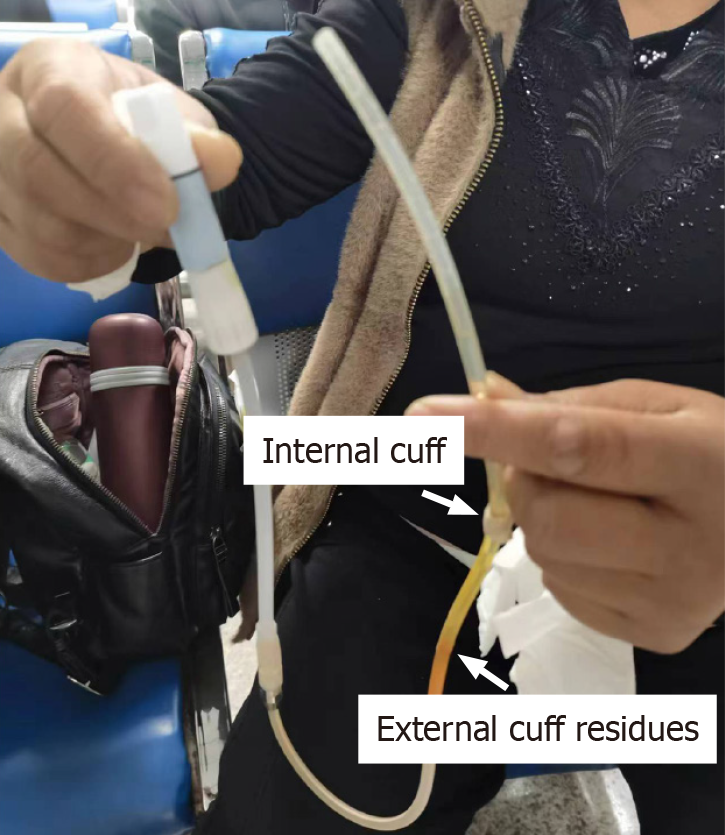
A 54-year-old woman with end-stage renal disease undergoing continuous ambulatory PD for five years reported spontaneous dislodgement of the PD catheter without pain during fluid exchange (Figure 1).
A double-cuff straight Tenckhoff catheter had been placed using the Seldinger technique.
The patient reported a tunnel infection with a negative smear culture four months after catheter insertion. The patient was treated with amoxicillin-clavulanic acid for two weeks. However, she did not undergo scheduled follow-up tunnel ultrasonography. Thereafter, she had a grayish-white discharge, oozing intermittently from the exit site, but no other symptoms. The patient did not receive additional antibiotics. Three months prior, she experienced peritonitis caused by Actinotignum schaalii. The peritonitis resolved after two weeks of benzathine, penicillin, and amikacin treatment without tunnel infection symptoms.
The patient has no significant personal or family history.
No skin dilatation or bleeding was observed at the exit site. No tenderness was observed in the tunnel or the abdominal area.
Laboratory test results revealed a white blood cell count and hemoglobin level of 7.12 × 109/L and 100.0 g/L, respectively. The levels of serum creatine, albumin, calcium, phosphate and intact parathyroid hormone were 1132.2 μmol/L, 32.0 g/L, 2.18 mmol/L, 2.16 mmol/L, and 311 pg/mL, respectively. Hypersensitive C-reactive protein levels were normal. The PD prescription contained a total volume of 8 L of 1.5% fluid. A peritoneal equilibration test revealed a high-average status.
Abdominal computed tomography (CT) after the catheter dislodgment revealed a tunnel infection involving the anterior sheath of the right rectus abdominis muscle (Figure 2). We retraced the patient's abdominal CT scan from one year previously and conducted a three-dimensional reconstruction. The catheter's measured length within the cavity was only 11.5 cm (the normal distance from the inner cuff to the catheter tip is 15.0 cm), indicating that the catheter had partially detached from the abdominal cavity (Figure 3).
PD catheter dislodgment.
Antimicrobial treatment with piperacillin sodium and tazobactam sodium was administered for two weeks.
PD was resumed with a new catheter on the left side of the abdomen.
To the best of our knowledge, only a few instances of complete PD catheter dislodgement have been reported. We suggest several possible reasons for the catheter spontaneously dislodging without an external force or pulling in this patient.
First, a recurrent tunnel infection was the main reason for catheter failure. As a result, the catheter lost its external cuff after the Dacron was encapsulated in the necrotic tissue and expelled from the body. Inflammation caused edema in the fibrous sheath tissue surrounding the catheter tunnel. When the tunnel infection extended to the rectus muscle, the pathway became dilated within the rectus sheath, providing space for the free movement of the catheter. Actinotignum schaalii is a rare pathogen that causes peritonitis, with only nine cases reported in the literature to date[4]. As the sym
Second, the placement of the PD catheter using the Seldinger technique may be a possible reason for catheter dislodgment. Because of the small incision, the anterior sheath of the rectus abdominis does not require sutures, and fixing the inner cuff to the peritoneum is not feasible. The intact inner cuff of this catheter demonstrates that it did not adhere to the surrounding tissues. During catheter tunnel construction and the early stages of tissue recovery, the inner cuff may completely or partially dislodge from the anterior sheath of the rectus abdominis. Interrupted sutures are required to close the anterior sheath around the catheter and ensure the position of the inner cuff in the rectus abdominis[6].
In conclusion, the spontaneous dislodgment of the PD catheter highlights the importance of thorough treatment of catheter-related infections and presents potential complications associated with catheter placement using the Seldinger technique.
The authors acknowledge the effort of the PD team in Sichuan Provincial People’s Hospital.
| 1. | Manera KE, Johnson DW, Craig JC, Shen JI, Gutman T, Cho Y, Wang AY, Brown EA, Brunier G, Dong J, Dunning T, Mehrotra R, Naicker S, Pecoits-Filho R, Perl J, Wilkie M, Tong A; SONG-PD Workshop Investigators. Establishing a Core Outcome Set for Peritoneal Dialysis: Report of the SONG-PD (Standardized Outcomes in Nephrology-Peritoneal Dialysis) Consensus Workshop. Am J Kidney Dis. 2020;75:404-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 128] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 2. | Ganapathy AS, Powell MS, Pirkle JL. Extrusion of both Superficial and Deep Cuffs of a Functional Double-Cuff Peritoneal Dialysis Catheter after Significant Weight Loss. Case Rep Nephrol Dial. 2021;11:190-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Koratala A, Casey MJ, Kazory A. Catheter Cuff Extrusion Following Exit-Site Infection in an Immunosuppressed Patient: One Case and Two Lessons. Blood Purif. 2018;45:343-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Levine MT. Peritoneal dialysis catheter-associated polymicrobial infection including Actinomyces neuii: Case report and brief literature review. Anaerobe. 2022;76:102602. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Chow KM, Li PK, Cho Y, Abu-Alfa A, Bavanandan S, Brown EA, Cullis B, Edwards D, Ethier I, Hurst H, Ito Y, de Moraes TP, Morelle J, Runnegar N, Saxena A, So SW, Tian N, Johnson DW. ISPD Catheter-related Infection Recommendations: 2023 Update. Perit Dial Int. 2023;43:201-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 58] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 6. | Zou Y, Ma Y, Chao W, Zhou H, Zong Y, Yang M. Assessment of complications and short-term outcomes of percutaneous peritoneal dialysis catheter insertion by conventional or modified Seldinger technique. Ren Fail. 2021;43:919-925. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |