Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4770
Revised: May 15, 2024
Accepted: May 30, 2024
Published online: July 26, 2024
Processing time: 97 Days and 1.4 Hours
According to the World Health Organization analgesic ladder, cancer-related pain generally begins with pharmacotherapy in a stepwise approach. Nevertheless, some patients continue to experience poorly controlled pain despite medications, particularly when considering adverse effects and self-care quality. Percutaneous cervical cordotomy is an alternative interventional procedure for unremitting unilateral intractable cancer-related pain.
The patient was diagnosed with lung cancer with destruction of the brachial plexus and ribs. For 2 mo, the patient experienced progressive severe weakness and pain in the right upper extremity. Notably, the pain intensity reached an extreme level, particularly when lying supine, even under heavy sedation. This heightened pain response posed a significant challenge; as a result, the patient was unable to undergo further evaluation through magnetic resonance imaging. Ultimately, he underwent percutaneous cervical cordotomy for symptom relief, resulting in complete resolution of right arm pain. After a 3-mo follow-up, the pain did not recur, and only a flurbiprofen local patch was required for mild scapular tightness.
Cordotomy, under careful patient selection, appears to enhance the quality of life of patients with unilateral cancer-related pain.
Core Tip: Percutaneous cervical cordotomy provides a valuable alternative for the management of intractable cancer-related pain resistant to analgesics. The presented case involves a patient with advanced bronchogenic carcinoma experiencing severe upper limb pain and restricted range of motion. Conscious sedation ensures a comfortable and safe procedure. After cordotomy, the patient experienced relief from cancer-related pain without relying on opioids, significantly improving his quality of life.
- Citation: Lu KY, Lin FS, Lin CS, Lao HC. Percutaneous cervical cordotomy for managing refractory pain in a patient with a Pancoast tumor: A case report. World J Clin Cases 2024; 12(21): 4770-4776
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4770.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4770
Spinal cordotomy, an invasive procedure for the treatment of intractable pain, is not controlled by conventional therapies, such as analgesics or nerve block. It aims to disrupt the nociceptive pathway in the anterolateral column, particularly the lateral spinothalamic tract, by thermal or mechanical destruction[1]. Spiller and Martin[2], who described the first “open” cordotomy in 1912, treated a patient who suffered from pain caused by a lower spinal cord tumor. In 1963, Mullan et al[3] introduced percutaneous cordotomy under fluoroscopy guidance and electrical monitoring. Percutaneous cordotomy, with its attendant real-time patient feedback, appears to be much safer than the open procedure; as a result, it was gene
A 59-year-old man visited our emergency department (ED) complaining of progressive right upper limb weakness, numbness, and persistent pain for 2 mo.
Over the past 2 mo, the patient sought medical attention at local clinics with limited success. Consequently, he came to our hospital for help. According to the patient, he experienced pain radiating from his right hand to the shoulder, consistent with the C5-T1 dermatome. He could not raise or hold his hand because of intermittent lancinating pain and shock-like sensations in the forearm. Profound muscle weakness and limited range of motion were noted, exacerbated by severe pain. Managing his symptoms required an upright position with the head leaned forward because lying down intensified the electric-like pain.
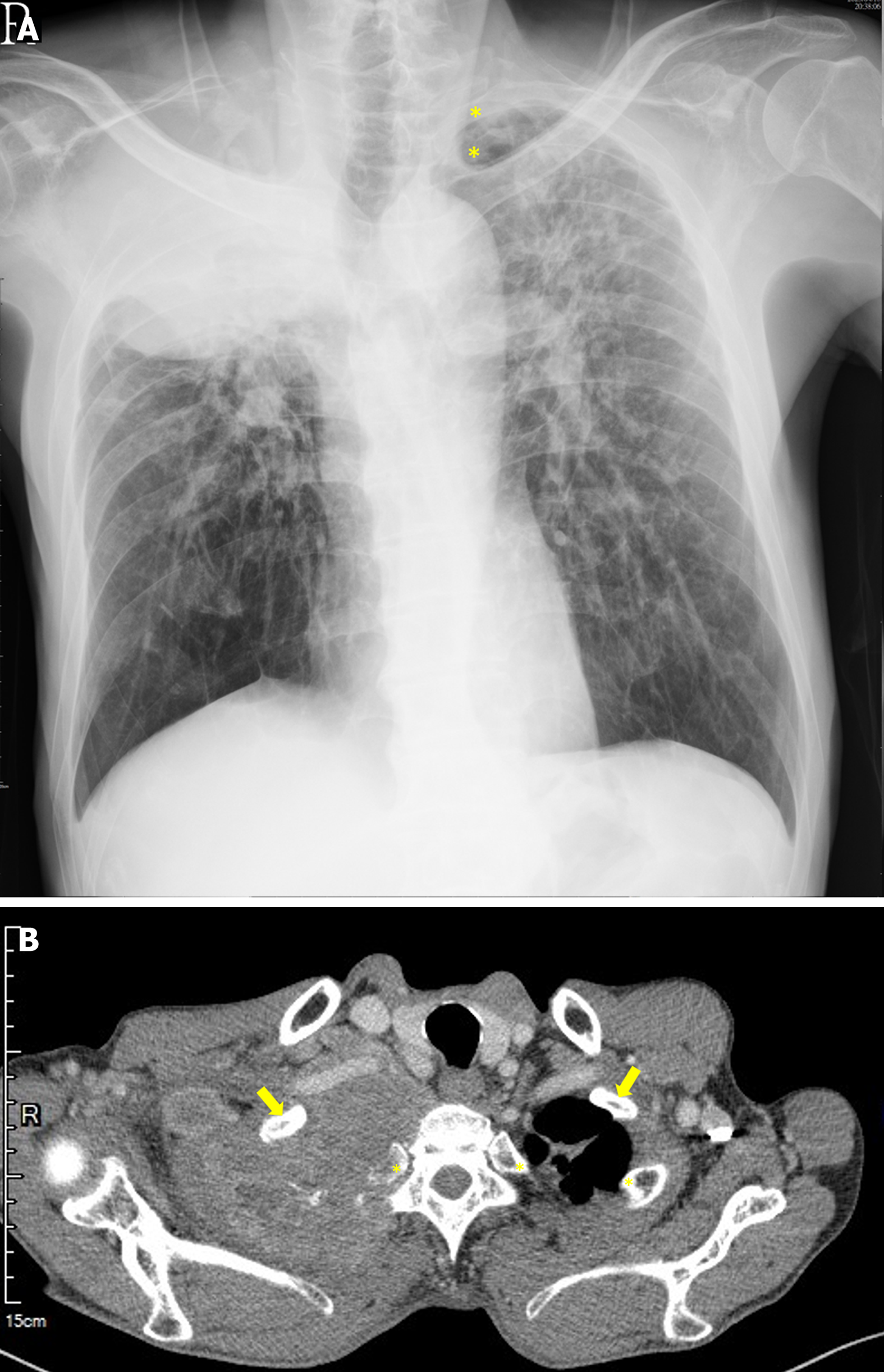
Upon examination in the ED, a chest X-ray (CXR) revealed progressive opacity in the right upper lobe, prompting further investigations. Subsequent chest computed tomography (CT) revealed a substantial soft tissue mass in the right apical lung exceeding 10 cm in diameter, with osteolytic destruction of the adjacent 1st to 3rd ribs, indicative of locally advanced bronchogenic carcinoma. After admission to the chest medicine ward, we were consulted for the treatment of his intractable pain.
Despite a daily oral equivalent of 200 mg morphine, the patient’s pain intensity, measured by the numeric rating scale, remained high with a maximum score of 7. Difficulties arose during examinations requiring a supine posture.
The patient denied any systematic disease.
The patient had no significant personal or family history.
The physical examination showed limited elevation of the shoulder, with a height < 1 cm. The range of motion of his right elbow was approximately 30°. This right elbow extension was limited. He could barely abduct or adduct his finger. No abnormalities were found in the examinations of other systems.
His hemoglobin level was 8.4 g/dL (reference, 13-18 g/dL); white blood cell count, 12400/mm3 (reference, 4000-10000/mm3); creatinine, 2.2 mg/dL (reference, 0.4-1.2 mg/dL); and blood urea nitrogen, 34 mg/dL (reference, 8-20 mg/dL). All other laboratory test results were within the normal ranges.
CXR at the ED revealed a huge space-occupying lesion at the right apical lung with adjunct bony destruction. Chest CT presented a soft tissue mass (> 10 cm in diameter) occupying the entire right apical lung, which was highly suggestive of a locally advanced bronchogenic carcinoma (Figure 1).
The patient was evaluated by multidisciplinary experts in radiology, oncology, chest medicine, chest surgery, psycho
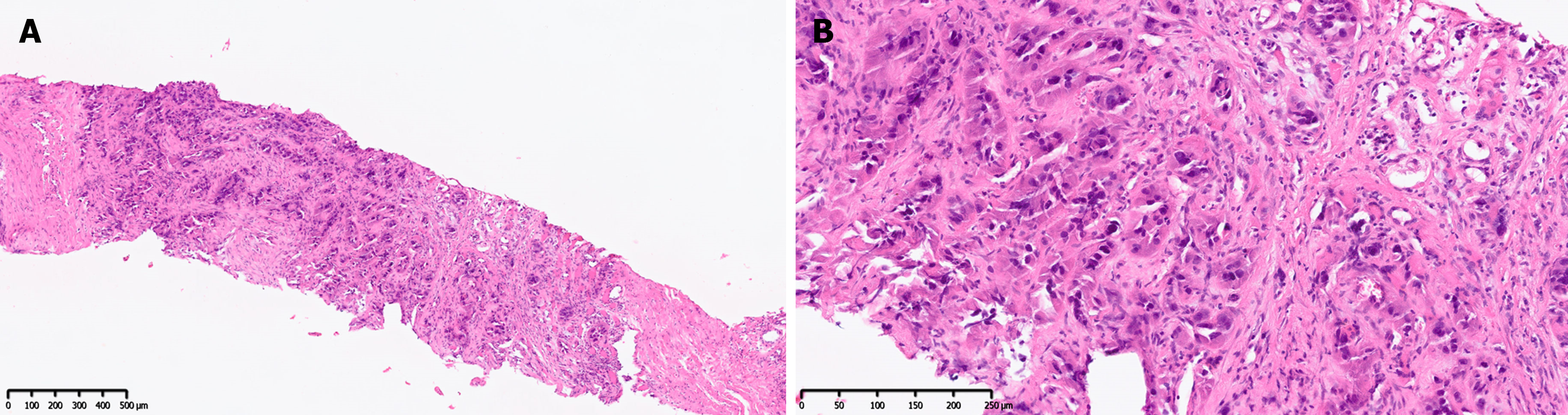
A definitive diagnosis of lung adenocarcinoma was confirmed by CT-guided biopsy. Pathological examination revealed that the lung parenchyma was infiltrated with adenocarcinoma cells with an acinar growth pattern (Figure 2).
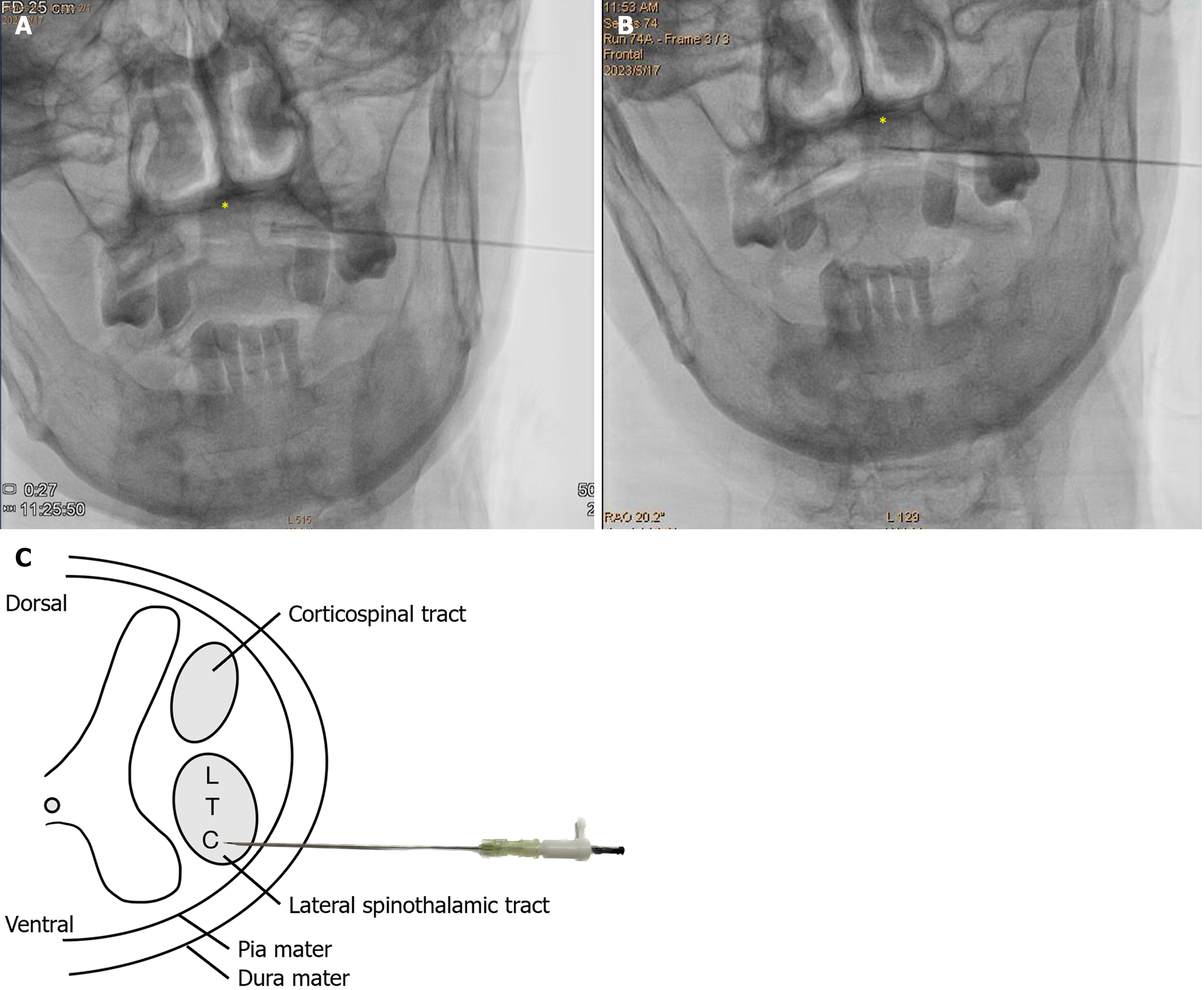
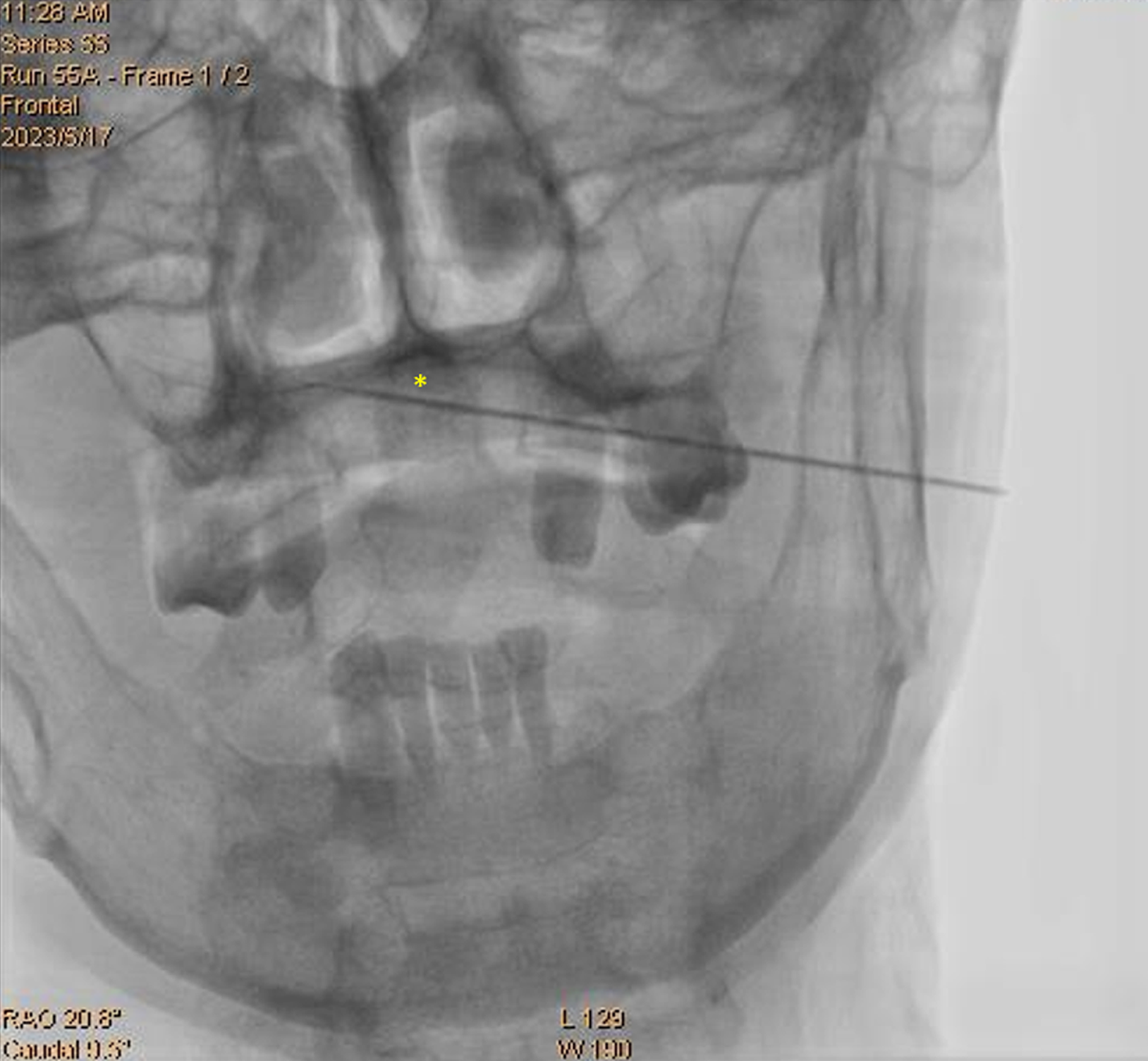
After extensive discussions, a percutaneous cervical cordotomy was performed under biplane fluoroscopic guidance. The patient was positioned supine and underwent conscious sedation, facilitated by dexmedetomidine infusion at a rate of 0.4-0.5 μg/kg/h, complemented by intermittent boluses of 1-2 mg remimazolam. The procedure utilized a 20-g spinal needle and a 28-g straight, sharp cannula with a 2-mm electrode tip (11.7 cm 28 G trocar, 21-G spinal needle, Cosman Electrode, LCETM LCED-TC; Cosman Medical, Burlington, MA, United States) to disrupt the nociceptive pathway in the anterolateral column at the C1-C2 vertebral level (Figure 3).
Sonography confirmed a depth from the skin to the dura mater of 6 cm at the left side of the neck. After confirmation of the entry point, local anesthetic was infiltrated to ease the passage of the needle into the C1-C2 interlaminar space. The anatomical schematic of the percutaneous cervical cordotomy is illustrated in Figure 3. The needle was advanced into the anterolateral quadrant of the spinal cord. Impedance changes were monitored to confirm the location of the electrode tip; an impedance of 150 Ω indicated the cerebrospinal fluid, whereas 600-700 Ω signified the spinal cord parenchyma. Upon assessment of the spinal cord, sensory and motor stimulations were utilized to confirm the target site, the lateral spinothalamic tract, and ensure that other neuropathways were not involved. To alleviate discomfort during radiofrequency (RF) thermocoagulation, an intermittent bolus of 10 mg propofol, for a total of 50 mg, was administered, achieving coagulation at 65 °C for 90 s.
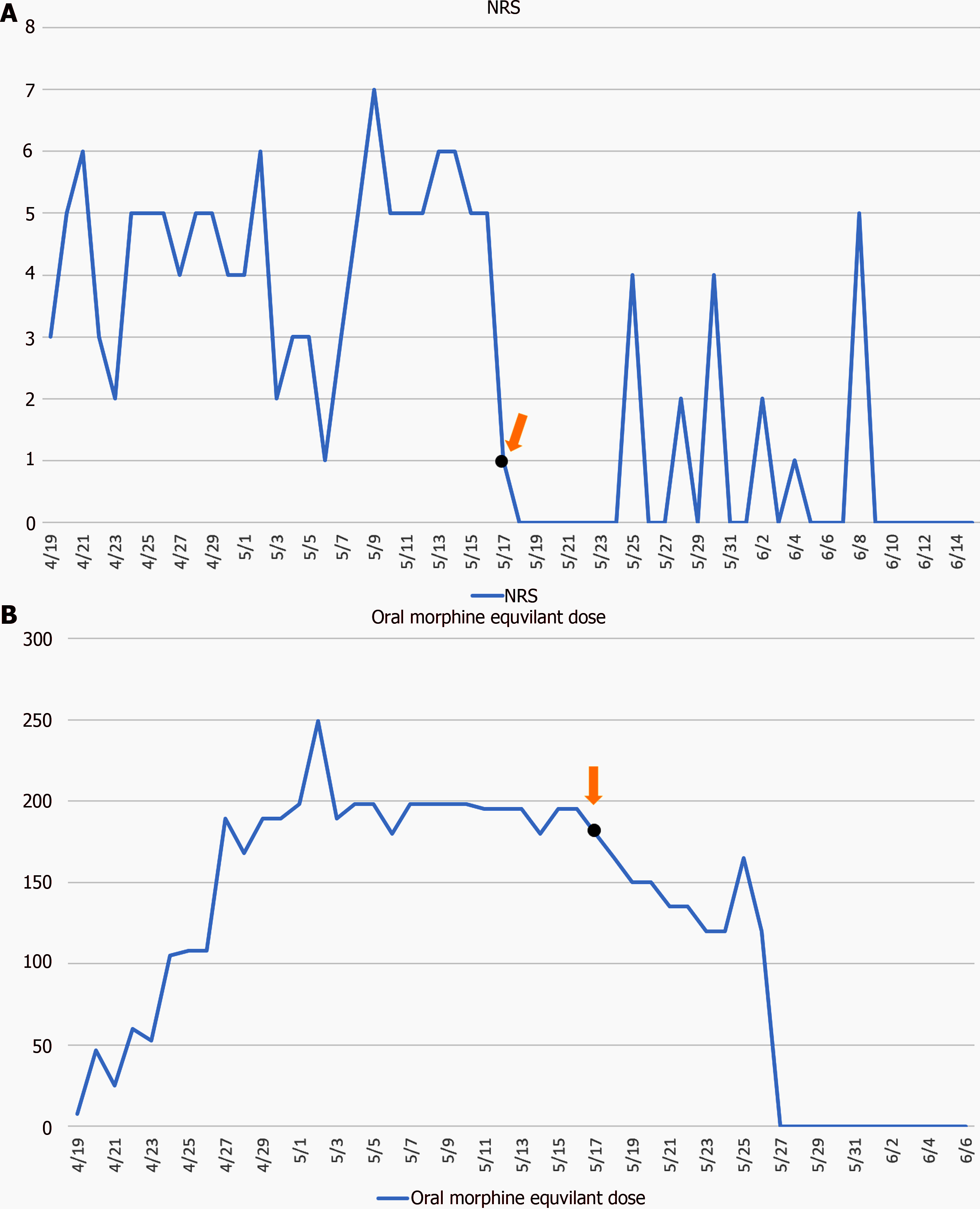
The patient exhibited a notable improvement in symptoms immediately upon awakening from sedation. Postoperatively, both the equivalent dosage of oral morphine and pain intensity markedly decreased (Figure 4). Subsequent palliative cancer management, including radiotherapy and chemotherapy, proceeded smoothly. Opioid analgesic dosage was gradually tapered, and the patient was entirely weaned off it within 3 wk. No significant respiratory or sympathetic dysfunction was noted, and a 3-mo follow-up revealed no pain recurrence; only a flurbiprofen local patch was required for mild scapular tightness.
In this study, we presented the challenging case of a patient diagnosed with lung adenocarcinoma complicated by the destruction of the brachial plexus and adjacent ribs, leading to severe, relentless neoplasm-related pain in the right upper limb despite aggressive pharmacotherapy. Despite efforts to obtain a preprocedural magnetic resonance imaging (MRI) for the evaluation of percutaneous cordotomy, the patient’s distress prevented successful cooperation, necessitating alternative imaging modalities. Consequently, we opted for biplane X-ray imaging under light sedation for the preprocedural assessment.
During the procedure, we encountered several technical challenges, notably in confirming the position of the needle tip using anterior-posterior and lateral X-ray views of the cervical spine. Despite our best efforts, impedance measurements of the RF generator did not consistently increase, particularly when the needle approached the midline and contralateral lamina (Figure 5). This discrepancy raised concerns about the accurate placement of the needle and potential inadvertent spinal cord penetration. Therefore, incorporating advanced imaging such as CT guidance[1] or MRI[5] during the procedure could enhance safety and precision in target localization. A hybrid operating room may also be beneficial.
To mitigate procedural discomfort and ensure patient safety, neurophysiological stimulation was employed for lesion confirmation after insertion into the cervical spinal cord. Given the need for patient cooperation during this critical phase, dexmedetomidine served as the primary anesthetic agent with adjuvant support. Despite meticulous planning, unex
In comparison with standard procedures outlined in textbooks, we opted against contrast instillation because of its potential interference with impedance measurements of the RF generator. Although contrast administration is recommended for visualizing the cervical spinal cord[7], our decision was guided by the need to ensure accurate needle placement without access to preprocedural MR images. Despite these deviations, our modified approach utilizing a smaller-gauge RF generator with a reduced electrode tip size yielded promising outcomes, with the patient experiencing pain relief and minimal postoperative complications during follow-up assessments.
Percutaneous cordotomy represents a viable interventional option for patients experiencing intractable cancer-related pain and potentially severe neuropathic pain resulting from nerve destruction or entrapment. Conscious sedation, facilitated by dexmedetomidine and remimazolam, provided effective anesthesia for ensuring proper positioning and maintaining a safe airway throughout the procedure.
We appreciate the expert comments of the reviewers and editors and the contacts they shared.
| 1. | Javed S, Viswanathan A, Abdi S. Cordotomy for Intractable Cancer Pain: A Narrative Review. Pain Physician. 2020;23:283-292. [PubMed] |
| 2. | Spiller WG, Martin E. The treatment of persistent pain of organic origin in the lower part of the body by division of the anterolateral column of the spinal cord. JAMA. 1912;58:1489-1490. [RCA] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 209] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Mullan S, Harper PV, Hekmatpanah J, Torres H, Dobbin G. Percutaneous Interruption of Spinal-Pain Tracts by Means of a Strontium90 Needle. J Neurosurg. 1963;20:931-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 111] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Winn HR. Neurosurgical Management of Intractable Pain. In: Mirzadeh Z, Rosenberg WS, Ben-Haim S, Follett KA. Youmans & Winn Neurological Surgery. 8th ed. Elsevier, 2023: chap 201. |
| 5. | Massire A, Taso M, Besson P, Guye M, Ranjeva JP, Callot V. High-resolution multi-parametric quantitative magnetic resonance imaging of the human cervical spinal cord at 7T. Neuroimage. 2016;143:58-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Paxinos G. The Human Nervous System. Elsevier, 1990. |
| 7. | Winn HR. Percutaneous Cordotomy and Trigeminal Tractotomy for Pain. In: Raslan AM, Stedelin BA. Youmans & Winn Neurological Surgery. 8th ed. Elsevier, 2023: chap 209. |