Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4331
Revised: April 24, 2024
Accepted: April 26, 2024
Published online: July 16, 2024
Processing time: 118 Days and 21.8 Hours
Nasal trauma presents a risk of foreign body invasion into the nasal cavity. However, in the early treatment stage of nasal trauma, patients and doctors are not always aware of possible foreign body invasion, resulting in delayed detec
Consultation with the patient revealed a history of nasal trauma 30 years prior that did not receive thorough examinations and imaging during treatment, resulting in a glass fragment retained in the nasal cavity adjacent to the orbit. After admission, computerized tomography (CT) confirmed the presence of the foreign body in the patient’s left nasal–maxillary sinus. The nasal foreign body led to symptoms such as chronic sinusitis, nasal polyps, fungal infection, and deviated nasal septum. The foreign body was successfully removed by nasal endoscopy, polypectomy, sinus fungal removal, left middle turbinate conchoplasty, fenestration via the right inferior meatus, nasal endoscopic maxillary sinus cystectomy, and septolplasty. The operation was successful and without any complications.
CT scans should be performed in addition to necessary debridement sutures to avoid possible foreign body invasion during nasal trauma. Surgical planning should be tailored to the patient’s specific situation. The surgical method should be carefully selected, and sufficient preparation should be undertaken before the surgery to avoid possible displacement of the nasal foreign body.
Core Tip: A 56-year-old man presented with persistent nasal congestion and purulent discharge caused by a glass foreign body retained in the nasal cavity adjacent to the orbit. This report describes the details of the patient’s medical history, clinical manifestations, diagnostic process, and successful surgical treatment and is further supported by a literature review.
- Citation: Wang D, Liu Q, Liu H, Wei JS. Nasal congestion caused by long-term retention of a nasal foreign body near the orbit: A case report. World J Clin Cases 2024; 12(20): 4331-4336
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4331.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4331
Nasal foreign bodies are commonly encountered in the emergency department and require prompt intervention to avoid the onset and progression of complications. Foreign bodies in the nasal cavity are frequently reported in children but may also be encountered in adults with mental disorders or nasal trauma[1,2]. Adult patients often lack awareness of nasal ectopia, which delays treatment. Foreign bodies can remain in the nasal cavity for weeks, months, or even years, and may be concealed by the nasal mucosa, causing rhinoliths to form[3]. Nasal foreign bodies can cause swelling and erosion of the nasal mucosa, ulcers, nosebleeds, and, in extreme cases, nasal septal perforations[4]. Purulent nasal discharge, nosebleeds, and foul-smelling nasal cavity, should raise suspicion of nasal foreign bodies[5].
Nasal trauma presents a risk of foreign body invasion into the nasal cavity. Small foreign bodies, such as glass fragments and sand particles, may enter the nasal cavity through a tear in the nose sustained during impact. Therefore, thorough examinations and documentation are crucial for the treatment of patients with nasal injuries. However, in the early treatment stage of nasal trauma, some patients and doctors may not be aware of possible foreign body invasion, which causes delayed detection, potentially leading to the long-term retention of nasal foreign bodies, which can cause symptoms such as nasal congestion, sinusitis, and nasal polyps.
This report describes a case of a nasal foreign body lodged close to the orbit, causing nasal congestion and other symptoms. A literature review was conducted to discuss the clinical manifestations, surgical methods, and precautions in dealing with nasal foreign bodies. This aims to enhance the comprehension of clinicians and patients regarding nasal trauma-induced foreign body invasion and provide feasible surgical reference for the removal of nasal foreign bodies and management of complications.
The patient, a 56-year-old man, complained of left nasal obstruction accompanied by yellow purulent discharge for 1 month and bloody nasal discharge for 2 d. He was admitted to our hospital on November 2, 2023.
The patient presented no obvious inducement or cause for left nasal congestion that began 1 month prior. The complaint was accompanied by yellow purulent discharge but no fever, recurrent epistaxis, headache, or continuous sneezing; and by a diminished sense of smell, nasal odor, left facial pain, and toothache but no aural fullness, tinnitus, or hearing loss. The symptoms were alleviated after treatment with anti-inflammatory drugs administered at the local clinic but subsequently recurred. The patient complained of bloody nasal discharge 2 d prior. The patient was admitted to our hospital for further diagnosis and treatment after an outpatient examination diagnosed him with a nasal mass on the left side. The patient had a fair mental state, fair appetite, good sleep, normal bowel movement and urination, good physical condition, and no significant changes in body weight since the onset of the complaints.
The patient had coronary heart disease and atrial fibrillation 8 years prior with no further details. He also revealed nasal trauma sustained more than 30 years ago with no further details. He had undergone cardiac radiofrequency ablation for atrial fibrillation 4 months prior. He had no significant history of blood transfusion, allergies, or vaccination.
The patient was born locally. He denied any history of long-term foreign residence, residence in epidemic areas, or exposure to specific chemicals, dust, drug abuse, prostitution, drugs, or radioactivity. He had a smoking history of more than 30 years with 10 cigarettes per day but denied any alcohol use.
The auricle showed no deformities, lacerations, redness, swelling, or traction pain. The external auditory canal was spacious and clean, without atresia, redness, swelling, bleeding, or water/pus discharge. Tympanic membrane: The light cone, anterior and posterior malleolar folds, malleolar prominence, malleolar stria, and the umbo of the tympanic membrane were visible, without congestion or perforation. Mastoid process: The skin showed no redness, tenderness, or laceration. No soft tissue defects were observed in the external nose. The nose showed no bruising or swelling; no deformities, bulges, collapse or skew, or skin lacerations were observed in the back of the nose. The skin of the nasal vestibule was not red, swollen, or chapped, and the nasal hair did not shed. Nasal cavity: The nasal septum was deviated to the right side without hematoma; the nasal mucosa was free from congestion and tearing. Bilateral inferior turbinates were swollen, with abundant yellow purulent discharge originating from the left common and middle nasal meatus. A neoplasm was found in the left nasal cavity, but no deep structures were seen. No neoplasms or purulent or bloody secretions were noted in the right middle nasal meatus and olfactory cleft. No tenderness was observed in the bilateral maxillary sinuses, ethmoid sinus, and frontal sinus. The uvula was centered; the pharyngeal mucosa was not congested; the bilateral tonsils were enlarged (grade I); and the surface was smooth with no secretions. The epiglottis was not curled but exhibited poor lifting; the mucosa was not red or swollen; and the glottic structure could not be detected.
Routine preoperative examination.
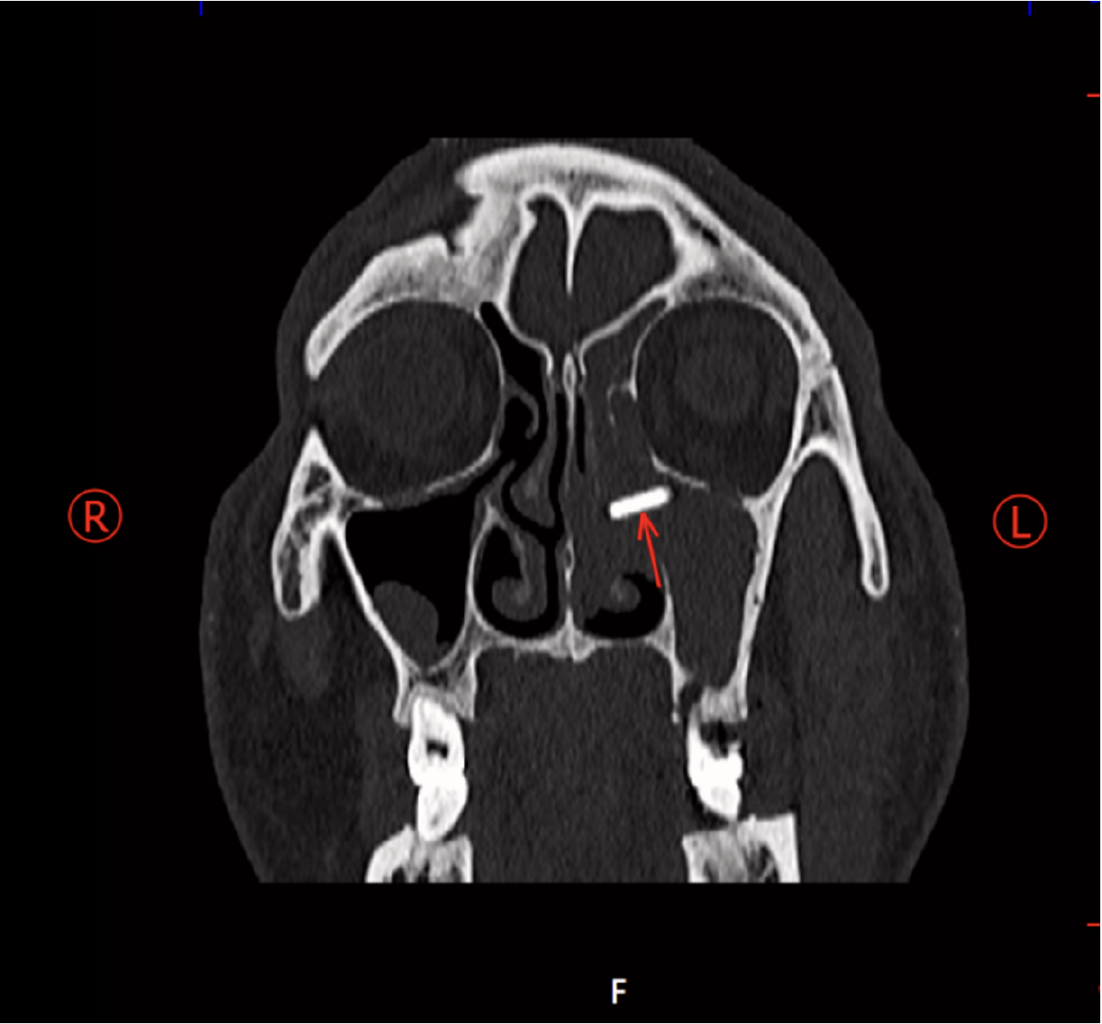
Computerized tomography (CT) of the paranasal sinuses revealed a high-density streak shadow in the left nasal cavity–maxillary sinus junction, indicating a high possibility of a foreign body (Figure 1). The soft tissue density shadow observed in the left nasal cavity was suspected to be a polyp. The patient’s condition was diagnosed as bilateral sinusitis, with signs of left-sided obstructive sinusitis. The possibility of a submucosal cyst of the right maxillary sinus, enlargement of the bilateral inferior turbinates, and deviated nasal septum were also raised.
A 56-year-old man presented with persistent nasal congestion and purulent discharge caused by a glass foreign body retained in the nasal cavity adjacent to the orbit.
Fenestration of left maxillary sinus, ethmoid sinus, and frontal sinus by nasal endoscopy; removal of foreign body in the left middle nasal meatus; left nasal polypectomy; left maxillary sinus fungal removal; left middle turbinate conchoplasty; fenestration via the right inferior meatus; nasal endoscopic maxillary sinus cystectomy; septolplasty; and plasma radiofrequency ablation of bilateral inferior turbinates.
After inducing general anesthesia, the patient was placed in the supine position, followed by routine skin preparation and draping. Surface contraction anesthesia of the nasal cavity was induced using tetracaine–epinephrine pads. Nasal endoscopy revealed that the nasal septum was left-deviated at a low position and right-deviated at a high position. After administering local infiltration anesthesia containing 1% lidocaine and a small amount of adrenaline at the skin–mucosa junction of the left nasal septum, an L-shaped incision was made at the junction with a bead slice to incise the mucoperichondrium on the left side of the nasal septum to the cartilage. A stripper was then used to separate the mucoperichondrium and mucoperiosteum on the left side of the nasal septum to the required extent, and the nasal septal cartilage was incised at approximately 2 mm after the mucoperichondrial incision to separate the contralateral mucope
During nasal endoscopy, tetracaine–epinephrine pads were used to contract and anesthetize the bilateral nasal mucosa. A neoplasm was found in the left middle nasal meatus, which was identified as a polypoid transformation of the left middle turbinate and left uncinate process. The polypoid tumor was then locally infiltrated with 1% lidocaine and a small amount of adrenaline and subsequently retrieved using nasal punch forceps and sent for rapid pathological examination. After removing part of the left middle turbinate, a foreign body was retrieved from the left middle meatus, which turned out to be a triangular piece of glass approximately 2 cm long (Figure 2). The left uncinate process was removed, and the left maxillary sinus opening was enlarged. The yellowish-brown caseous secretion was found to originate in the left maxillary sinus. The left maxillary sinus mucosa was significantly edematous and thickened. The caseous secretion was aspirated using an elbow aspirator for pathological examination, and the sinus cavity was rinsed repeatedly with normal saline. Subsequently, 70-degree nasal endoscopy was performed to examine the maxillary sinus for any residual secretions. The edema and hypertrophic mucosa were effectively removed using a suction cutter, ensuring sufficient hemostasis. Following that, the left ethmoidal vesicle was removed, and the left anterior and posterior ethmoidal sinuses and left frontal sinus were opened successively. Each sinus cavity exhibited edema and hypertrophy of the mucous membrane, which was then removed using a suction cutter, followed by sufficient hemostasis. Next, the right inferior turbinate was fractured and pushed inward, and the lateral wall of the right inferior nasal meatus was anesthetized with 1% lidocaine–adrenaline solution via local mucosal infiltration. The mucosa was removed using a suction cutter, leaving a fenestration approximately 1.5 cm × 1.5 cm in size in the inferior nasal meatus. Nasal endoscopy revealed a cyst-like neoplasm in the right maxillary sinus, with its root located on the lateral wall. The cyst was completely removed using large curved forceps, subsequent 70-degree nasal endoscopy confirmed the absence of any residual tumor. The root of the neoplasm was cauterized by bipolar suction electrocoagulation, and the right inferior turbinate was reduced after adequate hemostasis.
Bilateral inferior turbinate mucosae underwent low-temperature plasma radiofrequency ablation, followed by confirmation of reduced turbinate volume and ensuring adequate hemostasis. The bilateral nasal cavities were filled with NasoPore and an expansive sponge to complete the procedure. The intraoperative bleeding was about 150 mL, and the operation was uneventful. After recovery from anesthesia, the patient was transferred to the anesthesia recovery room. The pathological samples were reviewed by family members and sent for pathological examination. The patient was satisfied with the treatment.
The left nasal cavity presented with inflammatory edema, glandular fibrovascular polyps, subacute inflammation, and scattered eosinophilic infiltration. The caseous secretion from the left maxillary sinus was identified as a fungal mass with extensive degeneration and necrosis. The right maxillary sinus showed a retention cyst with chronic inflammation.
The majority of nasal foreign body cases were documented in infants or children, with only a few occurrences in adults. Nasal foreign bodies in adults occur because of: (1) Accident injuries; and (2) injuries due to concomitant mental disorders. Patil et al[6] reported a rare case of a nasal foreign body in a 42-year-old woman who was using a toothbrush head to relieve itching caused by allergic rhinitis when she fell, causing the toothbrush head to break and become lodged in the nasal cavity. Bahranifad et al[3] described a case of nasal lodgment of cotton resulting from a fall in the garden, which caused nasal mucosal congestion, swelling, and calcification into nasal stones. In this report, CT examination showed a hyperdense streak in the left superior nasal sinus. Consultation with the patient revealed a nasal injury caused by a fall 30 years ago. At that time, only debridement and suturing were performed, without thorough examinations and imaging, which resulted in the oversight of a foreign body in the nasal cavity. Therefore, patients with nasal trauma should undergo careful examination of the nasal cavity and be evaluated by CT to avoid long-term retention of foreign bodies in the nasal cavity and additional treatment costs.
Nasal foreign bodies present non-specific or asymptomatic symptoms, posing major challenges in clinical diagnosis. Novák et al[7] described the case of an elderly patient who underwent endoscopic surgery for severe craniofacial trauma and cerebrospinal fluid rhinorrhea. During the operation, a spectacle lens was found in the patient’s left nose. However, no foreign bodies had been found in the left nasal purulent secretions, ventilation impairment tests, and nasal endoscopy over the years. Thus, imaging technology plays an important role in identifying foreign bodies in the nasal cavity. A case report involving older adults found that CT imaging can accurately identify high-density foreign bodies in the mediastinum of the neck, whereas electronic laryngoscopy cannot detect foreign bodies in the larynx or pyriform sinus[8]. CT imaging also helps in distinguishing between rhinitis caused by small foreign bodies and those caused by non-foreign bodies. Lafuma et al[9] found that CT imaging can be used to distinguish grass awn foreign body rhinitis from non-foreign body rhinitis. Mendiratta et al[10] confirmed the wealth of information on anatomical variations that can be identified on CT, which would be pivotal in the thorough evaluation of patients with chronic sinusitis. Thus, CT is highly useful in detecting nasal foreign bodies. In the present study, the patient was thoroughly examined, and the presence of foreign bodies in the nasal cavity was determined by CT. In addition, this case illustrated that following the exclusion of rhinitis without evident foreign bodies or etiology, CT can be performed after assessing the patient’s trauma history, to investigate the potential presence of a concealed foreign body lodged deep within the nasal cavity.
Long-term retention of foreign bodies in the nasal cavity can cause chronic sinusitis and symptoms such as nasal congestion and nosebleeds[11]. Furthermore, nasal foreign bodies are typically found in the front of the nasal cavity, the inferior turbinate, or the septum. Most nasal foreign bodies can be removed with tweezers, curved hooks, or aspirators. However, when the foreign body is lodged in the upper sinus or larger than 3 mm, nasal endoscopic surgery under general anesthesia is required[12,13]. In the present case, the patient had retained a nasal foreign body for up to 30 years. Such prolonged retention of foreign bodies will cause continuous damage to the surrounding nasal tissues, specifically nasal mucosal damage and cell death. Cell death induces the release of numerous intracellular substances, which promote the release of cytokines and immune cells. This is the cause of chronic sinusitis, fungal infections, and nasal polyps in the current case. This condition is complex and necessitates additional treatment and management strategies. Nasal foreign bodies should be surgically removed. In addition to foreign body removal, procedures such as polypectomy, fungal removal, and turbinate rhinoplasty are also required. In the present case, the location of the foreign body close to the orbit is peculiar. During the operation, changes in intranasal pressure, sudden conditions, autoimmune reactions, and bone absorption may all cause the displacement of foreign bodies[14], which can invade the orbit and cause eye injury. Therefore, the surgical approach should be carefully selected, and adequate preoperative preparations should be undertaken. This study provides reference on a targeted surgical plan that can be performed in similar cases of nasal foreign body retention once the foreign object is accurately located.
In conclusion, nasal trauma increases the risk of fragment invasion, leading to the lodgment of foreign bodies in the nasal cavity. Early management of patients with nasal trauma should be conducted with caution, and CT scans should be performed in addition to necessary debridement sutures to avoid possible foreign body invasion. Surgical planning decisions should be tailored to the patient’s specific situation. Intraoperatively, the surgical method should be considered carefully, and sufficient preoperative preparation should be undertaken to avoid displacement of the nasal foreign body.
| 1. | Asiri M, Al-Khulban MS, Al-Sayed G. Foreign Body in the Nasal Cavity: A Case Report. Cureus. 2023;15:e50373. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Jung HJ, Kim SW, Lee JS, Choi HG, Wee JH. Analysis of Nasal Foreign Bodies in South Korea: Over 10-Year Experience. Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Bahranifad H, Zandifar Z, Zaheri PM, Wallin L, Karimi Akhormeh A, Parsa N. Prolonged Undiagnosed Nasal Foreign Body Case Report. Indian J Otolaryngol Head Neck Surg. 2022;74:1242-1245. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Baranowski K, Al Aaraj MS, Sinha V. Nasal Foreign Body. StatPearls. Treasure Island (FL) with ineligible companies. Disclosure: Mahmoud Al Aaraj declares no relevant financial relationships with ineligible companies. Disclosure: Virteeka Sinha declares no relevant financial relationships with ineligible companies, 2023. |
| 5. | Hira İ, Tofar M, Bayram A, Yaşar M, Mutlu C, Özcan İ. Childhood Nasal Foreign Bodies: Analysis of 1724 Cases. Turk Arch Otorhinolaryngol. 2019;57:187-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Patil PM, Anand R. Nasal foreign bodies: a review of management strategies and a clinical scenario presentation. Craniomaxillofac Trauma Reconstr. 2011;4:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Novák V, Hrabálek L, Hoza J, Stejskal P. Unusual foreign body in the nasal cavity after craniofacial injury. Rozhl Chir. 2023;102:165-168. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Ma Z. Successful removal of metallic foreign body in the neck-mediastinum via the parapharyngeal space approach. Ear Nose Throat J. 2022;1455613221084076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 9. | Lafuma F, Baudin Tréhiou C, Bernardin F, Blond L. Computed tomography may be helpful in discriminating grass awn foreign body rhinitis from non-foreign body rhinitis in dogs. Vet Radiol Ultrasound. 2021;62:533-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Mendiratta V, Baisakhiya N, Singh D, Datta G, Mittal A, Mendiratta P. Sinonasal Anatomical Variants: CT and Endoscopy Study and Its Correlation with Extent of Disease. Indian J Otolaryngol Head Neck Surg. 2016;68:352-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Yaroko AA, Baharudin A. Patterns of nasal foreign body in northeast Malaysia: A five-year experience. Eur Ann Otorhinolaryngol Head Neck Dis. 2015;132:257-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Çaytemel B, Çelik M, Öztürk İE, Türel MNK. Unusual Foreign Body in Nasal Cavity for 40 Years After Septoplasty. Ear Nose Throat J. 2021;100:423-424. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Lee JH. A Foreign Body in the Ostium of the Maxillary Sinus. Ear Nose Throat J. 2021;100:NP281-NP282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Du XW, Zhang JB, Xiao SF. Nasal septal foreign body as a complication of dental root canal therapy: A case report. World J Clin Cases. 2021;9:690-696. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |