Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4777
Revised: May 11, 2024
Accepted: June 20, 2024
Published online: July 26, 2024
Processing time: 84 Days and 0.5 Hours
Almost all cases of cervical cancer can be attributed to human papillomavirus (HPV) infection. The loop electrosurgical excision procedure (LEEP) is widely used to treat HPV-mediated disease; thus, cervical cancer is highly preventable. However, LEEP does not necessarily clear HPV rapidly and may affect the accuracy of the results of ThinPrep cytology test (TCT) and cervical biopsy due to the formation of cervical scars.
A 40-year-old woman underwent LEEP for cervical intraepithelial neoplasia grade 1 approximately 10 years ago. Subsequent standard cervical cancer screening suggested persistent HPV-52 infection, but TCT results were negative. Cervical biopsy under colposcopy was performed thrice over a 10-year period, yielding negative pathology results. She developed abnormal vaginal bleeding after sexual activity, persisting for approximately 1 year, and underwent hysteroscopy in our hospital. Histopathologic evaluation confirmed adenocarcinoma in situ of the uterine cervix.
Patients with long-term persistent, high-risk HPV infection and negative pa
Core Tip: The loop electrosurgical excision procedure (LEEP) is widely used to treat human papillomavirus (HPV)-mediated disease; thus, cervical cancer is highly preventable. However, LEEP does not necessarily clear HPV infection rapidly, and patients with persistent HPV infection after LEEP are at risk of cervical cancer. The formation of cervical scars after LEEP may affect the accuracy of ThinPrep cytology test and cervical biopsy results; thus, hysteroscopic resection of cervical canal tissue is recommended as a supplement to cervical biopsy because it helps define the lesion site and may yield a pathologic diagnosis.
- Citation: Li H, Mei SS, Mao PY, Wang XY, Yang HD. Hysteroscopic cervical biopsy for women with persistent human papillomavirus infection after loop electrosurgical excision procedure: A case report. World J Clin Cases 2024; 12(21): 4777-4782
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4777.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4777
Cervical cancer is the third most common malignancy in women worldwide. Almost all cases of cervical cancer can be attributed to human papillomavirus (HPV) infection[1]. With ongoing improvement in screening methods, the detection rates of premalignant cervical lesions have increased each year. The cervical loop electrosurgical excision procedure (LEEP) has become the classic treatment protocol for preinvasive HPV-mediated disease. HPV detection using the ThinPrep cytology test (TCT) and colposcopic cervical biopsy have become the primary follow-up approaches after LEEP[2]. However, these tests have led to new challenges; in particular, cervical scars may form after LEEP, which can cause partially or wholly invisible transformation areas in the squamocolumnar junction, thereby affecting the results of TCT and colposcopy.
Herein, we report a case of HPV infection that persisted after LEEP. Multiple TCT and colposcopic cervical biopsies yielded negative results. Through hysteroscopic exploratory diagnostic scraping, adenocarcinoma in situ of the uterine cervix was finally confirmed.
A 40-year-old woman presented to the gynecological department of our hospital with long-term persistent HPV infection but negative pathologic results of cervical biopsy after LEEP.
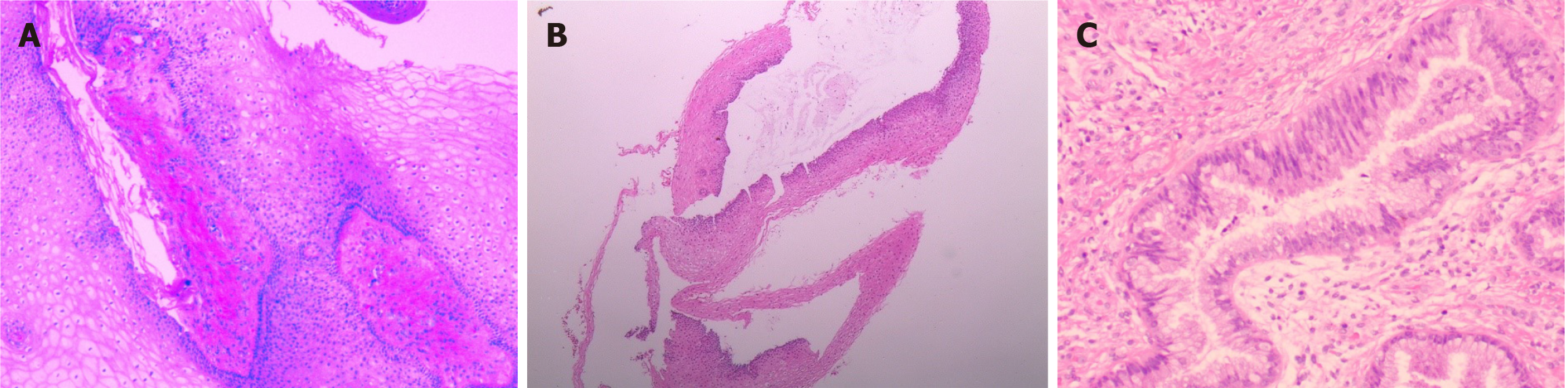
She had HPV-52 infection for > 10 years. In 2013, she underwent LEEP for HPV-52–induced cervical intraepithelial neoplasia grade 1 (CIN 1; Figure 1A). Subsequent standard cervical cancer screening suggested persistent HPV-52 infection, but TCT results were negative. In July 2015 and May 2019, she underwent cervical biopsy under colposcopy, which yielded negative histopathologic results. Her menstrual cycle was regular with 28-day intervals. Since 2022, she developed abnormal vaginal bleeding after sexual activity. Gynecological examinations revealed that the cervix was smooth after LEEP, and uterine ultrasonography indicated normal endometrial thickness. Short-acting contraceptives did not alleviate the bleeding. In May 2023, a third cervical biopsy and scratching of the cervical canal under colposcopy were performed, which also yielded negative pathology results (Figure 1B). In August 2023, she visited our outpatient department with persistent HPV-52 infection, negative TCT findings, and abnormal vaginal bleeding after sexual activity.
The patient had no notable medical history.
The patient had a no family history.
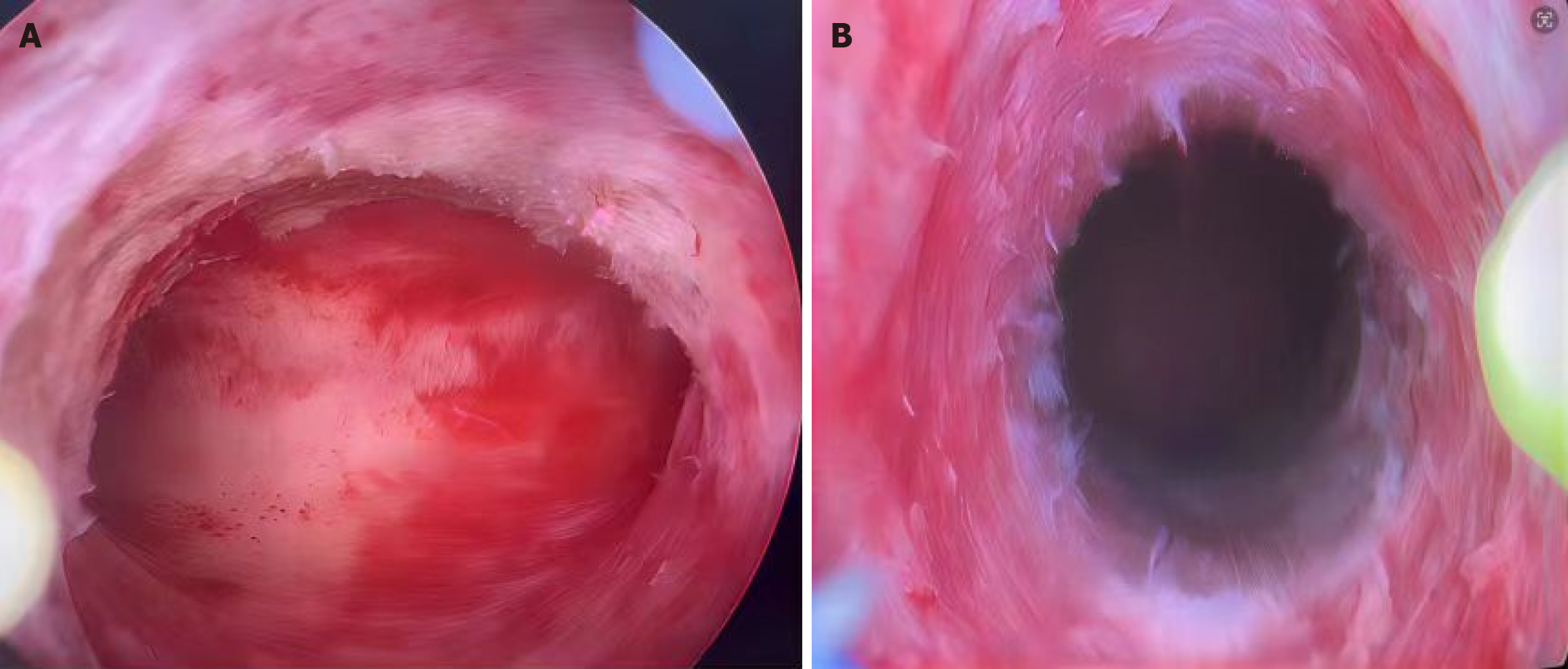
During gynecological examination, cotton swabs were blood stained after insertion into the cervical canal, although the cervical surface was smooth without any blood stain.
Squamous cell carcinoma antigen testing yielded negative results.
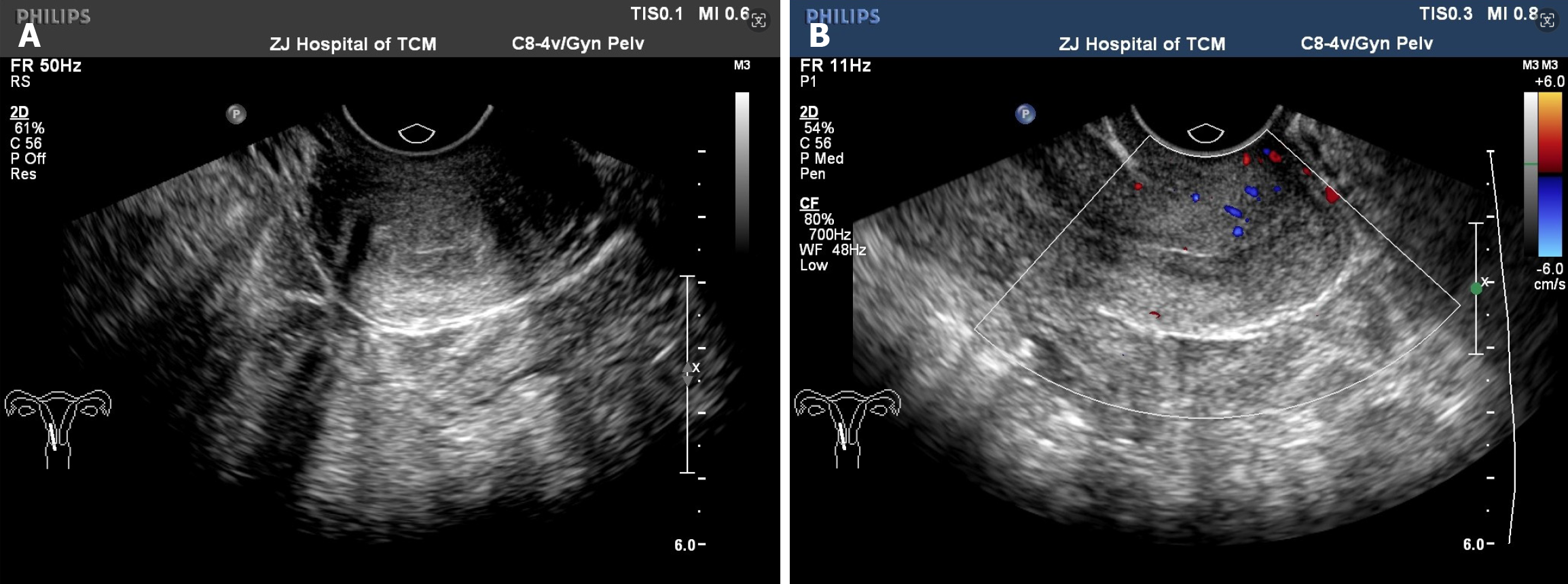
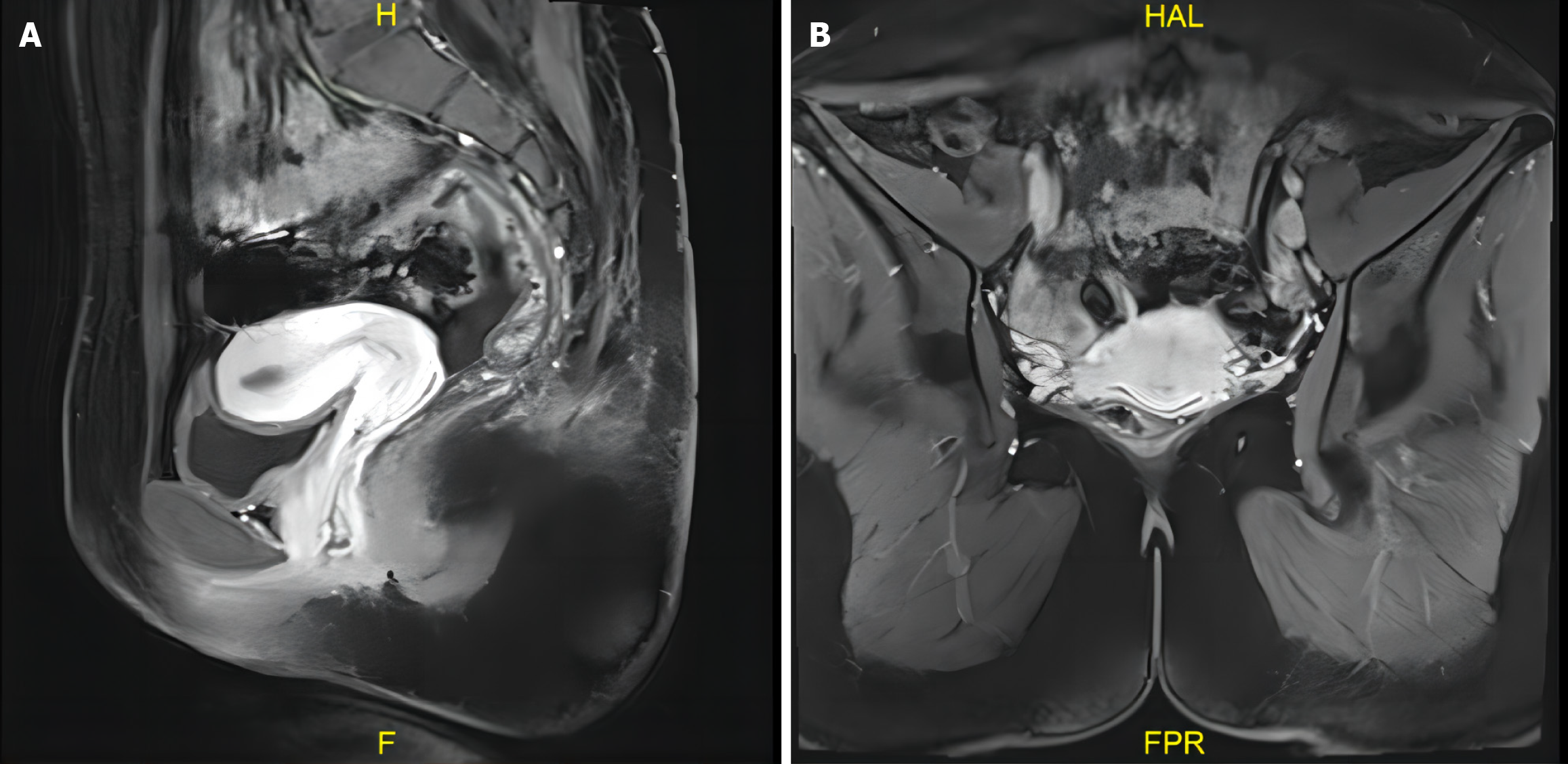
Uterine ultrasonography showed normal results (Figure 2). Pelvic magnetic resonance imaging revealed a normal uterus and cervix (Figure 3).
Histopathologic evaluation confirmed adenocarcinoma in situ of the uterine cervix.
Written informed consent was obtained (December 9, 2023) from the patient and her family after explaining the con
Histopathologic evaluation confirmed adenocarcinoma in situ of the uterine cervix (Figure 1C).
The major stages in cervical carcinogenesis include HPV infection, HPV persistence, progression to dysplasia, and invasion. In 2020, based on statistical data, approximately 604000 new cases of cervical cancer were diagnosed worldwide, leading to approximately 342000 deaths[3]. In the same year, the World Health Organization launched the global Cervical Cancer Elimination Initiative to accelerate the eradication of cervical cancer, which established the “90–70–90” target: 90% of girls should receive HPV vaccine before the age of 15 years, 70% of women should undergo high-quality cervical cancer screening at least twice between the ages of 35 and 45 years, and 90% of women diagnosed with cervical premalignant lesions or cancer should receive treatment and management[4]. Therefore, cervical cancer screening is widely conducted globally, and partial cervical resection is performed in patients with cervical premalignant lesions. LEEP is an established method of early cervical resection, and it contributes to the remission of persistent HPV infection; the rate of complete viral remission is 64.5%[5].
However, HPV infection is a single factor contributing to the development of cervical cancer[6]; therefore, patients with persistent HPV infection after LEEP need more extensive follow-up. Long-lasting HPV infections were traditionally believed to cause CIN in a slow, progressive, and consecutive manner: from normal tissue with HPV infection to CIN 1 (low grade), CIN 2 (moderate grade), CIN 3/CIS (high grade), and finally cancer. However, recent data indicate that CIN 1 may not necessarily precede the development of CIN 3 and that CIN 3 can evolve directly from normal tissue with HPV infection, as described by a molecular switch model. In this model, the severity of dysplasia was determined by the extent of methylation of certain genes, and this progression might not be linear[7].
Adenocarcinoma of the cervix accounts for approximately 25% of all cervical cancers. Compared with squamous cell carcinoma, adenocarcinomas of the cervix are more heterogeneous, with diverse pathologic types and worse prognoses, and early diagnosis significantly affects prognosis[8]. However, the occult lesions of cervical adenocarcinoma are mainly located in the columnar epithelium that coats the cervix as well as the stromal glands[9], which increase the difficulty of early diagnosis. In the current case, gynecological examination revealed cervical canal bleeding, which is one of the signs of cervical adenocarcinoma. TCT may be difficult to obtain the deep part of the cervical canal, and clinicians often do not perform deep sampling during cervical biopsy; thus, results may be inaccurate. Due to inertial thinking and over-reliance on colposcopic cervical biopsy, diagnoses are frequently missed. The formation of scars on the surface of the cervix after LEEP, leading to partially or wholly invisible transformation areas in the squamocolumnar junction, may affect the results of subsequent TCT screening and colposcopy[10].
Considering the patient’s 10-year history of HPV infection and abnormal bleeding, we decided to perform hysteroscopy. Histopathologic evaluation confirmed adenocarcinoma in situ of the uterine cervix. Therefore, hysteroscopic resection of cervical canal tissue is recommended as a supplement to cervical biopsy in cases of persistent HPV infection with abnormal bleeding for early diagnosis, treatment, and improved prognosis.
| 1. | Bedell SL, Goldstein LS, Goldstein AR, Goldstein AT. Cervical Cancer Screening: Past, Present, and Future. Sex Med Rev. 2020;8:28-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 208] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 2. | Chen LM, Liu L, Tao X, He Y, Guo LP, Zhang HW, Zhou XR, Sui L. [Analysis of recurrence and its influencing factors in patients with cervical HSIL within 24 months after LEEP]. Zhonghua Fu Chan Ke Za Zhi. 2019;54:534-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64628] [Article Influence: 16157.0] [Reference Citation Analysis (176)] |
| 4. | World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. Nov 17, 2020. [cited 11 May 2022]. Available from: https://www.who.int/publications/i/item/9789240014107. |
| 5. | Przybylski M, Pruski D, Millert-Kalinska S, Zmaczynski A, Baran R, Horbaczewska A, Jach R, Zaborowska L. Remission of HPV infection after LEEP-conization - a retrospective study. Ginekol Pol. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Chen H, Liu X, Xu L. Incisal margin condition after LEEP for cervical intraepithelial neoplasia patients and prognosis. Exp Ther Med. 2016;12:1019-1021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Massad LS, Einstein MH, Huh WK, Katki HA, Kinney WK, Schiffman M, Solomon D, Wentzensen N, Lawson HW; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. Obstet Gynecol. 2013;121:829-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 548] [Article Influence: 45.7] [Reference Citation Analysis (0)] |
| 8. | Stolnicu S, Segura S, Parra-Herran C, Horn LC, Hoang L, Terinte C, Pesci A, Aviel-Ronen S, Kyokawa T, Alvarado-Cabrero I, Oliva E, Soslow RA, Park KJ. Invasive Stratified Mucin-producing Carcinoma (ISMC) of the Cervix: A Study on Morphologic Diversity. Am J Surg Pathol. 2020;44:873-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Xiao ML, Qian T, Fu L, Wei Y, Ma FH, Gu WY, Li HM, Li YA, Qian ZX, Cheng JJ, Zhang GF, Qiang JW. Deep Learning Nomogram for the Identification of Deep Stromal Invasion in Patients With Early-Stage Cervical Adenocarcinoma and Adenosquamous Carcinoma: A Multicenter Study. J Magn Reson Imaging. 2024;59:1394-1406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Zhao C, Bi H, Zhao Y, Geng L, Liu J, Shen DH, Li S, You ZX, Li MZ, Li JR, Meng YG, Zhang GN, Sui L, Chang SF, Wei LH. [Chinese expert consensus on the management of high-grade intraepithelial neoplasia of cervix]. Zhognguo Fuchanke Linchuang Zazhi. 2022;23:220-223. [DOI] [Full Text] |