Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4082
Revised: May 14, 2024
Accepted: June 3, 2024
Published online: July 16, 2024
Processing time: 113 Days and 18.4 Hours
Prostate cancer (PC) is one of the most common malignant tumors in men, and bone metastasis is one of its common complications, which seriously affects the quality of life and prognosis of patients.
To investigate the diagnostic value of technetium-99m-methylene diphosphonate (99mTc-MDP) single photon emission computed tomography (SPECT)/CT imaging combined with the serum prostate-specific antigen (PSA)/free PSA ratio for PC bone metastasis (PCBM).
One hundred patients with PC who visited the Hospital of Chengdu University of Traditional Chinese Medicine from January 2020 to January 2022 were recruited as the experimental (Exp) group, while 30 patients with benign prostatic lesions (BPLs) were recruited as the control (Ctrl) group. All patients underwent 99mTc-MDP SPECT/CT imaging and serum PSA/fPSA testing. The SPECT/CT imaging results and serum PSA/fPSA ratios of patients were analyzed to evaluate their diagnostic values for PCBM.
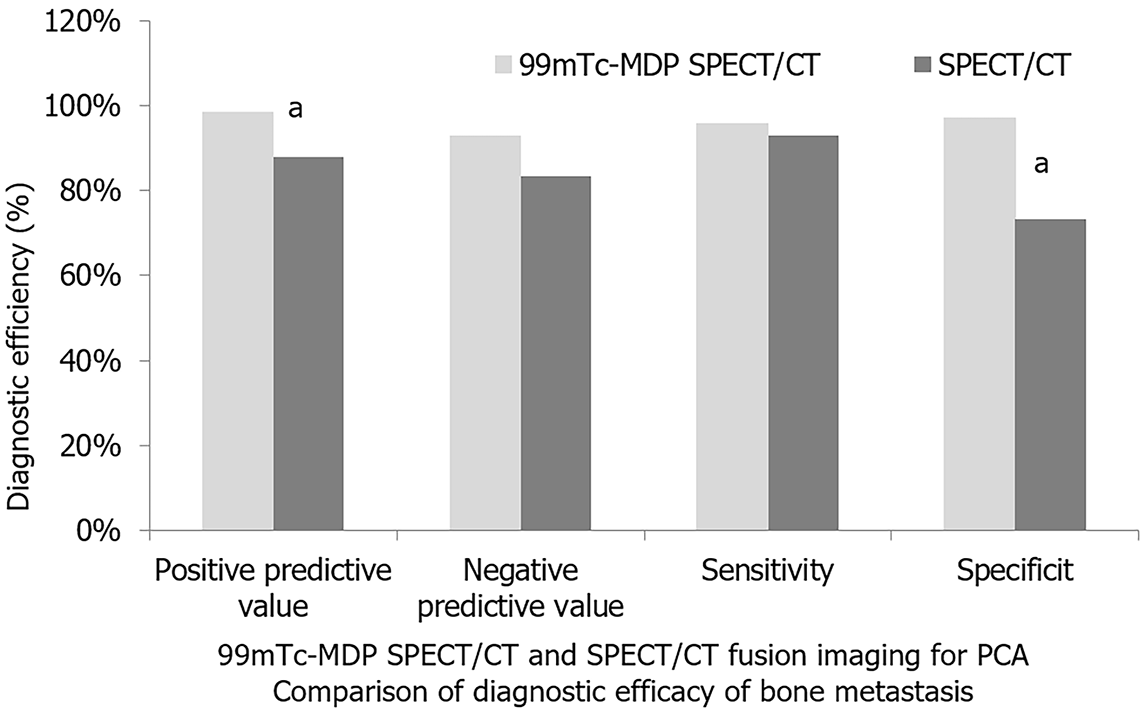
The difference in general information of the patients was not obvious, showing comparability. The two methods showed no visible differences in negative predictive value and sensitivity for patients with PCBM, but had great differences in positive predictive value and specificity (P < 0.05). The PSA/fPSA ratio of patients with PC in the Exp group was lower than those with BPLs, and patients with PCBM had a much lower PSA/fPSA ratio than those without PC (P < 0.05). The results confirmed that the combined use of 99mTc-MDP SPECT/CT imaging and serum PSA/fPSA ratio achieved a detection rate of 95% for PCBM.
The combination of 99mTc-MDP SPECT/CT and PSA/fPSA ratio is accurate and reliable for the diagnosis of PCBM, which provides an important reference for clinical practice.
Core Tip: This work investigated the diagnostic value of technetium-99m-methylene diphosphonate (99mTc-MDP) single photon emission computed tomography (SPECT)/ CT imaging combined with the serum prostate-specific antigen (PSA)/free PSA ratio for detecting bone metastasis in prostate cancer (PC). Compared to individual methods, the combination of SPECT/CT imaging and PSA/fPSA ratio demonstrated significantly higher positive predictive values and specificity. The PSA/fPSA ratio in PC bone metastasis (PCBM) patients was notably lower than in non-PCBM patients. The integrated approach achieved a 95% detection rate for PCBM, emphasizing its diagnostic efficacy.
- Citation: He J, Zhong YP, Zhang S. Technetium-99m-methylene diphosphonate single photon emission computed tomography/computed tomography combined with prostate-specific antigen/free prostate-specific antigen ratio for bone metastasis of prostate cancer. World J Clin Cases 2024; 12(20): 4082-4090
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4082.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4082
Prostate cancer (PC) is a malignant tumor that primarily occurs in the prostate tissue of males[1]. The prostate is an important component of the male reproductive system, located below the bladder and surrounding the urethra. PC typically grows slowly, and early-stage cases may not exhibit noticeable symptoms. However, as cancer cells proliferate, symptoms such as frequent urination, urgency, dysuria, and weak urine flow may manifest[2]. The diagnosis of PC is usually determined through prostate-specific antigen (PSA) testing and prostate biopsy. PC bone metastasis (PCBM) refers to the process in which PC cells spread from the primary site to the skeletal system[3]. This is one of the most common modes of metastasis in PC, with approximately 70% of PC patients experiencing bone metastasis in the advanced stages of the disease[4]. Bone metastasis can lead to symptoms such as osteoporosis, fractures, and pain, significantly impacting the quality of life for patients. The occurrence of bone metastasis is associated with the malignancy, course, and treatment modalities of PC. Treatment options for PC mainly include surgery, radiation therapy, chemotherapy, and hormone therapy. Surgery and radiation therapy are commonly used for early-stage PC, while chemotherapy and hormone therapy are more frequently employed for advanced cases.
Technetium-99m-methylene diphosphonate (99mTc-MDP) single photon emission computed tomography (SPECT)/CT imaging is a medical imaging technique used for detecting diseases and injuries in the skeletal system[5]. This technique combines two imaging modalities: SPECT and CT, enabling more accurate diagnostic results. In 99mTc-MDP SPECT/CT imaging, patients first receive an injection of the radiotracer 99mTc-MDP, which accumulates in the skeletal system. Subsequently, the patient undergoes a SPECT scan, which detects the distribution of the radiotracer. Finally, a CT scan is performed, providing detailed information about the bone structures. By combining the SPECT and CT images, physicians can more accurately diagnose diseases and injuries in the skeletal system, such as fractures, osteoporosis, tumors, and infections. Furthermore, 99mTc-MDP SPECT/CT imaging can also be used to assess treatment efficacy and monitor disease progression in the skeletal system[6,7].
The serum PSA/free PSA (fPSA) ratio refers to the ratio between PSA and fPSA detected in the blood[8]. This ratio is an indicator used to assess the risk of developing PC. In normal circumstances, the proportion of fPSA to total PSA is higher, while in PC patients, the proportion of fPSA is lower. Therefore, a lower serum PSA/fPSA ratio indicates a higher risk of PC. Generally, patients with a PSA/fPSA ratio below 0.15 require further PC screening to detect and treat PC at an early stage[9]. This indicator can assist physicians in more accurately diagnosing PC and help patients gain a better understanding of their health condition, enabling them to take appropriate preventive and treatment measures.
Currently, commonly used diagnostic methods for PCBM in clinical practice include bone scanning, CT, magnetic resonance imaging, and serum PSA/fPSA testing[10]. However, each of these methods has its advantages and limitations, and their individual applications are somewhat limited. Therefore, the aim of this work was to investigate the diagnostic value of 99mTc-MDP SPECT/CT imaging combined with serum PSA/fPSA ratio for PCBM.
The data of 100 patients with PC diagnosed by prostate biopsy or surgical pathology in Hospital of Chengdu University of Traditional Chinese Medicine (Chengdu, China), from January 2020 to January 2022, were retrospectively analyzed. The average age of the patients was 71.34 ± 5.76 years (range: 48-87 years), and the average body mass index was 23.5 ± 1.12 kg/m2 (range: 22-25 kg/m2). Patients with PC were the experimental group (Exp group). In addition, 30 patients with benign prostatic lesions (BPLs) were recruited as the control group (Ctrl group). All patients underwent 99mTc-MDP SPECT/CT imaging and serum PSA/fPSA detection. By analyzing the results of the two groups, the diagnostic value of SPECT/CT imaging results and serum PSA/fPSA ratio for PCBM was evaluated. Written informed consent was provided by all participants.
Inclusion criteria of Exp group were: (1) Patient age ≥ 18 years; (2) patients with no recent history of trauma or surgery; (3) patients who met the clinical diagnostic criteria of PC[11]; (4) patients who did not receive chemoradiotherapy drugs or hormone drugs; (5) patients and their families who provided written informed consent; (6) patients with complete clinical and imaging data; and (7) 99mTc-MDP SPECT/CT imaging and serum PSA/fPSA detection that could be accepted.
Exclusion criteria of Exp group were: (1) Patients with severe mental illness and cognitive impairment; (2) the presence of malignant tumors in other parts; (3) patients diagnosed with bone degenerative disease or chronic bone infection; (4) absolute contraindications to SPECT/CT imaging; (5) patients with severe cardiovascular, liver, and kidney dysfunction or other underlying diseases; (6) patients who received relevant treatment or diagnosis; and (7) unclear imaging images.
Prior to conducting the experiment, it was necessary to collect and organize the general information of all participating patients enrolled in this work. This information included but was not limited to, age, sex, occupation, work experience, educational level, marital status, family background, and income level. Data collection for this information was performed through methods such as questionnaire surveys, personal interviews, and medical records to ensure the accuracy and reliability of the research results.
99mTc-MDP imaging is a nuclear medicine technique used for the detection of diseases and injuries in the skeletal system[12]. This method involves the injection of a radiopharmaceutical agent called 99mTc-MDP (methylene diphosphonate), which is absorbed by the bones and emits gamma rays under the emission of the radioactive isotope, thereby forming an image. This imaging technique can detect conditions such as fractures, bone tumors, osteomyelitis, and arthritis in the skeletal system. Through this technique, physicians can conduct comprehensive examinations and evaluations of the skeletal system of the patient, aiding in the timely detection and treatment of skeletal system diseases, thereby improving treatment outcomes and quality of life.
SPECT/CT imaging fusion processing is a medical imaging technique that involves performing CT localization of a specific area followed by CT transmission scanning[13] with the parameters of 120 KeV, 200 mA/Layer, and 2 mm slice thickness. SPECT acquisition was automatically positioned, with a matrix of 64 × 64, continuous acquisition of 360°, and each dual-head rotating 180° with a step of 6° per frame for 15 s. The SPECT/CT images were reconstructed and fused using Astonish bone and Syntegra software. The resulting images were reviewed independently by two experienced nuclear medicine physicians in a blinded manner, and a consensus was reached. The positive diagnostic criteria for tumor bone metastasis generally involved the presence of multiple asymmetric radiotracer uptake abnormalities (two or more) in the whole-body bone imaging, excluding benign conditions such as surgery, fractures, and trauma, thereby indicating metastasis. If there were less than two lesions, the presence of osteoblastic or osteolytic changes at the site of radiotracer accumulation in CT scans and SPECT/CT fusion bone imaging, or the presence of lesions in locations such as the vertebral pedicle arch, can also be classified as bone metastasis. If there were evident changes in bone structure in the CT images but no apparent abnormal radiotracer distribution in the SPECT images, it can also be considered as metastasis. The final criteria for diagnosing suspicious lesions were presented in Table 1.
| No. | Criteria for diagnosing suspicious lesions |
| 1 | Results of two or more imaging techniques were consistent |
| 2 | Diagnosis was confirmed by pathological examination after operation or puncture |
| 3 | SPECT/CT follow-up review was combined with clinical history and other laboratory tests |
The 99mTc-MDP SPECT/CT imaging method is a medical imaging technique used for detecting skeletal system diseases[14]. This method involves the administration of a radiopharmaceutical called 99mTc-MDP, which is absorbed by the skeletal system after injection into the patient. The imaging is then performed using a SPECT/CT scanner. The radiopharmaceutical exhibited good biocompatibility and stability, allowing it to remain in the body for an extended period, thereby improving the quality and accuracy of the imaging. SPECT was a nuclear medicine imaging technique that detects the distribution of the radiopharmaceutical within the body. CT is an X-ray imaging technique that provides detailed information about the skeletal structure. The 99mTc-MDP SPECT/CT imaging method can be employed to detect skeletal system diseases such as fractures, osteoporosis, bone tumors, and bone metastasis. It offers high sensitivity and specificity, was non-invasive, safe, and fast, and has minimal adverse reactions and side effects for patients.
The examination utilized the Symbia intevo 6 SPECT/PET-CT system manufactured by SIEMENS (Hoffman Estates, USA), a leading company in medical imaging technology. This system was equipped with dual-head detectors and employed a low-energy high-resolution collimator for imaging. Prior to the examination, the patient received an intravenous injection of 99mTc-MDP with a dose of 925 MBq. Whole-body bone imaging, including anterior-posterior and posterior-anterior views, was conducted approximately 2.5 to 3 h after the injection. In some cases, localized imaging was also performed. Before the imaging procedure, the physician instructs the patient to empty their bladder and lie supine on the examination bed. Additionally, any metallic objects on the patient’s body are removed.
The serum PSA/fPSA test is a common screening method for PC. This test is typically performed using either enzyme-linked immunosorbent assay (ELISA) or radioimmunoassay techniques[15]. In this work, the ELISA method was utilized for detection[16]. PSA is a protein produced by the prostate gland. Its presence or risk of PC can be determined through blood testing. fPSA referred to PSA that was not bound to other proteins, while tPSA included all forms of PSA, comprising of PSA bound to other proteins. By measuring the ratio of fPSA to tPSA, doctors can assess the risk of PC.
The' fasting venous blood of patient was collected in the morning and centrifuged to obtain the serum, which was then frozen at -80 °C. After completion of serum collection from all patients, PSA/fPSA testing was performed following the steps outlined in Table 2.
| No. | Operations procedures of ELISA |
| 1 | Coating: the antigen or antibody solution to be detected was coated on the microporous plate and adsorbed on the pore wall |
| 2 | Blocking: a certain concentration of protein (such as bovine serum albumin) was added to block unadsorbed pore walls to avoid non-specific binding |
| 3 | Addition of a certain concentration of detection antibody: the detection antibody labeled with enzyme was added to the well, and the antigen or antibody has been adsorbed |
| 4 | Wash: the unbound antibody in the hole was absorbed with a buffer solution |
| 5 | Addition of substrate: substrate was added to catalyze the reaction by the enzyme to produce a measurable signal |
| 6 | Reading plate: the signal is read by the enzyme marker to calculate the concentration of antigen or antibody |
The experimental instruments included a SPECT/CT imaging system (the dual-head Symbia intevo 6 SPECT/CT system manufactured by SIEMENS) and a centrifuge (the Eppendorf 5804/5804R refrigerated centrifuge).
The experimental reagents included the 99mTc-MDP radioactive isotope used with an activity of 925-1110 MBq. The PSA/fPSA testing was performed using an ELISA PSA/fPSA testing kit.
In this work, the research data were processed using SPSS 20.0. The quantitative data, such as serum PSA and matrix metalloproteinase-9 (MMP9) expression, are presented as the mean ± standard deviation. For comparisons between two groups, t-test analysis was conducted. For comparisons involving multiple sample rates, the χ2 test was employed. P < 0.05 was considered statistically significant. Additionally, the independent samples t-test was utilized for group comparisons. Furthermore, receiver operating characteristic (ROC) curve analysis was performed to evaluate the diagnostic value of serum PSA and MMP9 levels in PC bone metastasis.
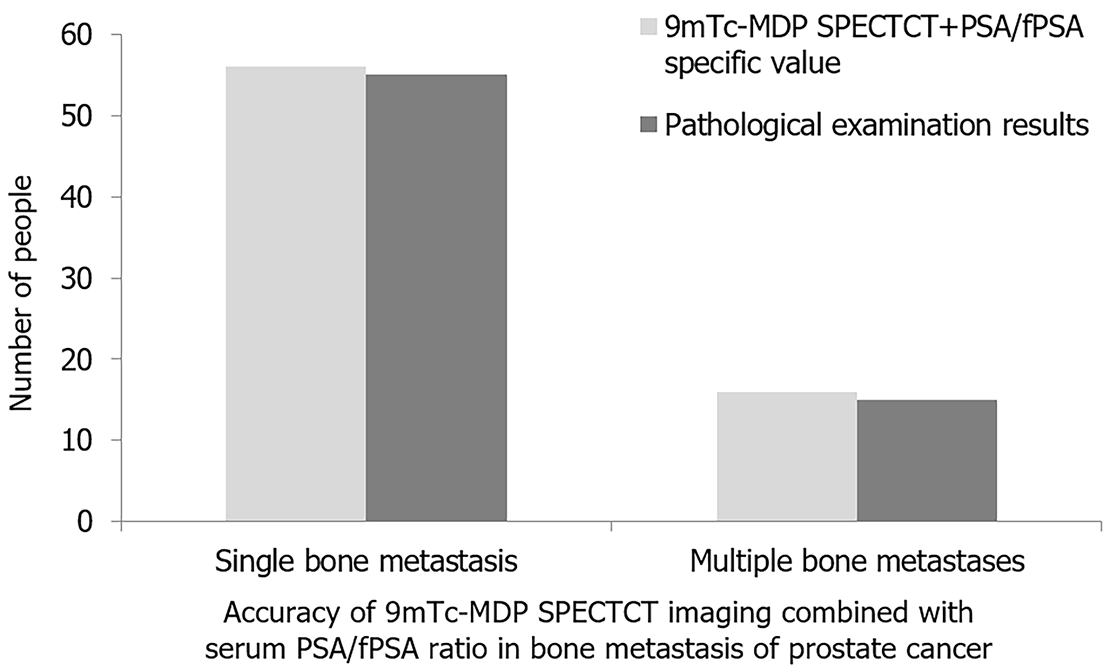
The Exp group consisted of patients with ages ranging from 50 years to 86 years, with a mean age of 72.5 years. Among them, 52 cases had low-grade carcinoma, 30 cases had moderate-grade carcinoma, and 18 cases had high-grade carcinoma. In the Ctrl group, the patient age ranged from 37 years to 65 years, with a mean age of 45.7 years. No obvious differences were observed between the Exp group and Ctrl group in terms of age, sex, occupation, work experience, education level, marital status, family background, or income level (P > 0.05). Postoperative pathological results revealed a total of 70 cases with PC bone metastasis, including 53 cases with multiple bone metastases and 17 cases with solitary bone metastasis.
A total of 100 postoperative pathological results from PC patients revealed 70 cases with PCBM and 30 cases without. The specific details of diagnosing PCBM using 99mTc-MDP SPECT/CT and SPECT/CT are illustrated in Figure 1. Difference in sensitivity and negative predictive value (NPV) was not great between 99mTc-MDP SPECT/CT and SPECT/CT for diagnosing PCBM (P > 0.05). However, a visible difference was found in positive predictive value (PPV) and specificity (P < 0.05).
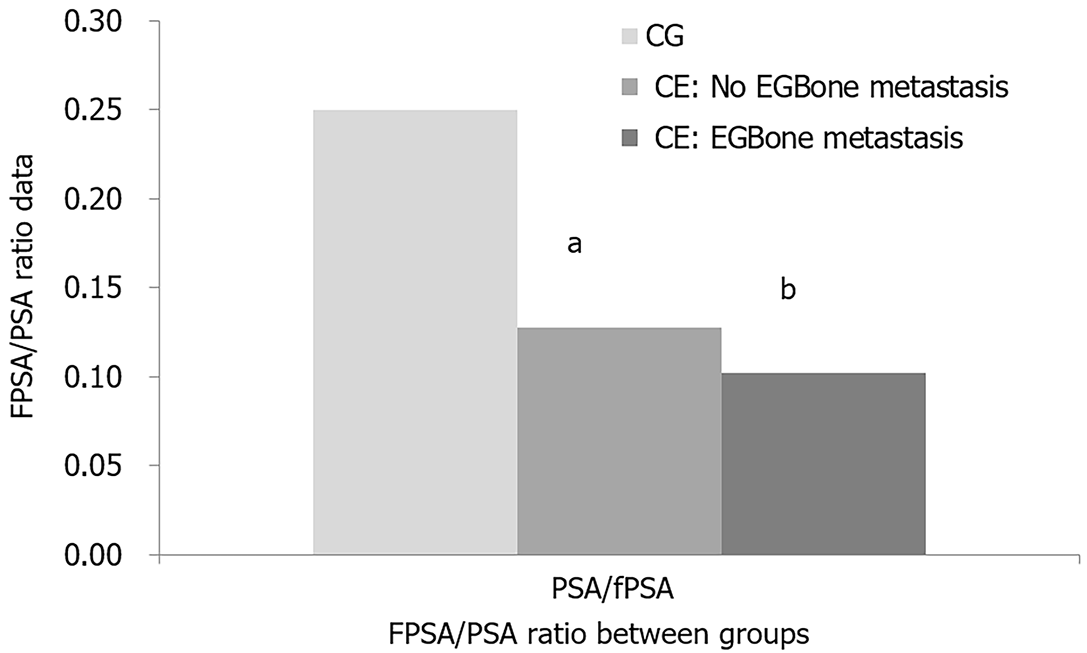
According to Figure 2, it was evident that the PSA/fPSA ratio of PC patients in the Exp group was much lower than that of patients in the Ctrl group. Specifically, among PC patients in the Exp group, those who developed bone metastasis had a greatly lower PSA/fPSA ratio compared to those who did not, showing a substantial difference with P < 0.05. This conclusion indicates that the PSA/fPSA ratio can serve as a predictive indicator for patients with PCBM. When the PSA/fPSA ratio was lower, patients may be more prone to developing bone metastasis. Therefore, regular monitoring of the PSA/fPSA ratio in PC patients can assist doctors in timely detection of the risk of bone metastasis and implementation of appropriate treatment measures.
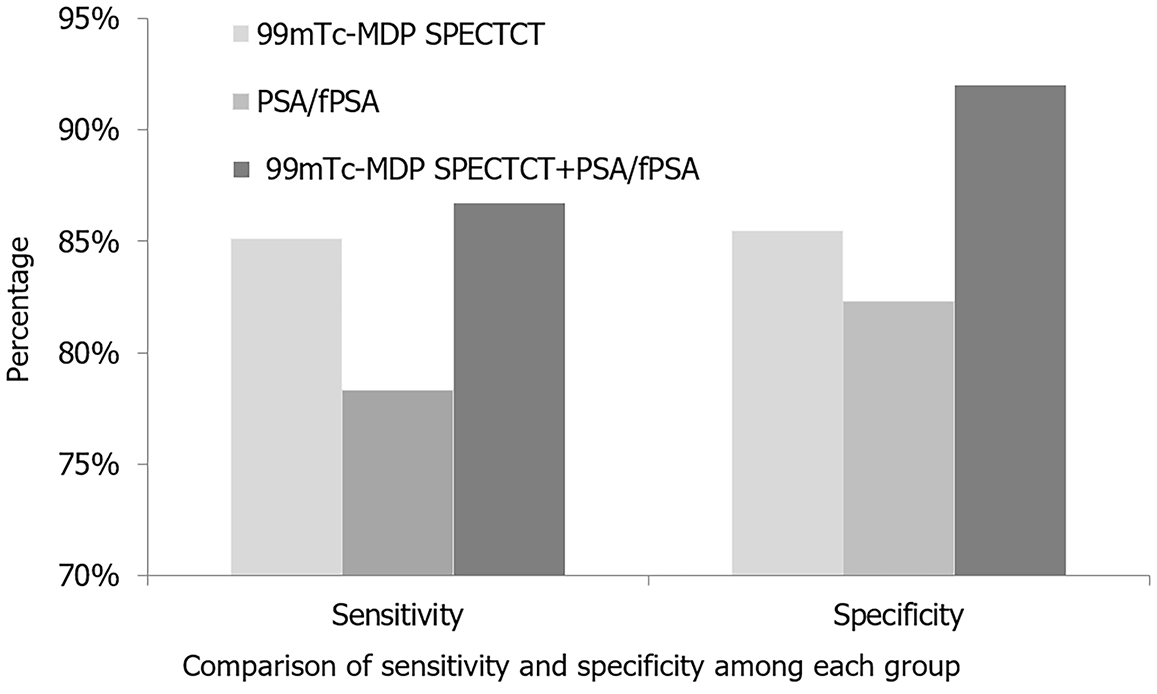
After evaluating PCBM using 99mTc-MDP SPECT/CT imaging, the diagnostic accuracy was found to be high with an area under the ROC curve of 0.979. Furthermore, when combined with the serum PSA/fPSA ratio for diagnosis, the accuracy of 99mTc-MDP SPECT/CT imaging was even higher, with an AOC of 0.986. This combination allowed for a more precise diagnosis of PCBM. Detailed information is presented in Figure 3.
The combined 9mTc-MDP SPECT/CT imaging with serum PSA/fPSA ratio achieved a 95% accurate detection rate for PCBM, as illustrated in Figure 4.
The prostate is an important organ in the male reproductive system, and its venous drainage passes through the prostatic venous plexus and eventually drains into the internal iliac vein[17]. Due to the extensive connectivity between the prostatic venous plexus and the vertebral venous plexus, PC is highly susceptible to bone metastasis[18]. Nuclear imaging using radioisotopes is essential in diagnosis, allowing early detection of metastatic lesions in bone, often 6 mo or more before X-ray findings[19]. Therefore, timely nuclear imaging is essential for PC patients, as it can help physicians to identify bone metastases in time, develop more effective treatment strategies, and improve treatment outcomes and survival rates[20]. 99mTc-MDP SPECT/CT imaging is a nuclear medicine imaging technique for the detection of bone diseases and tumors. It has the advantages of high sensitivity, high specificity, noninvasive measurement, and high safety. The combination of 99mTc-MDP SPECT/CT imaging and serum PSA/fPSA ratio is more effective in detecting PCBM patients. Some studies have shown that PSA is an effective predictor of bone metastasis in PC patients[21]. 99mTc-MDP SPECT/CT can accurately identify bone lesions and tumors, minimizing misdiagnosis and missed diagnosis. Serum MMP9 can effectively reflect the degree of malignant transformation of tumors. Yi et al[22] showed that 18F-fluorodeoxyglucose PET can be used to detect primary lesions and distant metastases of PC. Al-faham and Jolepalem[23] proposed that SPECT/CT and 99mTc-MDP bone scintigraphy were adopted for the diagnosis of symptomatic acromial bone. Mandegaran et al[24] showed that compared with Tc-MDP two-phase bone scan, Tc-MDP SPECT/CT has better sensitivity and specificity in the diagnosis of aseptic loosening and periprosthetic infection in patients undergoing painful knee arthroplasty. Viragh et al[25] and Mandegaran et al[26] indicated that 99mTc-MDP-SPECT/CT scan can obtain anatomical features and functional information of bone. These studies have shown that 99mTc-MDP SPECT/CT is a reliable, accurate, safe, and non-invasive imaging method for the diagnosis and treatment of bone diseases and tumors. In this work, the sensitivity of 99mTc-MDP SPECT/CT and NPV was roughly comparable, but the PPV and specificity of the Exp group were better than those of SPECT/CT imaging.
The PSA/fPSA ratio is also an important indicator of PC. PSA is a protein secreted by prostate cells, and its level can reflect the presence and malignancy of PC. fPSA refers to the free form of PSA, and its level can better reflect the risk of malignancy and metastasis of PC compared with total PSA[27]. Therefore, the combination of 99mTc-MDP SPECT/CT imaging and serum PSA/fPSA ratio can provide patients with more accurate diagnosis of PCBM and more accurate treatment plan for patients. In contrast to other studies[28,29], 99mTc-MDP SPECT/CT imaging combined with the serum PSA/fPSA ratio is able to detect very small tumors or abnormal cells. It also allows accurate identification of tumors or abnormal cells and minimizes the risk of misdiagnosis or missed diagnosis. In addition, it is a non-invasive testing method that does not require surgical or invasive intervention, ensuring minimal harm to the patient’s body. Serdarevic et al[30] used PSA/fPSA ratio to detect PSA immunity, and the measured tPSA and fPSA concentrations were different, which also provided a reference for the clinical judgment of prostate biopsy. Some studies have shown that 99mTc-MDP SPECT/CT imaging combined with serum PSA/fPSA ratio can improve the accuracy of detecting PCBM[31]. Compared with other methods, this method has higher sensitivity and specificity, enables earlier detection of bone metastases, and better differentiation between benign and malignant diseases. The results of this work showed that the PSA/fPSA ratio of PC patients in the Exp group was lower than that in the BPL group, and the PSA/fPSA ratio of the PCBM group was much lower than that of the no PC group. These results suggest that PSA/fPSA ratio has a certain diagnostic significance in the diagnosis of PCBM. First, the PSA/fPSA ratio was lower in PC patients in the Exp group than in BPL patients, suggesting that PC patients may contribute to a decrease in the PSA/fPSA ratio in the presence of bone metastases. This may be due to the release of PC cells into bone tissue due to bone metastasis, which makes the level of fPSA relatively low, resulting in a decrease in PSA/fPSA ratio. Second, the PSA/fPSA ratio of patients in the PCBM group was much lower than that in the no PC group, which further supports the potential value of the PSA/fPSA ratio in the diagnosis of PCBM. The lower PSA/fPSA ratio in PCBM patients may reflect the presence of bone metastases, since bone metastases usually result in PC cells being released into the bone marrow, thereby reducing PSA levels in the blood. Therefore, the decrease of PSA/fPSA ratio may indicate the presence of PCBM. In conclusion, the PSA/fPSA ratio of PC patients in the Exp group was lower than that of BPL patients and the PSA/fPSA ratio of PCBM patients was much lower than that of no PC patients, suggesting that PSA/fPSA ratio may be a useful indicator for evaluating PCBM. However, further studies are needed to verify this finding and to determine the accuracy and reliability of the PSA/fPSA ratio in clinical practice.
The results of this work demonstrated that the combination of 99mTc-MDP SPECT/CT imaging with the serum PSA/fPSA ratio can effectively diagnose PCBM with high accuracy and reliability. This method can serve as an important reference index for the clinical diagnosis of PCBM. However, this work was subjected to some limitations, such as a small sample size and regional representation of the patient samples. Therefore, further multicenter, large-sample, prospective studies are needed to validate the reliability and generalizability of the results obtained in this work. Only through more rigorous study design and comprehensive data analysis can it better evaluate the clinical applicability of this method and provide more scientific and precise guidance for diagnosing and treating PCBM.
| 1. | Zhang T, Li J, Dai J, Yuan F, Yuan G, Chen H, Zhu D, Mao X, Qin L, Liu N, Yang M. Identification of a novel stemness-related signature with appealing implications in discriminating the prognosis and therapy responses for prostate cancer. Cancer Genet. 2023;276-277:48-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Saberi F, Dehghan Z, Noori E, Taheri Z, Sameni M, Zali H. Identification of Critical Molecular Factors and Side Effects Underlying the Response to Thalicthuberine in Prostate Cancer: A Systems Biology Approach. Avicenna J Med Biotechnol. 2023;15:53-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 3. | Ye X, Huang X, Fu X, Zhang X, Lin R, Zhang W, Zhang J, Lu Y. Myeloid-like tumor hybrid cells in bone marrow promote progression of prostate cancer bone metastasis. J Hematol Oncol. 2023;16:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 4. | Li X, Peng B, Zhu X, Wang P, Xiong Y, Liu H, Sun K, Wang H, Ou L, Wu Z, Liu X, He H, Mo S, Peng X, Tian Y, Zhang R, Yang L. Changes in related circular RNAs following ERβ knockdown and the relationship to rBMSC osteogenesis. Biochem Biophys Res Commun. 2017;493:100-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Viragh K, Khoshchehreh M, Zung T, Ni C. 99mTc-MDP Bone Scintigraphy and SPECT/CT of Extensive Subcutaneous Calcification in the Setting of Cosmetic-Induced Lipogranulomatosis. Clin Nucl Med. 2022;47:e199-e200. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Abdelhafez YG, Godinez F, Sood K, Hagge RJ, Boutin RD, Raychaudhuri SP, Badawi RD, Chaudhari AJ. Feasibility of dual-phase (99m)Tc-MDP SPECT/CT imaging in rheumatoid arthritis evaluation. Quant Imaging Med Surg. 2021;11:2333-2343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Liu H, Xiong Y, Zhu X, Gao H, Yin S, Wang J, Chen G, Wang C, Xiang L, Wang P, Fang J, Zhang R, Yang L. Icariin improves osteoporosis, inhibits the expression of PPARγ, C/EBPα, FABP4 mRNA, N1ICD and jagged1 proteins, and increases Notch2 mRNA in ovariectomized rats. Exp Ther Med. 2017;13:1360-1368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 8. | Wu B, Shao Y, Lin X, Hasi C, Jia W, Wang D, Cao X. Comparisons of the diagnostic accuracy across prostate health index, prostate health index density, and percentage free prostate-specific antigen for clinically significant prostate cancer: a prospective diagnostic study. Transl Androl Urol. 2023;12:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Song SH, Kim H, Kim JK, Lee H, Oh JJ, Lee SC, Jeong SJ, Hong SK, Lee J, Yoo S, Choo MS, Cho MC, Son H, Jeong H, Suh J, Byun SS. A smart, practical, deep learning-based clinical decision support tool for patients in the prostate-specific antigen gray zone: model development and validation. J Am Med Inform Assoc. 2022;29:1949-1957. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Tang Q, Liang Z, Zhou Y, Huang Y. Exploration of the Value of Combined UA, IL-6, and fPSA/tPSA in the Diagnosis of Prostate Cancer. Comput Math Methods Med. 2022;2022:8542376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Song W, Ding N, Zhang X, Liu J, Wang Y, Yan J, Liu S. Mean Platelet Volume Enhances the Diagnostic Specificity of PSA for Prostate Cancer. Front Surg. 2022;9:845288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Chen M, Chen S, Li X, Li Y. An Ectopic Parathyroid Adenoma Mimicking Submandibular Gland on 99mTc-MIBI Parathyroid Scintigraphy. Clin Nucl Med. 2022;47:916-917. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Chen Y, Ning Y, Liu X, Cai M, Li S. A case of accidental local pulmonary (99m)Tc-MDP uptake on bone SPECT/CT. Clin Case Rep. 2022;10:e6656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Mattay GS, O'Leary C, Dubroff JG, R Pantel A. 99mTc-Mebrofenin SPECT/CT in Hepatic Infarction. Clin Nucl Med. 2021;46:e8-e10. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Sun X, Lu Y, Zhu H, Li R, Zhang D, Pang K. Effects of Psychological Intervention on Perioperative Quality of Life and Serum PSA and FPSA Levels of Patients with Prostate Cancer Treated with Integrated Traditional Chinese and Western Medicine. Evid Based Complement Alternat Med. 2021;2021:9286905. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 16. | Dos Santos GA, Viana NI, Pimenta R, de Camargo JA, Guimaraes VR, Romão P, Candido P, Dos Santos VG, Ghazarian V, Reis ST, Leite KRM, Srougi M. Upregulation of shelterin and CST genes and longer telomeres are associated with unfavorable prognostic characteristics in prostate cancer. Cancer Genet. 2024;284-285:20-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (1)] |
| 17. | Šimánek V, Vrzáková R, Viták R, Jirásko M, Fürst T, Topolčan O, Pecen L, Vurm V, Kučera R. Preanalytical stability of molecular forms of prostate-specific antigen in serum samples (PSA, free PSA, [-2]proPSA) and their impact on fPSA/tPSA ratio and PHI. Prostate. 2024;84:656-665. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Huang MP, Tang P, Klein CS, Wei XH, Du W, Fu JG, Huang TH, Chen H, Xie KJ. Free PSA performs better than total PSA in predicting prostate volume in Chinese men with PSA levels of 2.5-9.9 ng ml(-1). Asian J Androl. 2023;25:82-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 19. | Wang H, Trusheim ME, Kim L, Raniwala H, Englund DR. Field programmable spin arrays for scalable quantum repeaters. Nat Commun. 2023;14:704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Patel CM, Wadas TJ, Shiozawa Y. Progress in Targeted Alpha-Particle-Emitting Radiopharmaceuticals as Treatments for Prostate Cancer Patients with Bone Metastases. Molecules. 2021;26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Huang CY, Chen CH. Clinical characteristics and survival outcomes in patients with a high PSA and non-metastatic prostate cancer. J Formos Med Assoc. 2022;121:181-186. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Yi C, Yu D, Shi X, Zhang X, Luo G, He Q, Zhang X. The combination of 13N-ammonia and 18F-FDG whole-body PET/CT on the same day for diagnosis of advanced prostate cancer. Nucl Med Commun. 2016;37:239-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Al-faham Z, Jolepalem P. Use of SPECT/CT with 99mTc-MDP Bone Scintigraphy to Diagnose Symptomatic Os Acromiale. J Nucl Med Technol. 2015;43:236-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Mandegaran R, Agrawal K, Vijayanathan S, Gnanasegaran G. The value of 99mTc-MDP bone SPECT/CT in evaluation of patients with painful knee prosthesis. Nucl Med Commun. 2018;39:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 25. | Viragh K, Khoshchehreh M, Zung T, Ni C. 99mTc-MDP Bone Scintigraphy and SPECT/CT of Extensive Subcutaneous Calcification in the Setting of Cosmetic-Induced Lipogranulomatosis. Clin Nucl Med. 2022;47(2):e199-e200. . [PubMed] [DOI] [Full Text] |
| 26. | Mandegaran R, Dhillon S, Jen H. Beyond the bones and joints: a review of ligamentous injuries of the foot and ankle on (99m)Tc-MDP-SPECT/CT. Br J Radiol. 2019;92:20190506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Costa IAD, Hennenlotter J, Todenhöfer T, Neumann E, Deininger S, Aufderklamm S, Bedke J, Stenzl A, Rausch S. Determination of Free-PSA (fPSA) and fPSA/PSA-Ratio Using A Point-of-Care Device. Clin Lab. 2019;65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Bertok T, Jane E, Bertokova A, Lorencova L, Zvara P, Smolkova B, Kucera R, Klocker H, Tkac J. Validating fPSA Glycoprofile as a Prostate Cancer Biomarker to Avoid Unnecessary Biopsies and Re-Biopsies. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Zhu YC, Cai B, Jiang Q, Zhang Y, Sha J, Xie S. MXene-assisted organic electrochemical transistor biosensor with multiple spiral interdigitated electrodes for sensitive quantification of fPSA/tPSA. J Nanobiotechnology. 2021;19:386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Serdarevic N, Dabla P, Stanciu AE. Systematic Differences Between Total and Free Prostate-Specific Antigen Immunoassays: Comparison Using Passing and Bablok Regression. Indian J Clin Biochem. 2021;36:151-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 31. | Guan X, Sun Y, Zhang H, Liang K, Long K, Li J, Tang S, Liu C. Comparison of Architect i2000sr and Cobas e601 Systems for Determining Serum Human Chorionic Gonadotropin-Beta. Clin Lab. 2016;62:1815-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |