Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4174
Revised: May 21, 2024
Accepted: May 23, 2024
Published online: July 16, 2024
Processing time: 98 Days and 19.6 Hours
Breast cancer is one of the most common malignant tumors in women worldwide and poses a severe threat to their health. Therefore, this study examined patients who underwent breast cancer surgery, analyzed hospitalization costs and struc
To study the CHS-DRG payment system’s impact on breast cancer surgery costs.
Using the CHS-DRG (version 1.1) grouping criteria, 4073 patients, who under
In terms of hospitalization expenses, patients in the CHS-DRG payment group had lower medical, nursing, and management expenses than those in the diag
The CHS-DRG system can help control and reduce unnecessary medical expenses by controlling medicine costs, medical consumable costs, and the length of hospital stay while ensuring medical safety.
Core Tip: Patients undergoing the radical resection of breast malignant tumors and included under the China Healthcare Security Diagnosis Related Groups payment system have to bear lower medical, nursing, and management costs after hospitalization than those who are not managed by the system. Medicine and consumables, consumables, medicines, medical, medical technology, administrative, and nursing expenses and length of stay have a significant impact on hospitalization expenses.
- Citation: Hu YH, Li AD. Cost analysis of radical resection of malignant breast tumors under the China Healthcare Security Diagnosis Related Groups payment system. World J Clin Cases 2024; 12(20): 4174-4179
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4174.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4174
Diagnosis-related groups (DRGs) are used as a strategy for effectively controlling the rise in medical costs, with the aim of balancing medical quality and costs[1]. The National Medical Insurance Administration’s “Notice on Issuing the Three-Year Action Plan for the Reform of DRG/DIP Payment Methods”[2,3] aims to improve the efficiency of medical insurance fund utilization and standardize medical services. Hence, some designated medical institutions in Beijing have begun to implement the China Healthcare Security Diagnosis Related Groups (CHS-DRG) payment system[4]. Real-world studies systematically collect and analyze real-world data generated by clinical care using evidence-based medicine methods[5]. Breast cancer is one of the most common malignant tumors in women worldwide and poses a severe threat to their health. Therefore, this study examined patients who underwent breast cancer surgery, analyzed hospitalization costs and structure, and explored the impact of CHS-DRG management on patient costs. It aimed to provide medical institutions with ways to reduce costs, optimize cost structures, reduce patient burden, and improve service efficiency.
This study used data from the Beijing Area Impatient Medical Service Performance platform and examined patients discharged from a hospital between January and December 2023. According to the CHS-DRG grouping criteria, 4073 patients who underwent radical resection of malignant breast tumors were categorized under JA29, representing this procedure. Among them, 1028 cases were in the CHS-DRG payment patient group, and the remaining 3045 cases were in the control group and not included in the CHS-DRG payment group. This study compared patient costs for radical resection of malignant breast tumors with the city’s average cost to obtain the relative number of various cost ratios, including hospitalization, medical, nursing, medical technology, and management cost ratios. Medicine and consumable cost ratios were used for data correction. Further, the impact of the CHS-DRG system on hospitalization costs and cost structures was studied through real-world research to provide a basis for cost control and process optimization for patients undergoing radical resection of malignant breast tumors.
In this study, continuous variables were presented in the form of mean ± standard deviation. Differences between the DRG payment and non-payment groups were related to age, length of hospital stay, total hospitalization expenses, medicines and consumable expenses, medical expenses, nursing expenses, medical technology expenses, and mana
In this study, the average age of the patients was 52.85 ± 11.60 years, and the average length of hospital stay was 4.86 ± 2.10 days. The hospitalization cost ratio for all patients was 0.97 ± 0.18, of which the medical, nursing, medical technology, management and medicine cost ratios were 0.73 ± 0.14, 0.64 ± 0.22, 0.59 ± 0.22, 0.74 ± 0.55, and 1.57 ± 0.47, respectively. The medical consumables cost ratio was 1.28 ± 0.36.
As shown in Table 1, patients in the DRG payment group were older than those in the DRG non-payment group (53.50 ± 12.54 vs 52.63 ± 11.26, P < 0.05). There was no statistical difference in the length of hospital stay between the patients in the DRG payment and non-payment groups (4.77 ± 2.05 vs 4.89 ± 2.12, P > 0.05).
| Variable | Overall | DRG payment group | DRG non-payment group | P value |
| Age (year) | 52.85 ± 11.60 | 53.50 ± 12.54 | 52.63 ± 11.26 | 0.0484 |
| Length of hospital stay | 4.86 ± 2.10 | 4.77 ± 2.05 | 4.89 ± 2.12 | 0.1032 |
| Hospitalization expense ratio | 0.97 ± 0.18 | 0.97 ± 0.19 | 0.98 ± 0.18 | 0.1574 |
| Medical expense ratio | 0.73 ± 0.14 | 0.72 ± 0.12 | 0.73 ± 0.14 | 0.0044 |
| Nursing expense ratio | 0.64 ± 0.22 | 0.63 ± 0.20 | 0.65 ± 0.23 | 0.0419 |
| Medical technology expense ratio | 0.59 ± 0.22 | 0.60 ± 0.22 | 0.59 ± 0.22 | 0.2879 |
| Management expense ratio | 0.74 ± 0.55 | 0.70 ± 0.24 | 0.75 ± 0.62 | 0.0001 |
| Medicine expense ratio | 1.57 ± 0.47 | 1.56 ± 0.52 | 1.57 ± 0.45 | 0.8147 |
| Medical consumables expense ratio | 1.28 ± 0.36 | 1.27 ± 0.36 | 1.29 ± 0.35 | 0.137 |
In terms of hospitalization expenses, the medical expenses (0.72 ± 0.12 vs 0.73 ± 0.14, P < 0.05), nursing expenses (0.63 ± 0.20 vs 0.65 ± 0.23, P < 0.05) and administrative expenses (0.70 ± 0.24 vs 0.75 ± 0.62, P < 0.05) were lower for patients in the DRG payment group compared with those in the non-payment group. There was no statistical difference in the total hospitalization expenses (0.97 ± 0.19 vs 0.98 ± 0.18, P > 0.05), medical technology expenses (0.60 ± 0.22 vs 0.59 ± 0.22, P > 0.05), cost of medicines (1.56 ± 0.51 vs 1.57 ± 0.45, P > 0.05) and consumable costs (1.27 ± 0.36 vs 1.29 ± 0.35, P > 0.05) between the DRG payment and non-payment groups, respectively.
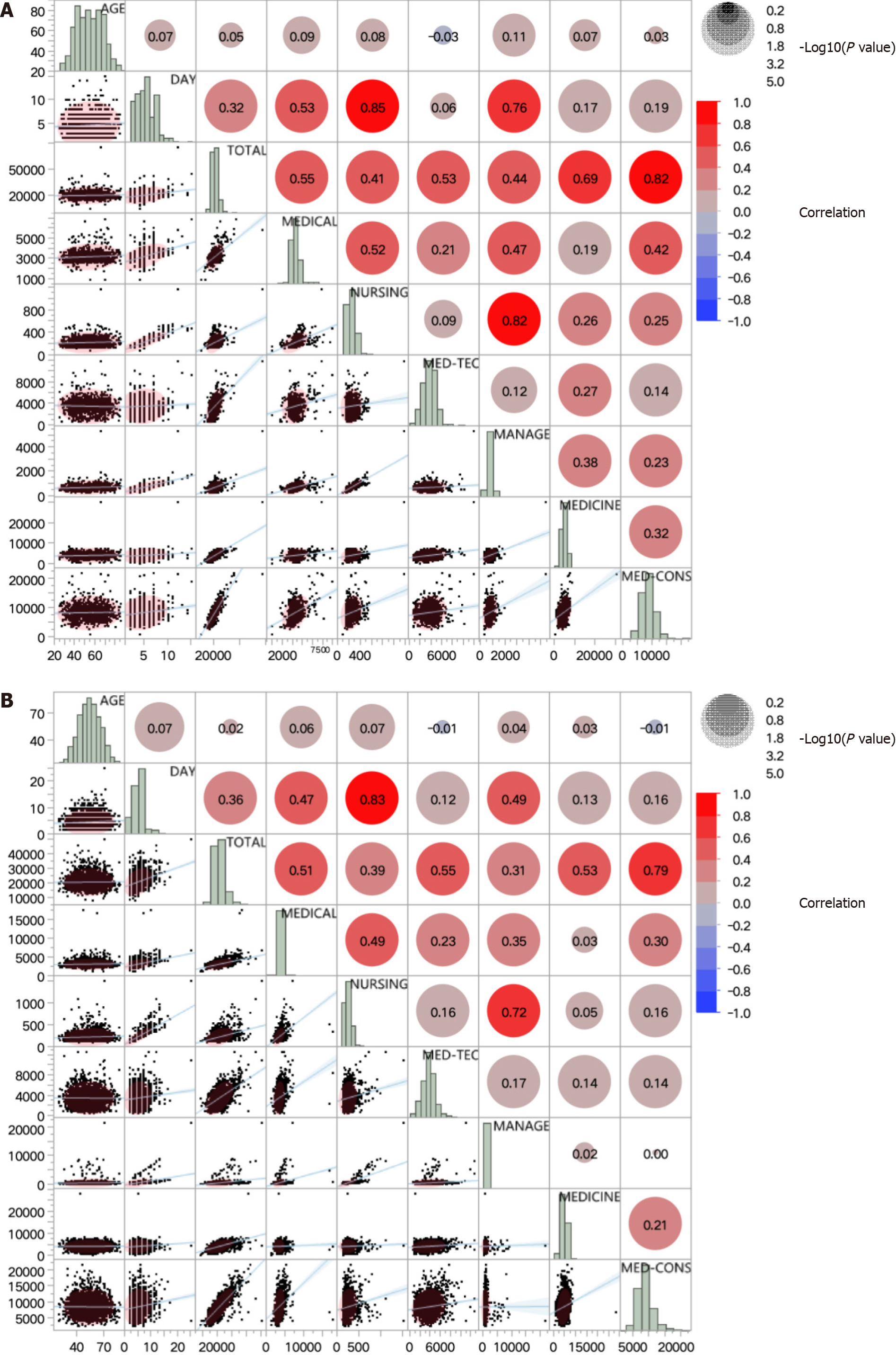
As shown in Figure 1A, for patients in the DRG payment group, the following factors affected the total hospitalization expenses in descending order of correlation: cost of medicines and medical consumables (r = 0.93, P < 0.05), cost of medical consumables (r = 0.82, P < 0.05), cost of medicines (r = 0.69, P < 0.05), medical expenses (r = 0.55, P < 0.05), medical technology expenses (r = 0.53, P < 0.05), management expenses (r = 0.44, P < 0.05), nursing costs (r = 0.41, P < 0.05), and length of hospital stay (r = 0.32, P < 0.05). There was no correlation between patient age and total hospitalization expenses. (r = 0.05, P < 0.05).
As shown in Figure 1B, for patients in the DRG non-payment group, the following factors affected the total hospitalization expenses in descending order of correlation: cost of medicines and medical consumables (r = 0.87, P < 0.05), cost of medical consumables (r = 0.79, P < 0.05), medical technology expenses (r = 0.55, P < 0.05), cost of medicines (r = 0.53, P < 0.05), medical expenses (r = 0.51, P < 0.05), nursing expenses (r = 0.39, P < 0.05), length of hospital stay (r = 0.36, P < 0.05), and administrative expenses (r = 0.31, P < 0.05). No correlation was observed for patient age (r = 0.02, P < 0.05).
In China, medical insurance payment reforms have been advancing steadily With the promotion of policies established by policy-making departments. For example, the purchase price of medicines is the same as the sales price; when implementing national centralized medicine procurement, the purchase price of medical consumables is the same as the sales price[6]. Simultaneously, the implementation of CHS-DRG requires medical institutions to enhance patient service quality, improve medical standards, optimize the internal resource allocation of medical institutions, promote medical resources to focus on key disciplines, and improve the operating efficiency of medical institutions. By analyzing the hospitalization costs of the patients undergoing radical resection for malignant breast tumors, we could explore the effects and influencing factors of the implementation of the CHS-DRG system. Identifying the focal points of management efforts is anticipated to enhance the hospitals’ internal management quality and operational efficiency. In general, reform policies have achieved positive results, thereby changing the profit model of medicines and medical consumables and promoting the enhancement of hospitals’ internal management. Implementation of the CHS-DRG system imposes greater demands on medical institutions; therefore, strengthening the internal management and optimizing the operational efficiency of hospitals is necessary.
The results indicate that including patients in the CHS-DRG payment system led significant advantages in terms of medical, nursing, and administrative expenses. The system has certain advantages in terms of controlling costs and reducing waste. Studies have shown that a DRG payment system can help promote standardized diagnosis and treat
Analysis of the composition of hospitalization costs for patients undergoing radical resection of malignant breast tumors showed that medicine and consumable costs were the main components, accounting for 21.58% and 40.78% of the total cost, respectively. Regardless of whether they were included in the CHS-DRG settlement, the total cost of hospitalization was closely related to the costs of medicines and medical consumables. Therefore, in cost management, reasonable control of medicine and consumable costs is crucial for reducing hospitalization costs of breast cancer surgery patients[8]. Medical institutions can establish a medicine and consumable cost assessment system for comparison with medical institutions of the same level to identify gaps and set them within a reasonable range. Additionally, the focus should be on medicines and medical consumables used in large quantities. By cooperating with peer institutions, they can jointly request the medical insurance management department to include these medicines and medical consumables in national or local centralized procurement to reduce unit prices, costs for medical institutions, and the cost consumption index, thereby improving medical efficiency.
The average length of hospital stay is an essential indicator for evaluating the operational efficiency of medical institutions. Shortening the length of hospital stay can help improve bed turnover rate, increase the efficiency of medical services, and alleviate the problems of medical treatment and hospitalization to a certain extent[9,10]. However, the average length of hospital stay cannot be reduced indefinitely. When service efficiency reaches a plateau, the blind pursuit of reducing the length of hospital stay may lead to doctors mismanaging or rejecting complex cases, adversely affecting patient care, departmental discipline, and hospital public welfare[10]. This study showed that the average length of hospital stay of the CHS-DRG group was slightly lower than that of the non-CHS-DRG group; both groups had shorter stays than the city’s average of 7.22 days, indicating that the hospital is a key player in managing the length of hospital stay. Leading specialties have shown stability or even improvement in controlling the average length of hospital stay, which helps improve the quality of medical services and ensure medical safety[11]. Although the CHS-DRG system cannot continuously reduce the average length of hospital stay, the management model and methods of leading specia
The CHS-DRG payment system can help control and reduce unnecessary medical expenses and achieve dual control over the quality and cost of medical services. This can be achieved by guiding medical institutions to actively change their management methods, focusing on cost-effectiveness, strengthening hospital refined management, controlling the cost of drugs and medical consumables through effective management methods and evaluation systems, and reasonably controlling the length of hospital stay while ensuring medical safety.
| 1. | Liu X, Liu F, Wang L, Wu M, Yang L, Wei L. Performance evaluation of medical service for breast cancer patients based on diagnosis related groups. BMC Health Serv Res. 2021;21:496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | National Healthcare Security Administration. Notice on issuing a list of national pilot cities for group payment based on disease diagnosis (YiBao Fa [2019] No. 34). Jun 5, 2019. [cited 24 March 2024]. Available from: http://www.nhsa.gov.cn/art/2019/6/5/art_37_1362.html. |
| 3. | National Healthcare Security Administration. Notice on issuing the three-year action plan for DRG/DIP payment method reform (YiBao Fa [2021] No. 48). Nov 26, 2021. [cited 24 March 2024]. Available from: http://www.nhsa.gov.cn/art/2021/11/26/art_104_7413.html. |
| 4. | Beijing Healthcare Security Administration. Notice on Issuing the Management Measures for Excluding Payment for CHS-DRG Paid New Drugs and Technologies (Trial Implementation) (Jing YiBao Zhongxin Fa [2022] No. 30). Jul 13, 2022. [cited 24 March 2024]. Available from: https://ybj.beijing.gov.cn/tzgg2022/202207/t20220713_2798069.html. |
| 5. | Makady A, de Boer A, Hillege H, Klungel O, Goettsch W; (on behalf of GetReal Work Package 1). What Is Real-World Data? A Review of Definitions Based on Literature and Stakeholder Interviews. Value Health. 2017;20:858-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 205] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 6. | Hu YH, Yu F, Li AD. Influence of Comprehensive Reform of Medical Consumption Linkage on Inpatient Cost of Cancer Patients from Perspective of DRG. Jiefangjun Yiyuan Guanli Zazhi. 2020;27:555-558, 579. [DOI] [Full Text] |
| 7. | Lei SY, Zheng RS, Zhang SW, Wang SM, Chen R, Sun KX, Zeng HM, Zhou JC, Wei WQ. Global patterns of breast cancer incidence and mortality: A population-based analysis of tumor registry data 2000-2020. Aizheng. 2022;41:324-335. |
| 8. | Li WJ, Xu XF, Tian LQ, Gao C. Analysis on Hospitalization Expenses and Its Influencing Factors of Breast Cancer Patients Based on DRG. Weisheng Jingji Yanjiu. 2021;38:76-79. |
| 9. | Yuan L, Li L, Qian ZX, Chen XY, Pan LL, Wang QH. Interrupted time series analysis for impacts of day surgery on average days of stay. Zhonghua Yiyuan Guanli Zazhi. 2018;34:805-809. [DOI] [Full Text] |
| 10. | Yuan L, Chen ZH, Huang GW, Pan LL, Wang QH. Practice and evaluation of accurate formulation of the goal of average length of stay in clinical department based on DRG. Zhongguo Yiyuan Guanli. 2021;41:34-38. |
| 11. | Liu JD, Yao M, Shen Y, Yao JB, Ye ZH. Research of Setting the Standardized Average Length of Stay Objectives for Specialties Based on DRG. Zhongguo Yiyuan Guanli. 2022;42:48-50. |