Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4191
Revised: May 16, 2024
Accepted: May 29, 2024
Published online: July 16, 2024
Processing time: 81 Days and 18.1 Hours
Tuberculosis (TB) is a chronic respiratory infectious disease that considerably jeopardizes human health, and there is no effective vaccine suitable for its pre
To investigate the promotion of medication adherence and disease cognition in patients with drug-resistant (DR-)TB using detailed nursing management.
In total, 114 patients with DR-TB who were diagnosed and treated at our hospital between January 2019 and January 2023 were included in this study. Patients in the control group (n = 57) were managed with conventional nursing care, while those in the observation group (n = 57) were managed with detailed nursing care. Medication adherence, disease awareness scores, medication safety, and nursing satisfaction were compared between the two groups after the intervention.
The post-intervention medication compliance rate was 91.23% in the observation group and 75.44% in the control group, with the former being 15.79% higher than the latter (P < 0.05). There was no statistically significant difference in the disease awareness scores between the two groups before the intervention; the disease awareness scores of the observation group were significantly higher than those of the control group after the intervention (P < 0.05). The incidence of gastrointes
Implementation of detailed nursing management for patients with DR-TB can effectively improve medication adherence, enhance awareness of the disease, ensure safety of medication, and improve satisfaction with nursing care.
Core Tip: To investigate the promotion of medication adherence and disease cognition in patients with drug-resistant tuberculosis using detailed nursing management. After the intervention, the results showed that the implementation of detailed nursing management for patients with drug-resistant tuberculosis can effectively improve patients’ medication adherence, enhance their awareness of the disease, ensure the safety of medication, and improve their satisfaction with nursing care, which is worthy of promotion and application in clinical practice.
- Citation: Chen YL, Xie YQ, Wei MY, Xu DM. Clinical effects of detailed nursing management interventions on medication adherence and disease perception in patients with drug-resistant tuberculosis. World J Clin Cases 2024; 12(20): 4191-4198
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4191.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4191
Tuberculosis (TB) is one of the top ten causes of death worldwide and one of the key chronic respiratory infectious diseases to be prevented and treated in China[1]. TB is primarily caused by the invasion of Mycobacterium tuberculosis (M. TB), which has a long incubation period, strong infectivity, is difficult to cure, and is easy to relapse[2]. In addition, the treatment cycle of TB is long, and it takes 1-2 years for its complete cure, which brings about a heavy psychological and economic burden to patients and their families[3].
TB is a chronic respiratory infectious disease that considerably jeopardizes human health, and there is no effective vaccine suitable for its prevention in the entire population. After diagnosis, most patients with TB often suffer from low self-esteem, fear, anxiety, and other psychological stresses owing to the contagious nature of the disease and fear of their own safety. Additionally, factors, such as adverse drug reactions, lack of knowledge about the disease, and recurrent illnesses often lead to decreased treatment adherence, thus affecting the effectiveness of treatment. Therefore, effective nursing interventions during treatment to improve patients’ knowledge of the disease and compliance with treatment and to ensure the safety of medication play an important role in improving the therapeutic effect.
Drug-resistant (DR-)TB refers to the resistance of M. TB to anti-TB drugs in patients infected with TB, which can be caused by insufficient courses of treatment, irrational chemotherapy regimens, and poor patient adherence to treatment[4]. Countries with a large number of patients with TB are characterized by a high number of DR-TB cases. Currently, DR-TB can be categorized into four types according to the degree of drug resistance: (1) Mono-resistant; (2) Multi-resistant; (3) Multi-resistant; and (4) Extensively drug-resistant.
Currently, DR-TB, particularly multidrug resistant TB (MDR-TB), is showing a global epidemic trend. As per the World Health Organization global TB report, China is among 22 countries with a high burden of TB and among 27 countries with a high burden of DR-TB worldwide. In 2018, patients with MDR-TB in China accounted for 14% of the world’s population, ranking second[5]. DR-TB has become a serious public health concern and social problem owing to its long infection period, difficult diagnosis, long treatment cycle, and high treatment cost[6].
At present, the clinical treatment of patients with MDR-TB is based on drugs that can control further disease development. However, the severity of the disease in this group of patients, coupled with the long treatment time, high treatment cost, and the increasing burden on the patient’s family, lead to a serious decline in the patient’s treatment adherence, thus affecting the clinical treatment effect and posing a threat to the patient’s quality of life and physical health[7]. As per the 2018 World Health Organization global TB report, the treatment success rate of patients with DR-TB is only 55% globally[8]. At present, the treatment of DR-TB mainly includes anti-TB drug therapy. The use of anti-TB drugs not only saves the lives of patients with DR-TB but also plays a key role in stopping the spread of the TB epidemic.
DR-TB shows a trend of high incidence, low detection rates, low treatment rates, and low cure rates. The rational use of anti-TB drugs and interruption of the transmission of infectious sources are fundamental to the eradication of DR-TB. China lacks effective isolation measures for DR-TB. Simultaneously, the long period of DR-TB treatment, the numerous adverse reactions of anti-TB drugs, and the lack of patient knowledge of related diseases have led to difficulties in treatment and care management[9]. The principle of anti-TB treatment is that patients with DR-TB must complete the entire course of treatment in strict accordance with the treatment plan and strictly follow the doctor’s instructions to take drugs regularly.
The non-compliance of patients with DR-TB during the course of treatment can easily lead to multidrug resistance. If patients strictly follow the doctor’s instructions for the entire course of regular medication, it can significantly increase the cure rate and improve their quality of life[10]. In addition, when patients with TB have low adherence to medication, it is easy to develop tuberculous meningitis with disease progression, which directly affects the long-term therapeutic effect and makes it difficult to effectively guarantee quality of life.
Currently, specialized care for patients with DR-TB is in the initial stage, with narrow coverage and a low level of care. This is an important reason for the low treatment compliance, poor self-management ability, and ineffective anti-TB treatment of patients. Appropriate nursing models are particularly important for patient treatment. Therefore, to improve the treatment adherence of patients with DR-TB and enhance patient knowledge of the disease, this study included 114 patients with DR-TB admitted from January 2019 to January 2023 as the research subjects and explored the application effect after the implementation of detailed nursing management.
A total of 114 participants were included in this study, all of whom were patients with DR-TB treated in our hospital from January 2019 to January 2023. Among them, 57 patients were managed with conventional nursing care (control group), with male-to-female ratios of 47.37% (27/57) and 52.63% (30/57), respectively. The youngest patient was 35-years-old, while the oldest patient was 62-years-old with a mean of 45.15 ± 3.17 years. Another 57 patients were managed with detailed care (observation group); 43.86% (25/57) and 56.14% (32/57) were male and female, respectively. The patients were aged 37-64 years with a mean of 46.56 ± 3.23 years. There was no statistically significant difference in the baseline data of sex and average age between the two patient groups (P > 0.05).
The following were the inclusion criteria: (1) Patients aged ≥ 18 years; (2) Patients who met the diagnostic criteria for DR-TB meaning patients with TB resistant to one or more anti-TB drugs confirmed by in vitro drug susceptibility testing; (3) Patients receiving anti-TB drug treatment; (4) Patients positive for M. TB; (5) Patients with a clear, conscious, and normal verbal communication ability; and (6) Patients with informed consent to participate in the study and those who signed a letter of consent. All participants agreed to participate in the study and signed informed consent forms. The following were the exclusion criteria: (1) Severe diseases of the liver, kidney, heart, or other vital organs; (2) TB drug allergy or other infectious diseases; (3) Psychiatric diseases; (4) Immune system diseases; (5) Hematologic diseases; (6) Malignant tumors; and (7) Dementia.
The control group underwent routine nursing management, including health education, medication guidance, and condition monitoring. The observation group implemented detailed care management as follows. It emphasized the consideration of the patient’s overall health status in nursing practice, including physical, psychological, social, spiritual, and environmental aspects. This model holds that health is not only the absence of disease but the well-being of the whole body, mind, and society.
Multidisciplinary teamwork: Holistic care usually involves the collaboration of multidisciplinary teams, including doctors, nurses, psychologists, social workers, etc. They provide comprehensive health management to patients through teamwork. A detailed care management team is set up, and internal meetings of the team to comprehensively analyze the issues that might have occurred in the work and potential problems and to clarify the key points of future work were conducted. There was organized regular training for the members of the team, with lectures delivered by experts, to further improve the professionalism and skills of the healthcare personnel.
Individualized care: Care plans and practices were tailored to the unique needs and circumstances of each patient. Special attention was paid to the patient’s personal preferences, cultural background, and lifestyle.
Specific measures were as follows: (1) The guidance of medication was strengthened. Relevant literature was searched, and the medication of patients was explored to implement targeted measures, which helped reduce the development of drug resistance. The importance of medication compliance was explained to ensure that the patients understood the harm of an arbitrary increase or decrease in the dosage of drugs. Patients were informed of the methods, effects, and adverse reactions of taking drugs to encourage patients to adhere to the treatment. The direct supervision of taking drugs was strengthened; (2) Life management was strengthened. The patient’s food intake was monitored and recorded. The patient’s etiology was considered to develop the corresponding nursing measures and diet plan. Appropriate activities to increase the metabolism and action of nutrients, thereby increasing appetite, were encouraged. Unpleasant or painful events before meals were prevented. A good dining environment was provided. The patients were provided with high-calorie, high-vitamin, and spicy food, and other contraindications. The principle of eating fewer and more meals was followed. Patients were encouraged to change their bad habits, asked to rest more, asked to ensure adequate sleep, and were guided to perform appropriate functional exercises to enhance their body’s immune ability and promote recovery; and (3) Psychological intervention. Mutual trust between patients and staff were increased. Staff accompanied the patient and explained the condition, treatment, and examination to reassure them. Staff avoided contact with patients who were also experiencing anxiety. When communicating with patients, staff used concise sentences, spoke slowly, and repeated key words. Staff listened patiently when the patient was interested in trying to communicate. Staff encouraged the patient to talk and give praise when the patient tried and succeeded. Communication with patients was strengthened to grasp the basic situation and changes in mental state of patients, which was conducive to the timely identification of those suffering from bad psychology. For those with bad psychology, targeted psychological counseling was provided, and disease-related knowledge was explained to patients (including the causes and mechanisms of the disease), which can improve patient understanding of the disease, correct wrong cognition, and help improve treatment compliance. Measures to distract the patient and reduce anxiety (e.g., listening to music, relaxation exercises, massage) were utilized. Helping patients recognize anxiety, learn or solve problems, and do a good job in psychological care were implemented.
Assessment of medication adherence: The Morisky Medication Adherence Scale medication adherence questionnaire was used, which contained whether to forget to take the medication, whether to stop the medication on their own, and whether to stop the medication on their own. The total score was 10 points: 8-10 points indicated full adherence; 6-8 points indicated partial adherence; and < 6 points indicated nonadherence. The total adherence rate was calculated using the following formula: Total adherence rate = (full adherence + partial adherence)/number of cases × 100.
Disease cognition assessment: The disease cognition questionnaire was designed by our hospital, and the questionnaire survey was conducted on the disease cognition of the two groups of patients before and after the intervention, which primarily contained disease transmission pathways, prevention methods, treatment principles, and rational use of medication, with a total score of 100. The higher the score indicated the higher the patient’s cognition of the disease.
Medication safety: The occurrence of adverse reactions in patients caused by drugs was recorded and analyzed.
Nursing satisfaction: Nursing satisfaction was scored in terms of service attitude, communication skills, professional skills, nurse-patient relationship, and health education using a questionnaire on the day of patient discharge.
The recorded and collected data were analyzed using SPSS 27.0. Measured data were expressed as (mean ± standard deviation) using t-test. Count data were expressed as n (%) and analyzed using χ2 test. The difference was considered statistically significant at P < 0.05.
Table 1 shows that in the observation group there were 28 cases of complete medication compliance, 24 cases of partial compliance, and 4 cases of non-compliance after the intervention, with a total compliance rate of 92.00%. In the control group, there were 21 cases of complete medication compliance, 22 cases of partial compliance, and 14 cases of noncompliance, with a total compliance rate of 75.44%. Medication compliance of the observation group was significantly higher than that of the control group, indicating the significance of detailed nursing management in improving the medication dependence of patients with DR-TB.
| Indicator | Observation, n = 57 | Control, n = 57 | t/χ2 | P value |
| Full compliance | 28 (49.12) | 21 (36.84) | NA | NA |
| Partial compliance | 24 (42.11) | 22 (38.60) | NA | NA |
| Non-compliance | 5 (8.77) | 14 (24.56) | NA | NA |
| Total compliance rate | 52 (91.23) | 43 (75.44) | 5.116 | 0.024 |
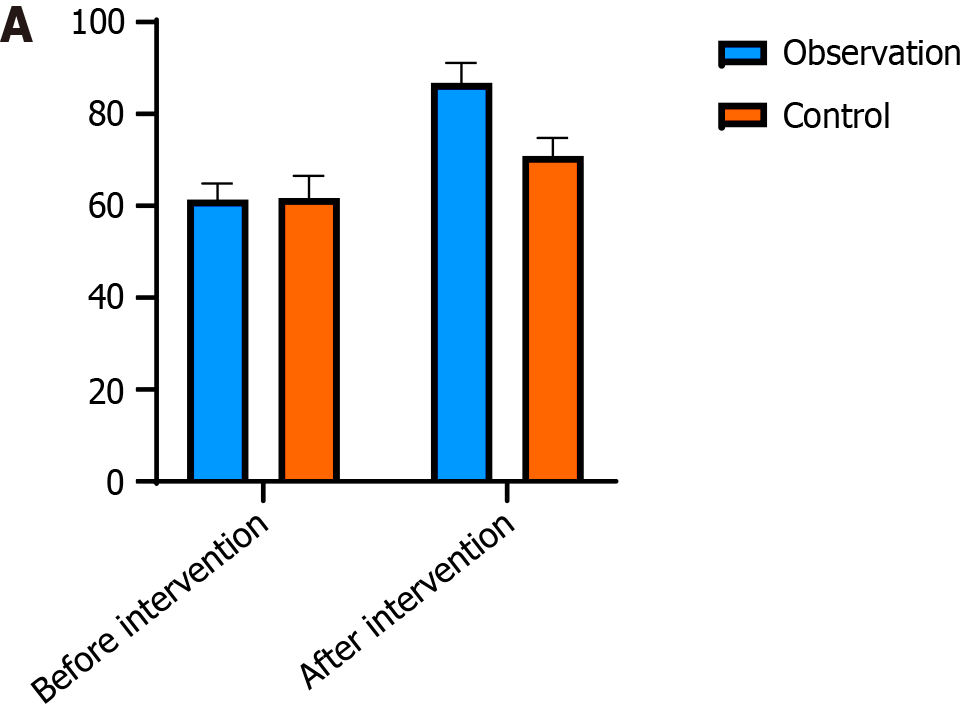
As shown in Table 2, the disease awareness scores of the two groups before intervention were 61.35 ± 3.54 and 61.74 ± 4.84, respectively, with no significant difference. After intervention, the disease cognition score of the observation group (86.82 ± 4.27) was significantly higher than that of the control group (70.86 ± 3.95) (P < 0.05), as shown in Figure 1.
| Indicators | Before intervention | After intervention |
| Observation, n = 57 | 61.35 ± 3.54 | 86.82 ± 4.27 |
| Control, n = 57 | 61.74 ± 4.84 | 70.86 ± 3.95 |
| t | 0.486 | 20.720 |
| P value | 0.628 | < 0.001 |
Table 3 presents the results of adverse reactions after medication in patients. The incidence rates of gastrointestinal reactions, arthralgias, hearing loss, electrolyte disorders, and liver and kidney function abnormalities in the observation group were 15.79%, 12.28%, 7.02%, 1.75%, and 5.26%, respectively, which were lower than those in the control group, which were 35.09%, 28.07%, 21.05%, 3.51%, and 17.54%, respectively. There were statistical differences between the two groups in terms of other adverse reactions, except electrolyte disturbances (P < 0.05).
| Indicators | Observation, n = 57 | Control, n = 57 | t/χ2 | P value |
| Gastrointestinal reaction | 9 (15.79) | 20 (35.09) | 5.596 | 0.018 |
| Joint swelling and pain | 7 (12.28) | 16 (28.07) | 4.412 | 0.036 |
| Hearing loss | 4 (7.02) | 12 (21.05) | 4.653 | 0.031 |
| Electrolyte disturbance | 1 (1.75) | 2 (3.51) | 0.422 | 0.516 |
| Liver and kidney dysfunction | 3 (5.26) | 10 (17.54) | 4.254 | 0.039 |
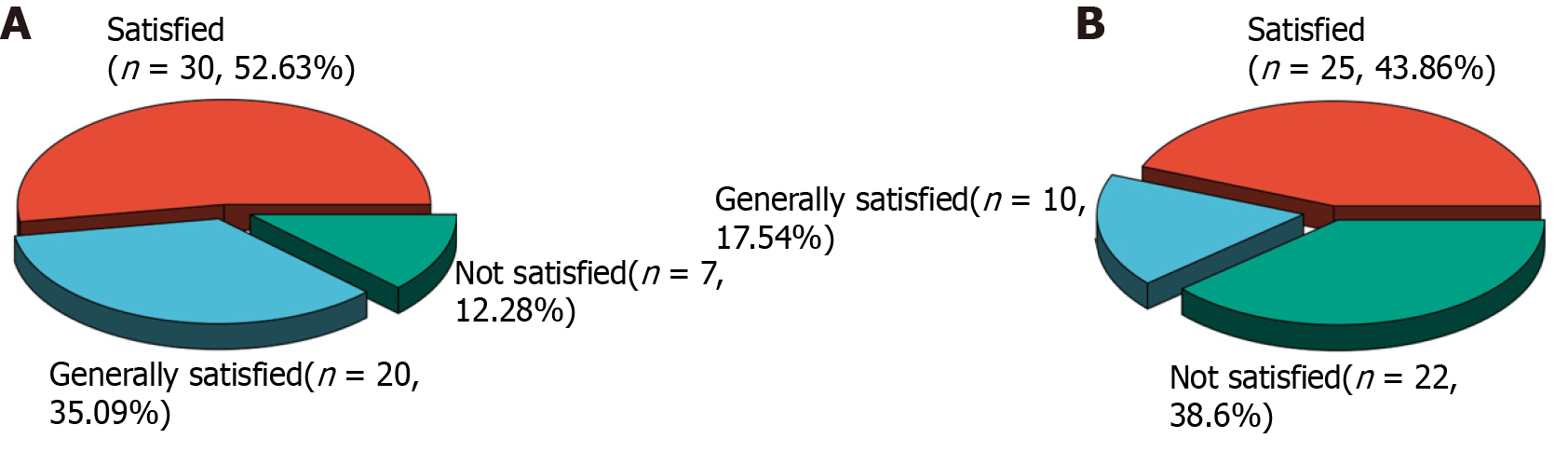
Table 4 depicts the results of patient satisfaction with nursing in each group. In the observation group, 30 patients were satisfied, 20 patients were almost satisfied, and 7 patients were not satisfied, with a satisfaction rate of 87.72%. In the control group, 25 patients were satisfied, 10 patients were almost satisfied, and 22 patients were not satisfied, with a satisfaction rate of 61.40%. The nursing satisfaction of the study group was 26.32% higher than that of the control group, as shown in Figure 2.
| Indicators | Observation, n = 57 | Control, n = 57 | t/χ2 | P value |
| Satisfied | 30 (52.63) | 25 (43.86) | NA | NA |
| Generally satisfied | 20 (35.09) | 10 (17.54) | NA | NA |
| Not satisfied | 7 (12.28) | 22 (38.60) | NA | NA |
| Total satisfaction | 50 (87.72) | 35 (61.40) | 10.406 | 0.001 |
TB is a chronic pulmonary infectious disease caused by M. TB infection and is one of the three major infectious diseases under global control. Therefore, the prevention and control of TB is not optimistic. The relative prevalence of TB is higher than that of other job groups, such as medical staff protection knowledge and behavior is insufficient, it is more likely to be infected by TB patients in the process of diagnosis and treatment. TB is primarily transmitted through the respiratory tract in the form of aerosol droplets. Early detection, diagnosis, and complete, appropriate, and regular treatment are the most important measures for curing TB[11]. Without timely and effective treatment, further disease progression may lead to lung failure, jeopardizing the patient’s life.
In DR-TB, M. TB infection in the patient has been confirmed to be resistant to one or more anti-TB drugs by in vitro drug susceptibility testing[12]. Global prevention and control are increasing because of the unregulated treatment of TB. Adverse consequences, such as treatment failure, disease recurrence, and the development of DR-TB, have seriously affected the physical and mental health of people. DR-TB, as a type of TB, has a significantly longer treatment time than TB and a significantly lower cure rate than TB[13]. DR-TB will not only affect the health of the patients but will also increase the risk of the spread of drug-resistant bacteria and the scope and intensity of the spread of the disease. This in turn will have an impact on social stability and sustainable economic development.
Some studies have shown that the cause of DR-TB is mainly irregular and intermittent drug use. With an increase in population mobility, the number of DR-TB cases is gradually increasing. At this stage, the widespread prevalence of DR-TB has brought great challenges to existing TB prevention and control[13]. Under the current routine care management model of DR-TB, the level of diagnosis and care for patients with DR-TB and the ability of healthcare professionals to configure equipment is lacking to varying degrees. The health education of patients is only at the level of general knowledge and lacks personalized guidance[14]. Detailed nursing management can fully mobilize the enthusiasm of patients with DR-TB for treatment, alleviate their psychological problems, improve their self-management ability and quality of life, and improve their prognoses.
Medication adherence is the degree of regular treatment of the disease by the patient as prescribed by the doctor, including consistency of medication, diet, lifestyle, and other behaviors according to the doctor’s instructions[15]. It is closely related to the type and dosage of the drug, adverse drug reactions, and knowledge of the disease[16]. Patients with low cognitive levels do not have sufficient knowledge about DR-TB and may even have misconceptions. In contrast, patients with a high level of cognition have a deeper understanding of the causes, treatment, care, rehabilitation, and medication of DR-TB and are well prepared for their possible effects, thus responding to the treatment in a more positive way. Therefore, the medical staff should be more proactive in providing comprehensive health education while actively treating diseases.
Detailed nursing management enables patients to acquire more disease-related knowledge, improves their self-care abilities, and increases their awareness of medication compliance. Patients consciously changed their bad behavioral habits and improved their medication compliance. The results of this study showed that the medication adherence of patients who implemented detailed nursing management increased by 15.79% (P < 0.05) compared with that of the control group. Detailed nursing management is an extension of clinical medical care work, an important measure of hospital humanized services, and its service level is related to the image and reputation of the department and even the medical institute. Therefore, specialized nurses need to have rich professional knowledge, skilled operating skills, and certain psychological knowledge and be good at communicating with patients and their families.
Establishing a good communication mechanism between doctors, nurses, and patients effectively strengthens unity and cooperation among doctors and nurses. Medical and nursing teams work together to help patients overcome the disease, supervise them to strictly implement the treatment principles of TB, and improve their cognitive levels. Through psychological guidance, panic about the intractability of the disease is alleviated, and motivation for treatment is improved. In recent years, with the transformation of the physiological–psychological–social medical model, humanistic care has become an important part of holistic nursing, primarily by improving nurses’ awareness of humanistic care. Through a series of detailed nursing service behaviors, the patient’s physical and mental comfort improved to the greatest extent, and the self-confidence of the patient to overcome the disease was improved so that the patient could actively cooperate with clinical treatment and nursing and promote the recovery of the disease.
The therapeutic effect on patients with DR-TB is closely related to the individualized treatment plan formulated by the medical staff[17]. Additionally, active cooperation among patients is necessary[18]. Patients’ adherence to medication is generally poor under the conventional care model, which may be attributed to their poor knowledge of the risk of the disease. This suggests that the development of medication adherence in patients with DR-TB should be emphasized during the treatment period, especially in terms of knowledge that is easily neglected by patients. Studies have shown that the higher the rate of patients’ knowledge of DR-TB, the more conducive it is to disease recovery.
Clinical healthcare workers should pay more attention to the role of health education[19]. It is crucial to impart relev
The incidence of drug-induced gastrointestinal reactions, joint swelling and pain, hearing loss, electrolyte disorders, and liver and kidney function abnormalities were lower in the observation group than in the control group (P < 0.05). The total satisfaction with patient care in the study group was 26.32% higher than that in the control group (P < 0.05). This might be due to the detailed nursing management mode through the collaboration of doctors and nurses that helped patients master their knowledge of TB, treatment methods, and related precautions. In addition, the patients’ cognitive levels regarding disease prevention and treatment improved. Simultaneously, the patients’ psychological states improved, and they mastered knowledge related to the disease and treatment, which in turn improved treatment compliance and promoted the therapeutic effect. This led the patients to comply with the doctor’s instructions for medication and reduce the incidence of drug resistance and adverse reactions. Establishing a good communication mechanism with patients, gaining their trust, improving nursing satisfaction, and ensuring treatment effects have a positive significance in the treatment of patients with TB.
There were some limitations to this study. Only a portion of patients with DR-TB were selected for this study, and the sample size was only 114 cases, which is not conducive to the promotion and application in other regions and groups. Therefore, in future studies, the sample size should be further expanded, and multiple departments should be included for comprehensive analysis. Multicenter research can also be used to compare the differences between patients with DR-TB in different regions and different groups to better explore the intervention effect of detailed nursing management in patients with DR-TB to guide clinical practice.
The implementation of detailed nursing management can effectively improve medication compliance of patients with DR-TB, enhance patient knowledge of the disease, improve the safety of medication, and increase patient satisfaction with nursing care. While ensuring a therapeutic effect, detailed nursing management has a positive significance in the treatment of patients with pulmonary TB and is worth popularizing and applying in the clinic.
| 1. | Helfinstein S, Engl E, Thomas BE, Natarajan G, Prakash P, Jain M, Lavanya J, Jagadeesan M, Chang R, Mangono T, Kemp H, Mannan S, Dabas H, Charles GK, Sgaier SK. Understanding why at-risk population segments do not seek care for tuberculosis: a precision public health approach in South India. BMJ Glob Health. 2020;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Mantri AK, Meena P, Puri AS, Kumar A, Sachdeva S, Srivastava S, Arivarasan K, Varakanahali S. Comparison of Interferon-Gamma Release Assay and Tuberculin Skin Test for the Screening of Latent Tuberculosis in Inflammatory Bowel Disease Patients: Indian Scenario. Tuberc Res Treat. 2021;2021:6682840. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Feng PI, Horne DJ, Wortham JM, Katz DJ; CDC Tuberculosis Epidemiologic Studies Consortium. Trends in tuberculosis clinicians' adoption of short-course regimens for latent tuberculosis infection. J Clin Tuberc Other Mycobact Dis. 2023;33:100382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Pedersen OS, Holmgaard FB, Mikkelsen MKD, Lange C, Sotgiu G, Lillebaek T, Andersen AB, Wejse CM, Dahl VN. Global treatment outcomes of extensively drug-resistant tuberculosis in adults: A systematic review and meta-analysis. J Infect. 2023;87:177-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Guo H, An J, Li S, Ding B, Zhang Z, Shu W, Shang Y, Wang Y, Cheng K, Wang Y, Xue Z, Ren W, Pan J, Luo T, Pang Y. Transmission and resistome of extremely drug-resistant tuberculosis in Beijing, China: A retrospective population-based epidemiological study. J Infect Public Health. 2023;16:1193-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 6. | Diriba G, Alemu A, Yenew B, Tola HH, Gamtesa DF, Mollalign H, Eshetu K, Moga S, Abdella S, Tollera G, Kebede A, Dangisso MH. Epidemiology of extensively drug-resistant tuberculosis among patients with multidrug-resistant tuberculosis: A systematic review and meta-analysis. Int J Infect Dis. 2023;132:50-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Katran ZY, Bulut İ, Babalık A, Keren M, Tepetam FM, Mersin SS, Örçen C, Yakut T, Yavuz D. Drug hypersensitivity in drug-resistant tuberculosis. World Allergy Organ J. 2023;16:100778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Oyewusi L, Zeng C, Seung KJ, Mpinda S, Kunda M, Mitnick CD, Kanu M, Tamirat M, Makaka J, Mofolo M, Maime R, Maama L, Senyo N, Oguntoyinbo B, Mayombo L, Franke MF. Low body mass index as a predictor of sputum culture conversion and treatment outcomes among patients receiving treatment for multidrug-resistant tuberculosis in Lesotho. Glob Health Action. 2024;17:2305930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 9. | Murhula Kashongwe I, Mawete F, Anshambi N, Maingowa N, Aloni M, Lukaso L'osenga L, Kaswa M, Munogolo Kashongwe Z. Challenge to treat pre-extensively drug-resistant tuberculosis in a low-income country: A report of 12 cases. J Clin Tuberc Other Mycobact Dis. 2020;21:100192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Atif M, Mukhtar S, Sarwar S, Naseem M, Malik I, Mushtaq A. Drug resistance patterns, treatment outcomes and factors affecting unfavourable treatment outcomes among extensively drug resistant tuberculosis patients in Pakistan; a multicentre record review. Saudi Pharm J. 2022;30:462-469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Quiroz YL, Choqueza SO, Soriano-Moreno AN, Alave JL. Association between concern about COVID-19, social support and knowledge about tuberculosis with adherence to antituberculosis treatment in Lima, Perú. Biomedica. 2023;43:270-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 12. | Lange C, Dheda K, Chesov D, Mandalakas AM, Udwadia Z, Horsburgh CR Jr. Management of drug-resistant tuberculosis. Lancet. 2019;394:953-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 188] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 13. | Bruzadelli Paulino da Costa F, Zamboni Berra T, Garcia de Almeida Ballestero J, Bartholomay Oliveira P, Maria Pelissari D, Mathias Alves Y, Carlos Vieira Ramos A, Queiroz Rocha de Paiva J, Kehinde Ayandeyi Teibo T, Alexandre Arcêncio R. Treatment of drug-resistant tuberculosis in children and young adolescents in Brazil. J Clin Tuberc Other Mycobact Dis. 2023;33:100388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 14. | Reuter A, Furin J. Celebrating choice in the care of people living with drug-resistant tuberculosis. Lancet. 2022;400:1489-1491. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Liu D, Huang F, Li Y, Mao L, He W, Wu S, Xia H, He P, Zheng H, Zhou Y, Zhao B, Ou X, Song Y, Song Z, Mei L, Liu L, Zhang G, Wei Q, Zhao Y. Transmission characteristics in Tuberculosis by WGS: nationwide cross-sectional surveillance in China. Emerg Microbes Infect. 2024;13:2348505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 16. | Jiang W. Addressing the adherence challenge in tuberculosis treatment: more than digital technologies. Lancet Glob Health. 2023;11:e634-e635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 17. | Iribarren SJ, Milligan H, Chirico C, Goodwin K, Schnall R, Telles H, Iannizzotto A, Sanjurjo M, Lutz BR, Pike K, Rubinstein F, Rhodehamel M, Leon D, Keyes J, Demiris G. Patient-centered mobile tuberculosis treatment support tools (TB-TSTs) to improve treatment adherence: A pilot randomized controlled trial exploring feasibility, acceptability and refinement needs. Lancet Reg Health Am. 2022;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 18. | Miiro E, Olum R, Baluku JB. Clinical features, resistance patterns and treatment outcomes of drug-resistant extra-pulmonary tuberculosis: A scoping review. J Clin Tuberc Other Mycobact Dis. 2023;33:100390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 19. | Riquelme-Miralles D, Palazón-Bru A, Sepehri A, Gil-Guillén VF. A systematic review of non-pharmacological interventions to improve therapeutic adherence in tuberculosis. Heart Lung. 2019;48:452-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |