Published online Jan 16, 2024. doi: 10.12998/wjcc.v12.i2.418
Peer-review started: October 18, 2023
First decision: December 7, 2023
Revised: December 18, 2023
Accepted: December 26, 2023
Article in press: December 26, 2023
Published online: January 16, 2024
Processing time: 84 Days and 5.5 Hours
Acute carpal tunnel syndrome (ACTS) is commonly caused by repetitive strain, trauma, or inflammatory conditions. However, ACTS due to tophaceous gout is a clinical event that remains poorly understood and underreported. This rare manifestation necessitates prompt diagnosis and intervention to prevent irreversible complications.
A 51-year-old man who had poorly controlled hyperuricemia presented with ACTS secondary to tophaceous gout. Because of rapid symptom progression symptoms and severe median nerve compression within 3 mo, the patient underwent emergency decompression surgery for both wrists at different time points. Postoperatively, he exhibited complete recovery of sensory and motor functions, with no recurrence at long-term follow-up. Favorable outcomes were achieved through immediate decompression surgery, anti-inflammatory medica
Prompt surgical intervention and optimal gout management are crucial for preventing irreversible nerve damage and ACTS recurrence.
Core Tip: Acute carpal tunnel syndrome (ACTS) secondary to tophaceous gout is a rare but severe condition that necessitates immediate and comprehensive treatment. Prompt surgical decompression is crucial for alleviating symptoms and preventing irreversible nerve damage. In addition, effective postoperative management strategies involving anti-inflammatory medications and active and passive range-of-motion exercises are required for full recovery. The underlying gout condition must be managed through urate-lowering agents and lifestyle modifications to prevent the recurrence of ACTS and other gout-related complications. Our case report emphasizes the need for a multidisciplinary approach for successful treatment and recurrence prevention.
- Citation: Yeoh SC, Wu WT, Shih JT, Su WC, Yeh KT. Subsequent bilateral acute carpal tunnel syndrome due to tophaceous infiltration: A case report. World J Clin Cases 2024; 12(2): 418-424
- URL: https://www.wjgnet.com/2307-8960/full/v12/i2/418.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i2.418
Acute carpal tunnel syndrome (ACTS) is characterized by the compression of the median nerve as it passes through the carpal tunnel in the wrist, resulting in symptoms such as pain, numbness, and weakness in the affected hand[1]. Although the etiology of ACTS is multifactorial, ranging from repetitive strain to anatomical abnormalities, it is rarely induced by gout[2]. Gout is a metabolic disorder resulting from the deposition of monosodium urate crystals in and around the joints, typically affecting the lower extremities[3]. Tophi—the hallmark of chronic gout—are nodular urate crystal masses that can develop in soft tissues surrounding the joints[4]. The confluence of ACTS and gout is a unique clinical event that poses diagnostic and therapeutic challenges. The onset of ACTS secondary to gout is rare, with sporadic cases reported after 2000[2,4-8]. Herein, we report a rare case of ACTS due to tophaceous infiltration secondary to gout. The patient sequentially developed ACTS in both upper extremities within 3 mo. This case report is presented, and a literature review was conducted to elucidate the clinical characteristics, diagnostic challenges, and therapeutic strategies for managing ACTS secondary to tophaceous gout. We hope to offer valuable insights into this rare but significant complication of gout.
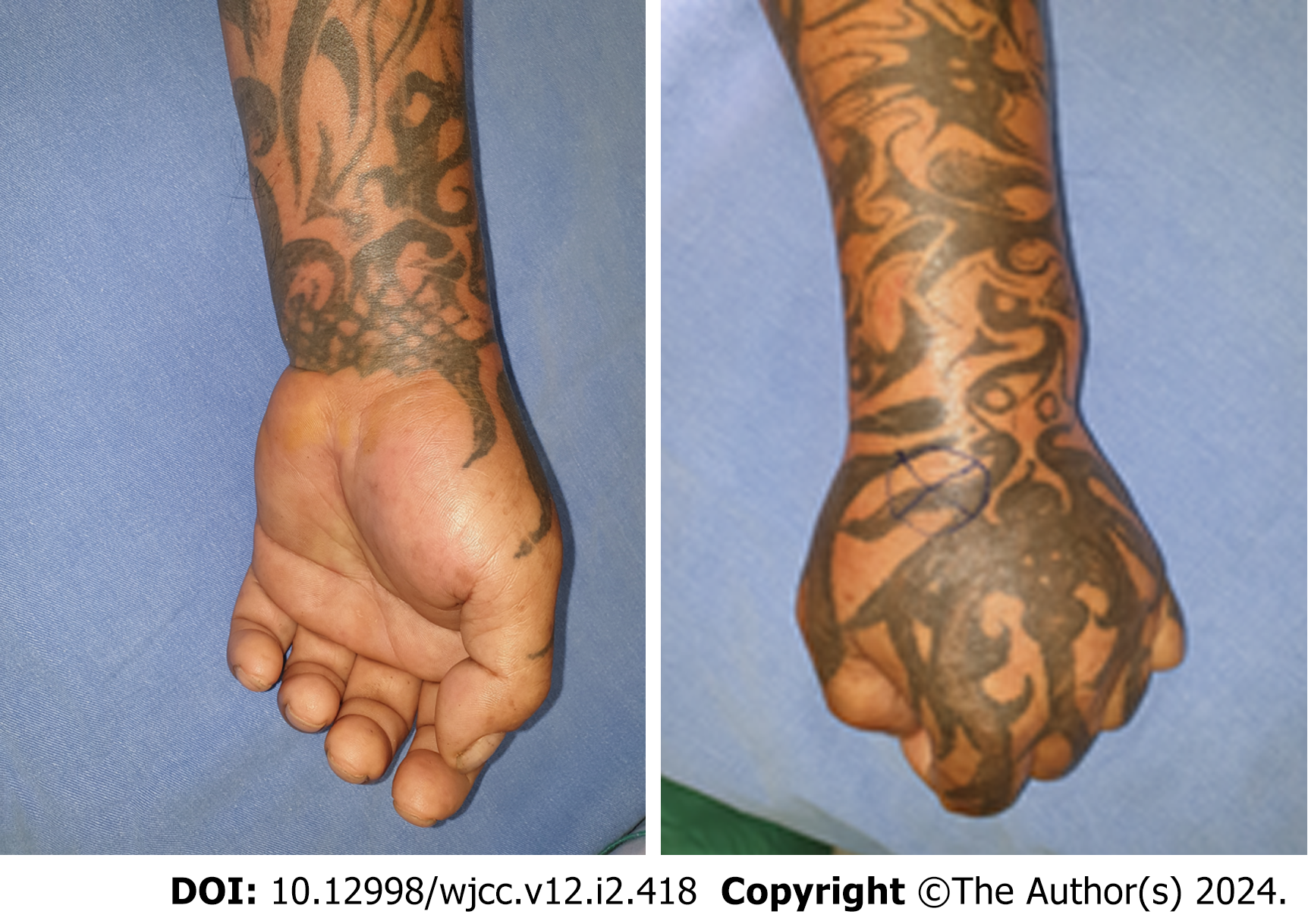
The 51-year-old man reported right wrist pain accompanied by severe swelling that extended to the right distal forearm (Figure 1). His symptoms started 24 h before presentation.
The patient reported right wrist pain accompanied by severe swelling that extended to the right distal forearm. His symptoms started 24 h before presentation. He also reported numbness and reduced range of motion (ROM) in his wrist and fingers. He denied any recent trauma or engaging in strenuous physical activity, drug abuse, or alcohol abuse. The administration of intravenous ketorolac acid 30mg and tramadol 100 mg did not alleviate his symptoms at all. Physical examination revealed that his right wrist was extremely tense and swollen, which was accompanied by severe tenderness, excruciating pain, and limited ROM due to extensive swelling. The patient also experienced severe numbness in his radial fingers and weakness in his thenar muscle.
The patient had a history of poorly controlled hyperuricemia and hypertension presented to our emergency department with severe pain in the right wrist. He was using a beta-blocker and calcium channel blocker for hypertension but had no history of anticoagulant use; his gout flare-ups were managed with a Cox-2-selective nonsteroidal anti-inflammatory drug.
The patient is a current smoker and frequently drinks beers. He has family history of gout.
Physical examination of the patient revealed that his right wrist was extremely tense and swollen, which was accompanied by severe tenderness, excruciating pain, and limited ROM due to extensive swelling. The patient also experienced severe numbness in his radial fingers and weakness in his thenar muscle.
Laboratory findings of the patient revealed leukocytosis and elevated levels of C-reactive protein and uric acid; however, no other abnormality was detected.
Wrist X-ray revealed no fracture or dislocation. The intravenous administration of nonsteroidal anti-inflammatory drugs and corticosteroids did not ameliorate his symptoms.
Orthopedic doctor was consulted for this situation and emergent decompression surgery for acute median nerve compression was suggested after discussion with the patient and his family.
ACTS of right upper limb, possibly gout-related.
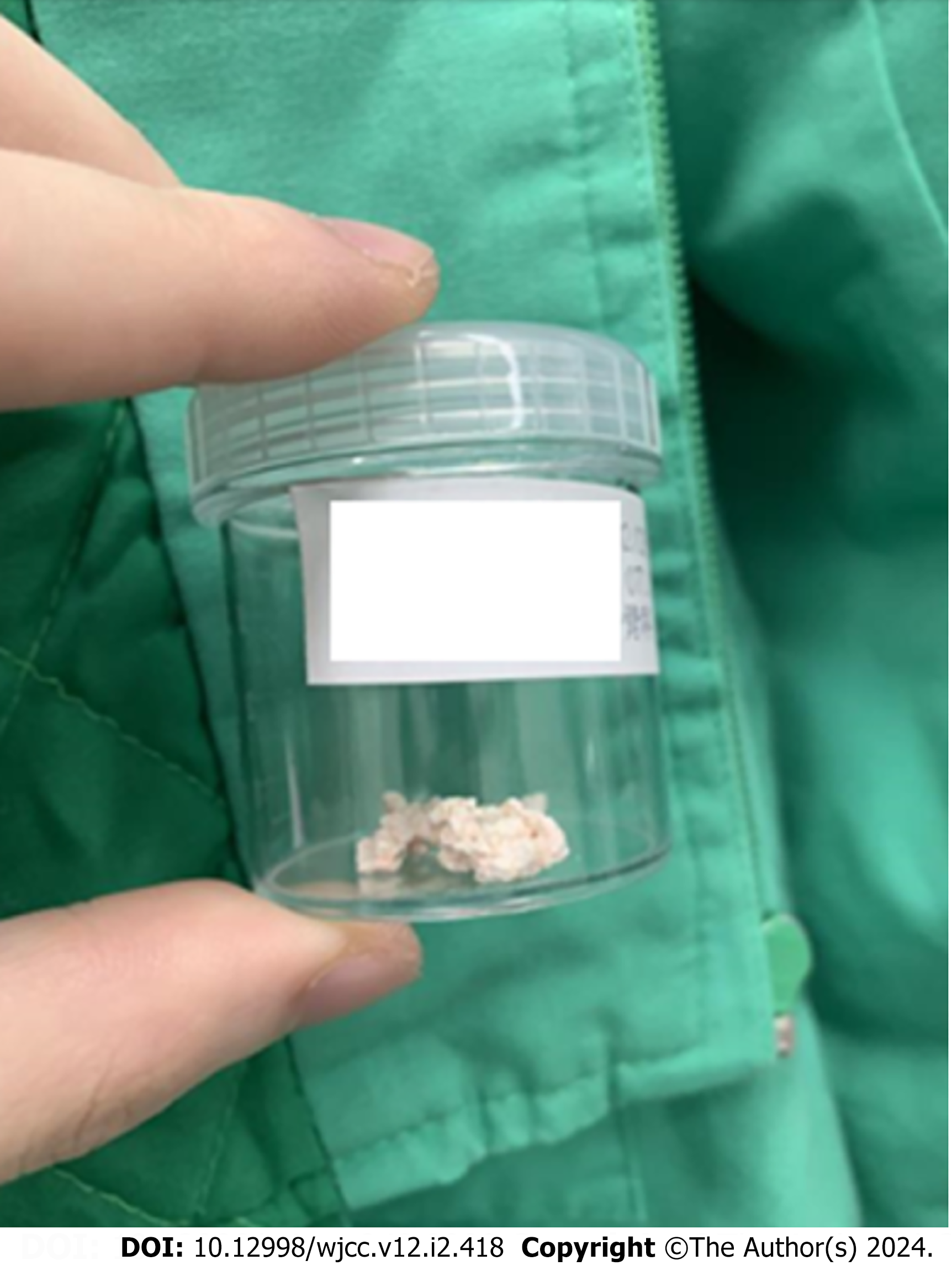
Rapid symptom deterioration prompted emergency decompression surgery; the carpal tunnel and volar compartment were decompressed within 24 h. Gout tophi were carefully removed during surgery, and no infection was detected. Postoperatively, the patient’s wrist swelling, and tenderness subsided, and his muscle weakness and numbness were mitigated. After 4 d, he was discharged from hospital with a prescription for etoricoxib and allopurinol, but he was subsequently lost to follow-up.
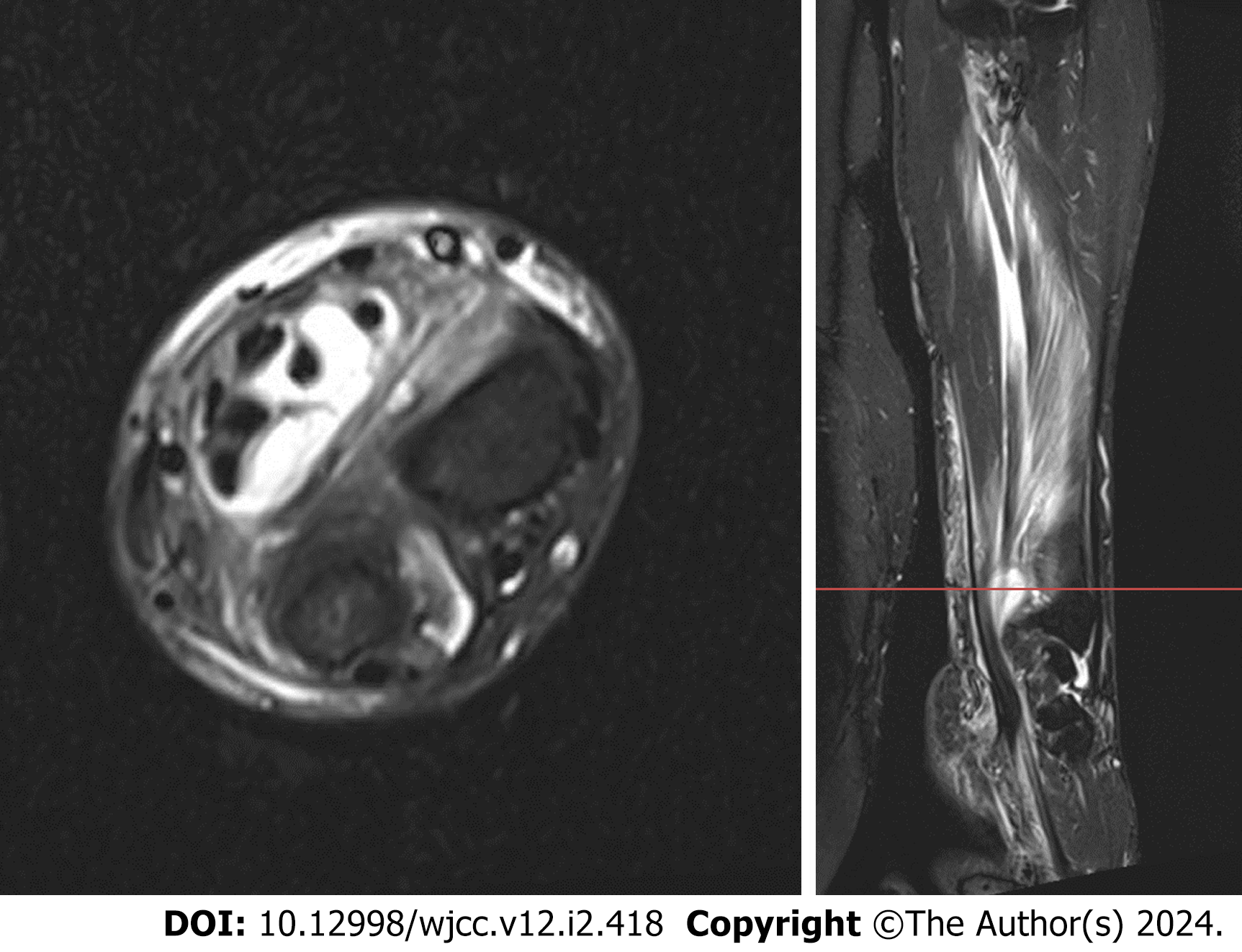
Two months after discharge, the patient presented with a similar clinical condition in his left forearm. Emergency magnetic resonance imaging revealed a collection of fluid within the flexor tendon sheath that extended to the carpal tunnel and Guyon canal (Figure 2). He underwent emergency decompression surgery, which included removing a gout tophus similar to the tophus that was previously removed (Figure 3). After decompression and profuse irrigation with normal saline, the around-wound skin was punctured multiple times with a 19-G needle and then closed in a single layer with 3-Nylon suture. We also placed a drain into the decompressed surgical site, which was retained for 5 days. Postoperatively, the patient’s symptoms were ameliorated, and he was discharged 36 h after surgery (Figure 4). Wrist splint protection was applied for 1 wk after surgery. For the next 6 wk, the patient engaged in active and passive ROM exercises with intermittent night splinting.
During the 12-mo postoperative follow-up period, the patient achieved favorable recovery of bilateral wrist function. He received allopurinol for persistent hyperuricemia control and etoricoxib for intermittent gout pain management. The patient resumed his daily life and work activities 6 wk after surgery. No adverse event occurred during the follow-up period.
We reported the case of a patient with ACTS secondary to tophaceous gout that was effectively managed through a multidisciplinary approach involving timely surgical decompression, pharmacologic anti-inflammatory interventions, immediate active and passive ROM exercises, and intermittent wrist splinting. ACTS induced by a gout flare-up represents a rare but critical clinical condition that may develop even in patients receiving standard urate-lowering therapies[2]. The co-occurrence of finger flexion deformity and carpal tunnel syndrome due to tophaceous deposits is an atypical manifestation of chronic gout, necessitating early differential diagnosis and urgent surgical intervention in the presence of symptoms[4-6]. Timely decompression surgery prevents irreversible nerve damage and alleviates flexor tendon rigidity[7]. Immediate surgical release may ensure long-term favorable outcomes, including the complete recovery of sensory and motor functions without the recurrence of ACTS[8]. The effective management of ACTS necessitates a comprehensive therapeutic strategy encompassing pharmacologic interventions such as urate-lowering agents (e.g., allopurinol), lifestyle modifications targeting modifiable risk factors, and patient education on the importance of treatment adherence and regular follow-up[8,9].
Very few studies have evaluated the efficacy of rehabilitation interventions or supervised rehabilitation after general surgery for carpal tunnel syndrome[10-12]. In their retrospective study, Mack et al[13] reported that patients who underwent surgery for carpal tunnel release and who reported fewer problems than did their counterparts exhibited favorable outcomes at only a single postoperative follow-up[13]. However, for patients with ACTS caused by gout infiltration, postoperative hand therapy may be necessary, although challenging, because of local inflammation, joint stiffness, and pain exacerbated by gout crystals. Active and passive ROM exercises should be initiated soon after surgery to prevent joint stiffness and adhesion formation[14]. Sensory re-education programs[15] and neural gliding exercises[16] may accelerate neural recovery. Shalimar et al[17] revealed that wrist splinting after limited open carpal tunnel release may not facilitate recovery during the immediate postoperative period[17]. However, adequate intermittent splinting after release surgery for ACTS secondary to tophaceous infiltration may prevent aggravated inflammation. Furthermore, functional rehabilitation interventions, which are often tailored to patients, may accelerate return to daily activities[14]. Future studies should focus on establishing evidence-based guidelines for postoperative hand therapy tailored to patients with ACTS secondary to tophaceous gout.
We performed preoperative ultrasound and dual-energy computed tomography (DECT) due to the urgent need for surgical decompression of the median nerve in the present patient. However, the sense of urgency raises questions regarding the role diagnostic imaging in cases involving gout tophi–induced ACTS. A preemptive diagnosis may be pivotal for a targeted surgical approach. The literature provides insights into the multifaceted presentation of wrist gout. Wilczynski et al[18] highlighted that wrist gout is frequently accompanied by diffuse synovitis and crystalline deposition and is often associated with ligament incompetence and scapholunate advanced collapse[18]. This finding suggests that a comprehensive wrist arthroscopy is necessary in similar cases to evaluate the intra-articular manifestations of gout. Klauser et al[19] and Cipolletta et al[20] emphasized the diagnostic power of ultrasonography. Klauser et al[19] identified the double contour sign in ultrasonography to be a highly sensitive indicator of intra-articular gout; therefore, ultrasonography may serve as a first-line diagnostic tool[19]. Cipolletta et al[20] indicated that a targeted ultrasonography has excellent diagnostic accuracy, surpassing that of approaches evaluating only the most clinically affected joint[20]. The aforementioned studies collectively suggest that ultrasonography is a rapid, noninvasive diagnostic tool that is particularly useful in emergency settings. However, the role of DECT, particularly in identifying extra-articular urate deposits, should not be disregarded. Our case underscores the need for future studies to establish a robust diagnostic algorithm that incorporates both ultrasound and DECT modalities for patients suspected of having ACTS secondary to tophaceous gout. Such an algorithm will allow for targeted therapeutic strategies, potentially averting the need for emergency surgery.
Although multiple relevant cases have been reported, our report offers additional novel insights in several key areas. First, it provides a comprehensive treatment approach integrating immediate surgical intervention with a specific postoperative management plan, which includes targeted anti-inflammatory medications, regimented active and passive ROM exercises, and intermittent wrist splinting, thereby offering holistic patient care from initial surgery to full recovery. Second, this report provides an in-depth documentation of the present patient’s long-term follow-up, highlighting treatment efficacy over an extended period—an aspect often underreported in the literature. Third, our report emphasizes the importance of managing an underlying gout condition to prevent recurrence, focusing on medication adherence and lifestyle modifications. This preventive strategy adds critical depth to the current understanding of ACTS management in patients with gout. Fourth, we quantitatively measured the recovery of sensory and motor functions, offering objective data that supplement the typically subjective reports in the literature. Finally, the report highlights the diagnostic challenges and the need for high clinical suspicion in cases where the typical causes of ACTS are not apparent, thereby aiding clinicians in making informed decisions in similar cases in the future. This case report presents certain limitations. Firstly, its findings are derived from the experience of a single patient, limiting their generalizability, and the unique characteristics of the patient, along with the specific treatment approach, may not be universally applicable across various clinical settings or populations. Secondly, sonographic examinations were not conducted due to the emergent nature of the symptomatic conditions. Thirdly, a more extended follow-up period in future studies could yield a deeper understanding of the long-term outcomes and recurrence rates associated with this pathology. Despite these limitations, our report contributes a unique perspective by integrating a comprehensive treatment approach, extensive follow-up, preventive strategies, quantitative assessments, and an understanding of diagnostic challenges, thereby enhancing the existing body of literature on this pathological condition.
The present case report highlights the importance of considering gout as a potential cause of tophaceous infiltration–induced ACTS in patients with poorly controlled hyperuricemia. Early diagnosis of this condition, timely implementation of surgical interventions, and prompt initiation of adequate postoperative hand rehabilitation programs are crucial for patient recovery. It also highlights the need for a multidisciplinary approach and patient education programs to manage underlying gout, potentially shaping evidence-based clinical guidelines and stimulating broader investigative studies.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gica N, Romania S-Editor: Li L L-Editor: A P-Editor: Cai YX
| 1. | Holbrook HS, Hillesheim RA, Weller WJ. Acute Carpal Tunnel Syndrome and Median Nerve Neurapraxia: A Review. Orthop Clin North Am. 2022;53:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 2. | Carr L, Brooke S, Ingraham J. Medically managed gout precipitating acute carpal tunnel syndrome. Hand (N Y). 2015;10:574-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Weaver JS, Vina ER, Munk PL, Klauser AS, Elifritz JM, Taljanovic MS. Gouty Arthropathy: Review of Clinical Manifestations and Treatment, with Emphasis on Imaging. J Clin Med. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Sakti M, Usman MA, Lee J, Benjamin M, Maulidiah Q. Atypical musculoskeletal manifestations of gout in hyperuricemia patients. Open Access Rheumatol. 2019;11:47-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Mak KCJ, IP FK, Wong TC, Wan SH, Chan SY. Carpal tunnel syndrome caused by gout: clinical presentations, surgical findings, and outcomes after surgery. J Orthop Trauma Rehabil. 2015;19:15-20. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Rand B, McBride TJ, Dias RG. Combined triggering at the wrist and severe carpal tunnel syndrome caused by gouty infiltration of a flexor tendon. J Hand Surg Eur Vol. 2010;35:240-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Kim HS. Carpal tunnel syndrome caused by tophaceous gout. Korean J Intern Med. 2014;29:544-545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Buruian A, Peixoto D, Ângelo S, Carvalho A, Mendes A, Pereira C. Acute Carpal Tunnel Syndrome Secondary to Gout Flare and Outcomes at 18 Months After Open Carpal Tunnel Decompression. J Hand Surg Glob Online. 2022;4:244-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Ragab G, Elshahaly M, Bardin T. Gout: An old disease in new perspective - A review. J Adv Res. 2017;8:495-511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 299] [Cited by in RCA: 307] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 10. | Peters S, Page MJ, Coppieters MW, Ross M, Johnston V. Rehabilitation following carpal tunnel release. Cochrane Database Syst Rev. 2016;2:CD004158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Gil JA, Weiss B, Kleiner J, Akelman E, Weiss AC. A Prospective Evaluation of the Effect of Supervised Hand Therapy After Carpal Tunnel Surgery. Hand (N Y). 2020;15:315-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Cantero-Téllez R, Naughton N, Algar L, Valdes K. Linking hand therapy outcome measures used after carpal tunnel release to the International Classification of Functioning, Disability and Health: A systematic review. J Hand Ther. 2019;32:233-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Mack EM, Callinan NJ, Reams M, Bohn DC, Chmielewski TL. Patient-reported outcomes after open carpal tunnel release using a standard protocol with 1 hand therapy visit. J Hand Ther. 2017;30:58-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Newington L, Brooks C, Warwick D, Adams J, Walker-Bone K. Return to work after carpal tunnel release surgery: a qualitative interview study. BMC Musculoskelet Disord. 2019;20:242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 15. | Jerosch-Herold C, Shepstone L, Miller L. Sensory relearning after surgical treatment for carpal tunnel syndrome: a pilot clinical trial. Muscle Nerve. 2012;46:885-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Tamaru Y, Yanagawa A, Matsugi A. Sensory Nerve Conduction Velocity Predicts Improvement of Hand Function with Nerve Gliding Exercise Following Carpal Tunnel Release Surgery. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Shalimar A, Nor-Hazla MH, Arifaizad A, Jamari S. Splinting after Carpal Tunnel Release: Does it really Matter? Malays Orthop J. 2015;9:41-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Wilczynski MC, Gelberman RH, Adams A, Goldfarb CA. Arthroscopic findings in gout of the wrist. J Hand Surg Am. 2009;34:244-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Klauser AS, Halpern EJ, Strobl S, Abd Ellah MMH, Gruber J, Bellmann-Weiler R, Auer T, Feuchtner G, Jaschke W. Gout of hand and wrist: the value of US as compared with DECT. Eur Radiol. 2018;28:4174-4181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 20. | Cipolletta E, Filippucci E, Abhishek A, Di Battista J, Smerilli G, Di Carlo M, Silveri F, De Angelis R, Salaffi F, Grassi W, Di Matteo A. In patients with acute mono/oligoarthritis, a targeted ultrasound scanning protocol shows great accuracy for the diagnosis of gout and CPPD. Rheumatology (Oxford). 2023;62:1493-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |