Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4508
Revised: May 6, 2024
Accepted: June 6, 2024
Published online: July 26, 2024
Processing time: 119 Days and 5.3 Hours
Pelvic floor dysfunction (PFD) is related to muscle fiber tearing during childbirth, negatively impacting postpartum quality of life of parturient. Appropriate and effective intervention is necessary to promote PFD recovery.
To analyze the use of hydrogen peroxide and silver ion disinfection for vaginal electrodes in conjunction with comprehensive rehabilitation therapy for postpar
A total of 59 women with PFD who were admitted to the hospital from May 2019 to July 2022 were divided into two groups: Control group (n = 27) received comprehensive rehabilitation therapy and observation group (n = 32) received intervention with pelvic floor biostimulation feedback instrument in addition to comprehensive rehabilitation therapy. The vaginal electrodes were disinfected with hydrogen peroxide and silver ion before treatment. Intervention for both groups was started 6 weeks postpartum, and rehabilitation lasted for 3 months. Pelvic floor muscle voltage, pelvic floor muscle strength, vaginal muscle voltage, vaginal muscle tone, pelvic floor function, quality of life, and incidence of post
Before comprehensive rehabilitation treatment, basic data and pelvic floor func
The combination of the pelvic floor biostimulation feedback instrument and comprehensive rehabilitation nursing can improve pelvic floor muscle strength, promote the recovery of vaginal muscle tone, and improve pelvic floor function and quality of life. The use of hydrogen peroxide and silver ion disinfectant demonstrated favorable antibacterial efficacy and is worthy of clinical application.
Core Tip: Pelvic floor dysfunction (PFD), a common disease in obstetrics and gynecology, is closely related to pregnancy and childbirth. PFD can significantly affect postpartum quality of life. This study compared the clinical effect of pelvic floor biostimulation feedback instrument intervention in patients with PFD based on comprehensive rehabilitation therapy and simple comprehensive rehabilitation treatment. The findings revealed the clinical advantages of pelvic floor biostimulation feedback instrument intervention from the perspectives of pelvic floor muscle voltage and strength, vaginal muscle voltage and tone, pelvic floor function, quality of life, and postpartum PFD incidence. Intervention with the pelvic floor biostimulation feedback instrument is a better choice for improving pelvic floor function and quality of life in patients with PFD.
- Citation: Zhou W, Guo H. Curative effect of hydrogen peroxide combined with silver ion disinfection on pelvic floor dysfunction. World J Clin Cases 2024; 12(21): 4508-4517
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4508.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4508
Pelvic floor dysfunction (PFD) is a common disease in obstetrics and gynecology, primarily caused by structural damage and functional defects in pelvic floor muscles. Symptoms of PFD may include stress urinary incontinence and uterine prolapse[1]. Pregnancy and delivery are the main factors contributing to PFD, because the growing fetus increases the size of the uterus, putting additional pressure on the pelvic floor supporting tissue, resulting in ligament relaxation and weakened pelvic floor support. During delivery, the tearing of muscle fibers further weakens the pelvic floor, leading to PFD, which significantly impacts postpartum quality of life[2,3].
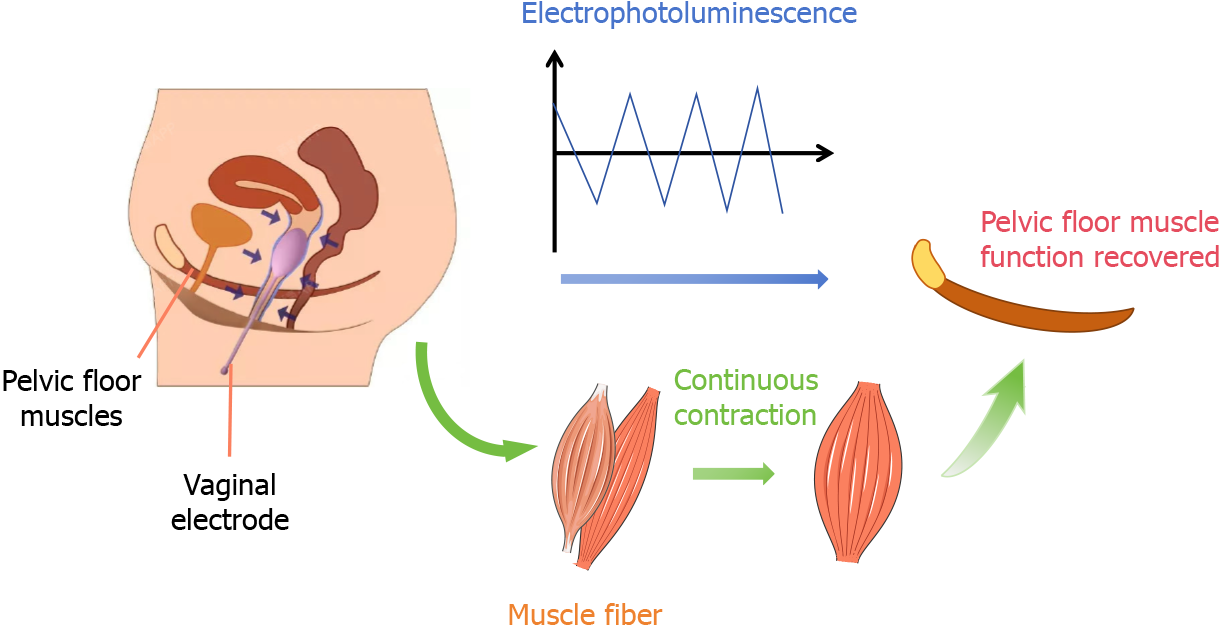
Pelvic floor rehabilitation is critical for parturient women. Most clinical rehabilitation treatments include pelvic floor muscle function training and electrical stimulation therapy. Comprehensive rehabilitation therapy aims to enhance the contractile force of pelvic floor muscles, reduce the occurrence of uterine prolapse and other symptoms, and restore the muscles to their prepregnancy state through pelvic floor muscle training. However, the improvement achieved using this method is limited[4,5]. Therefore, a passive pelvic floor rehabilitation training instrument, called the pelvic floor biostimulation feedback instrument, has been developed. This device uses different intensity currents applied to electrodes placed in the vagina to improve neuromuscular excitability, rhythmically contract pelvic floor muscles and nerves, and promote the functional recovery of the pelvic floor. This method, combined with pelvic floor muscle rehabilitation training, provides better treatment outcomes[6] (Figure 1).
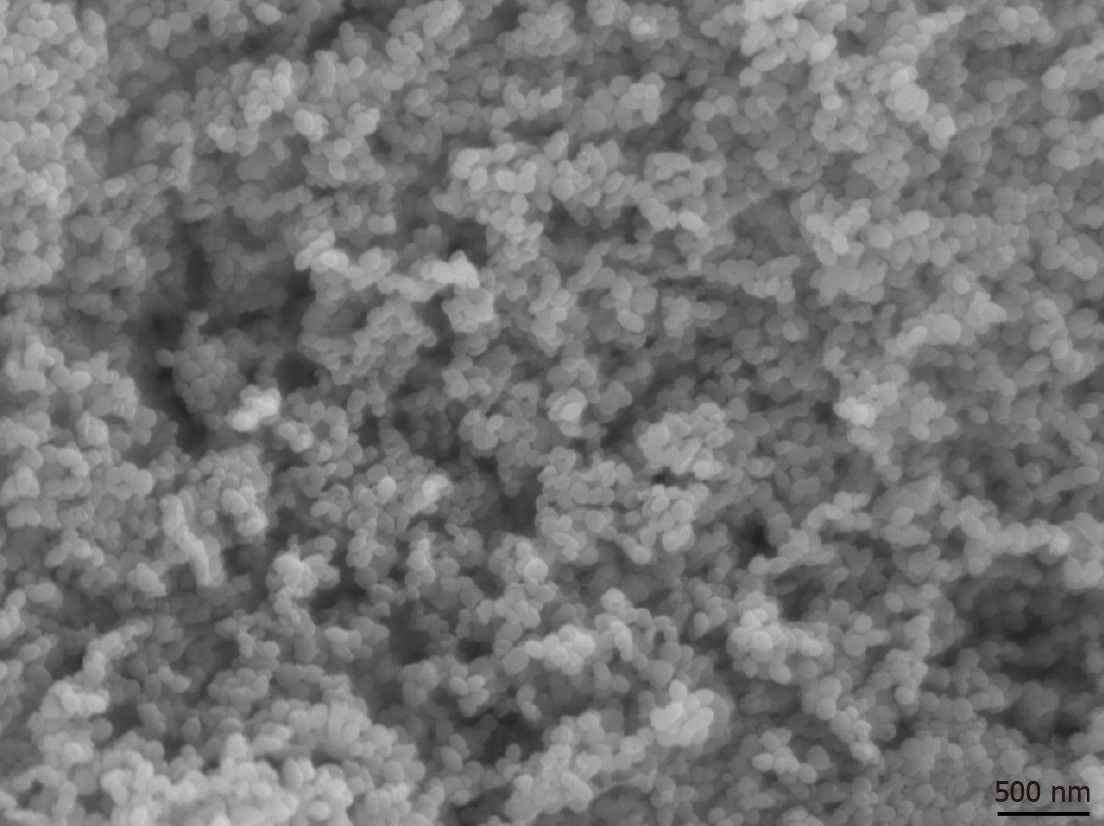
To reduce the incidence of infection during treatment, the vaginal electrodes used for pelvic floor rehabilitation must be used exclusively by one individual, but due to the high cost of consumables, they are used many times[7]. Furthermore, high temperature and high pressure disinfection cannot be performed on these electronic vaginal products, and improper disinfection may result in vaginal infections[8]. Hydrogen peroxide is one of the simplest active oxides that can be widely used as a disinfectant, oxidant, and oxygen provider[9]. Colloidal silver is added as a stabilizer to the hydrogen peroxide disinfectant to prevent its gradual decomposition and enhance its antibacterial capacity[10]. Colloidal silver consists of minuscule particles of metallic silver of nanometer diameters. By controlling reaction conditions, silver nanomaterials can form dispersed colloidal silver nanoparticles with strong antibacterial effects against bacteria, fungi, and viruses, etc. These are widely used in medical devices and as catalysts, etc.[11]. Compared to disinfection with hydrogen peroxide alone, disinfection with hydrogen peroxide and silver ion provides longer lasting disinfection and better bactericidal effects, requiring smaller dosages and providing higher chemical stability. This mixture is widely used in clinical stomatology, ICU, disinfection of medical equipment, etc.[12].
This study used disinfection with hydrogen peroxide and silver ions to sterilize vaginal electrodes, while investigating the impact of a biostimulation feedback instrument and comprehensive rehabilitation therapy on postpartum pelvic floor muscle function.
This study included 59 puerperal women with PFD who were admitted between May 2019 and July 2022 to West China Hospital, Sichuan University. The participants were divided into two groups: Control group (n = 27), which did not receive treatment with a biostimulation feedback instrument after surgery and observation group (n = 32), which received treatment with a biostimulation feedback instrument. The participants had an average age of 21-36 years, body mass index of 20-27 kg/m2, and 38-45 weeks of gestation. No significant differences in clinical or neonatal data were found between the two groups (Table 1).
| Control group (n = 27) | Observation group (n = 32) | P value | |
| Age (year) | 30.56 ± 4.29 | 31.38 ± 5.24 | 0.726 |
| BMI (kg/m2) | 23.47 ± 1.45 | 23.98 ± 1.32 | 0.529 |
| Gestational week (week) | 40.13 ± 0.38 | 39.84 ± 0.41 | 0.844 |
| Neonatal weight (kg) | 3.12 ± 0.31 | 3.24 ± 0.35 | 0.932 |
| Vaginal delivery | 20 | 26 | |
| Cesarean delivery | 7 | 6 | |
| Second stage of labor time (minute) | 63.75 ± 15.46 | 64.35 ± 16.77 | 0.473 |
The inclusion criteria for the patients were as follows: All women met the clinical diagnostic criteria for postpartum pelvic dysfunction, and their clinical data were complete. All patients had to have full-term pregnancy and were single parturients. The exclusion criteria for this study were patients with mental or cognitive disorders, history of pelvic diseases, and surgery for uterine fibroids; patients with vaginitis or malignant tumors; and maternal disease duration > 1 year.
The control group received comprehensive rehabilitation nursing, where the nursing staff explained the purpose, method, and precautions of pelvic floor rehabilitation prior to training. During training, they assisted the mothers in assuming a supine position with their legs apart, guided them to take deep breaths, and conducted muscle management and contraction training. The mothers were instructed to contract the anal muscles and lower abdominal perineal muscles while inhaling, maintaining contraction for 6 seconds, and then slowly relaxing the entire body while exhaling for 5 seconds. The mothers were asked to alternate this training for 20 minutes, twice a day. The maternal rehabilitation training intervention started 6 weeks postpartum and lasted for 3 months.
In the observation group, intervention involved use of a pelvic floor biostimulation feedback instrument (Nanjing McLand Medical Equipment Co., Ltd.). Before intervention, pregnant women were asked to empty their bladders and take a supine position. The electrode probe was slowly placed into their vagina. The current intensity was set to gradually increase from 0 mA, and the electrical stimulation frequency was adjusted to 50 Hz. It was appropriate for the women to feel strong contraction of the pelvic floor muscle without pain, to awaken proprioception. The frequency of electrical stimulation was adjusted to target both type I and type II muscle fibers. Active maternal contraction of pelvic floor muscles was guided based on feedback from the instrument. The intervention lasted for 15 min per session, five times per week, for 3 months.
The vaginal electrode surface was sampled using a sterile saline-soaked cotton swab prior to electrode disinfection. The electrodes were divided into three groups. The vaginal electrodes in all three groups were washed with running water, and the vaginal electrodes were disinfected with iodophor and disinfected with hydrogen peroxide and silver ion, respectively. The samples were collected after drying. Disinfection with hydrogen peroxide and silver ion (Norfol, Belgium) can be observed by scanning electron microscopy, small colloidal silver particles, the particles are circular, about 100 nm in diameter (Figure 2). To maintain ethical standards, the vaginal electrodes were wiped with iodophor cotton balls even after rinsing with running water, before being inserted into the vagina.
Samples were collected from the surface of the vaginal electrode using cotton swabs soaked in sterile normal saline. The samples were collected before disinfection, immediately after disinfection, 1 hour after disinfection, and 4 hours after disinfection. Once sampling was complete, the samples were sent to the laboratory for bacterial culture. The solution in the sampling tube was inoculated into the cell culture dish, cultured in the incubator at 37°C for 48 hours, and the number of colonies was counted. According to the Guidelines for Disinfection of Medical Devices in Healthcare Institutions, the number of bacterial colonies on the surface of medical devices entering human tissue should be ≤ 100 CFU/cm2[13].
After 3 months of rehabilitation treatment, the pelvic floor biostimulation feedback instrument was used to measure the following parameters: Maximum electromyography (EMG), averaged EMG, pelvic floor muscle strength, vagina electromyogram, and vaginal muscle tone. The contraction time of type I and type II muscle fibers was recorded for the two groups, and pelvic floor muscle strength was graded according to perineal muscle strength test[14]. PFDI-20[15] was used to evaluate pelvic floor function in both groups - the higher the score, the poorer the function. The GQOLI-74 questionnaire on quality of life included four items: Emotional function, material life, physical function, and social function. In addition, postpartum complications, such as stress urinary incontinence, uterine prolapse, and lumbosacral pain, were recorded in the two groups.
SPSS20.0 statistical software was used for data analysis. Measurement data were expressed as mean ± SD and a t-test was used. Statistical data were represented by n, (%), χ2 test was used, and rank sum test was used for rank data; P < 0.05 was considered statistically significant.
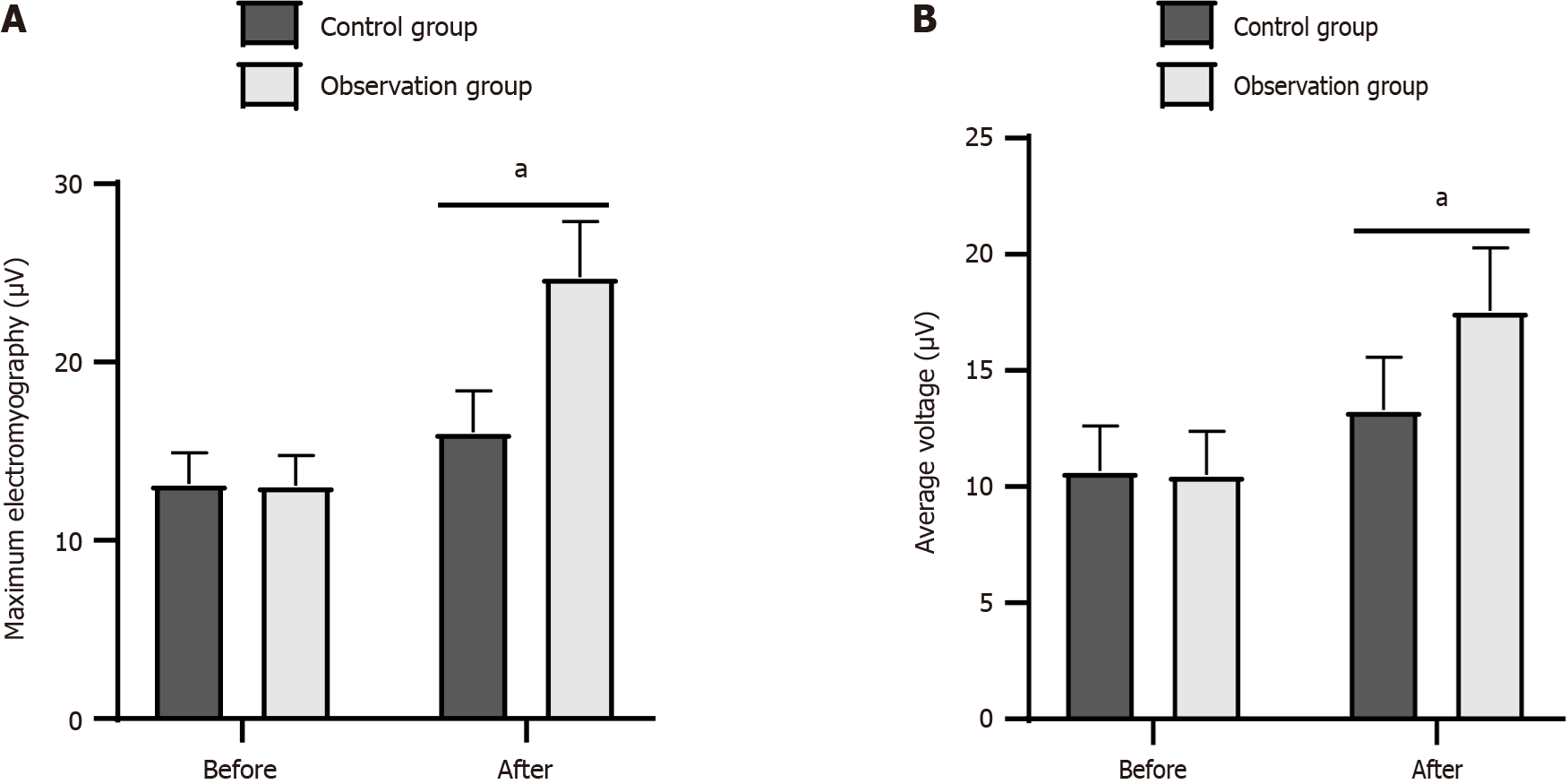
Before intervention, differences in maximum EMG and average muscle voltage were insignificant between the two groups (P > 0.05). However, after intervention, maximum EMG and average muscle voltage were significantly higher in the observation group than the control group (P < 0.05; Figure 3).
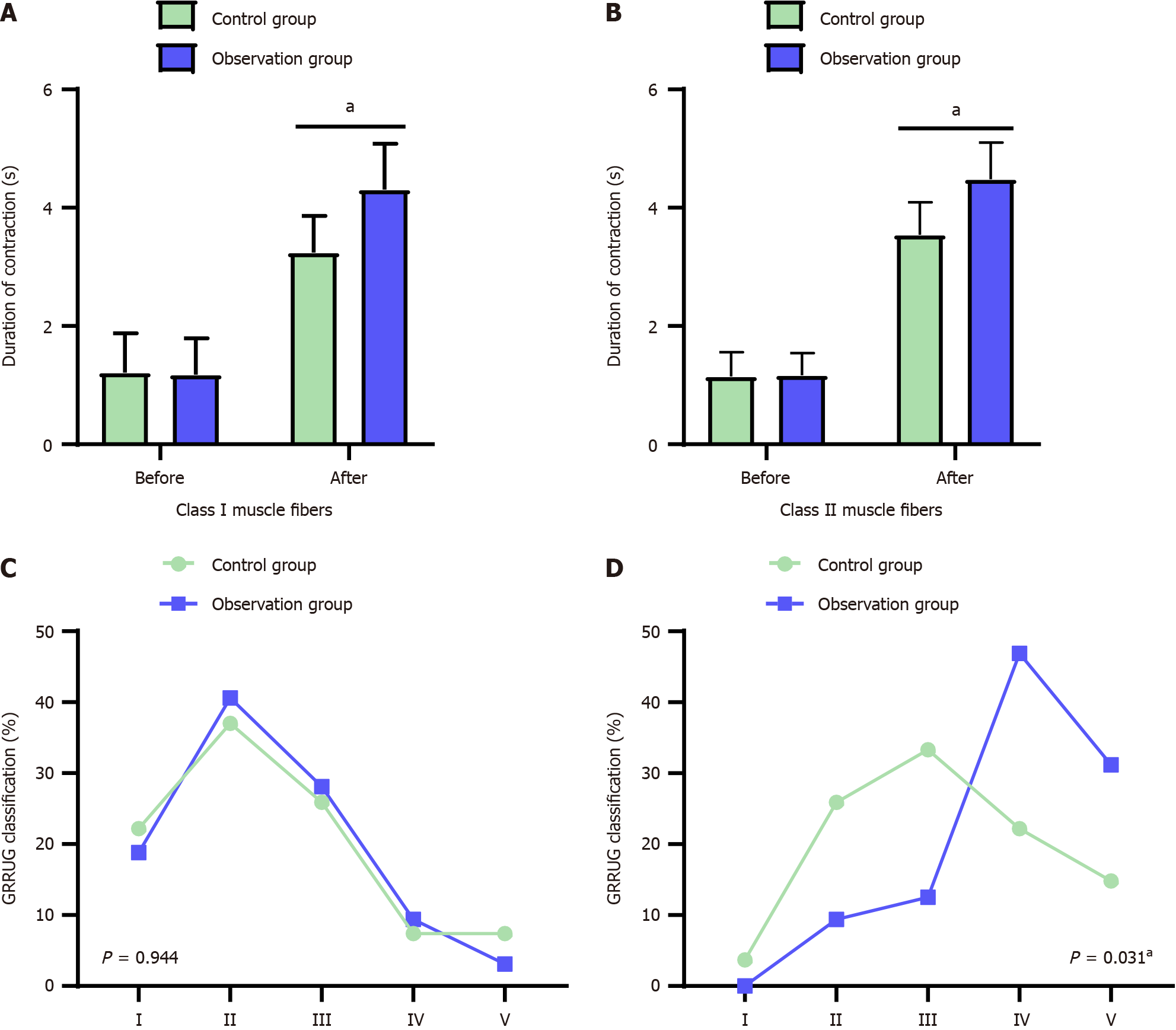
The contraction time of class I and II muscle fibers in both groups was longer after treatment than before treatment, with the observation group demonstrating significantly longer contraction time than the control group (all P < 0.05; Figure 4A and B). The puerperal pelvic floor muscle strength was graded (Figure 4C and D). Pelvic floor muscle strength improved after rehabilitation training, with the observation group demonstrating a more pronounced effect than the control group.
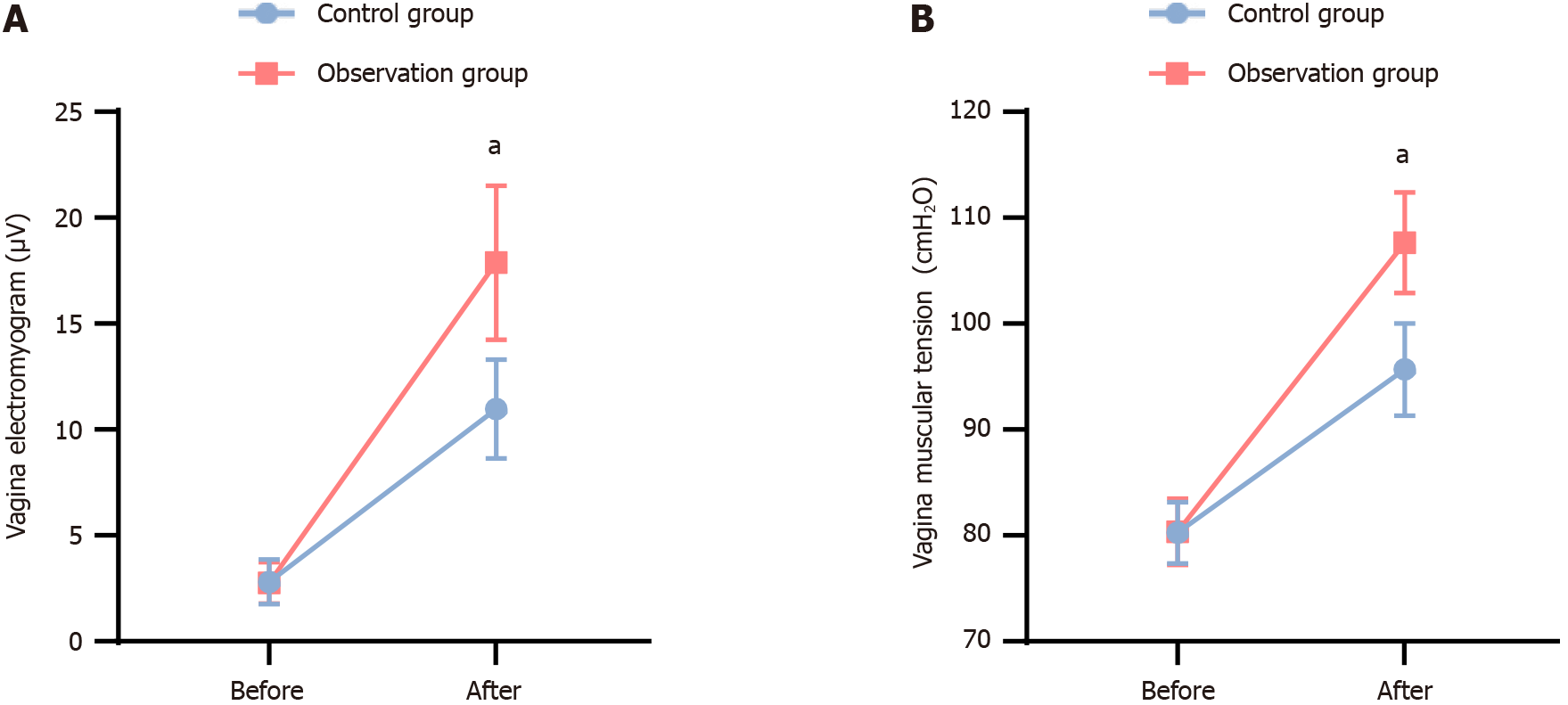
Before treatment, vaginal muscle voltage and vaginal muscle tension were not significantly different between the two groups. After treatment, both groups experienced a significant increase in vaginal muscle voltage and vaginal muscle tension, with the observation group showing higher values than the control group (P < 0.05; Figure 5).
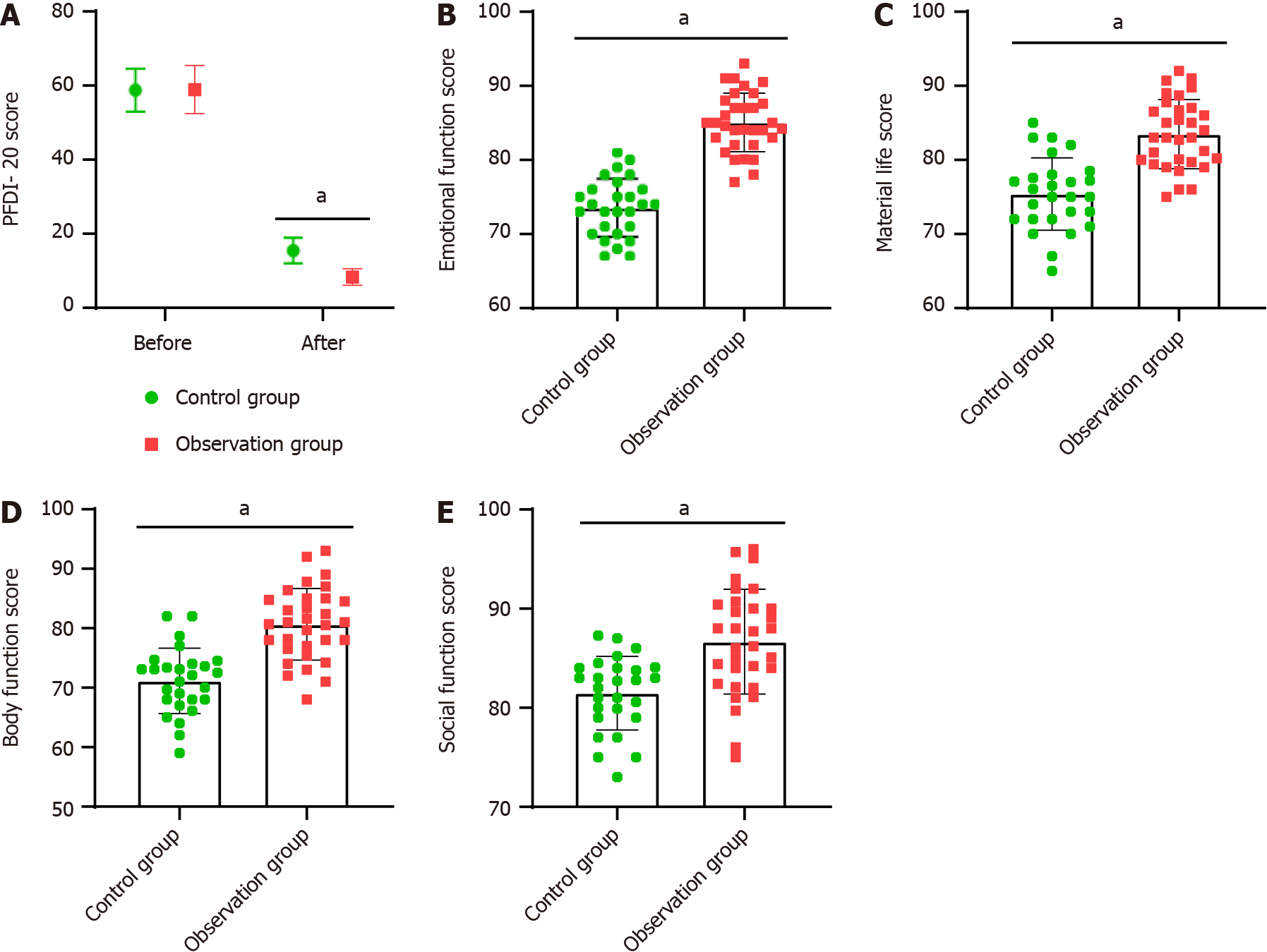
Before treatment, the PFDI-20 score was not significantly different between the two groups (P > 0.05). However, after treatment, both groups exhibited a significant reduction in PFDI-20 scores. The scores were lower in the observation group than the control group (P < 0.05; Figure 6A). After rehabilitation treatment, all GQOLI-74 scores significantly improved. The scores for emotional function, material life, physical function, and social function were higher in the observation group than the control group (P > 0.05; Figure 6B-E).
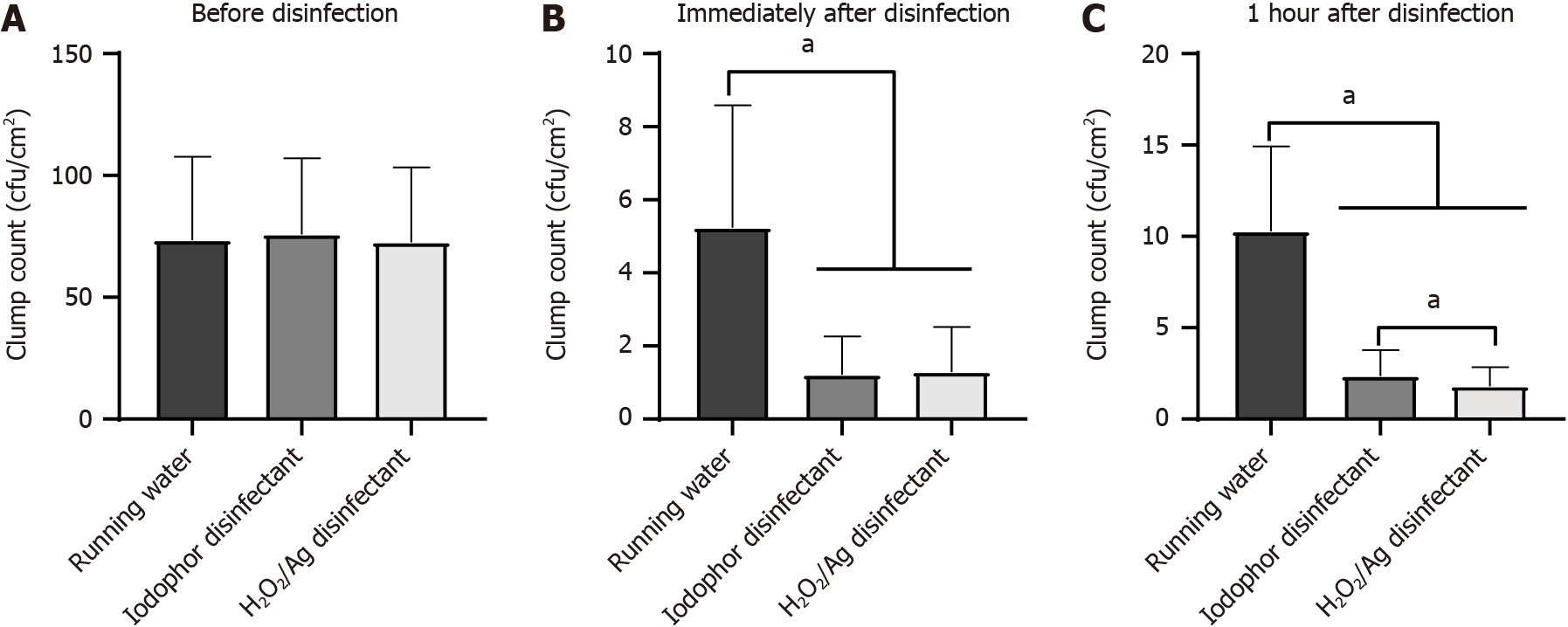
Samples were collected at different times before and after disinfection of the vaginal electrodes to check the number of bacterial colonies The total number of bacterial colonies on the surface of some electrodes exceeded the standard before disinfection, with no statistically significant differences between the three groups of electrodes (Figure 7A). The number of colonies was significantly reduced by immediate sampling after flushing and disinfection with running water, which met the safety standard, but the number of colonies was highest in the tap water group (Figure 7B). After 1 hour of disinfection, the number of colonies on the electrode surface rinsed with tap water increased and was highest in all groups. The number of colonies slightly increased in the iodor disinfection and H2O2/Ag disinfectant groups, with the iodor group exhibiting slightly higher counts than the H2O2/Ag disinfectant group (Figure 7C).
During rehabilitation treatment, postpartum women suffered PFD diseases, such as stress urinary incontinence and uterine prolapse (Table 2). The incidence of PFD diseases was significantly lower in the observation group than the control group (P = 0.017).
| Control group (n = 27) | Observation group (n = 32) | P value | |
| Stress incontinence | 2 | 1 | 0.456 |
| Prolapse of uterus | 3 | 0 | 0.053 |
| Lumbosacral pain | 1 | 0 | 0.272 |
| Population generation ratio (%) | 8 | 2 | 0.0171 |
Pelvic floor muscles, associated with the urethra, uterus, rectum, bladder, and other organs, maintain the normal physiological position of the pelvic organs[16]. They primarily consist of type I slow contracting muscle fibers and type II fast contracting muscle fibers. Type I muscle fibers support the pelvic cavity and have a longer contraction time[17]. Type II muscle fibers are responsible for pelvic and abdominal movements; allow for the closure of the urethra during increased abdominal pressure, but can cause short-term fatigue. As gestation progresses, the pressure on the pelvic floor gradually increases. During childbirth, the nerves and muscles of maternal pelvic floor tissues are excessively stretched by external forces, resulting in nerve atrophy, indirectly affecting pelvic floor muscles and causing PFD[18]. Therefore, for women with PFD, clinical intervention should be given as early as possible to minimize damage to pelvic floor function and improve the quality of life after delivery.
Comprehensive rehabilitation training integrates various intervention measures through health education to improve cognition of puerperal pelvic floor rehabilitation, focus on pelvic floor muscle function exercise, and promote puerperal exercise. Comprehensive rehabilitation training can also guide parturients to perform vaginal dumbbell and pelvic floor contraction training, accelerate pelvic floor blood circulation, stimulate pelvic floor muscle contraction, and improve pelvic floor muscle function[19]. However, comprehensive rehabilitation training is a lengthy process with slow results and uncertain effectiveness. Therefore, additional auxiliary intervention strategies are necessary in clinical practice to promote functional recovery of the maternal pelvic floor muscles[20]. In this study, pregnant women in the observation group underwent comprehensive rehabilitation treatment and nursing, where healthcare providers taught them and their family’s techniques for pelvic floor rehabilitation training. They utilized a biological stimulation feedback instrument to provide electrical stimulation to pelvic floor muscles, facilitating the learning and mastery of correct pelvic floor muscle recovery methods. Comprehensive rehabilitation training is not limited to specific settings and can be conducted in the hospital ward or at home, offering a simple, cost-effective, efficient, and accessible method for pelvic floor muscle restoration.
The biostimulation feedback instrument uses electrodes placed in the vagina to provide electrical stimulation of varying intensity. This stimulation aims to reinforce the pelvic floor muscle group, thereby stimulating the innervation nerve of the pelvic floor muscle. Ultimately, it improves the contractile function of the pelvic floor muscle and promotes postpartum recovery[21]. In this study, after 3 months of rehabilitation treatment, pelvic floor muscle voltage, contractility of pelvic floor type I and type II muscle fibers, vaginal muscle tension, vaginal muscle voltage, and quality of life scores were better in the observation group than the control group (P < 0.05). Thus, the combination of biostimulation feedback instrument and pelvic floor muscle function exercise improved pelvic floor muscle tension, improved the level of type I and type II muscle fibers of parturients, and improved vaginal muscle voltage, to effectively enhance the pelvic floor muscle function and improve quality of life. The observation group had a significantly lower incidence of PFD and better treatment outcomes. Clinical studies have shown that the stimulation of pelvic floor muscles with a biostimulation feedback instrument can improve the excitability of pelvic floor nerves, activate nerve cells with suspended function, promote the recovery of pelvic floor elasticity and muscle tension, and prevent the occurrence of urinary incontinence and uterine prolapse[22]. The biostimulation feedback instrument allows for real-time monitoring of the biological signals from maternal pelvic floor muscles, aiding both mothers and operators in understanding the state of maternal pelvic floor muscles. This is achieved through the simulation of signals, such as sound, light, and image, enabling better cooperation with the training mode and improved treatment outcomes[23].
In this study, bacterial cultures from vaginal electrode sampling showed that compared to the group rinsed solely with running water, the group cleaned and disinfected with iodophor or silver hydrogen peroxide ion disinfectant had < 100 CFU/cm2 bacteria. The qualification rate was 100%, indicating that the use of silver hydrogen peroxide ion disinfectant and iodophor had the same bactericidal effect. As the time after disinfection increased, bacteria in the running water washing group started to increase, whereas bacteria in the silver hydrogen peroxide disinfectant group showed the least increase. This suggests that the use of silver hydrogen peroxide ion disinfection prolongs the antibacterial time on the electrode surface. With increasing awareness of PFD diseases, more individuals are undergoing pelvic floor rehabilitation treatment. In the course of treatment, the cleaning and disinfection of vaginal electrodes has become the focus of studies. During pelvic floor rehabilitation treatment, the repeated insertion of vaginal electrodes will inevitably increase the chance of vaginal infection; therefore, cleaning and disinfecting vaginal electrodes should reduce the occurrence of infections.
In summary, the combination of biostimulation feedback instrument and pelvic floor muscle rehabilitation training for postpartum women with pelvic floor muscle dysfunction can effectively enhance their postpartum pelvic floor muscle function. This treatment option demonstrates an ideal therapeutic effect and is recommended for clinical application. Additionally, the use of silver hydrogen peroxide ion disinfectant for vaginal electrode disinfection displayed considerable antibacterial effect for a prolonged duration.
| 1. | Wallace SL, Miller LD, Mishra K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol. 2019;31:485-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 111] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 2. | Youssef A, Brunelli E, Pilu G, Dietz HP. The maternal pelvic floor and labor outcome. Am J Obstet Gynecol MFM. 2021;3:100452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Riaz H, Nadeem H, Rathore FA. Recent advances in the pelvic floor assessment and rehabilitation of Women with Pelvic Floor Dysfunction. J Pak Med Assoc. 2022;72:1456-1459. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 4. | Deffieux X, Vieillefosse S, Billecocq S, Battut A, Nizard J, Coulm B, Thubert T. Postpartum pelvic floor muscle training and abdominal rehabilitation: Guidelines. J Gynecol Obstet Biol Reprod (Paris). 2015;44:1141-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Starr JA, Drobnis EZ, Lenger S, Parrot J, Barrier B, Foster R. Outcomes of a comprehensive nonsurgical approach to pelvic floor rehabilitation for urinary symptoms, defecatory dysfunction, and pelvic pain. Female Pelvic Med Reconstr Surg. 2013;19:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Liu J, Yan W, Tang Y, Zhou Y, Yang S, Xiang J, Zeng X, Xie F, Li X. Therapeutic effect of proprioception training combined with pelvic floor electrical stimulation biofeedback on postpartum pelvic floor dysfunction. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2022;47:1253-1259. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Barbosa AMP, Parizotto NA, Pedroni CR, Avila MA, Liebano RE, Driusso P. How to report electrotherapy parameters and procedures for pelvic floor dysfunction. Int Urogynecol J. 2018;29:1747-1755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Dmochowski R, Lynch CM, Efros M, Cardozo L. External electrical stimulation compared with intravaginal electrical stimulation for the treatment of stress urinary incontinence in women: A randomized controlled noninferiority trial. Neurourol Urodyn. 2019;38:1834-1843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Martin NL, Bass P, Liss SN. Antibacterial Properties and Mechanism of Activity of a Novel Silver-Stabilized Hydrogen Peroxide. PLoS One. 2015;10:e0131345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | El-Gohary FA, Abdel-Hafez LJM, Zakaria AI, Shata RR, Tahoun A, El-Mleeh A, Abo Elfadl EA, Elmahallawy EK. Enhanced Antibacterial Activity of Silver Nanoparticles Combined with Hydrogen Peroxide Against Multidrug-Resistant Pathogens Isolated from Dairy Farms and Beef Slaughterhouses in Egypt. Infect Drug Resist. 2020;13:3485-3499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Sanli-Yurudu NO, Kimiran-Erdem A, Arslan-Aydogdu EO, Zeybek Z, Gurun S. Efficacy of Colloidal Silver-Hydrogen Peroxide and 2-Bromo-2-nitroporopane-1,3-diol Compounds Against Different Serogroups of Legionella pneumophila Strains. Indian J Microbiol. 2012;52:54-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Mosci D, Marmo GW, Sciolino L, Zaccaro C, Antonellini R, Accogli L, Lazzarotto T, Mongardi M, Landini MP. Automatic environmental disinfection with hydrogen peroxide and silver ions versus manual environmental disinfection with sodium hypochlorite: a multicentre randomized before-and-after trial. J Hosp Infect. 2017;97:175-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Ling ML, Ching P, Widitaputra A, Stewart A, Sirijindadirat N, Thu LTA. APSIC guidelines for disinfection and sterilization of instruments in health care facilities. Antimicrob Resist Infect Control. 2018;7:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Berghmans B. Physiotherapy for pelvic pain and female sexual dysfunction: an untapped resource. Int Urogynecol J. 2018;29:631-638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 74] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 15. | de Arruda GT, de Andrade DF, Virtuoso JF. Internal structure and classification of pelvic floor dysfunction distress by PFDI-20 total score. J Patient Rep Outcomes. 2022;6:51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Radzimińska A, Strączyńska A, Weber-Rajek M, Styczyńska H, Strojek K, Piekorz Z. The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: a systematic literature review. Clin Interv Aging. 2018;13:957-965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 79] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 17. | Koenig I, Eichelberger P, Leitner M, Moser H, Kuhn A, Taeymans J, Radlinger L. Pelvic floor muscle activity patterns in women with and without stress urinary incontinence while running. Ann Phys Rehabil Med. 2020;63:495-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Romeikienė KE, Bartkevičienė D. Pelvic-Floor Dysfunction Prevention in Prepartum and Postpartum Periods. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Liang P, Liang M, Shi S, Liu Y, Xiong R. Rehabilitation programme including EMG-biofeedback- assisted pelvic floor muscle training for rectus diastasis after childbirth: a randomised controlled trial. Physiotherapy. 2022;117:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 20. | Zhu Y, Li G, Zhu Y, Yu Y, Gong X. Comprehensive treatment of pelvic floor muscle training plus biofeedback electrical stimulation for stress urinary incontinence: a clinical study. Am J Transl Res. 2022;14:2117-2122. [PubMed] |
| 21. | Hagen S, Elders A, Stratton S, Sergenson N, Bugge C, Dean S, Hay-Smith J, Kilonzo M, Dimitrova M, Abdel-Fattah M, Agur W, Booth J, Glazener C, Guerrero K, McDonald A, Norrie J, Williams LR, McClurg D. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: multicentre randomised controlled trial. BMJ. 2020;371:m3719. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 22. | Chen Z, Huang H, Chen QY. Effect of modified Buzhong Yiqi decoction combined with pelvic floor muscle exercise-biofeedback-electrical stimulation on early stage postpartum pelvic floor dysfunction. Zhongguo Zhong Yao Za Zhi. 2018;43:2391-2395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Rivalta M, Sighinolfi MC, De Stefani S, Micali S, Mofferdin A, Grande M, Bianchi G. Biofeedback, electrical stimulation, pelvic floor muscle exercises, and vaginal cones: a combined rehabilitative approach for sexual dysfunction associated with urinary incontinence. J Sex Med. 2009;6:1674-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |