Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4748
Revised: June 5, 2024
Accepted: June 19, 2024
Published online: July 26, 2024
Processing time: 115 Days and 6.6 Hours
Granulomatous lobular mastitis (GLM) is a rare benign inflammatory disease of the breast and is classified under comedo mastitis in traditional Chinese medicine (TCM). The etiology of this disease is unknown, and it mainly occurs in women of childbearing age. The diagnosis depends on histopathological biopsy. At present, there is no systematic and standardized treatment plan for GLM. In the absence of evidence supporting an infectious etiology, affected patients might continue to receive multiple courses of antibiotics and unnecessary surgery.
A 37-year-old Chinese woman with a history of coronavirus disease 2019 infection presented with swelling and pain in the left breast. She also had erythema, nodules in the lower extremities, arthritis in both knees, cough, and headache. In the early stage of GLM, the mass was not significantly reduced by conservative treatment with internal application of TCM; hence, surgical treatment was carried out. The aim of postoperative treatment was to drain the pus, eliminate the necrosed tissue, and expand the muscles; fumigation and washing using TCM was applied.
Combined internal and external treatment with TCM, following the principle of “Prioritize internal treatment before ulceration and emphasize external treatment after ulceration” was effective in our patient with GLM. The prognosis was good. We believe that TCM offered valuable therapeutic benefits in this disease.
Core Tip: We focus on the treatment efficacy of combining traditional Chinese (TCM) and Western medicine for granulomatous lobular mastitis (GLM). GLM was treated conservatively with TCM in the early stages, but the disease symptoms did not significantly improve. Hence, surgery was required. Postoperatively, we drained the pus, removed decay, and dilated muscles through TCM-based fumigation and washing. The combination of TCM and Western medicine had a definite therapeutic effect on GLM and offered good prognosis. TCM offered valuable therapeutic benefits in this disease.
- Citation: Meng T, Chu ML, Wang B, Ye MN, Cheng YQ, Chen HF. Granulomatous lobular mastitis treated by a combined internal and external treatment of traditional Chinese medicine: A case report. World J Clin Cases 2024; 12(21): 4748-4754
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4748.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4748
Granulomatous lobular mastitis (GLM) is a rare chronic inflammatory breast disease characterized by aperiodic breast pain, breast lumps, and long-term recurrent episodes resulting in the formation of fistula or sinus tract[1]. While the etiology of GLM has not been fully elucidated, factors such as autoimmunity, hyperprolactinemia, hormonal imbalance, α 1-antitrypsin deficiency, smoking, and diabetes mellitus have been considered to play a role in its pathogenesis[1,2]. Therefore, there is currently no established, standardized treatment protocol for GLM.
At present, multiple therapeutic modalities are available for GLM, including hormone therapy, surgical treatment, and immunosuppressive therapy, each bearing its distinct strengths and limitations[2,3]. However, a systematic and standardized treatment protocol is yet unavailable. Traditional Chinese medicine (TCM) has been shown to have a significant therapeutic effect on GLM, especially in patients who require non-surgical treatment[4]. TCM follows the principle of “Prioritize internal treatment before ulceration, and emphasize external treatment after ulceration”, that is, conservative treatment should be adopted in the early stage of the disease; surgical debridement should be considered only if the results of conservative treatment are unsatisfactory. Moreover, postoperative TCM syndrome differentiation and dressing change can effectively promote wound healing[3-5].
A 37-year-old woman visited the Breast Surgery Department of Longhua Hospital on June 17, 2022, with a large, painful, ruptured, pus-filled left breast mass.
The patient developed a solid lump in her left breast towards the end of her coronavirus disease 2019 isolation period on April 30, 2022. A few days later, her left breast was injured by her baby's kick, accompanied by redness and swelling of the breast skin. One week later, she developed swelling and pain in both lower limbs accompanied by erythema nodules and cough. The patient received empirical cefuroxime for 2 weeks, with no relief of symptoms and subsequent headaches.
No special history of past illness.
No specific personal and family history.
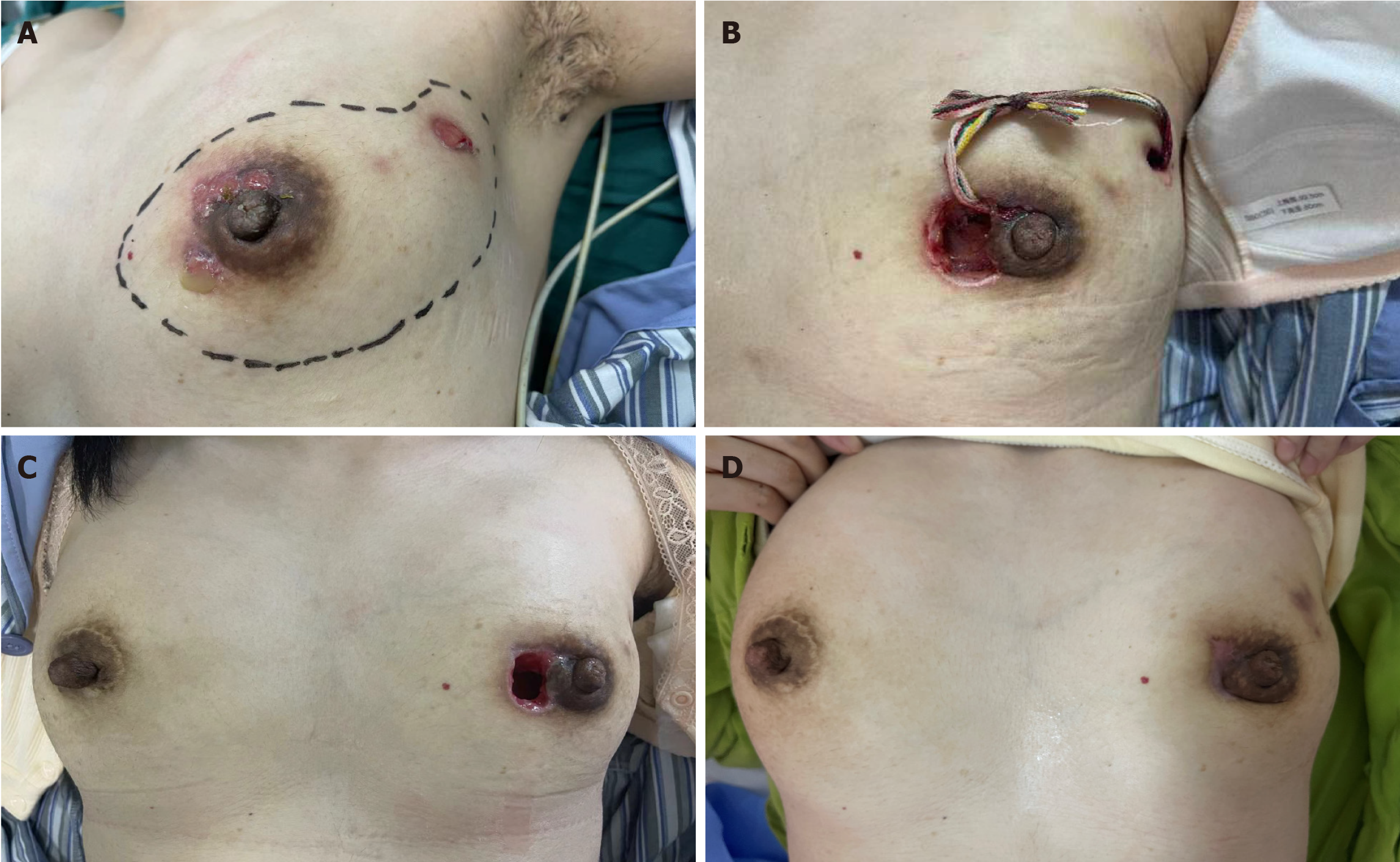
Physical examination showed a sunken left nipple and a hard palpable mass (12 cm × 15 cm) in the left breast and areola area, with obvious tenderness, multiple ulcerations, hypergranulated tissue, and slight pus discharge. Dark red patches were observed on both lower limbs (Figure 1).
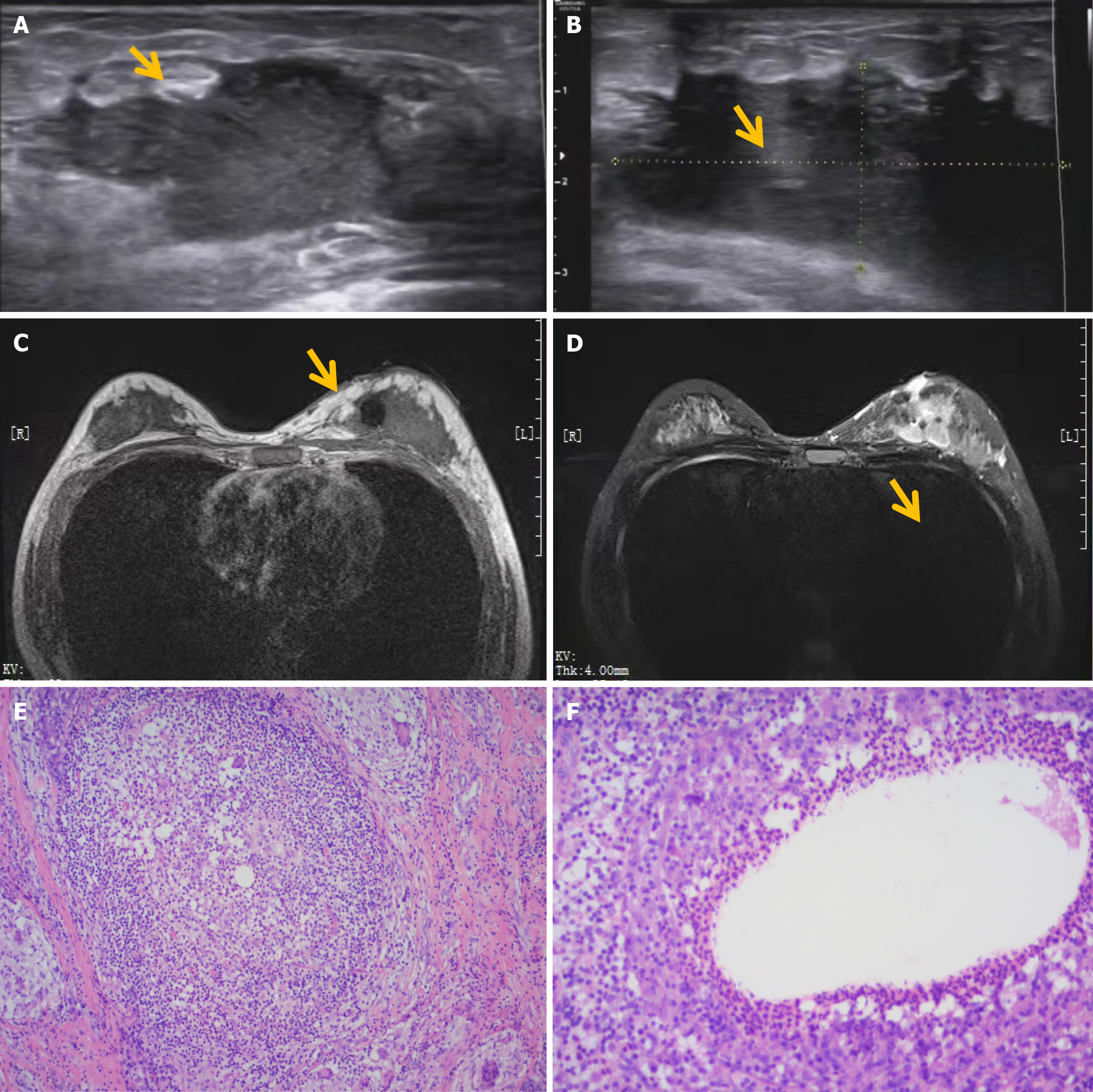
B-ultrasound examination showed irregularly contoured hypoechoic mass (Figure 2A and B).
Given these findings, the patient was finally diagnosed with GLM. The TCM diagnosis was acne-prone mastitis, and the syndrome differentiation was dampness-heat of liver channel.
The patient subsequently received TCM treatment with the principle of soothing the liver, removing heat, regulating blood flow, and eliminating the mass. The prescription of TCM was as follows: Bupleurum (9 g), Scutellaria (9 g), Radix paeoniae rubra (9 g), Angelica (12 g), Smilax china (15 g), Chinese honeylocust spine (9 g), Qingpi (9 g), Tangerine peel (9 g), Poria with hostwood (20 g), Saposhnikovia divaricata (9 g), Rehmannia glutinosa (20 g), Fructus crataegi (12 g), Radix codonopsis (12 g), Caulis spatholobi (20 g), Luffa (18 g), Radix cyathulae (15 g), Maize silk (20 g), Pinellia (9 g), Poria (20 g), Folium isatidis (20 g), Ramulus cinnamomi (9 g). The above ingredients were decocted in 200 mL water for one daily dose, for a total of 14 doses. In addition, Chonghe ointment and Baiyu ointment made by the hospital were used for external application. A 2-mm-thick layer of ointment on gauze was applied, covering an area larger than the lump. Chonghe ointment or Baiyu ointment was alternately used for 4-8 ha day.
After 14 days of continuous TCM treatment, the left breast mass remained, but its texture softened. The cough was under control, but the patient started experiencing headaches. Therefore, we removed angelica, smilax china, Chinese honeylocust spine, qingpi, poria with hostwood, and ramulus cinnamomic from the prescription and added radix puerariae (30 g), chuanxiong rhizoma (15 g), angelica dahurica (9 g), rhizoma corydalis (30 g), malt (60 g), and cortex mori (15 g), for a total of 28 doses. After 42 days of continuous TCM treatment, the left breast mass, headache, and dark red pigmentation remained, but the symptoms of joint pain, erythema nodosum, and cough improved. Open debridement was performed on August 1, 2022. The patient was treated with TCM syndrome differentiation and dressing change according to the different post-operative stages. Two incisions appeared post-operation, dressings, drainage, and medication on the incisions led to rapid relief of headache by the 5th post-operative day. On the 12th post-operative day, wound suppuration had cleared and was treated with TCM fumigation. Meanwhile, infrared radiation was used to warm Yang, dissipate accumulation, promote blood circulation, and generate muscle mass. After fumigation and washing, Kangfuxin liquid gauze was used to promote wound closure, and the wound surface healed 24 days after the operation. Physical breast ultrasound examination showed that the upper outer sores of the left breast had healed (Figure 3).
The patient was followed-up on September 24, 2022. There was no discomfort in the left breast and the ulcerated cavity had healed (Figure 4).
In TCM theory, the nipple belongs to the liver meridian and the breast belongs to the stomach meridian[6]. Liver Qi thrives in a state of relaxation and free-flowing and resists being constrained or suppressed. However, women are prone to depression, which depresses the liver and causes liver fire to build up over time[5,6]. Moreover, when liver Qi is not flowing smoothly, it can easily invade the spleen, causing the spleen to lose its function of transportation and transformation. Finally body fluids accumulate into phlegm, which makes the disease protracted and difficult to cure[7]. Chinese herbal medicine is usually used as a formulation guided by TCM theory, combining multiple herbs in the prescription[6-8]. The prescription used in this study is based on radix codonopsis and poria to invigorate the spleen and dissipate phlegm, and tangerine peel and Pinellia to dry and dampen the phlegm. Smilax china and Chinese honeylocust spine can reduce the swelling and discharge of pus[8]. Fructus crataegi can reduce fat turbidity and blood circulation detume
Based on internal treatment, external treatment was given to improve the treatment efficacy. After surgery, the external treatment was adjusted to steam fumigation and washing with TCM every day. TCM fumigation and washing can benefit qi and promote blood circulation with the help of medicinal force and heat, promote wound healing, and shorten the disease course. The fumigation and washing prescription of TCM (raw astragalus 30 g, angelica 9 g, salvia miltiorrhiza 30 g, ramulus cinnamomi 9 g, dandelion 30 g, radix curcumae 15 g, catechu 12 g, lycopus lucidus 15 g) is heated by a machine to form steam and act on the wound surface. The specific scheme is as follows: once a day for 30 minutes, and generally 12 days for a treatment cycle. The length of the cycle can be adjusted according to the size of the ulcer cavity. During fumigation and washing, the steam nozzle should be kept a proper distance from the wound surface to avoid scalding. Infrared radiation is also used to promote wound blood circulation and muscle relaxation[13,14].
Most patients with GLM are women of childbearing age[2]. Considering the breast aesthetics and psychological factors, conservative and less invasive treatment methods are often used in the early stage[4-6]. In the early stage of GLM, oral TCM combined with external application of plaster may completely relieve the swelling. If the condition does not improve, surgical intervention may be required. Our patient was treated according to the above-mentioned protocol and showed good recovery.
A combined method of internal and external treatment with TCM, following the principle of “Prioritize internal treatment before ulceration and emphasize external treatment after ulceration” was effective for GLM. The final prognosis was good, and TCM appears to offer good benefits in the treatment of this disease.
| 1. | Kornfeld HW, Mitchell KB. Management of idiopathic granulomatous mastitis in lactation: case report and review of the literature. Int Breastfeed J. 2021;16:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Özşen M, Tolunay Ş, Gökgöz MŞ. Granulomatous Lobular Mastitis: Clinicopathologic Presentation of 90 Cases. Turk Patoloji Derg. 2018;34:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Illman JE, Terra SB, Clapp AJ, Hunt KN, Fazzio RT, Shah SS, Glazebrook KN. Granulomatous diseases of the breast and axilla: radiological findings with pathological correlation. Insights Imaging. 2018;9:59-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Li ZY, Sun XM, Li JW, Liu XF, Sun ZY, Chen HH, Dong YL, Sun XH. Treatment of bilateral granulomatous lobular mastitis during lactation with traditional Chinese medicine: A case report. World J Clin Cases. 2021;9:8249-8259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 5. | Sripathi S, Ayachit A, Bala A, Kadavigere R, Kumar S. Idiopathic granulomatous mastitis: a diagnostic dilemma for the breast radiologist. Insights Imaging. 2016;7:523-529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Wang S, You F, Yuan Q. [Clinical efficacy of breast closure irrigation and drainage combined with external application of Sanhuang powder in the treatment of granulomatous lobular mastitis]. Shandong Yiyao Zazhi. 2023;10:59-62. [DOI] [Full Text] |
| 7. | Zhou QY, Zhai Z, Zhao LN, Liang C, Li TH, Zhu DS. [Clinical efficacy, safety, and GRADE evidence level evaluation of integrated traditional Chinese and Western medicine in the treatment of granulomatous mastitis patients]. Shijie Zhongxiyi Jiehe Zazhi. 2023;18:42-48. [DOI] [Full Text] |
| 8. | Zhang P, Xie F, Zhou G, Wu YG, Ma JY, Chen ZL. [Treating granulomatous mastitis from the perspective of "phlegm"]. Zhongguo Zhongyi Jichu Yixue Zazhi. 2023;29:154-156. [DOI] [Full Text] |
| 9. | Wang G, Gao L, Liu W, Ma QJ, Bai YZ, Liu XJ. [Minimally invasive circumcision combined with traditional Chinese medicine for the treatment of 40 cases of granulomatous mastitis]. Zhongguo Zhongxiyi Jiehe Waike Zazhi. 2019;25:819-821. [DOI] [Full Text] |
| 10. | Li L, Chen HH, Sun XH, Zhu JM, Liu XT, Li WY. [Research progress in the treatment of granulomatous mastitis with traditional Chinese medicine]. Zhongguo Zhongyiyao Xinxi Zazhi. 2022;29:139-142. [DOI] [Full Text] |
| 11. | Sun YY, Zhang WD, Wang DY, Shi XC. [Treatment of 30 cases of chronic non lactating mastitis with traditional Chinese medicine combined with minimally invasive circumcision]. Linchuang Yu Bingli Zazhi. 2021;41:1032-1038. [DOI] [Full Text] |
| 12. | Yang LP, Hu Y, Li WZ, Zhang JX, Liu XY. [Comparison of ultrasound and clinical efficacy between traditional Chinese medicine external treatment and hormone blockade treatment for granulomatous mastitis]. Xiandai Zhongxiyi Jiehe Zazhi. 2017;26:2546-2548. [DOI] [Full Text] |
| 13. | Liu L, Hou X, Li Q, Ma Y. [Clinical efficacy observation of traditional Chinese medicine oral administration combined with external application in the treatment of granulomatous mastitis in the mass stage]. Shiyong Yaowu Yu Linchuang Zazhi. 2021;4:12. [DOI] [Full Text] |
| 14. | Mu YJ, Wang TS, Feng X, Sun P, Gao S, Wang YK, Zuo XM, Zhu YY, Ma Y, Shi XG. [Clinical efficacy of external treatment with Zicao Yanghe Tang combined with hormone therapy for granulomatous mastitis in the mass stage and its effect on cell pyroptosis protein]. Hainan Yixueyuan Xuebao. 2023;29:1703-1709. [DOI] [Full Text] |