Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4180
Revised: May 21, 2024
Accepted: May 23, 2024
Published online: July 16, 2024
Processing time: 69 Days and 20.7 Hours
Rhinophyma, a late-stage subtype of rosacea, is characterized by excessive seba
To evaluate the clinical effectiveness and recurrence rates after treating severe rhinophyma with the five-blade scratcher.
This study retrospectively analyzed the clinical records of 28 patients with severe rhinophyma rosacea. The Global Flushing Severity Score (GFSS), Clinician Erythema Assessment (CEA), Rhinophyma Severity Index (RHISI), Glasgow Benefit Inventory (GBI), and satisfaction scores were used to assess the recovery of patients at 6 months and 5 years, with the recurrence rate calculated at 5 years postoperatively. In addition, the levels of pro-inflammatory factors (TNF-α, IL-1β, and IL-6) in the serum of patients before and after surgery were detected by ELISA.
The GFSS, CEA, and RHISI scores at 6 months and 5 years postoperatively were significantly lower than those preoperatively (P < 0.001 for both periods). Five-blade scratcher treatment greatly benefits patients as demon
The five-blade scratcher treatment demonstrates notable advantages, including simplicity, safety, efficacy, and cost-effectiveness, coupled with reduced bleeding, minimized scarring, lower recurrence rates, reduced the level of pro-inflammatory factors and improved patient satisfaction. Consequently, this therapeutic modality exhibits a viable option for individuals afflicted with severe rhinophyma.
Core Tip: Rhinophyma is known as a late-stage subtype of rosacea. This study aims to observe the clinical effectiveness and recurrence of severe rhinophyma with Xia’s surgical five-blade scratcher treatment. We assessed the Global Flushing Severity Score, Clinician Erythema Assessment, Rhinophyma Severity Index, Glasgow Benefit Inventory, and satisfaction and recurrence of Xia’s surgical five-blade scratcher treatment preoperatively and 6 months and 5 years postoperatively. Five-blade scratcher treatment was safe, effective, and economical, with less bleeding, less scar, low recurrence rates, and high patient satisfaction. It offers an alternative to conventional surgery for severe rhinophyma.
- Citation: Zheng YP, He XF, Zhang YF, Geng LX, Zhang HM, Wan H, He X. Five-blade scratcher for treating severe rhinophyma: A retrospective study. World J Clin Cases 2024; 12(20): 4180-4190
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4180.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4180
Rhinophyma, a chronic and progressive nasal disease, is characterized by benign skin thickening, surface irregularities, and telangiectasias with inflammatory infiltration, connective tissue hypertrophy, and sebaceous gland hyperplasia, causing a tumor-like growth of nasal tissues. Hypertrophic rhinophyma may cause nasal congestion and nocturnal apnea and affect the appearance of patients, resulting in functional, aesthetic, and psychosocial problems[1]. Chronic inflammation and fibrosis significantly influenced the development of rhinophyma, a condition whose precise etiology and pathogenesis remain elusive[2]. Additionally, Demodex folliculorum infection has attracted increasing attention from researchers. Histopathologic examination of rhinophyma has occasionally observed air follicle infection of Demodex. Furthermore, inflammation is increased in Demodex-infected rhinophyma, but the innate immune cells producing IL-4 and IL-13 are decreased[3]. Furthermore, Gether et al[4] revealed that rhinophyma occurred almost exclusively in males. Rhinophyma affects people aged 50–70 years in Caucasians and is very rare in African Americans and Asians[2].
The treatment goal of rhinophyma is to remove hypertrophic, hyperplastic tissue to restore normal contour, avoid scarring, and prevent nasal cancer development. No substantial evidence indicates rhinophyma as an independent risk factor for skin cancer, but basal cell carcinoma demonstrated an incidence of 3%–10% in rhinophymatous tissue[5]. Therefore, active early treatment is particularly important. The guidelines for rosacea published in the New England Journal in 2017[6] indicate a lack of rigorous randomized controlled trials for treating rhinophyma. The use of topical retinoids, oral doxycycline, oral tetracycline, or oral isotretinoin is recommended for treatment based on clinical expe
Our study retrospectively analyzed 28 patients aged 30–75 years in the outpatient or inpatient department of derma
Our study used a modified five-blade scratcher as the surgical instrument. The five-blade scratcher is composed of a handle, a grooved cutting edge, a fixing bolt, a fixing sleeve, and a blade. The bottommost of the five surgical blades is cast on the same plane to ensure that the tip of the blade is at the same level. The blade is fixed on the handle by screws, and the height of the blade exposed to the tool holder was changed by adjusting the screws.
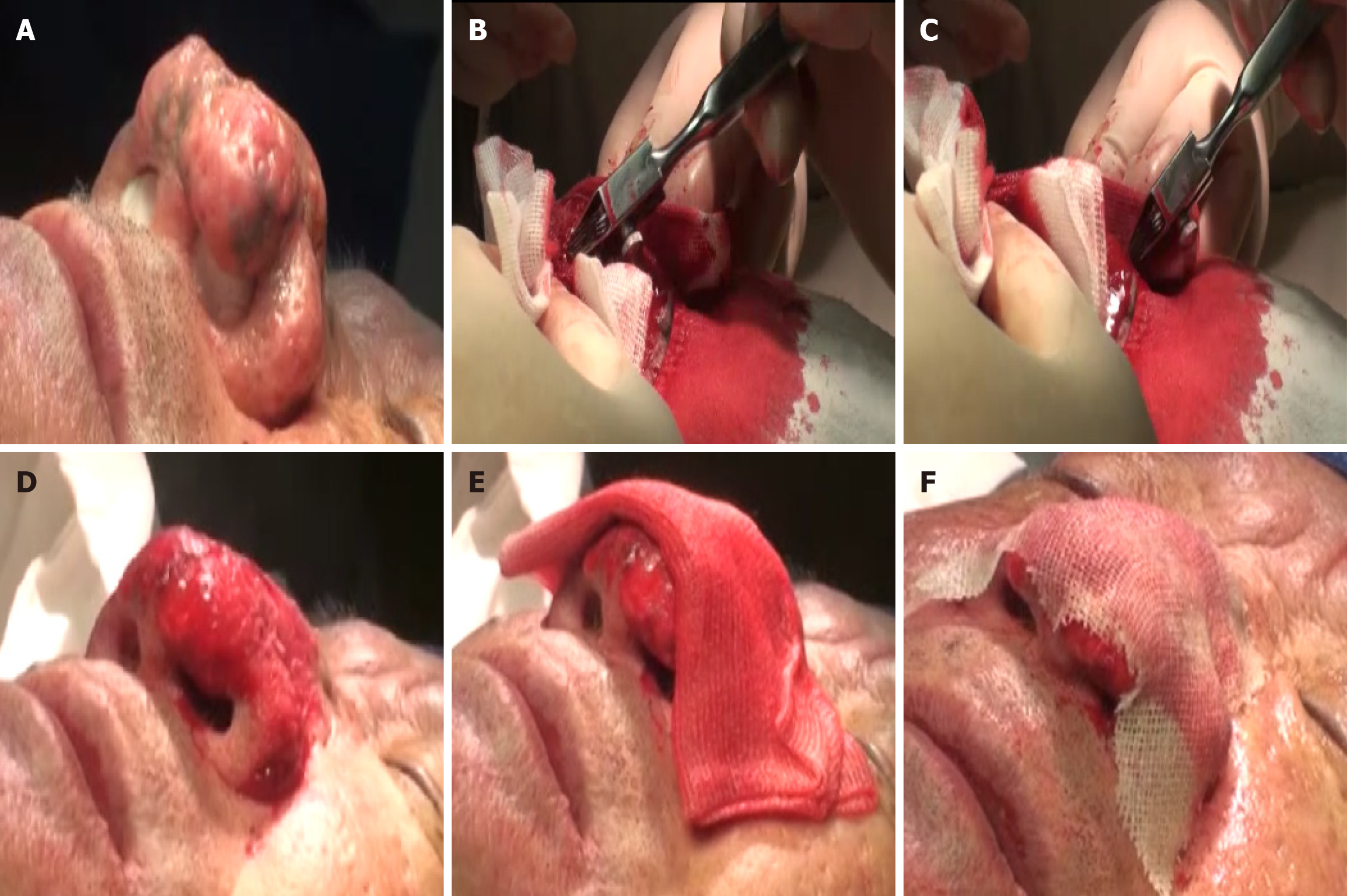
Sterile gauze is used to cover the nostrils to prevent blood from flowing into the nasal cavity, followed by routine iodophor disinfection of the skin area. Local anesthesia was administered with a 1% or 2% lidocaine solution containing epinephrine of 1:200000. We used a preoperative photograph of the patient to guide the determination of the patient’s nose contour according to the preoperative evaluation. The blade was then used to remove the hypertrophic nasal tip and nasal alar tissue, and electrocoagulation was utilized to assist resection and hemostasis. A five-blade scratcher was then used to decussate the lesions until a normal nasal profile appeared, and the final wound surface resembled that of a strawberry. Compression hemostasis was applied, followed by a cold compress placement with 5–6 pieces of gauze soaked in saline, and finally, the wound was covered with petrolatum gauze. Figure 1 shows the operative process.
Postoperative nursing consisted of a dressing change on the first postoperative day. The dressing was changed except for the petrolatum gauze, and this care was followed once a day for 5–7 days. Approximately 10 days postoperatively, the petrolatum gauze typically fell off by itself, revealing a new red and tender wound. The petrolatum gauze was removed the next day if there was more discharge, and daily dressing changes continued until the wound was dry. Postoperative wound pigmentation gradually appeared. This condition required no treatment, and a return to normal pigmentation generally occurred after 2–6 months.
The Global Flushing Severity Score (GFSS) was used to determine the severity of flushing in patients with rhinophyma[13]. The severity was recorded in a 0–10 score system, with higher numbers indicating more serious symptoms; GFSS of 0, 1–3, 4–6, 7–9, and 10 indicated no, mild, moderate, severe, and extremely severe flushing, respectively. GFSS scores were completed by telephone interviews with a non-medical staff at 6 months and 5 years postoperatively. The authors completed the statistical calculations.
We used the Clinician Erythema assessment (CEA) score to evaluate erythema improvement in patients[14]. CEA scores were recorded using a 5-point scale and defined as 0 (clearance), 1 (almost cleared), 2 (mild), 3 (moderate), and 4 (severe). We evaluated the improvement of CEA scores at 6 months and 5 years postoperatively compared with baseline. Two blinded dermatologists assessed the CEA score, and the average score was analyzed.
Wetzi proposed the Rhinophyma severity index (RHISI) for further assessment preoperatively and at 6 months and 5 years for rhinophyma[15]. The index measures rhinophyma digitally based on the degree of skin thickening, the presence of lobules and fissures, and the presence of strong asymmetry, cysts, or vessels. Three blinded, experienced dermatologists randomly graded the severity of rhinophyma based on standard photographs during the two follow-ups postoperatively as well as on a presurgical photograph.
Objective tools to assess patient satisfaction and quality of life are very important in facial plastic surgery. The Glasgow benefit inventory (GBI) is a specific scale proposed by Robinson et al[16], which is used to assess patient benefits postoperatively or other medical interventions. This scale is used to evaluate postoperative rhinophyma, which includes 18 items categorized into three dimensions: general, social, and physical health[11]. The questionnaire was completed by a telephone interview conducted by non-medical staff at 6 months and 5 years postoperatively. The interview process generally took 5–10 minutes. The authors completed statistical calculations.
Lazeri created a patient questionnaire to evaluate patient satisfaction[17]. This questionnaire is also widely used for postoperative assessment of patients with rhinophyma. Further, we conducted a telephone interview at 6 months and 5 years postoperatively for a questionnaire survey on patient satisfaction.
During the telephone interview 5 years postoperatively, the patient was asked for the presence of recurrence and reduction or aggravation compared with the preoperative period, as well as the severity of the recurrence (the collected data included recurrence within 5 years postoperatively).
To assess the concentrations of IL-6, IL-1β, and TNF-α in each group, the serum was collected and assayed using ELISA kits (Beyotime, China) according to the manufacturers’ instructions. The OD value was measured at the wavelength of 450 nm, and the concentrations of IL-6, IL-1β, and TNF-α were calculated based on a standard curve.
Statistical tests (the Wilcoxon 2-sample paired test in dependent groups) to evaluate differences in the scores of disease severity in the first, second, and third visits were performed following the data distribution analyses. A P-value of < 0.05 was considered to represent a statistically significant difference. IBM Statistical Package for the Social Sciences Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, United States) was used for data analysis.
Table 1 shows the demographic analysis. This study included 28 patients composed of 26 females and 2 males (male: female ratio of 13:1). The mean age of the patients was 52 years (range: 33–65 years), and the mean disease duration was 11.6 years (range: 5–20 years). No adverse events, such as postoperative bleeding, pain, or infection, occurred postoperatively.
| Patient | Sex | Age at presentation (years) | Duration of rhinophyma (years) |
| 1 | M | 53 | 12 |
| 2 | F | 47 | 8 |
| 3 | M | 50 | 10 |
| 4 | M | 54 | 8 |
| 5 | M | 46 | 6 |
| 6 | M | 56 | 14 |
| 7 | M | 58 | 15 |
| 8 | M | 65 | 20 |
| 9 | M | 55 | 15 |
| 10 | M | 60 | 20 |
| 11 | M | 53 | 16 |
| 12 | M | 62 | 18 |
| 13 | M | 65 | 15 |
| 14 | M | 48 | 8 |
| 15 | M | 39 | 5 |
| 16 | F | 52 | 10 |
| 17 | M | 49 | 8 |
| 18 | M | 45 | 6 |
| 19 | M | 50 | 8 |
| 20 | M | 43 | 6 |
| 21 | M | 38 | 6 |
| 22 | M | 47 | 8 |
| 23 | M | 50 | 10 |
| 24 | M | 33 | 10 |
| 25 | M | 63 | 15 |
| 26 | M | 60 | 20 |
| 27 | M | 57 | 13 |
| 28 | M | 58 | 15 |
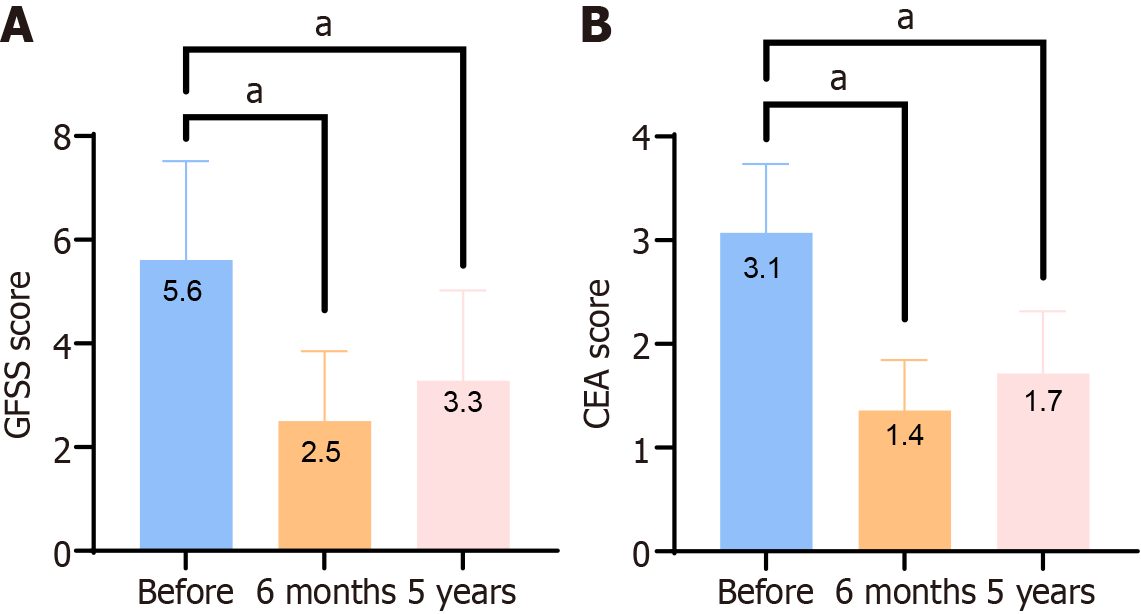
The clinical symptoms of all patients were significantly improved during postoperative recovery than preoperatively. The mean changes in GFSS and CEA scores were -3.1 and -1.7 during the 6-month follow-up session and -2.3 and -1.4 during the 5-year follow-up session, respectively, compared with the baseline (Figure 2). The differences were statistically significant (P < 0.001). These results indicate that the five-blade scratcher treatment improved the symptoms of flushing and erythema in patients with severe rhinophyma.
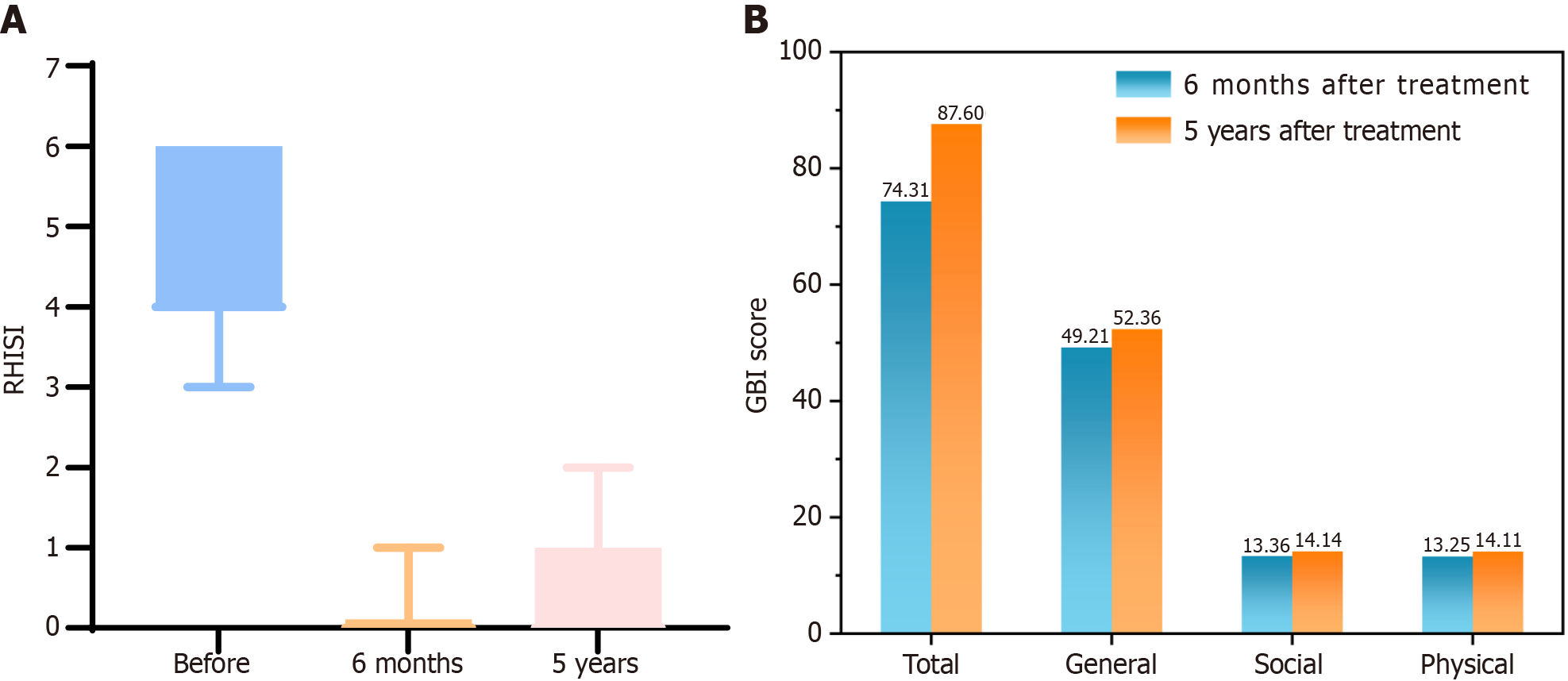
After the 6-month and 5-year follow-ups, 28 (100%) patients showed an improved RHISI. At 6 months postoperatively, RHISI scores were 100% improved in 25 patients. In particular, 3 patients demonstrated improved RHISI scores by 83.33%. RHISI scores were 100% improved in 18 patients at 5 years postoperatively. In particular, 3 patients improved their RHISI score by 83.33%, 2 patients by 75%, and the other 5 patients by 66.67% (Table 2). The median severity scores of the first visit [interquartile range (IQR): 2.00-4.00] were significantly higher than that of the second (IQR: 0-0.00) and third visits (IQR: 0-1.00; P < 0.001 and P < 0.001, respectively). A statistically significant difference was found between the median scores of the second and third visits (P = 0.002). The horizontal line in the boxes represents the median. The lower margin and the upper margin of the boxes indicate the greatest and least values, respectively (Figure 3A).
| Patient | RHISI (before treatment) | RHISI (6 months after treatment) | RHISI (5 years after treatment) | RHISI improvement (6 months, %) | RHISI improvement (5 years, %) |
| 1 | 6 | 0 | 1 | 100 | 83.33 |
| 2 | 3 | 0 | 0 | 100 | 100 |
| 3 | 4 | 0 | 0 | 100 | 100 |
| 4 | 4 | 0 | 1 | 100 | 75 |
| 5 | 3 | 0 | 0 | 100 | 100 |
| 6 | 4 | 0 | 0 | 100 | 100 |
| 7 | 6 | 0 | 0 | 100 | 100 |
| 8 | 6 | 1 | 2 | 83.33 | 66.67 |
| 9 | 4 | 0 | 0 | 100 | 100 |
| 10 | 6 | 0 | 2 | 100 | 66.67 |
| 11 | 4 | 0 | 0 | 100 | 100 |
| 12 | 6 | 1 | 2 | 83.33 | 66.67 |
| 13 | 6 | 0 | 0 | 100 | 100 |
| 14 | 4 | 0 | 1 | 100 | 75 |
| 15 | 6 | 0 | 0 | 100 | 100 |
| 16 | 3 | 0 | 0 | 100 | 100 |
| 17 | 4 | 0 | 0 | 100 | 100 |
| 18 | 3 | 0 | 0 | 100 | 100 |
| 19 | 4 | 0 | 0 | 100 | 100 |
| 20 | 3 | 0 | 1 | 100 | 66.67 |
| 21 | 4 | 0 | 0 | 100 | 100 |
| 22 | 4 | 0 | 0 | 100 | 100 |
| 23 | 6 | 0 | 0 | 100 | 100 |
| 24 | 6 | 0 | 1 | 100 | 83.33 |
| 25 | 6 | 0 | 0 | 100 | 100 |
| 26 | 6 | 0 | 1 | 100 | 83.33 |
| 27 | 6 | 1 | 2 | 83.33 | 66.67 |
| 28 | 6 | 0 | 0 | 100 | 100 |
The need for objective tools to assess patient satisfaction and quality of life cannot be overemphasized in facial plastic surgery. We combined the GBI score and satisfaction evaluation to assess the satisfaction of patients in all aspects postoperatively, as indicated in several published studies on the results of rhinophyma surgery. The total GBI results at 6 months and 5 years postoperatively were 74.31 and 87.60, respectively. Five-blade scratcher treatment can benefit patients, as demonstrated by the GBI outcome, and the benefit is more pronounced 5 years postoperatively. Patients reported that the questionnaire was easy to understand, with no difficulty in answering the questions (Figure 3B).
The patients were followed up for 5 years postoperatively. The patient’s medical records and treatment results were collected at 6 months and 5 years postoperatively, and the patient’s cognition was evaluated by questionnaires. The patient demonstrated a very high satisfaction score, and 89% and 93% of the patients were completely satisfied with the recovery at 6 months and 5 years, respectively, after rhinophyma surgery. The proportion of patients with good nasal appearance after 5 years was as high as 86% and that with positive self-image was as high as 89% at 6 months and 5 years postoperatively. The patient’s recommendation was 100%, indicating that the patient was very satisfied with the five-blade scratcher treatment for rhinophyma (Table 3).
| Question | 6 months after treatment (%) | 5 years after treatment (%) |
| Satisfaction | ||
| 0–3 | 0 (0) | 0 (0) |
| 4–6 | 0 (0) | 0 (0) |
| 7–9 | 3 (0.11) | 2 (0.07) |
| 10 | 25 (0.89) | 26 (0.93) |
| Effects maintained | ||
| Yes | 26 (0.93) | 24 (0.86) |
| Not sure | 2 (0.07) | 4 (0.14) |
| No | 0 (0) | 0 (0) |
| Self-impression | ||
| Excellent | 25 (0.89) | 25 (0.89) |
| Good | 2 (0.07) | 2 (0.07) |
| Sufficient | 1 (0.04) | 1 (0.04) |
| Disappointing | 0 (0) | 0 (0) |
| Back to social life | ||
| Too long | 0 (0) | 0 (0) |
| Long | 0 (0) | 0 (0) |
| Sufficient | 4 (0.14) | 4 (0.14) |
| Quick | 19 (0.68) | 19 (0.68) |
| Very quick | 5 (0.18) | 5 (0.18) |
| Recommend | ||
| Yes | 28 (1) | 28 (1) |
| Not sure | 0 (0) | 0 (0) |
| No | 0 (0) | 0 (0) |
A small number of patients (18%; 5/28) reported recurrence of rhinophyma postoperatively in our department. However, all patients with recurrent nasal tumors (100%; 5/5) reported that the appearance of the recurrent rhinophyma was less obvious than preoperatively. None of the patients considered that the recurrent rhinophyma after surgical treatment was comparable with or more severe than preoperatively (Table 4).
| Type | Percentage (%) |
| Recurrence of rhinophyma | 5/28 (18) |
| Improved postoperatively | 5/5 (100) |
| Same before/postoperatively | 0/5 (0) |
| Worse postoperatively | 0/5 (0) |
We selected three of the participants with recurrent rhinophyma and provided their photos (Figures 4 and 5).
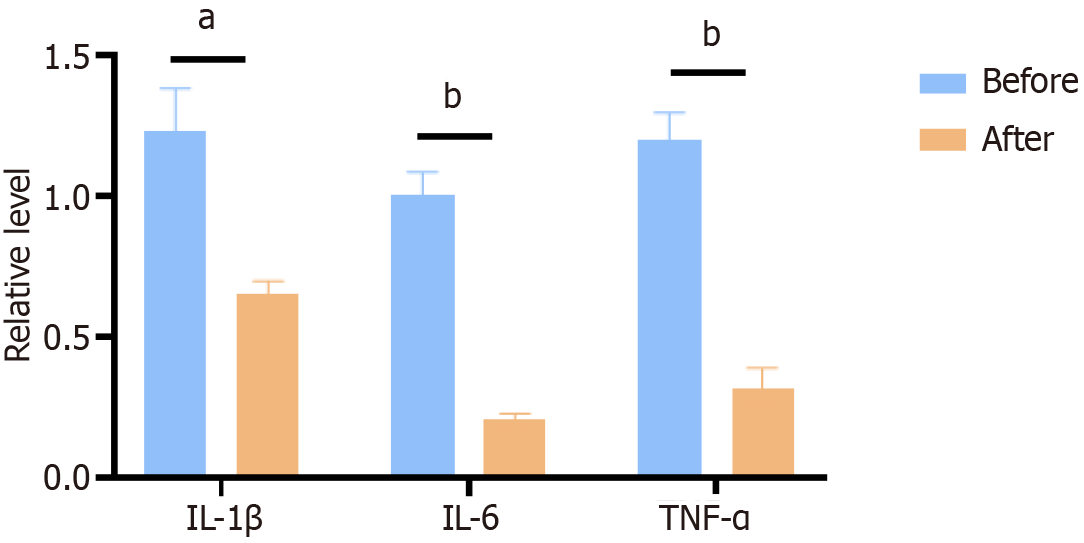
Next, we explored whether five-blade scratcher surgery affects the expression of pro-inflammatory factors in patients' serum. we compared inflammatory factors including IL-1β, IL-6, and TNF-α, between before and after surgery group. The results showed that the expression of TNF-α, IL-1β, and IL-6 were significantly decreased in the serum from after surgery group (Figure 6). Five-blade scratcher surgical treatment was able to alleviate inflammation levels in the patient's serum, indicating that Five-blade scratcher is an effective treatment for rhinophyma.
Rhinophyma is an advanced stage of rosacea. The nasal architecture destruction, airway obstruction development, and nasal aesthetic unit disfigurement cause a serious social psychological burden to patients and seriously affect the quality of life[2]. Drug treatment can only delay the early development of rhinophyma once rosacea enters the rhinophyma period, and the likelihood of spontaneous regression of the disease is low. Fibrotic lesions can only be treated surgically.
At present, surgical treatment has no gold standard, but the two steps of “excision” and “reconstruction” are usually the cornerstone of surgical treatment. Nasal neoplasm usually only invades the superficial dermis; thus, rhinophyma resection is classified according to the layer it is cut. Carbon dioxide laser, erbium YAG laser, grinding, and cryotherapy can be selected for light rhinophyma[9]. However, the risk of hypertrophic scar formation, insufficient pigmentation, postoperative erythema, and infection can occur in clinical practice[1,18]. Scalpel excision is the best choice for severe rhinophyma. It is not only a more cost-effective treatment but demonstrates relatively few postoperative complications[2]. At present, the predominantly used methods in clinical practice are full-thickness resection + flap/skin graft, cold blade/hot blade, or cosmetic subunit method[19]. Full-thickness resection is the removal of rhinophyma tissue to the whole dermis. This method completely removes the lesion site with a scalpel, and the wound is covered with a flap or skin graft after complete resection to achieve secondary healing. However, this method has some disadvantages because of the heterogeneity of transplantation, such as skin color and texture mismatch between the donor site and transplan
We aimed to explore a surgical method without scarring in severe rhinophyma; therefore, we pursued an alternative approach. The five-blade scratcher is a patented method for treating severe rhinophyma. Our previous studies only focused on describing the operative process, immediate postoperative recovery, and adverse reaction evaluation[23,24]. We did not systematically evaluate the long-term recurrence rate, and we aimed to follow up on recurrence, patient satisfaction, and quality of life for a long period after treatment. Therefore, we designed this study to evaluate the RHISI score, GBI score, patient satisfaction, and recurrence 6 months and 5 years postoperatively to assess the therapeutic effect of scratch surgery more systematically and comprehensively.
The scratching surgical method is a typical product of the combination of traditional Chinese medicine with a surgical treatment concept and modern western medicine surgical methods. This technique can be traced back to ancient cutting therapy, as the treatment of blood stasis syndrome. The criss-cross scratching method cuts off the dilated capillaries, removes the hyperplastic sebaceous glands, repairs the epidermal cells remaining in the hair follicles on the wound surface, and leaves no scar after healing. It is a major innovation in treating rhinophyma. The thickened tissue of rhinophyma is mainly composed of epidermis and superficial dermis. The middle and lower layers of the dermis, which is equivalent to extra hyperplastic tissue on the normal nose, attained no great damage. Therefore, in rhinophyma surgery, most of the hyperplastic tissue is first removed with an ordinary scalpel to make the nasal shape close to normal size. Criss-cross scratching follows, using the five-blade scratcher on the residual wound. Postoperatively, the middle and lower layers of the dermis, including sebaceous glands and the stratified squamous epithelium of hair follicles, remained intact. After scratching, numerous filiform, papillae-like structures remain on the wound surface. Hence, the surgical wound is gradually repaired, with epithelial healing rather than scar formation. We have developed several cautionary notes through continuous summarization of our experience, including (1) Before-and-after pictures of the nasal hyper
Our results reveal the feasibility of a five-blade scratcher for treating severe rhinophyma. This technique presents a viable alternative to traditional surgical approaches, providing potential benefits such as reduced trauma, improved prognoses, lower recurrence rates, and increased patient satisfaction. However, this study has limitations that should be addressed. First, the sample size is small, and subgroup analysis was not performed on patients of different ages or severities. Second, this is only a clinical study, and no experimental study confirmed that the surgical method improves rhino
| 1. | Kassirer SS, Gotkin RH, Sarnoff DS. Treatment of Rhinophyma With Fractional CO2 Laser Resurfacing in a Woman of Color: Case Report and Review of the Literature. J Drugs Dermatol. 2021;20:772-775. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Chauhan R, Loewenstein SN, Hassanein AH. Rhinophyma: Prevalence, Severity, Impact and Management. Clin Cosmet Investig Dermatol. 2020;13:537-551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Ricardo-Gonzalez RR, Kotas ME, O'Leary CE, Singh K, Damsky W, Liao C, Arouge E, Tenvooren I, Marquez DM, Schroeder AW, Cohen JN, Fassett MS, Lee J, Daniel SG, Bittinger K, Díaz RE, Fraser JS, Ali N, Ansel KM, Spitzer MH, Liang HE, Locksley RM. Innate type 2 immunity controls hair follicle commensalism by Demodex mites. Immunity. 2022;55:1891-1908.e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Gether L, Overgaard LK, Egeberg A, Thyssen JP. Incidence and prevalence of rosacea: a systematic review and meta-analysis. Br J Dermatol. 2018;179:282-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 134] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 5. | Fink C, Lackey J, Grande DJ. Rhinophyma: A Treatment Review. Dermatol Surg. 2018;44:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | van Zuuren EJ. Rosacea. N Engl J Med. 2017;377:1754-1764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 146] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 7. | Schaller M, Almeida LM, Bewley A, Cribier B, Dlova NC, Kautz G, Mannis M, Oon HH, Rajagopalan M, Steinhoff M, Thiboutot D, Troielli P, Webster G, Wu Y, van Zuuren E, Tan J. Rosacea treatment update: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol. 2017;176:465-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 8. | Payne WG, Ko F, Anspaugh S, Wheeler CK, Wright TE, Robson MC. Down-regulating causes of fibrosis with tamoxifen: a possible cellular/molecular approach to treat rhinophyma. Ann Plast Surg. 2006;56:301-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Dugourd PM, Guillot P, Beylot-Barry M, Cogrel O. Surgical treatment of rhinophyma: Retrospective monocentric study and literature review. Ann Dermatol Venereol. 2021;148:172-176. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Ramsdell WM. Two Alternative Approaches to "Treating Severe Rhinophyma: A Stepwise Approach". Dermatol Surg. 2023;49:208-209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Daoud M, Ullas G, Kumar R, Raghavan U. Rhinophyma: Combined Surgical Treatment and Quality of Life. Facial Plast Surg. 2021;37:122-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | el-Azhary RA, Roenigk RK, Wang TD. Spectrum of results after treatment of rhinophyma with the carbon dioxide laser. Mayo Clin Proc. 1991;66:899-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Tong Y, Luo W, Gao Y, Liu L, Tang Q, Wa Q. A randomized, controlled, split-face study of botulinum toxin and broadband light for the treatment of erythematotelangiectatic rosacea. Dermatol Ther. 2022;35:e15395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Suggs AK, Macri A, Richmond H, Munavalli G, Friedman PM. Treatment of Erythematotelangiectatic Rosacea With Pulsed-Dye Laser and Oxymetazoline 1.0% Cream: A Retrospective Study. Lasers Surg Med. 2020;52:38-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Wetzig T, Averbeck M, Simon JC, Kendler M. New rhinophyma severity index and mid-term results following shave excision of rhinophyma. Dermatology. 2013;227:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Robinson K, Gatehouse S, Browning GG. Measuring patient benefit from otorhinolaryngological surgery and therapy. Ann Otol Rhinol Laryngol. 1996;105:415-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 456] [Cited by in RCA: 479] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 17. | Lazzeri D, Larcher L, Huemer GM, Riml S, Grassetti L, Pantaloni M, Li Q, Zhang YX, Spinelli G, Agostini T. Surgical correction of rhinophyma: comparison of two methods in a 15-year-long experience. J Craniomaxillofac Surg. 2013;41:429-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Badawi A, Osman M, Kassab A. Novel Management of Rhinophyma by Patterned Ablative 2940nm Erbium:YAG Laser. Clin Cosmet Investig Dermatol. 2020;13:949-955. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Benyo S, Saadi RA, Walen S, Lighthall JG. A Systematic Review of Surgical Techniques for Management of Severe Rhinophyma. Craniomaxillofac Trauma Reconstr. 2021;14:299-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Seiverling EV, Neuhaus IM. Nare obstruction due to massive rhinophyma treated using the Shaw scalpel. Dermatol Surg. 2011;37:876-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Vural E, Royer MC, Kokoska MS. Sculpting resection of rhinophyma using the Shaw scalpel. Arch Facial Plast Surg. 2009;11:263-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Hassanein AH, Vyas RM, Erdmann-Sager J, Caterson EJ, Pribaz JJ. Management of Rhinophyma: Outcomes Study of the Subunit Method. J Craniofac Surg. 2017;28:e247-e250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Wang DM, He XF, He X, Zhang HM. A Surgical Management for Severe Rhinophyma With Five-Blade Scratcher. J Craniofac Surg. 2021;32:2821-2822. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Li W, He X, Chen W, Ding P, Zhang H. A Novel Surgical Approach for Rhinophyma: Experience From a Cohort of Thirty Patients. J Craniofac Surg. 2022;33:233-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |