Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4499
Revised: May 7, 2024
Accepted: June 6, 2024
Published online: July 26, 2024
Processing time: 119 Days and 5.3 Hours
The recovery of limb function after ankle fracture surgery is a gradual process. The main purpose of implementing early functional exercise, joint mobility, muscle contraction function, passive ankle flexion and extension exercises, or physical factor therapy techniques is to achieve the rapid recovery of normal physiological limb function. However, currently the most effective rehabilitation training method is staged limb functional exercise, which promotes rapid recove
To perform a functional evaluation and determine the influencing factors of staged functional training in patients with ankle fracture.
A retrospective study enrolled 150 patients who underwent surgical treatment for ankle fracture from May 2020 to May 2022 at our hospital. Univariate and multivariate linear regression analyses were performed on general data, func
Based on the AOFAS Ankle-Hindfoot Scale, the cases were divided into the excellent function (n = 111) and ordinary function (n = 39) groups. Univariate analysis revealed that monthly family income, education level, diabetes mellitus, functional exercise compliance scale of orthopedic patients score, SSRS, BK, PGE2, and 5-HT significantly influenced limb function after ankle fracture (P < 0.05); Multiple linear regression analysis showed that the functional exercise compliance scale score, SSRS, BK, PGE2, and 5-HT were independent risk factors affecting functional performance after staged functional exercise (P < 0.05).
Exercise compliance, SSRS, and pain level are the independent risk factors affecting functional performance after staged functional training following ankle surgery. Clinical nursing care after ankle surgery should include analgesic and health education measures to ensure optimal recovery of limb function.
Core Tip: This article examined the functional recovery assessment and influencing factors after implementing staged training exercise for ankle fractures. Social support, exercise compliance, and pain were identified as independent risk factors affecting ankle function recovery. The study findings can provide clear guidance on postoperative care for ankle surgery.
- Citation: Fang MQ. Functional assessment and influencing factors after staged functional training in patients with ankle fractures. World J Clin Cases 2024; 12(21): 4499-4507
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4499.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4499
An ankle fracture usually involves the breakage of either or both the tibia (leg bone) and fibula (bone on the outer side of the lower leg). Ankle fractures can be caused by external impact or high-energy injuries, such as falls, sports injuries, vehicular accidents, or other unforeseen situations. Symptoms of ankle fracture include severe pain, swelling, congestion, impaired movement, and joint dislocation. An epidemiological investigation and analysis by Kang et al[1] found that fracture incidence is highest among people aged 40-50 years, accounting for 24.04% in all age groups, with sprains and vehicular accidents being the main causes of fracture.
The treatment of treating ankle fractures depends on the fracture type and location, severity of concomitant injury, and patient’s age and overall health. Surgical methods include external and internal fixation. The goal of treatment is to ensure proper fracture healing, restore joint function, and reduce sequelae. Therefore, postoperative rehabilitation training is essential to restoring the patient’s ankle strength, flexibility, and balance. At present, no unified standard procedure has been established in clinical practice for the rehabilitation training of patients with ankle fracture[2,3]. Routine rehabilitation training usually implements a universal and general treatment strategy without considering the patient’s individual characteristics and condition. This may lead to insufficient training efficacy and failure to meet the unique needs of patients, resulting in unsatisfactory recovery of ankle joint function, lingering pain, and impaired sleep quality[4,5].
Staged functional training refers to gradual adaptive rehabilitation training implemented according to the different stages of patient rehabilitation to restore, improve, or maintain the patient’s body function. This rehabilitation training approach usually involves an individualized plan developed by a professional rehabilitation team according to the patient’s specific condition and rehabilitation needs[6,7]. Staged functional training is progressive, which helps avoid overtraining and excessive fatigue. Furthermore, it helps improve patients’ endurance and adaptability by restoring motor function, strength, balance, and coordination; reducing pain; improving sleep quality; and maximizing the restoration of autonomy in daily life[8]. However, relatively few reports have explored the application of staged functional training in postoperative rehabilitation of patients with ankle fractures in China. In this study, 150 patients with ankle fracture admitted to our hospital from May 2020 to May 2022 were selected by convenience sampling to comprehensively explore the risk factors affecting the results of staged functional training after ankle surgery on ankle function.
Equation [N = (U21-a/2S2)/d2, where statistics U1-α/2 = 1.96, standard deviation S = 10.90, and allowable error d = 1.5] as used to calculate the sample size, and the confidence interval was set at 95%. The minimum sample size obtained was 182 cases, with consideration of a loss-to-follow-up rate of 15%-20%. Data on 150 patients who underwent ankle fracture surgery at The Fourth Hospital of Wuhan from May 2020 to May 2022 were selected.
Inclusion criteria: (1) An ankle joint fracture diagnosed by computed tomography (CT), nuclear magnetic resonance imaging; (2) patients undergoing surgical treatment, including fracture reduction, internal fixation, and external fixation; (3) patients with swelling, pain, and limited movement at admission; and (4) patients aged ≥ 18 years.
Exclusion criteria: (1) Patients with pathological fracture; (2) patients who refuse to cooperate with nursing or relevant examinations; (3) patients with secondary osteoporosis; and (4) patients with concurrent serious organic diseases of the heart, liver, kidney, and endocrine system.
All patients received staged limb function training after surgery, including hospitalization and discharge. The hospitalization period included postoperative 1-2 days, 3-4 days, and 5-7 days. The discharge period included the 2nd-4th week, 5th-8th week, and 9th-12th week postoperatively. The specific steps of the rehabilitation strategy were as follows: (1) 1-2 days postoperatively: The rehabilitation physician and nursing staff guided the patient and his/her family members in the proper way of massaging the ankle joint and toe of the patient to promote blood circulation in the lower extremities and prevent deep vein thrombosis; (2) 3-4 days postoperatively: Passive movement of the ankle joint and toes should be promoted, including ankle flexion, extension, toe flexion, extension, unfolding and retraction. Varus, valgus, and internal and external rotation are prohibited. The passive activity should be performed for 15 minutes twice/day; (3) 5-7 days postoperatively: Depending on the degree of recovery and tolerance of the patient’s ankle joint, the intensity of passive movement was gradually increased to 3 times/day, and the duration of a single activity was increased from 15 minutes to 20-25 minutes. In addition, the patient was instructed to actively perform lower limb-raising exercise and properly perform ankle varus, valgus, and internal and external rotation activities for 15 minutes twice/day. The intensity of activity depended on the patient’s tolerance; (4) 2-4 weeks postoperatively: After the patient was discharged, rehabilitation training was continuously followed up by telephone follow-up, door-to-door guidance, and online WeChat com
General data: Patients’ sex, age, monthly family income, education level, diabetes mellitus status, body mass index (BMI), Lauge–Hansen classification, and affected side were extracted from medical records.
Functional exercise compliance scale for orthopedic patients: The functional exercise compliance scale for orthopedic patients[9] was used to evaluate patients’ exercise compliance at 12 weeks postoperatively. The scale consists of 15 items on the three dimensions of physical, psychological, and active learning-related exercise compliance. Each item is evaluated using a 4-point scale, with a possible total score of 15-60 points. The higher the score, the higher the patient’s functional exercise compliance.
Social support Rating Scale (SSRS): The SSRS[10] was used to evaluate the patient’s social support at 12 weeks postoperatively. The scale mainly included three dimensions of subjective support (the total score of items 1, 3, 4, and 5), objective support (the total score of items 2, 6, and 7), and support availability (the total score of items 8-10). Items 1-4 and 8-10 are evaluated on a 5-point scale. Items A, B, C, and D4 of item 5 are evaluated on a 4-point scale. If no source is selected for items 6-7, 0 points will be scored; if several sources are identified, what point will be scored? Higher total scores indicate higher social support.
Ankle function: Ankle function was assessed using the American Orthopedic Foot and Ankle Score (AOFAS) Ankle-Hindfoot scoring system[11] at 12 weeks postoperatively, including ankle and plantar flexion angles. Measurements were performed with a protractor, with the patient’s ankle joint in the neutral position designated as 0°. Measurements were performed three times, and the average value of the three measurements was the final measurement result. The scoring system evaluates pain (40 points), function (50 points), and alignment (10 points). Function assesses movement limitation, need for auxiliary support, maximum walking distance, walking surface, sagittal plane movement (flexion and dorsiflexion), hindfoot movement (varus and valgus), and ankle and hindfoot stability (anteroposterior and valgus). The total possible score of the scoring system is 0-100 points. The higher the score, the better the recovery of ankle joint function. The patients were divided based on total score: Those who scored ≥ 90 points were placed in the good function group, and those who scored < 90 points were placed in the general function group.
Serum pain factors: At 12 weeks postoperatively, 4 mL of blood was drawn from the elbow vein on an empty stomach in the morning. The blood sample was sent to the laboratory for centrifugation at 3600 r/min for 10 min. The supernatant was collected and refrigerated in a cryogenic refrigerator at -80°C. Serum bradykinin (BK), prostaglandin (PGE2), and 5-hydroxytryptamine (5-HT) were detected by enzyme-linked immunosorbent assay.
Patients with ankle fracture were enrolled based on the inclusion and exclusion criteria. Before the study, medical staff were trained and assessed in a unified manner. After training, they could participate in the study only after passing the assessment. Consistency in implementing standard operating procedures during data collection, research ethics, and confidentiality requirements were ensured throughout the study. Data were regularly monitored and reviewed for quality and consistency, including double data entries, logicality checks, and outlier detection. Processes for quality control and quality assurance were strictly implemented, including the review of study procedures, standard operating procedures, and data security and integrity.
SPSS.26.0 was used to process the data. The Kolmogorov-Smirnov test was performed to validate the normal distribution of the measurement data. The t-test was performed, and data were expressed as mean ± SD. Count data were expressed as number and percentage and analyzed using the χ2 test. Binary logistic regression analysis was performed to determine the independent risk factors affecting functional performance after staged functional training following ankle surgery. Statistical significance was indicated by P < 0.05.
Before treatment, there was no statistical significance in the comparison of plantar flexion angle, dorsiflexion angle and AOFAS Ankle-Hindfoot scores of subjects with ankle fracture (P > 0.05); after 1 month and 2 months of intervention, the plantar flexion angle, dorsiflexion angle and AOFAS Ankle-Hindfoot scores of subjects with ankle fracture were significantly higher than those before and after 1 month of intervention (P < 0.05; Table 1).
| Group | Plantarflexion angle | Dorsal extension angle | AOFAS Ankle-Hindfoot Score (points) | ||||||
| Before intervention | 1 month after intervention | 3 months after intervention | Before intervention | 1 month after intervention | 3 months after intervention | Before intervention | 1 month after intervention | 3 months after intervention | |
| Subject | 11.95 ± 2.07 | 24.41 ± 2.67a | 33.91 ± 3.11b | 6.53 ± 1.47 | 11.83 ± 1.92a | 15.73 ± 3.26b | 53.11 ± 6.01 | 64.74 ± 6.08a | 81.84 ± 10.16b |
| t value | 0.951 | 8.538 | 8.975 | 1.578 | 7.329 | 9.772 | 1.192 | 4.381 | 3.839 |
| P value | 0.343 | < 0.001 | < 0.001 | 0.117 | < 0.001 | < 0.001 | 0.235 | < 0.001 | < 0.001 |
The functional status after staged sexual training following ankle fracture surgery as a dependent variable, whereas sex, age, monthly family income, education level, and presence or absence of diabetes mellitus status, Lauge–Hansen classification, start time of postoperative exercise, BMI, presence of lower tibiofibular fixation, score, and SSRS score, BK, PGE2, and 5-HT were used as independent variables. Univariate analysis showed that monthly family income, education level, diabetes mellitus status, start time of postoperative exercise, lower tibiofibular fixation, functional exercise compliance scale score, SSRS score, BK, PGE2, and 5-HT were all associated with limb function after staged sexual training following ankle fracture surgery (Table 2).
| Independent variables | Grouping | Excellent functional group (n = 111) | General functional group (n = 39) | χ2 | P value |
| Sex | Male | 69 | 19 | 2.151 | 0.142 |
| Female | 42 | 20 | |||
| Age (years) | 46.58 ± 4.35 | 46.77 ± 4.28 | 0.236 | 0.814 | |
| Monthly household income (RMB) | ≤ 5000 | 34 | 19 | 4.132 | 0.042 |
| > 5001 | 77 | 20 | |||
| Educational level | High school and below | 42 | 22 | 4.070 | 0.044 |
| Junior college or above | 69 | 17 | |||
| Comorbid diabetes | Yes | 81 | 21 | 4.852 | 0.028 |
| No | 30 | 18 | |||
| Lauge–Hansen classification | Pronation-abduction | 31 | 9 | 2.269 | 0.518 |
| Pronation-external rotation | 26 | 13 | |||
| Supination-adduction | 29 | 7 | |||
| Supination-external rotation type | 25 | 10 | |||
| Start time of postoperative exercise (hour) | 48-72 | 69 | 17 | 4.070 | 0.044 |
| > 72 | 42 | 22 | |||
| BMI (kg/m2) | 24.65 ± 3.68 | 24.74 ± 3.72 | 0.131 | 0.896 | |
| Lower tibiofibular fixation | Yes | 83 | 22 | 4.635 | 0.031 |
| No | 28 | 17 | |||
| Functional exercise compliance scale (points) | Male | 49.65 ± 9.46 | 42.36 ± 8.79 | 4.214 | < 0.01 |
| SSRS (points) | Female | 30.64 ± 3.45 | 24.36 ± 2.46 | 10.461 | < 0.01 |
| BK (μg/L) | 6.41 ± 1.32 | 8.75 ± 1.47 | 9.243 | < 0.01 | |
| PGE2 (ρg/mL) | ≤ 5000 | 170.66 ± 19.62 | 214.14 ± 18.70 | 12.048 | < 0.01 |
| 5-HT (ng/L) | > 5001 | 97.84 ± 18.75 | 121.44 ± 16.38 | 6.977 | < 0.01 |
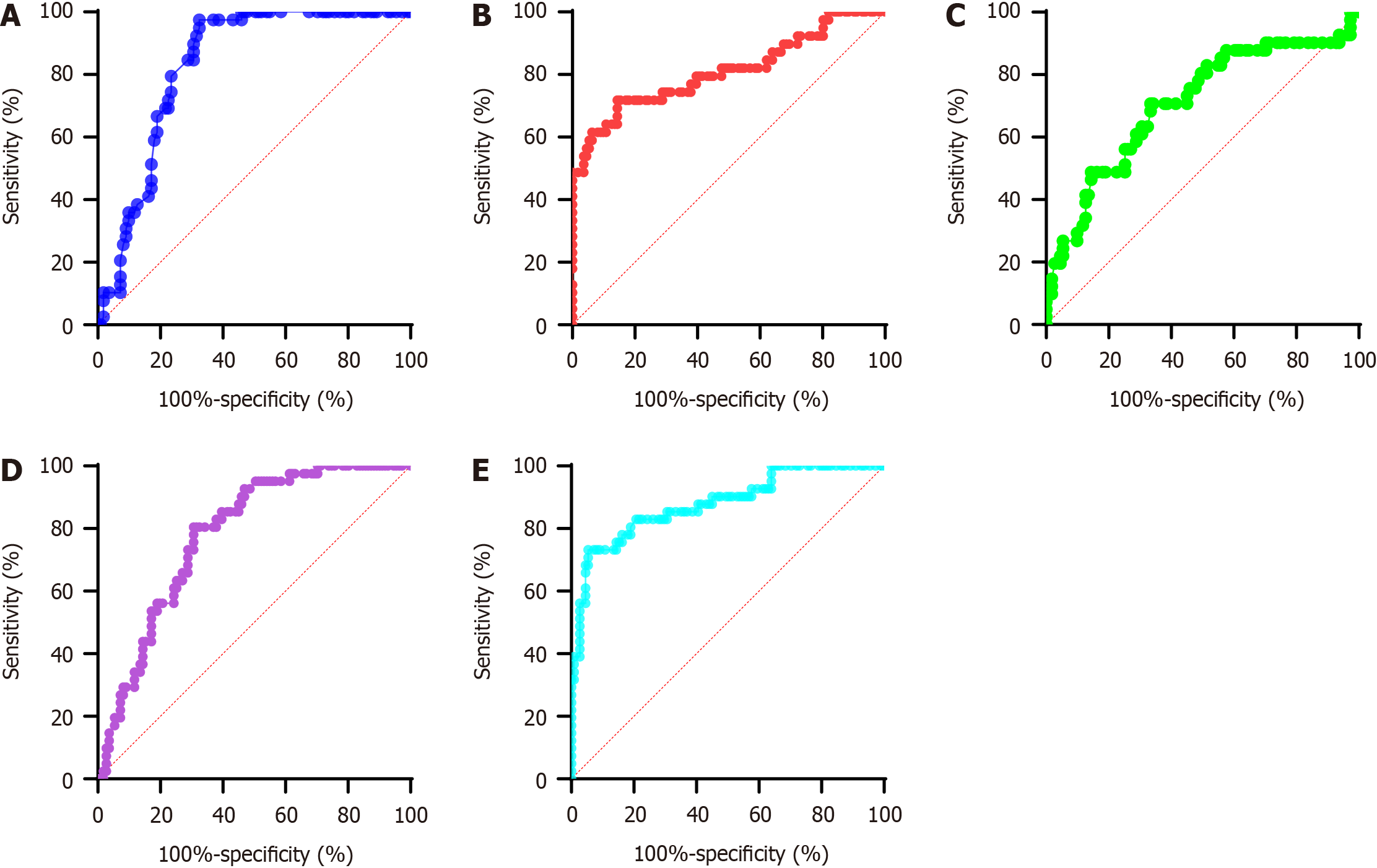
The independent risk factors affecting functionality after staged functional training following ankle surgery were further analyzed. Binary logistic regression analysis was performed using functional status as dependent variable. Monthly family income, education level, diabetes mellitus status, start time of postoperative exercise, tibiofibular fixation, functional exercise compliance scale, SSRS, BK, PGE2, and 5-HT were used as independent variables. The assignment table of variables is detailed in Table 3. The analysis revealed that the functional exercise compliance scale score, SSRS scale score, BK, PGE2, and 5-HT were the independent risk factors associated with postoperative functional training after ankle fracture surgery (Table 4 and Figure 1).
| Variables | Assignment method | |
| Dependent variable | Functional status | General function group = 1, excellent function group = 0 |
| Independent variables | Monthly household income | ≤ RMB 5000 = 1, > RMB 5001 = 0 |
| Educational level | High school and below = 1, junior college or above = 0 | |
| Comorbid diabetes | Yes = 1, No = 0 | |
| Start time of postoperative exercise | 48-72 hours = 1, > 72 hours = 0 | |
| Lower tibiofibular fixation | No = 1, yes = 0 | |
| Functional exercise compliance scale | Input as original value | |
| SSRS | Input as original value | |
| BK | Input as original value | |
| PGE2 | Input as original value | |
| 5-HT | Input as original value | |
| Independent variables | β | SE | Wald χ2 | P value | OR | 95%CI | |
| Lower limit | Upper limit | ||||||
| Functional Exercise Compliance Scale for orthopedic patients | -4.941 | -6.914 | -2.967 | 1.001 | -0.247 | -4.937 | < 0.001 |
| SSRS | -9.664 | -12.377 | -6.951 | 1.375 | -0.341 | -7.026 | < 0.001 |
| BK | -9.664 | -12.377 | -6.951 | 1.375 | -0.341 | -7.026 | < 0.001 |
| PGE2 | -2.995 | -5.466 | -0.525 | 1.252 | -0.112 | -2.392 | 0.018 |
| 5-HT | -11.507 | -15.358 | -7.655 | 1.953 | -0.289 | -5.892 | < 0.001 |
Ankle fractures usually involve the tibia and fibula and are commonly caused by falls, sports injuries, and vehicular accidents, among others. Surgical treatment is currently the first-line treatment in clinical practice. However, because of the long postoperative recovery time of ankle fractures, delayed and ineffective rehabilitation training will have adverse effects on ankle functional rehabilitation. Therefore, clinical attention should be focused on postoperative rehabilitation exercises. Although routine rehabilitation training is simple and easy, no nursing interventions have been established for the different stages of functional recovery. However, staged functional training enables targeted rehabilitation training according to the characteristics of different rehabilitation stages and the patient’s rehabilitation progress. This training method divides the rehabilitation process into different stages, and each stage has specific goals and training methods to gradually restore limb function and mobility[12].
In the rehabilitation of patients with ankle fractures, plantar flexion angle, dorsiflexion angle, and AOFAS Ankle-Hindfoot Score are commonly used measures to assess ankle function and rehabilitation progress. Plantar flexion angle is the extent of dorsal flexion of the ankle and reflects the range of motion and flexibility of the ankle joint. During rehabilitation, the progress of patients’ recovery and functional mobility (e.g., ankle stiffness or dysfunction) can be determined by measuring the plantar flexion angle. The dorsiflexion angle is the degree of ankle extension toward the sole of foot. Similarly, the dorsiflexion angle is an indicator of the range of motion and rehabilitation progress of the ankle joint. In patients with ankle fractures, measuring the dorsiflexion angle can help determine ankle flexibility and rehabilitation. The AOFAS Ankle-Hindfoot Score is a standard scoring system for assessing ankle and hindfoot function. The score is a functional assessment of different aspects, such as pain, gait, joint stability, ankle range of motion, balance, and daily living functions[13]. The AOFAS Ankle-Hindfoot Score is a comprehensive assessment of ankle joint and hindfoot function and a means of tracking rehabilitation progress. In this study, after 1 and 2 months of intervention, the plantar flexion angle, dorsiflexion angle, and AOFAS Ankle-Hindfoot scores of subjects after staged functional training following ankle fracture surgery were significantly higher than those before intervention (P < 0.05).
Functional exercise after ankle surgery helps promote blood flow around the ankle joint and accelerate the recovery process. Appropriate exercise can facilitate lymphatic and blood reflux, thereby reducing postoperative swelling and pain. Continuous functional training helps maintain muscle strength around the ankle joint and prevent muscle atrophy caused by postoperative braking. Exercise gradually restores the normal range of motion of the ankle joint and prevents joint dysfunction due to adhesion or stiffness[14]. Patient compliance with functional exercise is influenced by psychological factors. Positive attitude, confidence in rehabilitation, and good self-management can help improve exercise compliance, which in turn, maximizes the recovery of ankle function. Functional exercise compliance has many positive effects on functional recovery. To maximize rehabilitation, patients should faithfully adhere to the physician’s advice and insist on appropriate functional exercise after surgery. Furthermore, medical staff and rehabilitation therapists should also provide sufficient guidance and support to help patients increase their exercise compliance[15].
The mechanism of social support on postoperative ankle function is a complex research field. Social support encompasses the material or emotional support an individual receives from their social network, which can include family, friends, the wider community, or other social institutions. Social support plays an important role in rehabilitation after ankle surgery. First, social support can provide the necessary emotional support for patients. Surgery is a strong psychophysiological stressor, and patients often face emotional problems, such as pain, anxiety, and depression. At this time, the care, understanding, and encouragement provided by families, friends, and medical staff can help patients relieve tension, bolster rehabilitation confidence, and improve treatment compliance[16]. Second, social support can help patients obtain better postoperative and life care, such as assistance in functional exercises and provision of a nutritious diet. The care and help given by family members and friends can help patients recover better. In addition, social support can also include information and knowledge support for patients. Postoperative patients need to understand the different aspects of rehabilitation training and daily rehabilitation nursing to improve self-management and rehabilitation progress. Medical staff and rehabilitation physicians can also provide patients with relevant information to help them better understand and retain rehabilitation knowledge and skills. In conclusion, the impact of social support on postoperative function after ankle surgery is manifold in providing patients with the emotional support, postoperative nursing, and life care, as well as the information and knowledge they might need to achieve optimal recovery. Therefore, in rehabilitation after ankle surgery, the role of social support should be emphasized, and patients should be encouraged to actively seek and utilize social support resources for optimal recovery[17]. At the same time, medical staff and social workers should also evaluate the patient’s social support status and provide necessary support and help if needed.
BK, PGE 2, and 5-HT are bioactive substances with distinct roles in pain transmission and inflammatory response. BrBK is a peptide produced in vascular endothelial cells and has strong physiological activity[18]. The release of BK promotes vasodilation and increased permeability while enhancing pain perception at nerve endings. In tissue damage or inflammation, BK levels are often elevated, which indicates increased pain. PGE2 is a prostaglandin-like substance and an important mediator of inflammatory response. It can increase pain perception by stimulating inflammatory cells to release PGE2 receptors at nerve endings. PGE2 also participates in the inflammatory process, promotes congestion, edema, and the release of inflammatory mediators in local tissues, resulting in aggravated tissue injury and pain. 5-HT is a neurotransmitter that mainly functions in the central nervous system and peripheral tissues. It helps transmit pain signals in peripheral nerve terminals[19]. Furthermore, 5-HT can promote pain symptoms by stimulating 5-HT receptors and increasing neuronal excitability and pain perception. The interactions among BK, PGE2, and 5-HT in pain perception and inflammatory response form a complex regulatory network. However, the reduction of pain symptoms can be effectively mediated through periodic functional training[20].
In conclusion, the independent risk factors affecting functional performance after staged functional training following ankle surgery are exercise compliance, social support and pain level. Clinical nursing care after ankle surgery needs to integrate analgesic and health education measures to promote and optimize limb function recovery. To optimize rehabilitation, patients should follow the physician’s advice and insist on appropriate functional exercise after surgery. Furthermore, medical staff and rehabilitation therapists should also provide patients sufficient guidance and support to improve their exercise compliance. Relevant studies that analyzed independent risk factors affecting intervention nursing in ankle function recovery are lacking. Further nursing studies involving larger datasets and multiple centers need to be performed to provide robust data and reference for clinical practice.
| 1. | Kang HJ, Lee JW, Kwon YM, Kim SJ. Epidemiology of Ankle Fractures in Korea: A Nationwide Population-Based Study. J Korean Med Sci. 2022;37:e288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Moseley AM, Beckenkamp PR, Haas M, Herbert RD, Lin CW; EXACT Team. Rehabilitation After Immobilization for Ankle Fracture: The EXACT Randomized Clinical Trial. JAMA. 2015;314:1376-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Keene DJ, Williamson E, Bruce J, Willett K, Lamb SE. Early ankle movement versus immobilization in the postoperative management of ankle fracture in adults: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2014;44:690-701, C1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Beckenkamp PR, Lin CC, Herbert RD, Haas M, Khera K, Moseley AM; EXACT Team. EXACT: exercise or advice after ankle fracture. Design of a randomised controlled trial. BMC Musculoskelet Disord. 2011;12:148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Auais MA, Eilayyan O, Mayo NE. Extended exercise rehabilitation after hip fracture improves patients' physical function: a systematic review and meta-analysis. Phys Ther. 2012;92:1437-1451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 118] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 6. | Smith JM, Boe EA, Will R. Physician Wellness in Orthopedic Surgery: Challenges and Solutions. Orthop Clin North Am. 2021;52:41-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Moustafa A, Khan MS, Alsamman MA, Jamal F, Atalay MK. Prognostic significance of T1 mapping parameters in heart failure with preserved ejection fraction: a systematic review. Heart Fail Rev. 2021;26:1325-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Schneider W, Jurenitsch S. Normative data for the American Orthopedic Foot and Ankle Society ankle-hindfoot, midfoot, hallux and lesser toes clinical rating system. Int Orthop. 2016;40:301-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17520] [Cited by in RCA: 21820] [Article Influence: 606.1] [Reference Citation Analysis (0)] |
| 10. | Keene DJ, Costa ML, Tutton E, Hopewell S, Barber VS, Dutton SJ, Redmond AC, Willett K, Lamb SE. Progressive functional exercise versus best practice advice for adults aged 50 years or over after ankle fracture: protocol for a pilot randomised controlled trial in the UK - the Ankle Fracture Treatment: Enhancing Rehabilitation (AFTER) study. BMJ Open. 2019;9:e030877. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Bruder AM, Shields N, Dodd KJ, Hau R, Taylor NF. A progressive exercise and structured advice program does not improve activity more than structured advice alone following a distal radial fracture: a multi-centre, randomised trial. J Physiother. 2016;62:145-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Kandemir V, Akar MS, Yiğit Ş, Durgut F, Atiç R, Özkul E. Can American Orthopaedic Foot and Ankle Society (AOFAS) score prevent unnecessary MRI in isolated ankle ligament injuries? J Orthop Surg (Hong Kong). 2022;30:10225536221131374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Büker N, Şavkın R, Ök N. Comparison of Supervised Exercise and Home Exercise After Ankle Fracture. J Foot Ankle Surg. 2019;58:822-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Velasco BT, Chien B, Kwon JY, Miller CP. Online Ratings and Reviews of American Orthopaedic Foot and Ankle Surgeons. Foot Ankle Spec. 2020;13:43-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Macaulay A, Nandyala SV, Miller CP, Ghorbanhoseini M, Walley KC, Kwon JY. Potential for Bias and the American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Scoring System. Foot Ankle Spec. 2018;11:416-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Song Y, Liu Y, Yuan Y, Jia X, Zhang W, Wang G, Jia Y, Wang X, Liu L, Li W, Li X, Cai N, Liu C, Li Y, Han Y, Zhou Y, Mi X, Shi C, Wang JQ, Vuylsteke A, Guo X, Li Z. Effects of general versus subarachnoid anaesthesia on circadian melatonin rhythm and postoperative delirium in elderly patients undergoing hip fracture surgery: A prospective cohort clinical trial. EBioMedicine. 2021;70:103490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Gibbs JL, Diogenes A, Hargreaves KM. Neuropeptide Y modulates effects of bradykinin and prostaglandin E2 on trigeminal nociceptors via activation of the Y1 and Y2 receptors. Br J Pharmacol. 2007;150:72-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Cheng H, Huang H, Guo Z, Chang Y, Li Z. Role of prostaglandin E2 in tissue repair and regeneration. Theranostics. 2021;11:8836-8854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 152] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 19. | Gibbs E, Chakrapani S. Structure, Function and Physiology of 5-Hydroxytryptamine Receptors Subtype 3. Subcell Biochem. 2021;96:373-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Naqvi WM, Qureshi MI. Rapid Synthesis of the Literature on the Evolution of Gamification in Distal Radial Fracture Rehabilitation. Cureus. 2022;14:e29382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |