Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4317
Revised: April 29, 2024
Accepted: May 22, 2024
Published online: July 16, 2024
Processing time: 154 Days and 17.4 Hours
Mast cell leukemia (MCL), a subtype of systemic mastocytosis (SM), is an extremely rare clinical entity characterized by a very poor prognosis. Chemothe
The authors, hereby, report a case of a 46-year-old female patient diagnosed with MCL-the rarest subtype of SM. The patient presented to the gastroenterology clinic with multiple, various, and unspecific gastroenterological symptoms. Concomitance of skin lesions significantly contributed to a relatively prompt diagnosis. The serum tryptase level was extremely high and bone the marrow aspirate showed an infiltration of atypical mast cells. The disease was rapidly progressive and primary refractory to chemotherapy and the patient succumbed to the illness about a month after the initiation of treatment.
Despite its “hematological nature”, MCL, in most cases presents dominantly with unspecific gastroenterological symptoms. Thus, a high disease awareness among physicians other than hematologists is necessary to improve treatment outcomes. Serum tryptase level, due to its non-invasive nature and easy access, may serve as an initial step to estimate the probability of mastocytosis.
Core Tip: Mastocytosis is a group of neoplastic diseases characterized by excessive proliferation and infiltration of pathologic mastocytes into many organs in the human body. The clinical course of the illness may vary from indolent types, with average life expectancy, to advanced severe forms associated with poor prognosis. A disease may present with plenty of unspecific symptoms resulting in a long-lasting diagnostic process. We report a rare case of mast cell leukemia (MCL) in a 46-year-old female with weakness, unintentional weight loss, spine pain, vomiting, diarrhea, and epigastric pain occurring within several months before hospitalization. Although MCL is still associated with a high morbidity index, other less aggressive forms of systemic mastocytosis may be successfully treated with chemotherapy.
- Citation: Wysocki MT, Gonciarz M, Puła B. Treatment refractory mast cell leukemia with dominant gastrointestinal manifestation and concomitant skin symptoms: A case report. World J Clin Cases 2024; 12(20): 4317-4324
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4317.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4317
Mastocytosis is a group of neoplastic diseases characterized by the excessive proliferation and infiltration of pathologic mastocytes into many organs in the human body. The annual incidence of the disease is estimated to be about 5-10 cases per million individuals in the general population. The clinical course of the illness may vary from indolent types with average life expectancy to advanced severe forms associated with poor prognosis. Multiple and various non-specific symptoms are both effects of organ infiltration (e.g., hepatosplenomegaly, malabsorption, peripheral blood cytopenias, osteolytic lesions, and pathological fractures) and the release of mast cell mediators such as histamine (skin symptoms, diarrhea, vomiting, peptic ulcers)[1-6]. Consequently, a mastocytosis diagnosis is often only made several years after the onset of symptoms.
A 46-year-old female patient with no past medical history was urgently admitted to our Gastroenterology Department due to progressive weakness, unintentional weight loss (approximately 7 kg within a month), night sweats, vomiting with food content, diarrhea, epigastric pain, lumbar spine pain and paroxysmal pressing pain in the chest.
These symptoms had appeared with variable intensity for the 10 months and exacerbated within the last two months before hospitalization. According to the patient, the most severe and dominant complaints affected the gastrointestinal system.
On account of the presenting symptoms, the patient was consulted twice in the emergency department and diagnosed on an outpatient basis. Initially, the only abnormalities in laboratory tests were macrocytic anemia with a hemoglobin of 8.1 g/dL, mean corpuscular value (MCV) 101 fl, and thrombocytopenia with a platelet count of 127 × 109/l. Inflammatory markers, pancreatic and hepatic enzymes, as well as cholestasis workup, assessed several times over several months, remained within the normal range. Only mild hepatosplenomegaly was found in the ultrasound of the abdomen. During one of her visits to the emergency department, due to an unclear clinical picture, the diagnostics were extended to include a contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis, which showed hepatomegaly 170 mm in the CC length with multiple, small contrast-enhancing focal lesions, splenomegaly 160 mm in the CC length, dilation of the portal and splenic vein, L5 vertebra fracture and enlargement of the uterus with features of pelvic congestion syndrome.
Due to partial relief after the administration of analgesics and antiemetic drugs, the patient did not consent to hospitalization and agreed to continue diagnostics on an outpatient basis.
A gastroscopy showed features of gastritis with the presence of hemorrhagic erosions in the stomach and duodenum and small ulcerations up to 5 mm, with no signs of active bleeding. Helicobacter pylori eradication treatment was administered due to a positive urease test. The histopathological examination of biopsies obtained revealed chronic, active, atrophic gastritis. Histopathological and immunological diagnostic tests for celiac disease were negative. A colonoscopy showed no abnormalities or pathological findings. In gynecological diagnostics, neoplasms of the reproductive organs were excluded.
Despite the treatment, the symptoms did not subside, and the patient`s condition continued to deteriorate, leading to an admission to the Department of Gastroenterology. There has not been any hematologic malignancy reported in the patient`s family medical history so far.
The physical examination showed signs of severe cachexia and peripheral edema. During her hospitalization, we observed paroxysmal, sharply demarcated erythema of the skin (flushes) on the face and chest. According to the patient, these changes appeared for several months, usually during times of emotional stress. They were short-lasting and resolved spontaneously.
In laboratory tests, macrocytic anemia with thrombocytopenia persisted. Additionally, hypoalbuminemia and elevated prothrombin time were observed, with no deviations in other biochemical parameters-Table 1. The peripheral blood smear showed significant anisocytosis and poikilocytosis of red blood cells. Anemia due to deficiencies was excluded concentrations of iron, vitamin B12, and folic acid were within the normal reference range. No monoclonal protein was found in the serum proteinogram, and calcium and parathyroid hormone concentrations were normal.
| Parameter, unit | Result | Normal range |
| WBC (×109/L) | 6.99 | 4.30–9.64 |
| RBC (×1012/L) | 2.71 | 3.81–5.13 |
| HGB (g/dL) | 8.5 | 12.0–15.1 |
| Htc (%) | 27 | 35-46 |
| MCV (fl) | 103 | 80-99 |
| MCH (pg) | 31.4 | 27.0–33.5 |
| MCHC (g/dL) | 31.3 | 31.5–36.0 |
| RDW (CV%) | 20.1 | 11.2–13.7 |
| PLT (× 109/L) | 112 L | 163-347 |
| Neutrophil (× 109/L) | 4.0 | 1.93– 5.87 |
| Lymphocyte (× 109/L) | 1.59 | 1.23–3.42 |
| Monocyte (× 109/L) | 1.14 H | 0.26–0.78 |
| Eosinophil (× 109/L) | 0.03 | 0.03–0.37 |
| Basophil (× 109/L) | 0.02 | 0.02–0.08 |
| APTT (s) | 28.3 | 23-35 |
| PT (s) | 16.8 | |
| INR | 1.48 | |
| Albumin (g/dL) | 3.5 | 3.9–4.9 |
| Total protein (g/dL) | 5.2 | 6.4–8.3 |
| Calcium (mg/dL) | 8.9 | 8.6-10.2 |
| Sodium (mmol/L) | 138 | 136-145 |
| Potassium (mmol/L) | 4.6 | 3.5–5.1 |
| Parathyroid hormone (pg/mL) | 9.2 | 15-65 |
| Iron (μg/dL) | 67 | 60-180 |
| Vit B12 (pg/mL) | 200 | 191-663 |
| Folic acid (ng/mL) | 5.2 | 4.5–37.3 |
| C-reactive Protein (mg/dL) | 0.3 | 0-0.8 |
| Alanine aminotransferase (U/L) | 10 | 0-33 |
| Aspartate aminotransferase (U/L) | 10 | 0-31 |
| Bilirubin (mg/dL) | 0.3 | 0-1.2 |
| Alkaline phosphatase (U/L) | 69 | 35-104 |
| Lipase (U/L) | 31 | 0-67 |
| Amylase (U/L) | 6 | 0-100 |
| Creatinine (mg/dL) | 0.5 | 0.5-0.9 |
| Thyroid-stimulating hormone (μIU/Ml) | 0.352 | 0.27-4.2 |
| Lactate Dehydrogenase (U/L) | 126 | 135-223 |
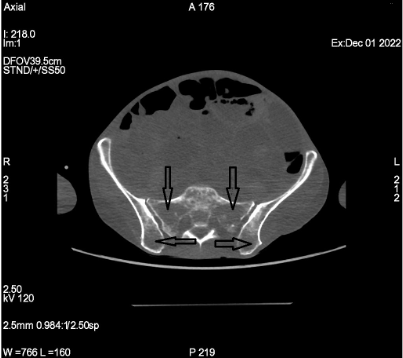
Moreover, a CT scan of the chest and abdomen revealed further progression of lytic lesions in the bones (Figure 1) and multilevel compression fractures of the spine suggesting a neoplastic process.
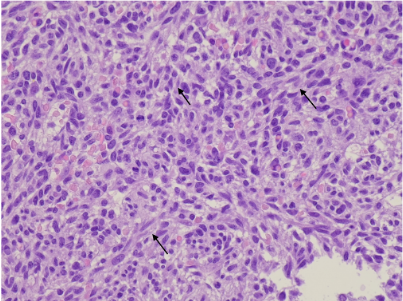
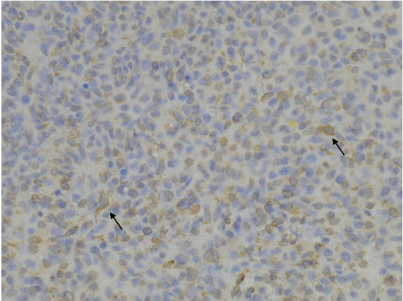
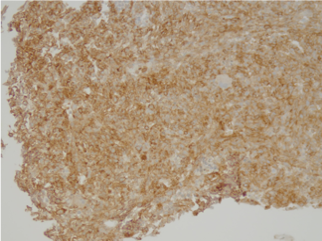
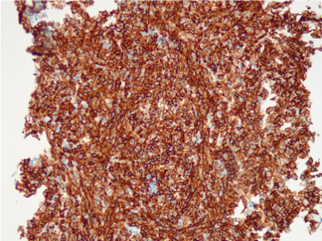
Based on the overall clinical picture and the diagnostics performed so far, a suspicion of systemic mastocytosis (SM) was raised, leading to further diagnostic tests, including serum tryptase level and a bone marrow trephine biopsy. The assessed serum tryptase level was extremely high 1834 ug/L (normal range up to 11.4 ug/L), while the cytological and immunophenotypic examination of the bone marrow aspirate showed infiltration of atypical mast cells with immuno
The patient was transferred for further treatment to the Hematology Department, where she was qualified for a chemo
Unfortunately, the patient had the primary refractory disease (77.4% mast cells in bone marrow aspirate after the first chemotherapy cycle vs 73.3% before treatment), and she succumbed to the illness about a month after the initiation of treatment due to cytopenic complications (central nervous system and gastrointestinal bleeding).
As mentioned above, SM is a rare medical condition, with MCL most likely being its rarest subtype. It belongs to the group of advanced SM, along with aggressive SM and SM with associated hematologic (myeloid) neoplasm[7,8]. It takes an acute form with organ damage (the so-called C findings, i.e., cytopenias resulting from bone marrow infiltration, hepatomegaly with impairment of liver function, splenomegaly with hypersplenism, malabsorption with weight loss and osteolytic changes and/or pathological fractures) or, much more rarely, the chronic form without C symptoms. Additionally, due to the presence of atypical immature mast cells in the peripheral blood, a distinction is made between the more common aleukemic form (< 10% of mast cells) and the rarer leukemic form (> 10%). MCL has a very poor prognosis with a median overall survival (OS) of approximately 1.6 years). It can occur de novo (70.7%) or secondary to other forms of mastocytosis as a disease progression (29.3%). For the definitive diagnosis of SM, a histopathological examination of the affected organ (except for the skin) is necessary[1,5-10]. The criteria for diagnosis are presented in the Table 2. The diagnosis of MCL requires the presence of > 20% of atypical/immature mast cells in a bone marrow aspiration biopsy.
| Criteria | Description |
| Major criterion | Multifocal dense infiltrates of mast cells MCs (≥ 15 MCs in aggregates) in bone marrow trephine biopsies and/or in sections of other extracutaneous organ(s) |
| Minor criteria | (1) Presence of atypical mast cells in bone marrow smears or spindle-shaped mast cells in biopsies of internal organs (except skin) constituting > 25% of all types of mast cells |
| (2) Presence of KIT gene mutation in the bone marrow or another extracutaneous organ(s) | |
| (3) MCs in bone marrow, blood, or other extracutaneous organs expressing CD25 and/or CD2 and/or CD30 | |
| (4) Serum tryptase concentration > 20 ng/ml (does not apply to patients with other malignancies of the hematopoietic system accompanying mastocytosis) | |
| According to WHO 2022, a major and one minor OR at least three minor SM criteria must be fulfilled to establish a diagnosis | |
| According to ICC 2022, a major criterion or at least 3 minor SM criteria must be fulfilled to establish a diagnosis | |
At the time of diagnosis, the patient fulfilled the major criterion and three minor criteria. After a few weeks, a negative result of the D816V KIT mutation was obtained. In addition, all C findings were present, and an acute, aleukemic variant was diagnosed with no evidence of a secondary nature (transformation from another SM variant).
Elevated serum tryptase concentration is not necessary for diagnosis. Still, due to its availability and non-invasive nature, it is very helpful in identifying the disease (concentrations > 20 ng/mL are associated with a high probability of SM). Hence, it may be the first-choice test when a biopsy of the affected organ or bone marrow is not readily available. However, it should be emphasized that an average value does not rule out the diagnosis[9,11]. Other non-specific laboratory abnormalities seen in SM (anemia, thrombocytopenia, elevated transaminases, and bilirubin) do not usually contribute to an earlier diagnosis.
Gastrointestinal symptoms are among the most common symptoms of SM, including MCL. They result primarily from the release of mediators (diarrhea, peptic ulcer disease, flatulence, abdominal pain), and, to a lesser extent from mast cell infiltration (malabsorption). They do not differ from those found in other, more common gastroenterological diseases. Any disease-specific endoscopic changes do not accompany them. Mast cell infiltration in the gastrointestinal tract, if present, may be focal and subtle, and its detection in the histopathological examination may require specific and non-routine staining (CD117, tryptase, CD25)[2,9,10].
In our patient’s case, gastroenterological symptoms were also dominant. Still, the key role in the relatively quick diagnosis (on the eighth day of hospitalization) was attributed to skin lesions in the form of urticaria and sudden skin flushing. While symptoms from the gastrointestinal tract are typical for advanced SM, skin lesions are usually observed in indolent forms[2,10]. In the histopathological examination of the gastric mucosa collected during gastroscopy, no mast cell infiltration was found in our patient (however, the assessment was performed about a month before admission and SM was not suspected at that time; therefore, no additional staining for atypical mast cells was performed).
As mentioned earlier, MCL has an inferior prognosis, and so far, no therapy allows for a long-term response. Based on current medical knowledge, the basic SM treatment (including MCL) is oral tyrosine kinase inhibitors (midostaurin and avapritinib). The use of midostaurin significantly prolonged survival (2.3 vs 1.1 years in patients not treated with midostaurin)[1,10,11]. In addition, regimens with cladribine and interferon-α are used. Allogeneic hematopoietic cell transplantation is a therapeutic option for young patients in good general condition who have responded to che
In the treatment of gastroenterological symptoms associated with the release of mediators (mostly histamine), H2-blockers are mainly used. In the case of SM, they are more effective than PPIs, which are recommended as first-line drugs in alleviating symptoms in other cases of peptic ulcer disease. Considering this, a better response to treatment with H2-blockers may suggest mastocytosis as the cause of peptic ulcer disease. Other drugs used to treat gastrointestinal symptoms are ketotifen, sodium cromoglycates (diarrhoea, abdominal pain), leukotriene modifiers, and glucocorticoids (ascites and malabsorption)[2,4,10].
Other diseases that should be included in the differential diagnosis of our patient's case are primarily hematological neoplasms with particular emphasis on myeloproliferative neoplasms, and endocrine disorders such as primary hyperparathyroidism, Cushing's syndrome or neuroendocrine neoplasms.
In most cases, MCL, despite its “hematological nature”, presents dominantly with unspecific gastroenterological symptoms. Diagnosing SM/MCL, especially in the absence of skin lesions, may be challenging. Many patients remain without proper treatment for extended periods of time, receiving only symptomatic therapy that results in progressive multiple-organ damage. Thus, a high disease awareness among physicians other than hematologists is necessary to improve treatment outcomes. Gastrological symptoms refractory to or frequently relapsing after first-line therapeutical are good reason for further investigation. Serum tryptase level, due to its non-invasive nature and easy access, may serve as an initial step to estimate the probability of mastocytosis[1,2,4,11].
| 1. | Zanelli M, Quintini M, Magnasco S, Aprile L, Palicelli A, Zizzo M, Sanguedolce F, Ricci S, Pancetti S, Zuccalà V, Martino V, Broggi G, Caltabiano R, Cavazza A, Parente P, Mecucci C, Martino G, Ascani S. Mast Cell Leukemia: An Update with a Practical Review. Cancers (Basel). 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Zanelli M, Pizzi M, Sanguedolce F, Zizzo M, Palicelli A, Soriano A, Bisagni A, Martino G, Caprera C, Moretti M, Masia F, De Marco L, Froio E, Foroni M, Bernardelli G, Alvarez de Celis MI, Giunta A, Merli F, Ascani S. Gastrointestinal Manifestations in Systemic Mastocytosis: The Need of a Multidisciplinary Approach. Cancers (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Leguit RJ, Wang SA, George TI, Tzankov A, Orazi A. The international consensus classification of mastocytosis and related entities. Virchows Arch. 2023;482:99-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 4. | Valent P, Akin C, Bonadonna P, Hartmann K, Brockow K, Niedoszytko M, Nedoszytko B, Siebenhaar F, Sperr WR, Oude Elberink JNG, Butterfield JH, Alvarez-Twose I, Sotlar K, Reiter A, Kluin-Nelemans HC, Hermine O, Gotlib J, Broesby-Olsen S, Orfao A, Horny HP, Triggiani M, Arock M, Schwartz LB, Metcalfe DD. Proposed Diagnostic Algorithm for Patients with Suspected Mast Cell Activation Syndrome. J Allergy Clin Immunol Pract. 2019;7:1125-1133.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 148] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 5. | Pardanani A. Systemic mastocytosis in adults: 2023 update on diagnosis, risk stratification and management. Am J Hematol. 2023;98:1097-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 39] [Reference Citation Analysis (0)] |
| 6. | Jawhar M, Schwaab J, Meggendorfer M, Naumann N, Horny HP, Sotlar K, Haferlach T, Schmitt K, Fabarius A, Valent P, Hofmann WK, Cross NCP, Metzgeroth G, Reiter A. The clinical and molecular diversity of mast cell leukemia with or without associated hematologic neoplasm. Haematologica. 2017;102:1035-1043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 73] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 7. | Leguit R, Hebeda K, Kremer M, van der Walt J, Gianelli U, Tzankov A, Orazi A. The Spectrum of Aggressive Mastocytosis: A Workshop Report and Literature Review. Pathobiology. 2020;87:2-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, Bejar R, Berti E, Busque L, Chan JKC, Chen W, Chen X, Chng WJ, Choi JK, Colmenero I, Coupland SE, Cross NCP, De Jong D, Elghetany MT, Takahashi E, Emile JF, Ferry J, Fogelstrand L, Fontenay M, Germing U, Gujral S, Haferlach T, Harrison C, Hodge JC, Hu S, Jansen JH, Kanagal-Shamanna R, Kantarjian HM, Kratz CP, Li XQ, Lim MS, Loeb K, Loghavi S, Marcogliese A, Meshinchi S, Michaels P, Naresh KN, Natkunam Y, Nejati R, Ott G, Padron E, Patel KP, Patkar N, Picarsic J, Platzbecker U, Roberts I, Schuh A, Sewell W, Siebert R, Tembhare P, Tyner J, Verstovsek S, Wang W, Wood B, Xiao W, Yeung C, Hochhaus A. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia. 2022;36:1703-1719. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 2161] [Article Influence: 720.3] [Reference Citation Analysis (0)] |
| 9. | El Hussein S, Chifotides HT, Khoury JD, Verstovsek S, Thakral B. Systemic Mastocytosis and Other Entities Involving Mast Cells: A Practical Review and Update. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Lee HJ. Recent advances in diagnosis and therapy in systemic mastocytosis. Blood Res. 2023;58:96-108. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Kennedy VE, Perkins C, Reiter A, Jawhar M, Lübke J, Kluin-Nelemans HC, Shomali W, Langford C, Abuel J, Hermine O, Niedoszytko M, Gorska A, Mital A, Bonadonna P, Zanotti R, Tanasi I, Mattsson M, Hagglund H, Triggiani M, Yavuz AS, Panse J, Christen D, Heizmann M, Shoumariyeh K, Müller S, Elena C, Malcovati L, Fiorelli N, Wortmann F, Vucinic V, Brockow K, Fokoloros C, Papageorgiou SG, Breynaert C, Bullens D, Doubek M, Ilerhaus A, Angelova-Fischer I, Solomianyi O, Várkonyi J, Sabato V, Rüfer A, Schug TD, Hermans MAW, Fortina AB, Caroppo F, Bumbea H, Gulen T, Hartmann K, Elberink HO, Schwaab J, Arock M, Valent P, Sperr WR, Gotlib J. Mast cell leukemia: clinical and molecular features and survival outcomes of patients in the ECNM Registry. Blood Adv. 2023;7:1713-1724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |