Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4527
Revised: May 9, 2024
Accepted: June 13, 2024
Published online: July 26, 2024
Processing time: 111 Days and 9.7 Hours
Psychological intervention nursing (PIN) has been considered to have a curative effect on cesarean section (CS) post
To explore the effects of PIN combined with acupressure massage on CS post
A retrospective study was conducted on 150 pregnant women admitted to an obstetrics department between January 2020 and January 2023. The control group (CG) received acupressure therapy (n = 73), and the intervention group (IG) received acupressure therapy and PIN therapy (n = 77). Postoperative recovery time was assessed by anal-exhausting, defecation, bed activity, breastfeeding, and hospital stay times. Adverse effects, including infection, bleeding, limb numbness, intrauterine hematoma, urinary retention, and venous thromboembolism, were recorded. the pain visual analogue scale (VAS) was used to evaluate the degree of pain. Anxiety and depression status were qualitatively assessed using the self-rating anxiety scale (SAS), self-rating depression scale (SDS), and Edinburgh postpartum depression scale (EPDS). The Pittsburgh sleep quality index (PSQI) was used to compare sleep quality between the groups.
The baseline data and SAS, SDS, EPDS, and PSQI scores did not significantly differ before CS (P > 0.05) and neither did complication rates between the two groups after CS (P > 0.05). However, anal-exhausting, defecation, waking up, breastfeeding, and hospitalization times were significantly shorter for participants in the IG than those for participants in the CG (P < 0.05). The VAS, SAS, SDS, EPDS, and PSQI scores of the IG were significantly lower than those of the CG (P < 0.05).
PIN, combined with acupressure massage, effectively promotes maternal recovery, reduces post-CS pain, and improves post
Core Tip: The combination of acupressure and psychological care can significantly promote early recovery after cesarean delivery. This comprehensive intervention can effectively reduce pain after cesarean delivery and is beneficial in alleviating negative postpartum emotions and enhancing the psychological state of patients. Following the comprehensive intervention, the quality of maternal sleep is markedly enhanced, facilitating the promotion of physical recovery and health.
- Citation: Liu XY, Chen XB, Wen YL, Guo XP, Zhou XB. Effect of psychological nursing intervention combined with acupressure on postoperative recovery of women after cesarean section. World J Clin Cases 2024; 12(21): 4527-4535
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4527.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4527
Cesarean section (CS) is currently the most common major surgery worldwide. The World Health Organization estimates that approximately 15% of deliveries are performed via CS[1]. However, post-CS pain is inevitable, with 53.7% of all patients experiencing severe pain that is related to decreased sleeping quality and impairment of mood[2,3]. Furthermore, CS-related pain is positively associated with the occurrence of postpartum depression[4]. Regarding the relationship between newborns and the mother, post-CS pain poses a potential challenge into impacting the holistic health, quality of interaction, and even early initiation of breastfeeding[5]. Post-CS pain is also associated with a decrease in daily activity recovery[6].
The current primary treatment for post-CS pain involves using analgesic medications[7]. However, concerns about potential adverse effects of analgesic medications on maternal and infant health often restrict their use. The pharmacokinetic and pharmacological properties of certain anesthetic drugs can pose a potential risk of interfering with early breastfeeding[8]. Moreover, adverse reactions, such as vomiting, occur more frequently[9]. Additionally, the use of opioid analgesics during CS is associated with increased occurrence of sedation and respiratory suppression[10,11]. Conse
However, the improvement of postoperative negative emotions and sleeping quality with analgesic medications remains controversial[13,14]. A meta-analysis indicated that factors such as the maternal age, body mass index (BMI), and administration of analgesic drugs contributed to heterogenous conclusions for the effectiveness of managing postoperative negative emotions[9]. Additionally, one-third of pregnant women experience significant delivery-related mental stress that not only resulted in perinatal depression but also possibly induced childbirth-related post-traumatic stress disorder[15], which occurs in 5%–6% of all postpartum women and can reach 18.5%–41.2% in complex deliveries[16]. Therefore, early psychological interventions could contribute to beneficial outcomes of mental health for post-CS women. Two studies have indicated positive correlations between poor sleeping quality and intensified post-CS pain with an increased dose of analgesic drugs and low birth-weight of newborns[17,18]. Hence, negative emotions and enhancing sleeping quality should be proactively addressed as soon as possible.
Psychological intervention nursing (PIN) integrates psychological intervention based on the Information-Motivation-Behavioral Skills (IMB) model into nursing practices to support maternal mental health. PIN provides information, boosts motivation, and imparts the essential skills to adopt healthy behaviors, strengthen psychological adaptations, improve mental health conditions, and enhance treatment outcomes[19,20]. Xu et al[21] found that applying the IMB model in psychological interventions effectively mitigated anxiety and depressive feelings in postpartum mothers.
Currently, PIN and targeted acupressure massage are classified as complementary alternative therapies, offering promising opportunities to alleviate post-CS pain, reduce adverse emotional states, and improve sleeping quality[7]. Therefore, this study aimed to explore the effects of combining PIN with acupressure massage on effectively promoting maternal recovery, reducing post-CS pain, and improving postoperative negative emotions and sleeping quality.
This study retrospectively collected data on 150 pregnant women admitted to the Second Affiliated Hospital of Gannan Medical University from January 2020 to January 2023. Participants were divided based on their different treatment regimens: (1) The control group (CG) that included 73 individuals who received hand acupoint massage during hospitalization; and (2) the intervention group (IG) 77 individuals who received psychological intervention in addition to hand acupoint massage.
Inclusion criteria were: (1) Patients aged 18-35 years old; (2) Voluntary choice of CS to terminate the pregnancy and successful completion of CS without death; (3) Meeting the indication for elective CS and undergoing a lower segment transverse CS; and (4) An interval of > 18 months between the previous CS and the current one.
Exclusion criteria were: (1) A history of mental illness and sleep disorders; (2) The presence of cognitive and language communication barriers; (3) The presence of other serious underlying diseases, organ dysfunction, and malignant tumors; and (4) An inability to tolerate acupoint massage.
The IG of postpartum women received individualized PIN based on the IMB model in addition to acupoint massage. Detailed measures included information, motivation, and behavioral skills interventions.
Information intervention involved nurses collecting basic information, such as age, income, family relationships, and occupation, through questionnaires and face-to-face communication upon admission. This process also gathered data on relevant illnesses, treatment methods, pain education, psychological status, and emotional support. Nurses introduced the basic nursing knowledge (surgical-related information, operating room and ward environments, precautions, and points of cooperation), procedure of CS, the epidemiology of CS complications, and key points for post-CS recovery, ensuring patients had a comprehensive understanding of CS. Nurses compiled these details into the health brochure and distributed this to every postpartum woman in the IG. Meanwhile, nurses patiently addressed participant inquiries to provide psychological counseling and communication support.
Motivational intervention was conducted based on the psychological stage of the patient: (1) Unconscious stage: Establishing trust with pregnant women, engaging in sincere communication, encouraging them to share their thoughts, patiently listening, expressing understanding, and answering their questions thoroughly. Understanding the psychological needs and changes of pregnant women, providing 1-2 postoperative recovery success stories to boost their confidence and help establish trust between nurses and pregnant women; (2) Intention period: Before the CS operation, providing detailed explanations to patients about the significance of CS, surgical procedures, potential risks, precautions, prognosis, and the importance of moderate activity after CS. Listing potential consequences of negative behaviors and attitudes in writing and informing patients that behavioral changes can significantly avoid these serious consequences; (3) Preparation stage: Guiding pregnant women to express their willingness to adopt healthy behaviors, discussing and setting short-term goals with pregnant women, analyzing their feasibility, and helping them build confidence; (4) Change stage: Assisting pregnant women in establishing post-CS recovery goals and implementation plans and ensuring their feasibility, communicating with pregnant women, guiding them to review CS-related knowledge, identifying pregnant women with low completion of stage goals in a timely manner, analyzing the reasons for this, and devising new motivational support strategies; and (5) Maintenance stage: Encouraging pregnant women to make full use of existing resources, maintaining long-term healthy behaviors. Encouraging the active involvement of family members, increasing communication with pregnant women, advising family members to provide more care and support, and encouraging com
Behavioral skills intervention: (1) Detailed preoperative explanation to patients, regarding potential discomfort and complications during CS. Discussing the safety and prognosis of the CS to encourage active patient cooperation; (2) Rapid recovery of behavioral skills: Within 6-hour post-CS, women could lay flat without a pillow; at 2-hour post-surgery, patients were assisted in the first passive turning, followed by subsequent turns every 2 hours. Passive or active turning and small-range flexion and extension exercises were conducted for hip, ankle, and knee joints based on the recovery status of the patient to strengthen leg muscles. Exercises included straight leg lifts, knee bending, and dorsal flexion and extension to reinforce abdominal muscle strength; hanging back and bending both legs to strengthen back muscles; Kegel exercises for pelvic floor muscles and fascia. During Kegel exercises, women adopted a free body position, attempting to contract the urethra, anus, and perineum for 5–10 seconds, performed three times a day for 5 minutes each, and resting for 5–10 seconds between exercises based on the patient condition. All exercises were adjusted according to the recovery status of the patient and immediately discontinued if any discomfort was noticed. The intensity of exercises could be adjusted for subsequent sessions based on the previous maximum intensity. Once the lower limb muscle strength reached level 4, the patient could start assisted ambulation with the help of nursing staff and family members, consume liquid food, pass gas through the anus after 24 hours, and have the catheter removed for urination 24-48 hours post-surgery; (3) Social and family support: Family members received guidance on breastfeeding and assisting the mother with breastfeeding for the first time. Tailored and reasonable dietary plans were designed based on individual female needs for adequate nutrition and energy. Encouragement was provided to family members to strictly adhere to the nutritional supplementation requirements for the postpartum woman; and (4) Self-regulation strategies: Immediate reporting and close monitoring of any post-CS discomfort and proactive execution of corresponding rapid recovery behavioral tasks. Considering that the CS incision typically heals within approximately 5 weeks, mothers were provided guidelines for managing incision health and encouraged to monitor the condition of the wound.
The nursing staff applies lubricating oil to their palms and rubs them together to generate warmth. Using the palm or the edge of the hand, they perform circular movements firmly against the area around the navel, upper abdomen, and both sides of the abdomen, rotating the hands in a clockwise manner, alternating between them for 10 minutes. Subsequently, they target acupoints: Zhongwan (located on the anterior midline, four inches above the navel), Xiawan (located on the anterior midline, two inches above the navel), and Tianshu (located two inches lateral to the navel), massaging each acupoint for 10 minutes. These procedures are performed three times a day, and self-massage is permissible if the mother experiences significant pain. The massage technique should be gentle, incorporating intermittent deep pressure and acupressure techniques, while attentively monitoring the tolerance of the expectant mother to the acupoint massage.
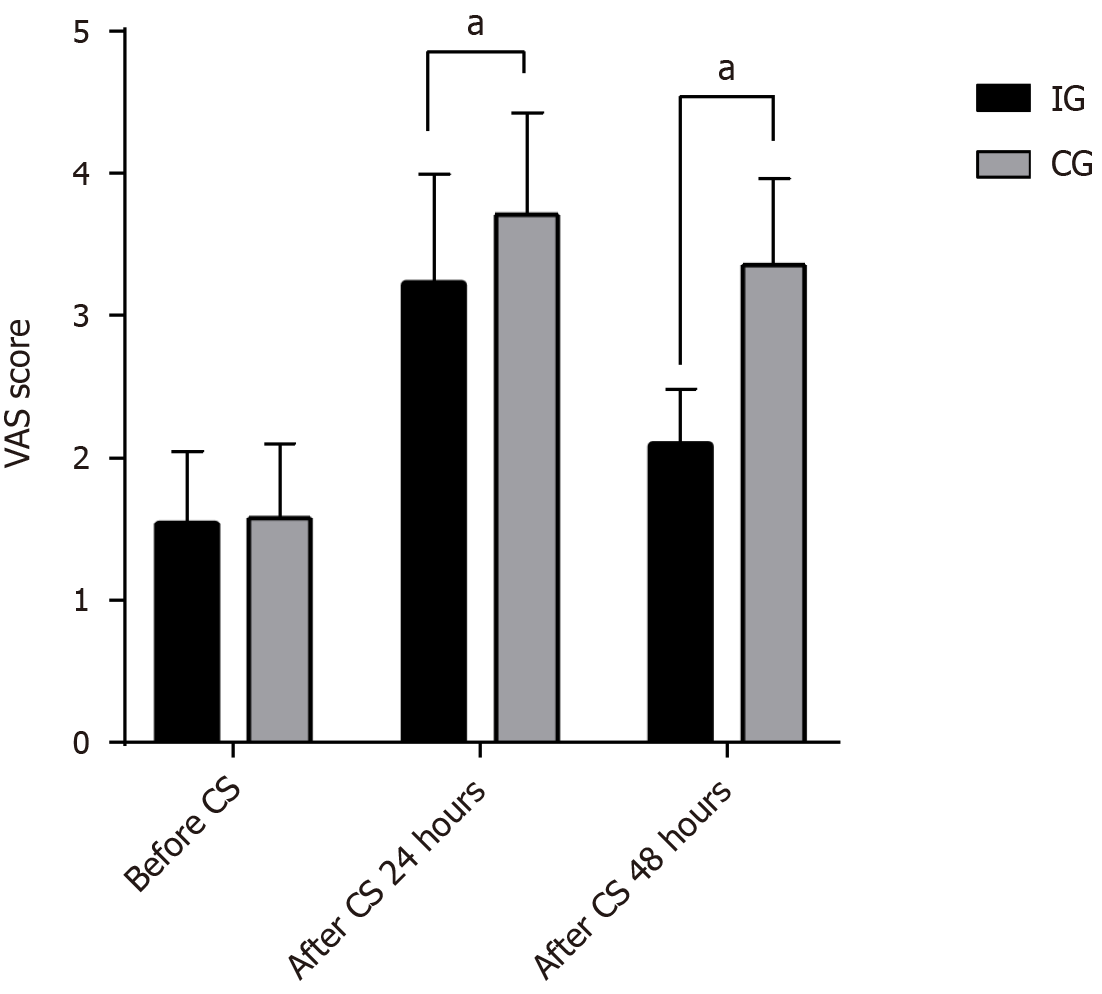
Baseline data included the age, gestational weeks, use of patient-controlled intravenous analgesia (PCIA), gestational period (premature, full-term, and overdue birth), history of prior CS, and reasons for the current CS (fetal distress, pregnancy complications, voluntary request) collected from two groups of patients. To assess the postoperative recovery time, we compared times for anus-exhausting, defecation, out-of-bed activity, breastfeeding, and hospital stay between the two groups. Regarding complications, we observed and recorded postoperative complications such as infection, bleeding, lower limb numbness, intrauterine hematoma, urinary retention, and venous thromboembolism in the two groups. Additionally, the pain visual analogue scale (VAS) scores were performed to observe the degree of pain at pre-CS, and at 24- and 48-hour post-CS in the two groups. The total score of VAS ranges from 0 to 10, with higher scores indicating stronger pain.
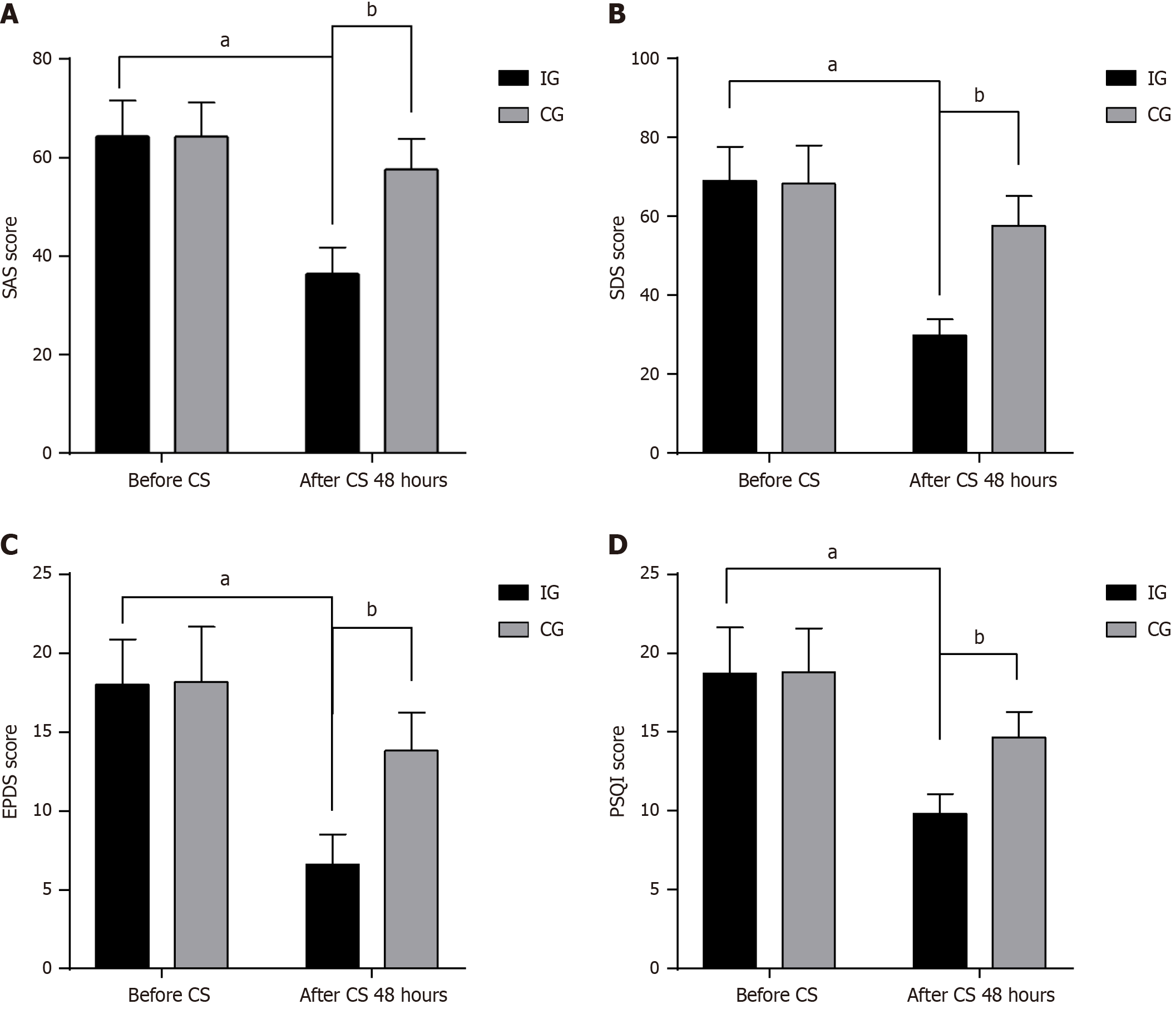
Evaluations of postoperative negative emotions included the administration of the self-rating anxiety scale (SAS), self-rating depression scale (SDS), and Edinburgh postpartum depression scale (EPDS) to compare negative emotions at pre-CS and 48-h post-CS in the two groups. The SAS and SDS each contain 20 items, each of which is scored from 0-4. The higher the total score, the higher the degree of anxiety and depression. The EPDS contains 10 items, each item of which is scored from 0-3. The higher the total score, the higher the degree of depression.
The assessment and comparison of sleep quality between the two groups of patients were conducted using the Pittsburgh sleep quality index (PSQI) before and 48 hours after the surgical procedure. The total score of the PSQI ranges from 0 to 21. A higher total score indicates a lower sleeping quality.
SPSS 26.0 software was used for statistical analysis. Continuous variables are presented as mean ± SD, while categorical variables are presented as n (%). Independent sample t-tests were used to compare intergroup differences for continuous variables, and paired sample t-tests were used to compare pre- and posttreatment differences. For categorical variables, the differences between groups were assessed using the χ2 test, Fisher’s exact probability test and rank-sum test. A significance level of 0.05 indicates a significant difference.
In this study, 77 and 73 pregnant women were respectively allocated to two groups: IG and CG. The groups did not significantly differ in age, gestational weeks, BMI, cesarean history, use of PCIA, gestational period, or reasons for CS (P > 0.05).
The age of IG and CG participants was 29.51 ± 3.66 years and 29.36 ± 3.58 years, respectively. The gestational weeks of IG and CG participants were 39.15 ± 2.08 weeks and 39.21 ± 1.99 weeks, respectively. The BMI of IG and CG participants was 22.97 ± 0.93 kg/m2 and 22.89 ± 0.96 kg/m2, respectively (Table 1).
| Baseline data | IG (n = 77) | CG (n = 73) | t/χ2 | P value |
| Age, year | 29.64 ± 3.43 | 29.01 ± 3.33 | 1.134 | 0.258 |
| Gestational weeks, weeks | 39.23 ± 2.00 | 38.96 ± 1.70 | 0.906 | 0.367 |
| BMI, kg/m2 | 23.00 ± 0.87 | 22.93 ± 0.90 | 0.476 | 0.635 |
| Cesarean history | 0.018 | 0.894 | ||
| Nulliparas | 43 (55.84) | 39 (53.42) | ||
| Multiparas | 34 (44.16) | 34 (46.58) | ||
| Use of PCIA | 70 (90.90) | 65 (89.04) | 0.012 | 0.913 |
| Gestational period | - | 0.785 | ||
| Premature birth | 4 (5.19) | 5 (6.85) | ||
| Full-term birth | 70 (90.90) | 64 (87.67) | ||
| Overdue birth | 3 (3.91) | 4 (5.48) | ||
| Reasons of CS | 0.385 | 0.825 | ||
| Fetal distress | 9 (11.69) | 7 (9.59) | ||
| Pregnancy complications | 21 (27.27) | 18 (24.66) | ||
| Voluntary request | 47 (61.04) | 48 (65.75) |
In the IG, the proportion of pregnant women with nulliparas or multiparas was 53.42% and 44.16%, respectively, and in the CG, this was 46.58% and 44.16%, respectively. The proportion of pregnant women in the IG and CG who accepted PCIA was 90.90% and 89.04%, respectively. In the gestational period, the proportion of pregnant women in the IG and CG with premature birth was 5.19% and 6.85%, with full-term birth was 90.90% and 87.67%, and with overdue birth was 3.91% and 5.48%, respectively. For the reasons for CS, the proportion of pregnant women in the IG and CG with fetal distress was 11.69% and 9.59%, with pregnancy complications was 27.27% and 24.66%, and with voluntary request was 61.04% and 65.75%, respectively.
Compared with participants in the CG, those in the IG exhibited shortened postoperative recovery times for anus-exhausting, defecation, out-of-bed activity, breastfeeding, and hospital stay. Anus-exhausting times of the IG and CG were 17.17 ± 2.88 hours and 19.63 ± 5.34 hours, respectively (P < 0.05). Defecation times of the IG and CG were 28.27 ± 2.97 hours and 30.76 ± 2.62 hours, respectively (P < 0.05). Out-of-bed activity times of the IG and CG were 18.72 ± 3.12 hours and 20.04 ± 4.12 hours, respectively (P < 0.05). Breastfeeding times of the IG and CG were 22.70 ± 1.84 hours and 23.37 ± 1.71 hours, respectively (P < 0.05). Hospital stay times of the IG and CG were 5.66 ± 1.12 days and 6.29 ± 1.34 days, respectively (P < 0.05; Table 2).
| Postoperative recovery time | IG (n = 77) | CG (n = 73) | t value | P value |
| Anus exhausting time, hour | 17.19 ± 2.88 | 19.63 ± 5.34 | 3.504 | 0.001 |
| Defecation time, hour | 28.27 ± 2.97 | 30.76 ± 2.62 | 5.429 | < 0.001 |
| Out-of-bed activity time, hour | 18.72 ± 3.12 | 20.04 ± 4.12 | 2.235 | 0.027 |
| Breastfeeding time, hour | 22.70 ± 1.84 | 23.37 ± 1.71 | 2.316 | 0.022 |
| Hospital stay time, day | 5.66 ± 1.12 | 6.29 ± 1.34 | 2.980 | 0.003 |
In terms of the incidence of complications, no significant differences were present between the IG and CG in the incidence of infection, bleeding, limb numbness, intrauterine hematoma, urinary retention, or venous thromboembolism (P > 0.05; Table 3).
| Complications | IG (n = 77) | CG (n = 73) | χ2 | P value |
| Infections | 0 (0.00) | 3 (4.11) | - | 0.113 |
| Bleeding | 1 (1.30) | 4 (5.48) | - | 0.201 |
| Limb numbness | 1 (1.30) | 3 (4.11) | - | 0.357 |
| Intrauterine hematoma | 0 (0.00) | 1 (1.37) | - | 1.000 |
| Urinary retention | 0 (0.00) | 3 (4.11) | - | 0.113 |
| Venous thromboembolism | 0 (0.00) | 1 (1.37) | - | 1.000 |
As shown in Figure 1, the VAS scores before CS did not significantly differ between the two groups (P > 0.05), with the IG at 1.55 ± 0.50 and the CG at 1.58 ± 0.53. At 24-hour post-CS, the VAS scores of the IG were significantly lower than those of the CG (P < 0.05) at 3.23 ± 0.76 and 3.71 ± 0.72 (P < 0.05), respectively. At 48-hour post-CS, the VAS scores of the IG were significantly lower than those of the CG (P < 0.05) at 2.10 ± 0.38 and 3.36 ± 0.61, respectively.
This study used the SAS, SDS, and EPDS scores to quantitatively evaluate the postoperative negative emotions, especially in depression and anxiety (Figure 2). The SAS scores did not significantly differ between the IG and CG before CS (P > 0.05), with scores of 64.33 ± 6.87 and 64.39 ± 7.17, respectively. However, at 48-hour post-CS, the IG scores were significantly lower than the CG scores (P < 0.05) at 36.44 ± 5.32 and 57.63 ± 6.21, respectively. The SDS scores, did not significantly differ between the IG and CG before CS (P > 0.05), with scores of 69.05 ± 8.54 and 68.33 ± 9.62, respectively. However, at 48-hour post-CS, the IG scores were significantly lower than the CG scores (P < 0.05) at 29.83 ± 4.03 and 57.62 ± 7.49, respectively. The EPDS scores did not significantly differ between the IG and CG before CS (P > 0.05), with scores of 18.01 ± 2.88 and 18.18 ± 3.51, respectively. However, at 48-h post-CS, the IG scores were significantly lower than the CG scores (P < 0.05) at 6.61 ± 1.91 and 13.82 ± 2.42, respectively.
This study also used the PSQI score to quantitatively evaluate the sleeping quality (Figure 2). The PSQI scores did not significantly differ between the IG and CG before CS (P > 0.05), with scores of 18.71 ± 2.77 and 18.81 ± 2.92, respectively. However, at 48-hour post-CS, the IG scores were significantly lower than the CG scores (P < 0.05) at 9.83 ± 1.24 and 14.68 ± 1.59, respectively.
Although CS can resolve some complex pregnancy issues, this causes significant trauma to the maternal body[22]. Post-CS pain restricts movement, delaying early activity and affects the postpartum recovery, lactation, and breastfeeding[5]. Pain may cause reluctance in breastfeeding or reduced nursing sessions due to discomfort. Furthermore, post-CS pain impacts the sleep quality of the mother, decreasing high-quality sleep or causing frequent awakenings[2]. This continuous discomfort may cause fatigue and anxiety, hindering both physical recovery and mental well-being[23]. Post-CS pain could exacerbate anxiety, depression, and reduced sleeping quality, forming a vicious cycle where negative emotions and low-quality sleep mutually exacerbate the degree of pain[17,24,25]. Therefore, choosing safe and effective pain management coupled with psychological intervention is crucial. This study aimed to apply psychological intervention combined with acupressure massage and then observe the postoperative recovery time, complications, degree of pain, emotional state, and sleeping quality in pregnant women.
This study found that postoperative anus-exhausting, defecation, out-of-bed activity, breastfeeding, and hospital stay times were shorter in those receiving psychological intervention care. This suggests that psychological intervention care combined with acupressure massage could effectively promote early recovery. Moreover, the IG participants had lower VAS scores, indicating better pain relief compared with acupressure massage alone. Additionally, our research demonstrates that pregnant women receiving PIN had significantly lower SAS, SDS, EPDS, and PSQI scores than those in the CG. This implies that PIN can effectively improve postoperatively negative emotions in pregnant women. These research findings are similar to those in other studies[22,26,27]. However, the two groups did not show a difference in the incidence of complications, which could be associated with the relatively small sample number. Additionally, psychological intervention measures could enhance pain-relief effectiveness of analgesic medications. Haiying et al[28] found that under intravenous analgesia with naloxone and butorphanol, psychological intervention significantly alleviated anxiety and improved relief of perioperative pain. Furthermore, psychological intervention measures can reduce adverse emotions among specific groups of pregnant women, such as those experiencing high or severe levels of fear of childbirth[29].
Therefore, using the IMB model to analyze the potential reasons discussed above leads to the following conclusions: (1) Information intervention: pregnant women may lack an objective understanding of pregnancy and childbirth-related knowledge, leading to concerns about maternal and infant health, which can cause anxiety, depression, and other negative emotions. Additionally, anesthesia and surgical trauma may cause physiological and psychological stress reactions in mothers[25]. These negative emotions may increase serotonin secretion, reducing the tolerance of the mother to pain[30]. Using the IMB model, patients could gain more detailed knowledge about CS and postpartum recovery, which may help alleviate postpartum psychological stress and enhance recovery confidence; (2) Motivation intervention may help to establish a correct understanding of CS and encourage involvement of family and society. These measures help strengthen the attention paid by pregnant women to their health, correcting their mindsets from a psychological standpoint, and emphasizing postpartum recovery; and (3) Behavioral intervention assists postpartum women in correctly conducting early recovery training and effectively controlling postpartum pain. These interventions guide postpartum women to adapt better to physiological changes post-surgery and aid in their faster recovery.
Based on acupressure massage, PIN promoted early recovery, controlled post-CS pain, and improved negative emotions and sleeping quality. However, this study has some limitations because of the small sample size, the limited number of observed indicators, and a short postpartum follow-up period, potentially leading to limited and biased conclusions.
| 1. | Parasiliti M, Vidiri A, Perelli F, Scambia G, Lanzone A, Cavaliere AF. Cesarean section rate: navigating the gap between WHO recommended range and current obstetrical challenges. J Matern Fetal Neonatal Med. 2023;36:2284112. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Emrich NLA, Tascón Padrón L, Komann M, Arnold C, Dreiling J, Meißner W, Strizek B, Gembruch U, Jiménez Cruz J. Risk Factors for Severe Pain and Impairment of Daily Life Activities after Cesarean Section-A Prospective Multi-Center Study of 11,932 Patients. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Ryali S, Kumar MS, Ryali VSSR, Paspulati S. Is cesarean section a clinical marker for psychiatric and sleep disorder in young mothers? A cross-sectional study from rural South India. Ind Psychiatry J. 2023;32:158-163. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Agarwal P, Dasari P, Sarkar S. Mode of Delivery and Postpartum Depression: A Cohort Study. J Obstet Gynaecol India. 2023;73:88-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Hooda R, Malik N, Pathak P, More H, Singh V. Impact of Postoperative Pain on Early Initiation of Breastfeeding and Ambulation After Cesarean Section: A Randomized Trial. Breastfeed Med. 2023;18:132-137. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Sharpe EE, Booth JL, Houle TT, Pan PH, Harris LC, Aschenbrenner CA, Eisenach JC. Recovery of physical activity after cesarean delivery and its relationship with pain. Pain. 2019;160:2350-2357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Zimpel SA, Torloni MR, Porfírio GJ, Flumignan RL, da Silva EM. Complementary and alternative therapies for post-caesarean pain. Cochrane Database Syst Rev. 2020;9:CD011216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Wilińska M, Walas W, Kamińska E, Malec Milewska M, Sękowska A, Helwich E. Do drugs used in obstetric anesthesia interfere with early breastfeeding? Characteristics of the pharmacodynamic and pharmacokinetic properties of certain drugs. Part 2. Dev Period Med. 2019;23:233-244. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Li Q, Wang S, Mei X. A single intravenous administration of a sub-anesthetic ketamine dose during the perioperative period of cesarean section for preventing postpartum depression: A meta-analysis. Psychiatry Res. 2022;310:114396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 10. | Ching Wong SS, Cheung CW. Analgesic Efficacy and Adverse Effects of Meperidine in Managing Postoperative or Labor Pain: A Narrative Review of Randomized Controlled Trials. Pain Physician. 2020;23:175-201. [PubMed] |
| 11. | Bauchat JR, Weiniger CF, Sultan P, Habib AS, Ando K, Kowalczyk JJ, Kato R, George RB, Palmer CM, Carvalho B. Society for Obstetric Anesthesia and Perinatology Consensus Statement: Monitoring Recommendations for Prevention and Detection of Respiratory Depression Associated With Administration of Neuraxial Morphine for Cesarean Delivery Analgesia. Anesth Analg. 2019;129:458-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 12. | Chen Y, Xiang XY, Chin KHR, Gao J, Wu J, Lao L, Chen H. Acupressure for labor pain management: a systematic review and meta-analysis of randomized controlled trials. Acupunct Med. 2021;39:243-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Liu QR, Zong QK, Ding LL, Dai HY, Sun Y, Dong YY, Ren ZY, Hashimoto K, Yang JJ. Effects of perioperative use of esketamine on postpartum depression risk in patients undergoing cesarean section: A randomized controlled trial. J Affect Disord. 2023;339:815-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 14. | Guo Y, Ding X, Wang S, Wang F, Zheng Z, Zou L. Analgesic Effect of Esketamine Combined with Tramadol for Patient-Controlled Intravenous Analgesia After Cesarean Section: A Randomized Controlled Trial. J Pain Res. 2023;16:3519-3528. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 15. | Dekel S, Stuebe C, Dishy G. Childbirth Induced Posttraumatic Stress Syndrome: A Systematic Review of Prevalence and Risk Factors. Front Psychol. 2017;8:560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 184] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 16. | Yildiz PD, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. J Affect Disord. 2017;208:634-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 403] [Article Influence: 50.4] [Reference Citation Analysis (0)] |
| 17. | Orbach-Zinger S, Fireman S, Ben-Haroush A, Karoush T, Klein Z, Mazarib N, Artyukh A, Chen R, Ioscovich A, Eidelman LA, Landau R. Preoperative sleep quality predicts postoperative pain after planned caesarean delivery. Eur J Pain. 2017;21:787-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 18. | Peltonen H, Paavonen EJ, Saarenpää-Heikkilä O, Vahlberg T, Paunio T, Polo-Kantola P. Sleep disturbances and depressive and anxiety symptoms during pregnancy: associations with delivery and newborn health. Arch Gynecol Obstet. 2023;307:715-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Yao X, Zhang L, Du J, Gao L. Effect of Information-Motivation-Behavioral Model Based on Protection Motivation Theory on the Psychological Resilience and Quality of Life of Patients with Type 2 DM. Psychiatr Q. 2021;92:49-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Lee SG, Kim B. Factors Affecting Nurses' Health Promotion Behavior during the COVID-19 Pandemic Based on the Information-Motivation-Behavioral Skills Model. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Xu L, Fang L, Xu Q, Shen D. Study on the effect of intervention on postpartum psychological improvement and body recovery of caesarean section women based on information-motivation-behavioural skills model. Nurs Open. 2023;10:4705-4712. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Chen I, Opiyo N, Tavender E, Mortazhejri S, Rader T, Petkovic J, Yogasingam S, Taljaard M, Agarwal S, Laopaiboon M, Wasiak J, Khunpradit S, Lumbiganon P, Gruen RL, Betran AP. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst Rev. 2018;9:CD005528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 23. | Wilson JM, He J, Flowers KM, Kovacheva V, Soens M, Schreiber KL. Pain Severity and Pain Interference in Late Pregnancy: An Analysis of Biopsychosocial Factors Among Women Scheduled for Cesarean Delivery. Pain Med. 2023;24:652-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 24. | Gamez BH, Habib AS. Predicting Severity of Acute Pain After Cesarean Delivery: A Narrative Review. Anesth Analg. 2018;126:1606-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 25. | Lin R, Lu Y, Luo W, Zhang B, Liu Z, Xu Z. Risk factors for postpartum depression in women undergoing elective cesarean section: A prospective cohort study. Front Med (Lausanne). 2022;9:1001855. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 26. | Fenwick J, Toohill J, Gamble J, Creedy DK, Buist A, Turkstra E, Sneddon A, Scuffham PA, Ryding EL. Effects of a midwife psycho-education intervention to reduce childbirth fear on women's birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth. 2015;15:284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 27. | Saisto T, Salmela-Aro K, Nurmi JE, Könönen T, Halmesmäki E. A randomized controlled trial of intervention in fear of childbirth. Obstet Gynecol. 2001;98:820-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 28. | Haiying Z, Lijun Z, Yanjun L, Peiwu C, Aiyu W. Postoperative analgesic effect of different doses of naloxone combined with butorphanol and psychological nursing intervention. Pak J Pharm Sci. 2018;31:2229-2234. [PubMed] |
| 29. | Striebich S, Mattern E, Ayerle GM. Support for pregnant women identified with fear of childbirth (FOC)/tokophobia - A systematic review of approaches and interventions. Midwifery. 2018;61:97-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 82] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 30. | Chalermkitpanit P, Thonnagith A, Engsusophon P, Charuluxananan S, Honsawek S. Noradrenaline, Serotonin, GABA, and Glycine in Cerebrospinal Fluid during Labor Pain: A Cross-Sectional Prospective Study. Pain Res Manag. 2017;2017:2752658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |