Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4558
Revised: May 21, 2024
Accepted: May 30, 2024
Published online: July 26, 2024
Processing time: 90 Days and 23.6 Hours
Joint replacement is a common treatment for older patients with high incidences of hip joint diseases. However, postoperative recovery is slow and complications are common, which reduces surgical effectiveness. Therefore, patients require long-term, high-quality, and effective nursing interventions to promote rehabilitation. Continuity of care has been used successfully in other diseases; however, little research has been conducted on older patients who have undergone hip replacement.
To explore the clinical effect of continuous nursing on rehabilitation after dis
A retrospective analysis was performed on the clinical data of 113 elderly patients. Patients receiving routine nursing were included in the convention group (n = 60), and those receiving continuous nursing, according to various methods, were included in the continuation group (n = 53). Harris score, short form 36 (SF-36) score, complication rate, and readmission rate were compared between the con
After discharge, Harris and SF-36 scores of the continuation group were higher than those of the convention group. The Harris and SF-36 scores of the two groups showed an increasing trend with time, and there was an interaction effect between group and time (Harris score: Fintergroup effect = 376.500, Ftime effect = 20.090, Finteraction effect = 4.824; SF-36 score: Fintergroup effect = 236.200, Ftime effect = 16.710, Finteraction effect = 5.584; all P < 0.05). Furthermore, the total complication and readmission rates in the conti
Continuous nursing could significantly improve hip function and quality of life in older patients after joint replacement and reduce the incidence of complications and readmission rates.
Core Tip: Hip joint diseases are frequent in the older population. The prevalence rate is high, and its damage to the health and life of the older individuals poses a substantial burden. Here, we analyzed the effect of continuous care on rehabilitation after discharge of older patients undergoing joint replacement. Using the Harris score, short form 36 score, complication rate, and readmission rate as observational indicators, we proposed the effectiveness of extended continuous care in the rehabilitation after discharge of older patients who have undergone joint replacement, which is a breakthrough in the efficacy and rehabilitation of older patients undergoing joint replacement.
- Citation: Qi XY, Zhou HY, Xing YH. Effect of continuous nursing on rehabilitation of older patients with joint replacement after discharge. World J Clin Cases 2024; 12(21): 4558-4565
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4558.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4558
Clinical hip diseases include avascular necrosis of the femoral head, femoral neck fracture, and hip degenerative diseases, which can cause functional disability and reduce the quality of life of patients[1]. These diseases tend to occur in the older population. Recently, the prevalence of hip diseases in older individuals is on the rise, which poses substantial risks to their health and quality of life. Currently, hip replacement is a routine method to treat hip diseases, which can effectively relieve clinical symptoms, correct morphological deformity, and restore limb function, thus improving quality of life[2].
Patients who have undergone hip replacement often recover slowly, and functional recovery takes a long time. Clinical follow-up has showed that postoperative complications, such as joint stiffness, respiratory system infection, urinary tract infection, and lower extremity venous thrombosis, are prone to occur, affecting the expected efficacy[3]. Therefore, long-term, high-quality, and effective nursing care for patients after surgery is an important aspect of clinical nursing and ensures the effect of surgery and postoperative rehabilitation. In the past, rehabilitation nursing mainly focused on patients during hospitalization. The nursing time was limited, and there was a lack of attention to rehabilitation nursing after discharge. Continuous nursing extends care to the family and patients after discharge, thereby enhancing the scope of nursing services[4]. The scope of this nursing model is more specific and refined, considers the nursing needs of patients, particularly older patients, and has been successfully applied in postoperative rehabilitation nursing of various diseases[5,6]. Reports on the application of continuous nursing in the rehabilitation of older patients undergoing joint replacement are few. Therefore, this study aimed to adopt a retrospective method to further explore the clinical effects of continuing care on the rehabilitation of older patients after discharge following joint replacement and to provide data reference for the postoperative rehabilitation of these patients.
A retrospective analysis was performed to collect clinical data from older patients who underwent hip replacement in our hospital from October 2020 to January 2022. The included patients met the following conditions: (1) Meeting the clinical diagnostic criteria of hip joint disease after undergoing imaging examination[7]; (2) aged ≥ 60 years; (3) meeting the indications for hip replacement and who underwent the surgery for the first time; and (4) those whose treatment compliance was adequate, and follow-up was completed normally. The exclusion criteria were as follows: (1) Patients with osteoarthritis; (2) patients with coagulation dysfunction; (3) patients with dysfunction of the heart, liver, lung, and other important organs; and (4) patients with incomplete clinical, surgical, and follow-up data. Finally, a total of 113 patients were enrolled. Patients receiving routine nursing were included in the convention group (n = 60), and those receiving continuous nursing, according to various nursing methods, were included in the continuation group (n = 53).
The care of all patients in this study was performed by the same group of experienced and trained nurses.
Conventional nursing method: This method involves the use of routine care practices. Patients were provided with routine nursing care during hospitalization and postoperative routine rehabilitation nursing. Before discharge, the patients were informed in detail regarding matters requiring attention after discharge and related rehabilitation training procedures, and postoperative functional recovery education brochures were distributed accordingly. The patients were instructed to visit our hospital for regular re-examination at 1, 3, and 6 months after discharge.
Continuous nursing method: Continuous nursing was adopted based on the convention group method. At different stages after discharge, the patients were given rehabilitation guidance, complication prevention guidance, psychological support, and reminders of hospital revisits, and were required to fill in questionnaires by door-to-door visits or telephone follow-ups according to their needs. Within 6 months after discharge, the researchers visited the patients once every 2 weeks, provided limb joint and muscle strength recovery training, provided advice on daily living habits and emotional encouragement, and urged patients to regularly review their results. Each visit or telephone follow-up did not exceed 30 min. We provided the patients with rehabilitation guidance, i.e. education regarding care after hip replacement.
According to the actual condition of the patient, a low-intensity independent activity training plan was formulated, and rehabilitation training was performed thrice a week. The patient’s family members were asked about the patient’s self-management status and compliance in daily life and were encouraged to provide the patient with adequate emotional support. We determined the physical rehabilitation status of the patients by telephone every month. Unhealthy lifestyle was corrected in time, and the patients were informed to have outpatient reviews. According to the postoperative rehabilitation situation of each patient, the exercise program was refined regularly, and the number of weekly rehabilitation training was increased as appropriate. Patients with satisfactory recovery were encouraged to further undergo hip abductor strength training to prevent joint dislocation.
Harris score: The Harris score was used to evaluate hip function of patients after discharge (including the day of discharge, 3 months after discharge, and 6 months after discharge)[8]. The assessment included performance of daily activities, range of motion, pain, deformity, gait, walking distance, and the use of a walking aid. The maximum score was 100 points, and higher scores indicated better recovery of joint function. A total score of 90-100 indicated excellent, 80-89 indicated good, 70-79 indicated medium, and < 70 indicated poor recovery.
Short form 36 score: The Chinese version of the short form 36 (SF-36) Health Survey[9] was used to evaluate the health status and quality of life of the patients after discharge. The scale evaluated eight dimensions, including general health, physical health, physical function, emotional function, social function, physical pain, vitality of life, and mental health. The conversion score of each dimension was calculated as: [(actual score - lowest possible score of this dimension)/difference between the highest and lowest possible scores of this dimension] × 100. After conversion, the scores of each dimension ranged from 0 to 100, and the lower the score, the more serious the effect in the dimension. The Harris score of patients was the sum of the conversion scores of all dimensions, and higher scores indicate a higher quality of life.
Postdischarge complications and readmission rate: Postoperative complications were recorded during the follow-up period, including hip dislocation, joint stiffness, respiratory infection, urinary tract infection, pressure ulcers, and lower extremity venous thrombosis. The reason for readmission was treatment for postoperative complications.
The data of this study were processed using Statistical Package for the Social Sciences, and count data are represented as mean ± standard deviation. Student’s t-test was used to compare two groups, and repeated measures analysis of variance was used to compare data at different time points between the groups. The count data are represented as the number of cases (percentage), and the chi-squared or rank sum test was performed. When 1 ≤ theoretical frequency < 5, the χ2 was taken as the correction value, and when theoretical frequency < 1, the χ2 was the exact value. The significance level for the test was α = 0.05.
The baseline data of patients in the continuation and convention groups were compared and are shown in Table 1.
| Baseline data | Convention group, n = 60 | Continuation group, n = 53 | χ2/t | P value |
| Sex | 0.022 | 0.883 | ||
| Male | 32 (53.33) | 29 (54.72) | ||
| Female | 28 (46.67) | 24 (45.28) | ||
| Age in years | 67.32 ± 12.28 | 66.51 ± 12.54 | 0.347 | 0.730 |
| Clinical diagnosis | 0.122 | 0.941 | ||
| Hip fracture | 35 (58.33) | 32 (60.38) | ||
| Ischemic necrosis of femoral head | 22 (36.67) | 19 (35.85) | ||
| Degenerative disease of the hip joint | 3 (5.00) | 2 (3.77) | ||
| Modus operandi | 0.941 | 0.864 | ||
| Unilateral total hip replacement | 5 (8.33) | 6 (11.32) | ||
| Bilateral total hip replacement | 39 (65.00) | 33 (62.26) | ||
| Unilateral femoral head replacement | 16 (26.67) | 14 (26.42) | ||
| Prosthesis fixation | 0.834 | 0.761 | ||
| Cement fixation | 39 (65.00) | 30 (56.60) | ||
| Cementless fixation | 21 (35.00) | 23 (43.40) |
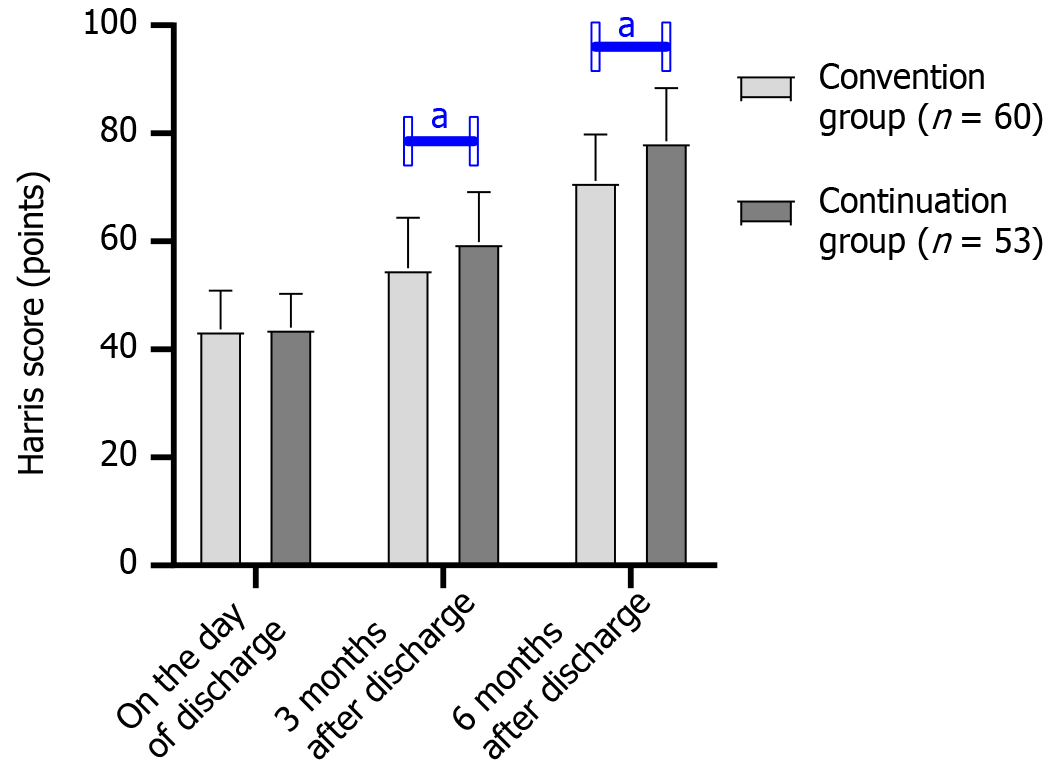
Three months and six months after discharge, the Harris score of the continuation group was higher than that of the convention group (P < 0.05). The Harris scores in both the continuation and conventional groups increased with time, and an interaction effect was observed between group and time (intergroup effect: F = 376.500, P < 0.001; time effect: F = 20.090, P < 0.001; interaction effect: F = 4.824, P = 0.009; Table 2 and Figure 1).
| Time | Convention group, n = 60 | Continuation group, n = 53 | t | P value |
| On the day of discharge | 43.68 ± 7.22 | 44.03 ± 6.25 | 0.274 | 0.785 |
| 3 months after discharge | 55.07 ± 9.32 | 59.86 ± 9.24 | 2.737 | 0.007 |
| 6 months after discharge | 71.22 ± 8.57 | 78.52 ± 9.86 | 4.211 | < 0.001 |
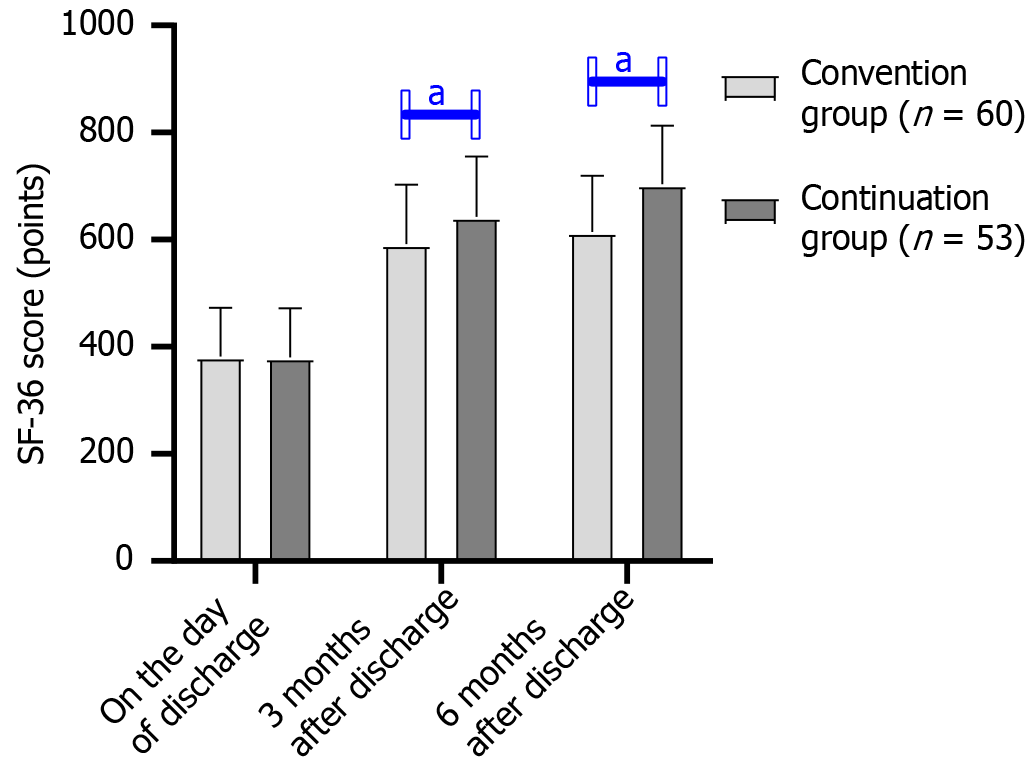
Three months and six months after discharge, the SF-36 score of the continuation group was higher than that of the convention group (P < 0.05). The SF-36 scores of both the groups increased with time, and an interaction effect was observed between group and time (intergroup effect: F = 236.200, P < 0.001; time effect: F = 16.710, P < 0.001; interaction effect: F = 5.584, P = 0.004; Table 3 and Figure 2).
| Time | Convention group, n = 60 | Continuation group, n = 53 | t | P value |
| On the day of discharge | 382.45 ± 90.22 | 380.16 ± 92.14 | 0.133 | 0.894 |
| 3 months after discharge | 592.36 ± 110.32 | 643.24 ± 112.37 | 2.425 | 0.017 |
| 6 months after discharge | 614.35 ± 105.22 | 703.88 ± 108.92 | 4.440 | < 0.001 |
The total complication and readmission rates in the continuation group were lower than those in the convention group (P < 0.05) (Table 4).
| Group | Complication | Readmission (rate) | ||||
| Hip dislocation | Lower extremity venous thrombosis | Joint stiffness | Urinary tract infection | Aggregate | ||
| Convention group, n = 60 | 3 (5.00) | 2 (3.33) | 3 (5.00) | 4 (6.67) | 12 (20.00) | 8 (13.33) |
| Continuation group, n = 53 | 0 (0.00) | 1 (1.13) | 1 (1.13) | 0 (0.00) | 2 (2.26) | 0 (0.00) |
| z/χ2 | 0.777 | 5.413 | 5.764 | |||
| P value | 0.791 | 0.020 | 0.006 | |||
The number of older patients undergoing hip replacement is increasing every year, and their average hospital stay duration is only approximately 2 weeks; therefore, they cannot receive long-term functional training nursing care in the hospital after surgery[10]. However, patients often require approximately 6 months of functional training after surgery to restore limb function to the preoperative state. The recovery effect after hip replacement is not only related to the technical proficiency of a surgeon but also related to the long-term postoperative formal functional training of a patient[11]. However, most of the postoperative functional training of patients occurs after discharge, and their rehabilitation training activities are not within the professional supervision of medical staff.
Older patients often face difficulties in scientifically applying the rehabilitation nursing knowledge learned during their hospitalization to daily training. Continuous nursing is a method implemented outside the hospital that can meet the nursing needs of older patients after hip replacement[12]. Therefore, exploring the effect of continuous nursing on older patients with hip replacement is necessary. In this study, patients who received continuous nursing had increased Harris and SF-36 scores and decreased overall complication and readmission rates at 3 months and 6 months after discharge compared with those of patients who received routine nursing. Continuous nursing could promote the recovery of hip function, improve the quality of life of older patients undergoing hip replacement, reduce the incidence of postoperative complications, and reduce the possibility of readmission.
The Harris score is a widely used measure of hip function and is often used to evaluate the effectiveness of hip preservation and joint replacement. The SF-36 score is used to assess the patient’s health status and quality of life. Older patients who underwent hip replacement had poor initiative and unclear rehabilitation purpose in the rehabilitation process. Furthermore, the number, intensity, and time of rehabilitation training were often unorganized. The training time could be missed easily and was not adhered to for a long time. These factors were not conducive to the recovery of hip function after surgery. After discharge, patients were provided with functional training, scientific guidance, and psychological support through home visits and telephone follow-up. This is conducive to the smooth progress of scientific and reasonable rehabilitation training after discharge to promote the recovery of hip function and ensure the postoperative rehabilitation effect.
Continuous nursing was implemented to strengthen the isotonic muscle strength of patients, aid their caregivers outside the hospital, and improve attention to the prevention of hip dislocation and falls so that the daily training of patients after discharge was more systematic and scientific. In the continuous nursing process, the nursing staff de
The SF-36 score of patients receiving continuous nursing significantly increased, indicating that this nursing method had advantages in improving the overall health of patients, particularly physical health, physical function, emotional function, social function, physical pain, life vitality, mental health, and other aspects. Rehabilitation after hip replacement is a long-term process. Postoperative limb function defects lead to mobility inconvenience, which adversely affects patient physiology and psychology, resulting in poor quality of life[18]. Continuous nursing could relieve psychological anxiety and improve the psychological state of patients by providing them with health education, psychological support, and effective communication through out-of-hospital visits and follow-ups. Furthermore, planned health education for patients could help them master the appropriate rehabilitation methods, which are conducive to reducing the occurrence of complications[19], as was observed in the current study[20]. However, this study had some limitations. This was a single-center study with a small sample size, which may have led to selection bias. Moreover, this study was a retrospective study, and not a randomized controlled trial; thus, confounding bias may have occurred. Insufficient research may also skew the results. Therefore, randomized controlled trials and multicenter clinical studies are planned to confirm the results of this study.
Continuing care could significantly improve hip function and quality of life in older patients undergoing joint replacement and reduce the incidence of complications and the readmission rate.
| 1. | Hulshof CTJ, Pega F, Neupane S, Colosio C, Daams JG, Kc P, Kuijer PPFM, Mandic-Rajcevic S, Masci F, van der Molen HF, Nygård CH, Oakman J, Proper KI, Frings-Dresen MHW. The effect of occupational exposure to ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int. 2021;150:106349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | HEALTH Investigators; Bhandari M, Einhorn TA, Guyatt G, Schemitsch EH, Zura RD, Sprague S, Frihagen F, Guerra-Farfán E, Kleinlugtenbelt YV, Poolman RW, Rangan A, Bzovsky S, Heels-Ansdell D, Thabane L, Walter SD, Devereaux PJ. Total Hip Arthroplasty or Hemiarthroplasty for Hip Fracture. N Engl J Med. 2019;381:2199-2208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 286] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 3. | Ren Y, Cao SL, Li Z, Luo T, Feng B, Weng XS. Comparable efficacy of 100 mg aspirin twice daily and rivaroxaban for venous thromboembolism prophylaxis following primary total hip arthroplasty: a randomized controlled trial. Chin Med J (Engl). 2021;134:164-172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Wimberly AS, Hyatt JM, McKay JR. Effect of continuing care for people with cocaine dependence on criminal justice sentences. Behav Sci Law. 2018;36:116-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Rikard RV, Berkowsky RW, Cotten SR. Discontinued Information and Communication Technology Usage among Older Adults in Continuing Care Retirement Communities in the United States. Gerontology. 2018;64:188-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | McGillion MH, Parlow J, Borges FK, Marcucci M, Jacka M, Adili A, Lalu MM, Ouellette C, Bird M, Ofori S, Roshanov PS, Patel A, Yang H, O'Leary S, Tandon V, Hamilton GM, Mrkobrada M, Conen D, Harvey V, Lounsbury J, Mian R, Bangdiwala SI, Arellano R, Scott T, Guyatt GH, Gao P, Graham M, Nenshi R, Forster AJ, Nagappa M, Levesque K, Marosi K, Chaudhry S, Haider S, Deuchar L, LeBlanc B, McCartney CJL, Schemitsch EH, Vincent J, Pettit SM, DuMerton D, Paulin AD, Simunovic M, Williams DC, Halman S, Harlock J, Meyer RM, Taylor DA, Shanthanna H, Schlachta CM, Parry N, Pichora DR, Yousuf H, Peter E, Lamy A, Petch J, Moloo H, Sehmbi H, Waggott M, Shelley J, Belley-Cote EP, Devereaux PJ; PVC-RAM-1 Investigators. Post-discharge after surgery Virtual Care with Remote Automated Monitoring-1 (PVC-RAM-1) technology versus standard care: randomised controlled trial. BMJ. 2021;374:n2209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Magaziner J, Mangione KK, Orwig D, Baumgarten M, Magder L, Terrin M, Fortinsky RH, Gruber-Baldini AL, Beamer BA, Tosteson ANA, Kenny AM, Shardell M, Binder EF, Koval K, Resnick B, Miller R, Forman S, McBride R, Craik RL. Effect of a Multicomponent Home-Based Physical Therapy Intervention on Ambulation After Hip Fracture in Older Adults: The CAP Randomized Clinical Trial. JAMA. 2019;322:946-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 8. | Stirling P, Viamont-Guerra MR, Strom L, Chen AF, Saffarini M, Nover L, Laude F. Does Cup Position at the High Hip Center or Anatomic Hip Center in THA for Developmental Dysplasia of the Hip Result in Better Harris Hip Scores and Revision Incidence? A Systematic Review. Clin Orthop Relat Res. 2021;479:1119-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Hersnaes PN, Gromov K, Otte KS, Gebuhr PH, Troelsen A. Harris Hip Score and SF-36 following metal-on-metal total hip arthroplasty and hip resurfacing - a randomized controlled trial with 5-years follow up including 75 patients. BMC Musculoskelet Disord. 2021;22:781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Chen J, Yue C, He P, Huang Z, Li L, Zhang X, Fan Y, Liu Y. Comparison of clinical outcomes with hip replacement versus PFNA in the treatment of intertrochanteric fractures in the elderly: A systematic review and meta-analysis (PRISMA). Medicine (Baltimore). 2021;100:e24166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Svinøy OE, Bergland A, Risberg MA, Pripp AH, Hilde G. Better before-better after: efficacy of prehabilitation for older patients with osteoarthritis awaiting total hip replacement-a study protocol for a randomised controlled trial in South-Eastern Norway. BMJ Open. 2019;9:e031626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Dowzicky PM, Shah AA, Barg FK, Eriksen WT, McHugh MD, Kelz RR. An Assessment of Patient, Caregiver, and Clinician Perspectives on the Post-discharge Phase of Care. Ann Surg. 2021;273:719-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Toye C, Parsons R, Slatyer S, Aoun SM, Moorin R, Osseiran-Moisson R, Hill KD. Outcomes for family carers of a nurse-delivered hospital discharge intervention for older people (the Further Enabling Care at Home Program): Single blind randomised controlled trial. Int J Nurs Stud. 2016;64:32-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Aoun SM, Stegmann R, Slatyer S, Hill KD, Parsons R, Moorin R, Bronson M, Walsh D, Toye C. Hospital postdischarge intervention trialled with family caregivers of older people in Western Australia: potential translation into practice. BMJ Open. 2018;8:e022747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Pfluegler G, Borkovec M, Kasper J, McLean S. The immediate effects of passive hip joint mobilization on hip abductor/external rotator muscle strength in patients with anterior knee pain and impaired hip function. A randomized, placebo-controlled crossover trial. J Man Manip Ther. 2021;29:14-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 16. | Pevnick JM, Keller MS, Kennelty KA, Nuckols TK, Ko EM, Amer K, Anderson L, Armbruster C, Conti N, Fanikos J, Guan J, Knight E, Leang DW, Llamas-Sandoval R, Matta L, Moriarty D, Murry LT, Muske AM, Nguyen AT, Phung E, Rosen O, Rosen SL, Salandanan A, Shane R, Schnipper JL. The Pharmacist Discharge Care (PHARM-DC) study: A multicenter RCT of pharmacist-directed transitional care to reduce post-hospitalization utilization. Contemp Clin Trials. 2021;106:106419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Provencher V, Clemson L, Wales K, Cameron ID, Gitlin LN, Grenier A, Lannin NA. Supporting at-risk older adults transitioning from hospital to home: who benefits from an evidence-based patient-centered discharge planning intervention? Post-hoc analysis from a randomized trial. BMC Geriatr. 2020;20:84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 18. | Holsgaard-Larsen A, Hermann A, Zerahn B, Mejdahl S, Overgaard S. Effects of progressive resistance training prior to total HIP arthroplasty - a secondary analysis of a randomized controlled trial. Osteoarthritis Cartilage. 2020;28:1038-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Howie CM, Mears SC, Barnes CL, Stambough JB. Readmission, Complication, and Disposition Calculators in Total Joint Arthroplasty: A Systemic Review. J Arthroplasty. 2021;36:1823-1831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 20. | Zheng Y, Wang H, Wang H, Xu J, Chen P. The efficacy of a phone assistance nursing program for functional outcomes in patients after shoulder instability surgery: A protocol for randomized controlled trial. Medicine (Baltimore). 2020;99:e22756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |