Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4074
Revised: April 19, 2024
Accepted: April 23, 2024
Published online: July 16, 2024
Processing time: 130 Days and 4.2 Hours
Breast cancer (BC) is the second leading cause of tumor-related mortality after lung cancer. Chemotherapy resistance remains a major challenge to progress in BC treatment, warranting further exploration of feasible and effective alternative therapies.
To analyzed the quality of life (QoL) and survival of patients with BC treated with integrated traditional Chinese and Western medicine (TCM-WM).
This study included 226 patients with BC admitted to the First Affiliated Hospital of Guangxi University of Traditional Chinese Medicine between February 2018 and February 2023, including 100 who received conventional Western medicine treatment (control group) and 126 who received TCM-WM treatment (research group). The total effective rate, side effects (alopecia, nausea and vomiting, hepatorenal toxicity, and myelosuppression), QoL assessed using the European Organization for Research and Treatment of Cancer Core Quality of Life Ques
The research group showed statistically better overall efficacy, EORTC QoL-C30 scores, and 1-year OS than the control group, with markedly lower side effects and 1-year recurrence and metastasis rates. Moreover, the posttreatment levels of serum inflammatory in the research group were significantly lower than the baseline and those in the control group.
Overall, TCM-WM demonstrated significantly improved therapeutic efficacy while ensuring drug safety in BC, which not only improved patients’ QoL and prolonged survival, but also significantly inhibited the inflammatory response.
Core Tip: This study mainly analyzed the effects of integrated traditional Chinese and Western medicine (TCM-WM) on the quality of life (QoL) and survival in breast cancer (BC). Based on the total effective rate, medication side effects, QoL, 1-year overall survival, recurrence and metastasis rates, and serum inflammatory factors, we confirmed that TCM-WM showed significantly enhanced therapeutic efficacy while upholding medication safety, thereby improving QoL and survival and significantly inhibiting the inflammatory response. The findings indicate the potential of TCM-WM as a clinically effective BC treatment that can improve the QoL and prolong the survival of patients.
- Citation: Wang YK, Zhu RW, Gao ZP, Tao Y. Quality of life and survival analyses of breast cancer cases treated with integrated traditional Chinese and Western medicine. World J Clin Cases 2024; 12(20): 4074-4081
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4074.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4074
Breast cancer (BC) is a fatal neoplastic disease and the second largest tumor-related cause of death after lung cancer[1]. Age of menarche, number of pregnancies, parity, breast biopsy history, and family history of BC are some of the risk factors with varying degrees of influence on BC occurrence or progression[2]. The disease can be divided according to molecular subtype into hormone (estrogen, progesterone) receptor positive, human epidermal growth factor receptor 2 overexpression (HER2+), and triple negative BC (TNBC). Hormone receptor positive BC is the most common subtype[3-5]. Despite advances in BC diagnosis and treatment, chemotherapy resistance remains a major challenge to progress in BC treatment[6]. Moreover, although many women with BC have survived the disease, they still suffer from physical abnormalities, such as chronic pain, lymphedema, and hallucinatory breast pain, and symptoms, such as fatigue, decreased mobility, cognitive dysfunction, and emotional disturbance, which negatively affect quality of life (QoL)[7]. Therefore, the discovery of a feasible and effective alternative therapy has great clinical significance in improving patients’ QoL and prolonging their survival.
Commonly used standard Western medicine treatments for BC include surgery, chemoradiotherapy, and targeted therapy, all of which having varying degrees of efficacy[8,9]. However, Western medicine treatment also has its limitations. For example, surgical intervention cannot always completely remove the tumor and is otherwise unsuitable for patients with tumor spread. Chemoradiotherapy has potential side effects and is hindered by drug resistance, whereas targeted therapy is limited in trial scope and expensive[10,11]. In contrast, integrated traditional Chinese and Western medicine (TCM-WM) therapy, which includes moxibustion, acupuncture, qigong, cupping, Chinese herbal medicine, traditional Chinese medicine (TCM) massage, and other intervention options, can provide patients with a personalized overall treatment plan after TCM dialectical diagnosis[12]. Moreover, TCM-WM treatment has advantages over traditional Western medicine, mainly in terms of reducing gastrointestinal adverse reactions, lowering abnormally high tumor marker levels, and improving QoL[13]. Lee et al[14] highlighted that the use of different types of TCM therapy in cancer treatment can stabilize the body’s immunity and inhibit tumor development. Furthermore, its combination with Western medicine therapy improves the prognosis and survival of patients with BC.
This study primarily explored the clinical efficacy of TCM-WM in patients with BC and its influence on patients’ QoL and survival, hoping to provide a reliable clinical reference for improving the treatment efficacy of BC.
In total, 226 patients with BC admitted to the First Affiliated Hospital of Guangxi University of Traditional Chinese Medicine between February 2019 and February 2022 were enrolled, including 100 patients who received conventional Western medicine therapy (control group) and 126 who received TCM-WM (research group). The two groups were clinically comparable without significant difference in general information (P > 0.05).
The inclusion criteria were as follows: met the relevant diagnostic criteria for BC and were confirmed as BC by postoperative pathology; patients were further divided into the following disease subtypes according to TCM dialectics: liver Qi stagnation, Qi-blood deficiency, Chong-Ren disharmony, and toxic-heat accumulation; positive test for progesterone receptor or estrogen receptor; no contraindications for the therapy used in this study, and could accept and complete the treatment with a life expectancy ≥ 6 months; and intact clinical data and no deliberate concealment of clinical history.
The exclusion criteria were as follows: Received systematic chemoradiotherapy, endocrine therapy, or targeted therapy; complications involving other malignant tumors; heart, lung, and kidney dysfunction; immune system diseases or diabetes; alcohol abuse history; poor compliance; and cognitive impairment.
The control group was treated with conventional Western medicine. Chemotherapy regimens, such as CAF (cyclophosphamide, adriamycin and 5-fluorouracil), TAC (platinum drugs, adriamycin and cyclophosphamide), and TEC (doxorubicin, cyclophosphamide, and epirubicin), were administered according to the patient’s condition.
In addition to the said regimens, the research group was further given TCM therapy. Patients with BC accompanied by liver Qi stagnation, Qi-blood deficiency, Chong-Ren disharmony, or toxic-heat accumulation were given Chaihu Shugan Powder, Xiangbei Yangrong Decoction, Xiangbei Yangrong Decoction + Xiaoyao Powder, or Huoxue Sanyu Decoction + Huanglian Jiedu Decoction, respectively. In addition, moxibustion, acupuncture, qigong, cupping, TCM massage, and other treatments were given depending on the patient’s condition.
Treatment efficacy. Evaluation criteria for treatment efficacy: Significantly effective refers to the disappearance of BC tumor lesions, areolar abnormalities, pain, and other symptoms after treatment; effective means that, after treatment, the development of the lesion is well suppressed, and the related clinical symptoms are obviously alleviated; ineffective refers to the absence of improvement in lesions and clinical symptoms after treatment. The total effective rate is the percentage of the sum of obvious and effective cases in the total number of cases.
Side effects of medication: The number of adverse reactions, such as alopecia, nausea and vomiting, hepatorenal toxicity, and myelosuppression, in both groups were observed and recorded, and the incidence rates were calculated.
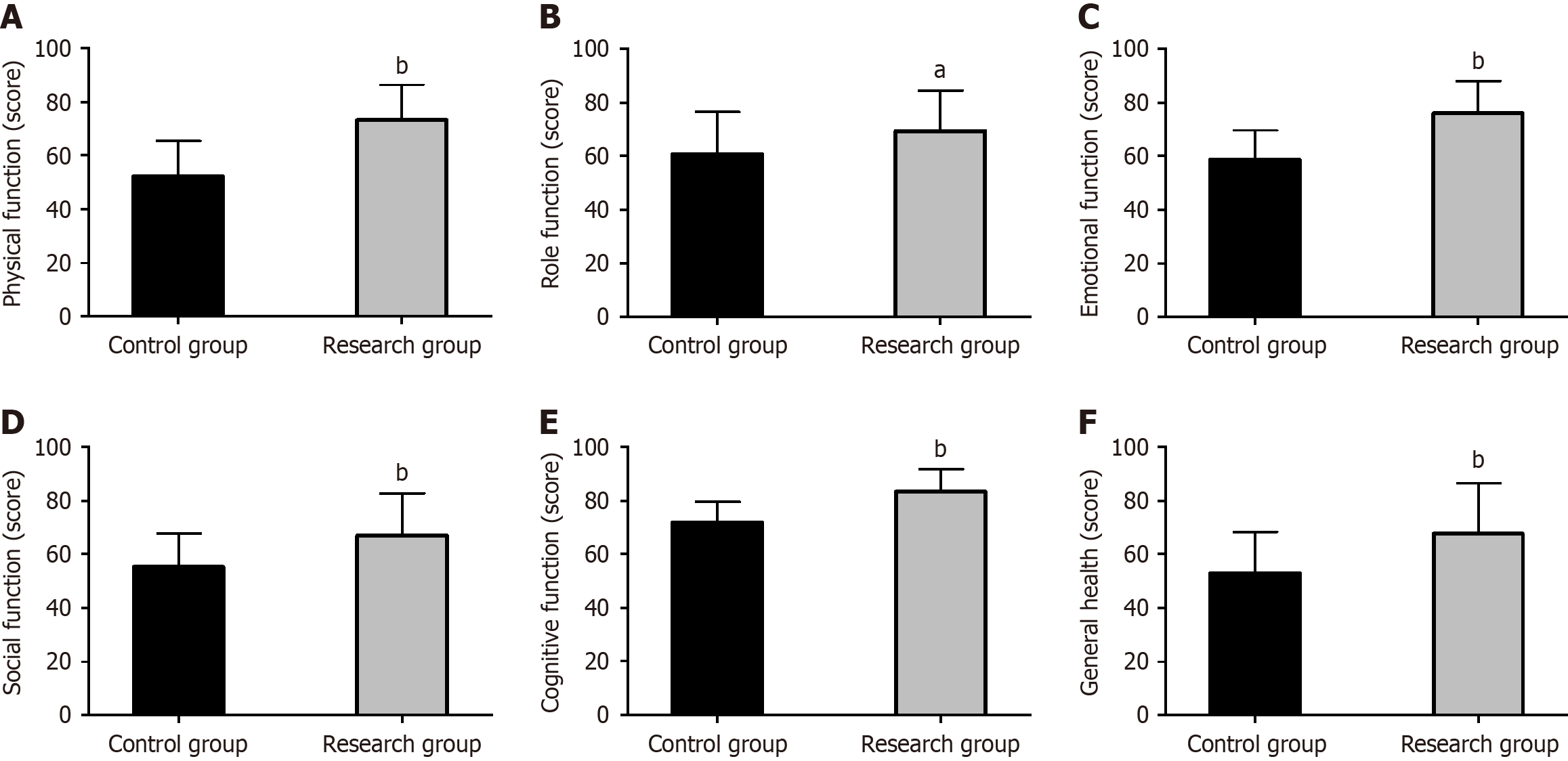
QoL: The European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire (EORTC QLQ-C30) was used to assess QoL in terms of physical, role, emotional, social, and cognitive functions and overall health. The score, ranging from 0 to 100, is directly proportional to the patient’s QoL.
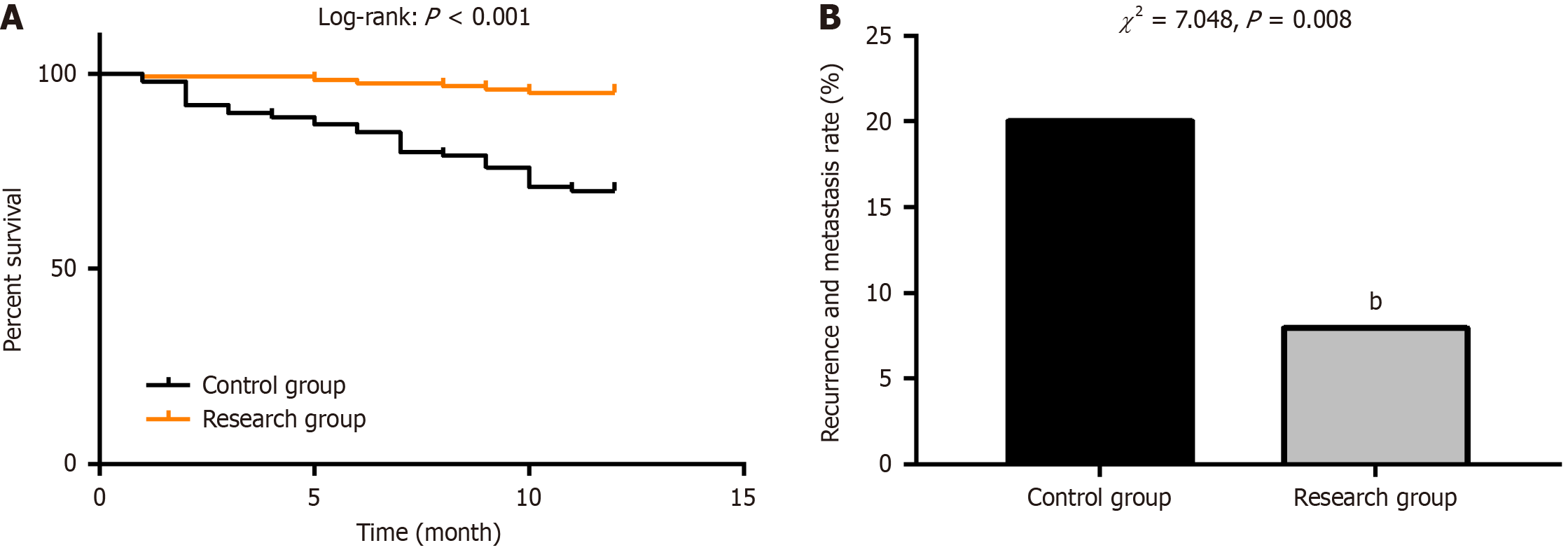
OS: All patients were followed up once every 3 months for 1 year through telephone consultation and medical history inquiry. The 1-year OS and recurrence and metastasis rates were recorded.
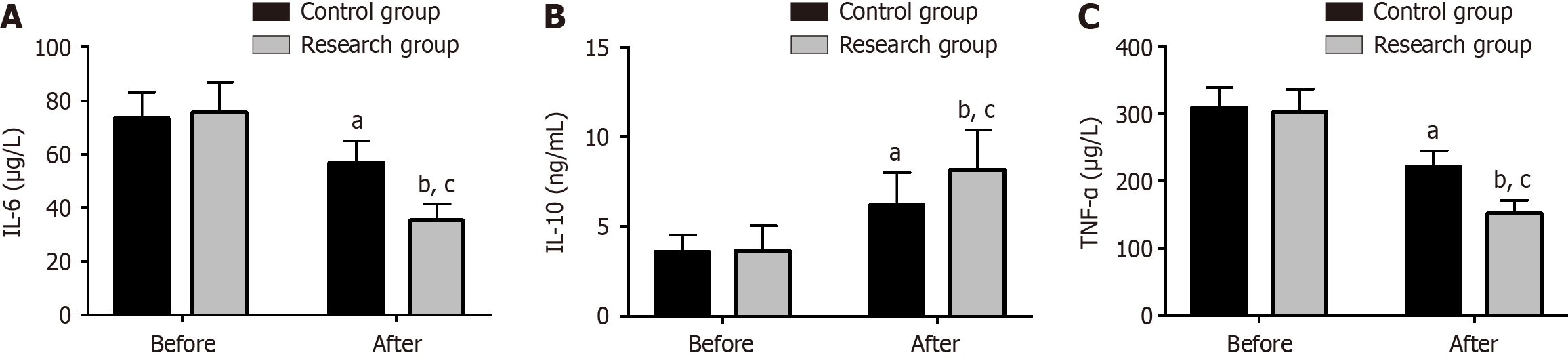
Serum inflammatory factors: Venous blood (3 mL) was collected from patients before and after treatment, and serum was obtained after centrifugation for enzyme-linked immunosorbent assay (ELISA) measurements of interleukin (IL)-6, IL-10, and tumor necrosis factor alpha (TNF-α).
Data were imported into the SPSS 26.0 software for analyses, with the statistical significance level set at P < 0.05. Normally distributed data were expressed as mean ± SD, and the independent sample t-test was used for between-group comparisons. Count data were expressed as number (percentage), and the χ2 test was used for intergroup comparisons. The survival curve was plotted using the Kaplan–Meier method.
The mean age, disease course, tumor diameter, TNM stage, pathological type, syndrome type, and other general information did not differ significantly between the control and research groups (P > 0.05; Table 1).
| Factors | n | Control group (n = 100) | Research group (n = 126) | χ2/t value | P value |
| Mean age (yr) | 226 | 46.83 ± 6.95 | 45.12 ± 9.54 | ||
| Disease course (months) | 226 | 13.52 ± 3.57 | 14.30 ± 4.06 | ||
| Tumor diameter (cm) | 226 | 2.0 ± 0.78 | 2.07 ± 0.95 | ||
| TNM stage | 0.460 | 0.794 | |||
| I | 47 | 22 (22.00) | 25 (19.84) | ||
| II | 127 | 57 (57.00) | 70 (55.56) | ||
| III | 52 | 21 (21.00) | 31 (24.60) | ||
| Pathological type | 1.392 | 0.707 | |||
| Invasive ductal carcinoma | 81 | 36 (36.00) | 45 (35.71) | ||
| Invasive lobular carcinoma | 103 | 48 (48.00) | 55 (43.65) | ||
| Mucinous adenocarcinoma | 24 | 8 (8.00) | 16 (12.70) | ||
| Medullary carcinoma | 18 | 8 (8.00) | 10 (7.94) | ||
| Syndrome type | 1.790 | 0.617 | |||
| Liver Qi stagnation | 65 | 29 (29.00) | 36 (28.57) | ||
| Qi-blood deficiency | 35 | 15 (15.00) | 20 (15.87) | ||
| Chong-Ren disharmony | 97 | 40 (40.00) | 57 (45.24) | ||
| Toxic-heat accumulation | 29 | 16 (16.00) | 13 (10.32) |
A significant intergroup difference in the total effective rate was observed (P < 0.05), with that of the research group being significantly higher total effective rate than the control group (90.48% vs 79.00%; P < 0.05; Table 2).
| Factors | Control group (n = 100) | Research group (n = 126) | χ2 | P value |
| Markedly effective | 44 (44.00) | 74 (58.73) | ||
| Effective | 35 (35.00) | 40 (31.75) | ||
| Ineffective | 21 (21.00) | 12 (9.52) | ||
| Overall efficacy | 79 (79.00) | 114 (90.48) | 5.888 | 0.015 |
The incidence rates of alopecia, nausea and vomiting, hepatorenal toxicity, and myelosuppression were significantly lower in the research group than in the control group (P < 0.05; Table 3).
| Factors | Control group (n =100) | Research group (n = 126) | χ2 | P value |
| Alopecia | 20 (20.00) | 7 (5.56) | 11.060 | < 0.001 |
| Nausea and vomiting | 14 (14.00) | 5 (3.97) | 7.286 | 0.007 |
| Hepatorenal toxicity | 11 (11.00) | 3 (2.38) | 7.127 | 0.008 |
| Myelosuppression | 9 (9.00) | 2 (1.59) | 6.616 | 0.010 |
Comparison of the EORTC QoL-C30 scores assessed from the domains of physical, role, emotional, social, and cognitive functions and overall health revealed that the research group had higher scores than the control group (P < 0.05; Figure 1).
The 1-year OS of the research group was significantly higher than that of the control group, while the 1-year recurrence and metastasis rates were significantly lower (P < 0.05; Figure 2).
Analysis of serum inflammatory factors by ELISA showed no evident intergroup differences in pre-treatment IL-6, IL-10, and TNF-α levels (P > 0.05). However, IL-6 and TNF-α in both groups were significantly reduced after treatment (P < 0.05), with even lower IL-6 and TNF-α levels in the research group (P < 0.05). Conversely, a significant increase in IL-10 was observed in both groups (P < 0.05), with a higher level in the research group than in the control group (P < 0.05; Figure 3).
The morbidity and risk of mortality of BC continue to increase in non-developed countries, and the lifetime risk of female BC is approximately 12.5%[15,16]. According to GLOBOCAN 2018, BC has directly affected 2.1 million people worldwide and has contributed to 630,000 deaths[17]. Therefore, the optimization of treatment strategies for BC is urgently needed to reduce the risk of associated death.
In this study, the control group underwent chemotherapy as one of the standard Western treatments for BC. Chemotherapy is commonly used to treat various cancers but can cause side effects, such as nausea, vomiting, decreased white blood cell count, and peripheral nerve damage[18]. In addition to chemotherapy, the research group was further treated with TCM therapy. TCM for BC is administered on the principle that the onset and progression of BC are closely related to the spleen and stomach; thus, TCM treatment of this disease mainly focuses on strengthening the spleen and stomach, invigorating spleen and supplementing Qi, benefiting Qi and nourishing the blood, strengthening body resistance and eliminating evil, and dissolving lumps and resolving masses to enhance immunity and improve QoL and outcomes[19,20]. TCM therapy is often used as a supplementary and alternative medicine in the treatment of various diseases to alleviate clinical symptoms, minimize the side effects of chemotherapy-related drugs, improve treatment efficacy and survival outcomes, and reduce the risk of tumor metastasis and recurrence to a certain extent[21,22]. patients in this study were classified into the following four subtypes according to TCM syndrome differentiation: liver Qi stagnation, Qi-blood deficiency, Chong-Ren disharmony, and toxic-heat accumulation. Chaihu Shugan Powder, Xiangbei Yangrong Decoction, Xiangbei Yangrong Decoction + Xiaoyao Powder, and Huoxue Sanyu Decoction + Huanglian Jiedu Decoction were administered, respectively. The treatment principles for patients with liver Qi stagnation are mainly to disperse stagnated liver Qi to relieve depression and soften and resolve hard masses. Treatment of patients with Qi-blood deficiency focuses on reinforcing Qi and nourishing blood, and detoxifying and resolving hard masses. The main principles of treatment for patients with Chong-Ren disharmony are soothing the liver, tonifying the kidneys, and harmonizing the Chong and Conception vessels. Finally, treatment of patients with toxic-heat accumulation is mainly to clear away heat and toxic materials, eliminate tumors, and relieve pain[23].
The research group obtained a total effective rate higher than that in the control group (90.48% vs 79.00%), suggesting that TCM-WM therapy has a superior curative effect in patients with BC. In terms of safety, significantly lower incidence rates of alopecia, nausea and vomiting, hepatorenal toxicity, and myelosuppression were observed in the research group, indicating the TCM-WM therapy is safer than conventional Western medicine therapy. In terms of QoL d, we observed higher EORTC QoL-C30 scores in the domains of physical, role, emotional, social, and cognitive functions and overall health, demonstrating that TCM-WM therapy improved the QoL of patients with BC. A systematic review and meta-analysis study found that TCM therapy for patients with BC contributed significantly alleviated musculoskeletal pain and improved QoL, with fewer adverse events, which is similar to our findings[24]. The 1-year OS in the research group was significantly higher (95.24% vs 70.00%), whereas the 1-year recurrence and metastasis rates were significantly lower than those in the control group (7.94% vs 20.00%), indicating that TCM-WM can improve survival and reduce the risk of recurrence and metastasis within 1 year. Chaihu Shugan Powder has been found to be a safe supplementary therapeutic option to chemotherapy. It not only helps to enhance the curative effect and reduce the risk of myelosuppression, but also significantly improves prognosis in BC[25], which is also similar to our findings. Lee et al[26] confirmed that TCM adjuvant therapy in patients with advanced BC treated with taxanes effectively improved the survival rate, consistent with our research results. Furthermore, consistent with our results, the application of TCM therapy in TNBC reduced the risk of disease-related recurrence and metastasis by 11%[27]. ELISA revealed that IL-6 and TNF-α were significantly decreased in the research group after treatment and were lower compared with the control group, whereas IL-10 was significantly upregulated and higher vs the control group. Therefore, intervention with TCM-WM for patients with BC has a superior regulatory effect on the inflammatory response.
This study has several limitations. First, only 1 year of follow-up was conducted, which should be extended to 3–5 years to further understand the long-term efficacy of TCM-WM therapy and its impact on the prognosis of patients with BC. Second, the accuracy of the study results may be biased due to the small number of cases (n = 226) included, all of which were from a single institution. Finally, risk factors affecting the efficacy or side effects of medication in patients with BC were not analyzed, which should be further explored to optimize the management of patients with BC.S.
TCM-WM therapy for patients with BC has definite curative effects and higher safety compared with Western medicine therapy alone. Treatment with TCM-WM improved QoL, increased the 1-year OS, reduced the risk of 1-year tumor recurrence and metastasis, and regulated and ameliorated the serum inflammatory microenvironment.
| 1. | Grabinski VF, Brawley OW. Disparities in Breast Cancer. Obstet Gynecol Clin North Am. 2022;49:149-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 61] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 2. | Budny A, Starosławska E, Budny B, Wójcik R, Hys M, Kozłowski P, Budny W, Brodzik A, Burdan F. [Epidemiology and diagnosis of breast cancer]. Pol Merkur Lekarski. 2019;46:195-204. [PubMed] |
| 3. | Nagini S. Breast Cancer: Current Molecular Therapeutic Targets and New Players. Anticancer Agents Med Chem. 2017;17:152-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 336] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 4. | Andrahennadi S, Sami A, Manna M, Pauls M, Ahmed S. Current Landscape of Targeted Therapy in Hormone Receptor-Positive and HER2-Negative Breast Cancer. Curr Oncol. 2021;28:1803-1822. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 5. | Yip CH, Rhodes A. Estrogen and progesterone receptors in breast cancer. Future Oncol. 2014;10:2293-2301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 135] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 6. | Mehraj U, Dar AH, Wani NA, Mir MA. Tumor microenvironment promotes breast cancer chemoresistance. Cancer Chemother Pharmacol. 2021;87:147-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 146] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 7. | Lovelace DL, McDaniel LR, Golden D. Long-Term Effects of Breast Cancer Surgery, Treatment, and Survivor Care. J Midwifery Womens Health. 2019;64:713-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 203] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 8. | Al-Hilli Z, Wilkerson A. Breast Surgery: Management of Postoperative Complications Following Operations for Breast Cancer. Surg Clin North Am. 2021;101:845-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 9. | Fisusi FA, Akala EO. Drug Combinations in Breast Cancer Therapy. Pharm Nanotechnol. 2019;7:3-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 254] [Article Influence: 42.3] [Reference Citation Analysis (0)] |
| 10. | Chargari C, Deutsch E, Blanchard P, Gouy S, Martelli H, Guérin F, Dumas I, Bossi A, Morice P, Viswanathan AN, Haie-Meder C. Brachytherapy: An overview for clinicians. CA Cancer J Clin. 2019;69:386-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 168] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 11. | Burstein HJ, Curigliano G, Thürlimann B, Weber WP, Poortmans P, Regan MM, Senn HJ, Winer EP, Gnant M; Panelists of the St Gallen Consensus Conference. Customizing local and systemic therapies for women with early breast cancer: the St. Gallen International Consensus Guidelines for treatment of early breast cancer 2021. Ann Oncol. 2021;32:1216-1235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 442] [Cited by in RCA: 499] [Article Influence: 124.8] [Reference Citation Analysis (0)] |
| 12. | Porter D, Cochrane S, Zhu X. Current Usage of Traditional Chinese Medicine for Breast Cancer-A Narrative Approach to the Experiences of Women with Breast Cancer in Australia-A Pilot Study. Medicines (Basel). 2017;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Bai X, Ta N, Gong GH, Zhang B, Wei CX. Effects of Integrated Chinese Traditional Medicine and Conventional Western Medicine on the Quality of Life of Breast Cancer Patients: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2022;2022:3123878. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Lee YC, Chen YH, Huang YC, Lee YF, Tsai MY. Effectiveness of Combined Treatment with Traditional Chinese Medicine and Western Medicine on the Prognosis of Patients with Breast Cancer. J Altern Complement Med. 2020;26:833-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 15. | Fahad Ullah M. Breast Cancer: Current Perspectives on the Disease Status. Adv Exp Med Biol. 2019;1152:51-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 351] [Article Influence: 58.5] [Reference Citation Analysis (0)] |
| 16. | Pearce L. Breast cancer. Nurs Stand. 2016;30:15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55842] [Article Influence: 7977.4] [Reference Citation Analysis (132)] |
| 18. | Gadisa DA, Assefa M, Wang SH, Yimer G. Toxicity profile of Doxorubicin-Cyclophosphamide and Doxorubicin-Cyclophosphamide followed by Paclitaxel regimen and its associated factors among women with breast cancer in Ethiopia: A prospective cohort study. J Oncol Pharm Pract. 2020;26:1912-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Lin YH, Chiu JH. Use of Chinese medicine by women with breast cancer: a nationwide cross-sectional study in Taiwan. Complement Ther Med. 2011;19:137-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Yuan Z, Pan Y, Leng T, Chu Y, Zhang H, Ma J, Ma X. Progress and Prospects of Research Ideas and Methods in the Network Pharmacology of Traditional Chinese Medicine. J Pharm Pharm Sci. 2022;25:218-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 59] [Reference Citation Analysis (1)] |
| 21. | Li L, Wang R, Zhang A, Wang L, Ge Q, Liu Y, Chen T, Wang CC, Leung PC, Sun Q, Fan X. Evidence on Efficacy and Safety of Chinese Medicines Combined Western Medicines Treatment for Breast Cancer With Endocrine Therapy. Front Oncol. 2021;11:661925. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Wang BR, Chang YL, Chen TJ, Chiu JH, Wu JC, Wu MS, Chou CL, Chou YC. Coprescription of Chinese herbal medicine and Western medication among female patients with breast cancer in Taiwan: analysis of national insurance claims. Patient Prefer Adherence. 2014;8:671-682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Ji Q, Luo YQ, Wang WH, Liu X, Li Q, Su SB. Research advances in traditional Chinese medicine syndromes in cancer patients. J Integr Med. 2016;14:12-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 24. | Poo CL, Dewadas HD, Ng FL, Foo CN, Lim YM. Effect of Traditional Chinese Medicine on Musculoskeletal Symptoms in Breast Cancer: A Systematic Review and Meta-Analysis. J Pain Symptom Manage. 2021;62:159-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Xiao K, Li K, Long S, Kong C, Zhu S. Potential Molecular Mechanisms of Chaihu-Shugan-San in Treatment of Breast Cancer Based on Network Pharmacology. Evid Based Complement Alternat Med. 2020;2020:3670309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Lee YW, Chen TL, Shih YR, Tsai CL, Chang CC, Liang HH, Tseng SH, Chien SC, Wang CC. Adjunctive traditional Chinese medicine therapy improves survival in patients with advanced breast cancer: a population-based study. Cancer. 2014;120:1338-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 27. | Wang Y, Li JW, Qin YN, Sun CP, Chen JJ, Ruan YY, Chen LX, Liu S, Liu GY. Clinical observation on the effect of Chinese medicine-"TCM formula" intervention on recurrence and metastasis of triple negative breast cancer. Complement Ther Med. 2020;52:102456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |