Published online Jan 16, 2024. doi: 10.12998/wjcc.v12.i2.392
Peer-review started: September 20, 2023
First decision: November 20, 2023
Revised: December 2, 2023
Accepted: December 22, 2023
Article in press: December 22, 2023
Published online: January 16, 2024
Processing time: 112 Days and 22.7 Hours
Multiple primary cancers are rare occurrences that can involve either metachro
On December 30, 2014, a 51-year-old Chinese man was admitted to our hospital with complaints of intermittent painless gross hematuria for the preceding week. A computed tomography (CT) scan revealed wall thickening in the left ureter’s upper segment, while a CT urography revealed a left renal pelvis tumor. A successful laparoscopic radical resection of the left renal pelvis tumor was subsequently performed at Shanghai Zhongshan Hospital in January 2015. The pathological findings after the surgery revealed a low-grade papillary urothelial carcinoma of the renal pelvis. The final pathological tumor stage was pT1N0M0. After surgery, this patient received 6 cycles of intravenous chemotherapy with gemcitabine and carboplatin, as well as bladder infusion therapy with gemcitabine. On December 18, 2017, the patient was admitted once again to our hospital with a one-day history of painless gross hematuria. A CT scan showed the presence of a space-occupying lesion on the posterior wall of bladder. Cystoscopic examination revealed multiple tumors in the bladder and right cutaneous ureterostomy was performed under general anesthesia on December 29, 2017. The postoperative pathological findings disclosed multifocal papillary urothelial carcinoma of the bladder (maximum size 3.7 cm × 2.6 cm). The bladder cancer was considered a metastasis of the renal pelvis cancer after surgery. The pathological tumor stage was pT1N0M1. The patient refused chemotherapy after surgery. After another six years, the patient returned on February 28, 2023, complaining of periumbilical pain that had lasted six days. This time, a CT scan of the abdomen showed a tumor in the ascending colon, but a subsequent colonoscopy examination indicated a tumor in the descending colon. On March 12, 2023, a subtotal colectomy and an ileosigmoidal anastomosis were carried out under general anesthesia. Postoperative pathological findings revealed that all three tumors were adenocarcinomas. The final pathological tumor stage was pT3N0M0. The patient had an uneventful postoperative recovery and was discharged without complications.
The case of this elderly man presents a rare occurrence of metachronous primary cancers in the renal pelvis and colon. Bladder cancer is considered a metastasis of renal pelvis cancer after surgery. Optimal treatment can be implemented by evaluating the patient’s histological features, clinical history, and tumor distribution correctly.
Core Tip: In this report, we present a case study of an elderly man who was diagnosed with three heterochronous cancers in the renal pelvis, bladder, and colon. The case of this elderly man presents a rare occurrence of metachronous primary cancers in the renal pelvis and colon. The bladder cancer is considered to be metastasis of renal pelvis cancer after operation. Optimal treatment can be implemented by evaluating the patient’s histological features, clinical history, and tumor distribution correctly.
- Citation: Chen J, Huang HY, Zhou HC, Liu LX, Kong CF, Zhou Q, Fei JM, Zhu YM, Liu H, Tang YC, Zhou CZ. Three cancers in the renal pelvis, bladder, and colon: A case report. World J Clin Cases 2024; 12(2): 392-398
- URL: https://www.wjgnet.com/2307-8960/full/v12/i2/392.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i2.392
The occurrence of multiple primary cancers (MPCs) was originally described by Billroth in 1889 as the development of two or more tumors in a single individual with varied histological characteristics and originating from different body parts, each with their own metastatic deposits. MPCs are classified into two groups, namely synchronous and metachronous[1]. Metachronous MPCs manifest as cancers occurring six months or more after the first primary cancer[2,3]. Most MPCs manifest as double primary cancers, while triple primary cancers are extremely rare. This article describes an unusual case of metachronous primary cancers involving the urinary system and digestive system in a single patient.
A 51-year-old male Chinese citizen was admitted to our hospital on December 30, 2014, with intermittent painless gross hematuria.
The patient’s symptoms began one week earlier when he experienced intermittent painless gross hematuria.
The patient had been diagnosed with liver cysts and gallbladder stones, but had no history of surgery.
The patient had no family history of cancer.
Upon hospitalization, the patient’s vital signs were stable. The patient’s temperature was 36.7 °C, the heart rate was 90 beats per minute, the respiratory rate was 20 breaths per minute, the blood pressure was 162/96 mmHg, and the oxygen saturation in room air was 100%. A physical examination did not reveal any pathological signs.
Routine laboratory testing showed an elevation of urinary protein (1+), urinary occult blood (3+), urinary red blood cells (374/μL), and urinary white blood cells (29/μL). Other laboratory test results, including tumor markers, were within normal limits.
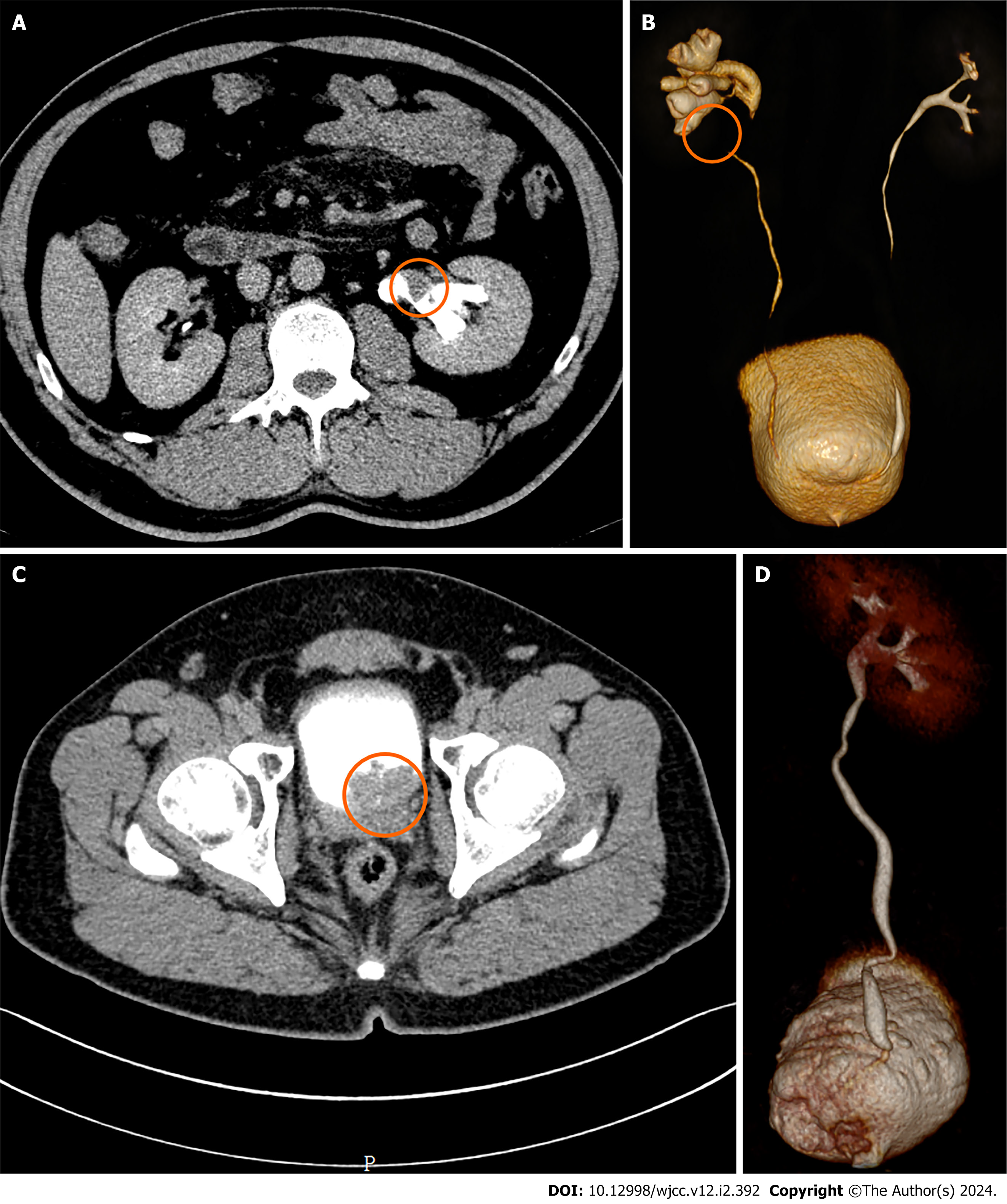
A computed tomography (CT) scan of the abdomen yielded results indicating local wall thickening in the upper segment of the left ureter. CT urography (CTU) revealed a tumor involving the left renal pelvis (Figure 1A and B). Surgery was advised, but the patient requested a transfer to Shanghai Zhongshan Hospital. Laparoscopic radical resection of the left renal pelvis tumor was performed under general anesthesia in January 2015, after excluding surgical contraindications and the surgery was successful. The postoperative pathological findings revealed urothelial carcinoma of the renal pelvis.
The patient recovered without complications after surgery and was discharged from Shanghai Zhongshan Hospital. The pathological findings revealed a noninvasive low-grade papillary urothelial carcinoma of the renal pelvis. The final pathological tumor stage was pT1N0M0. After surgery, this patient received 6 cycles of intravenous chemotherapy with gemcitabine and carboplatin, as well as bladder infusion therapy with gemcitabine. Regular outpatient follow-up appointments at our hospital were scheduled in order to detect any recurrence.
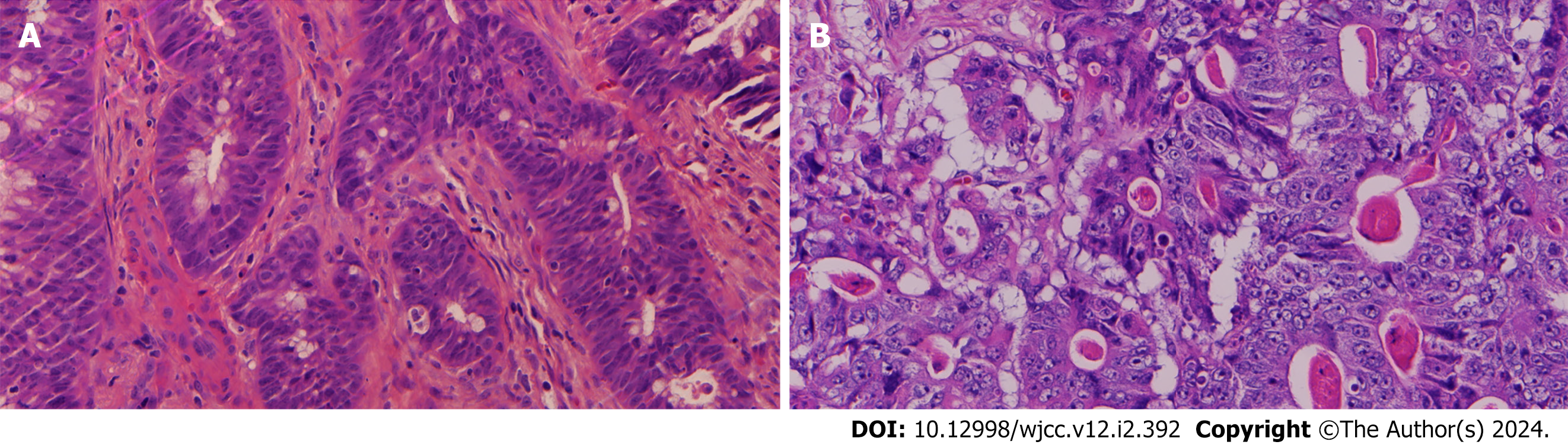
Three years later, on December 18, 2017, the patient was readmitted to our hospital because of painless gross hematuria lasting for one day. Routine laboratory tests showed an elevation of urinary protein (1+), urinary occult blood (2+), and urinary red blood cells (133/μL). A CT scan of the abdomen showed a space-occupying lesion on the posterior wall of the bladder. A CTU revealed a filling defect from the bladder (Figure 1C and D). Cystoscopic examination revealed a tumor on the left wall of the bladder, adjacent to the right ureteral opening and the specimen was biopsied. The pathological result was urothelial carcinoma (Figure 2). On December 29, 2017, laparoscopic total cystectomy and right cutaneous ureterostomy were performed after excluding surgical contraindications. The patient was placed under general anesthesia and the surgery was successful. The postoperative pathological findings revealed papillary urothelial carcinoma of the bladder (multifocal, maximum 3.7 cm × 2.6 cm) (Figure 2). The bladder cancer was considered a metastasis of the renal pelvis cancer after surgery. The pathological tumor stage was pT1N0M1. The patient refused postoperative chemotherapy.
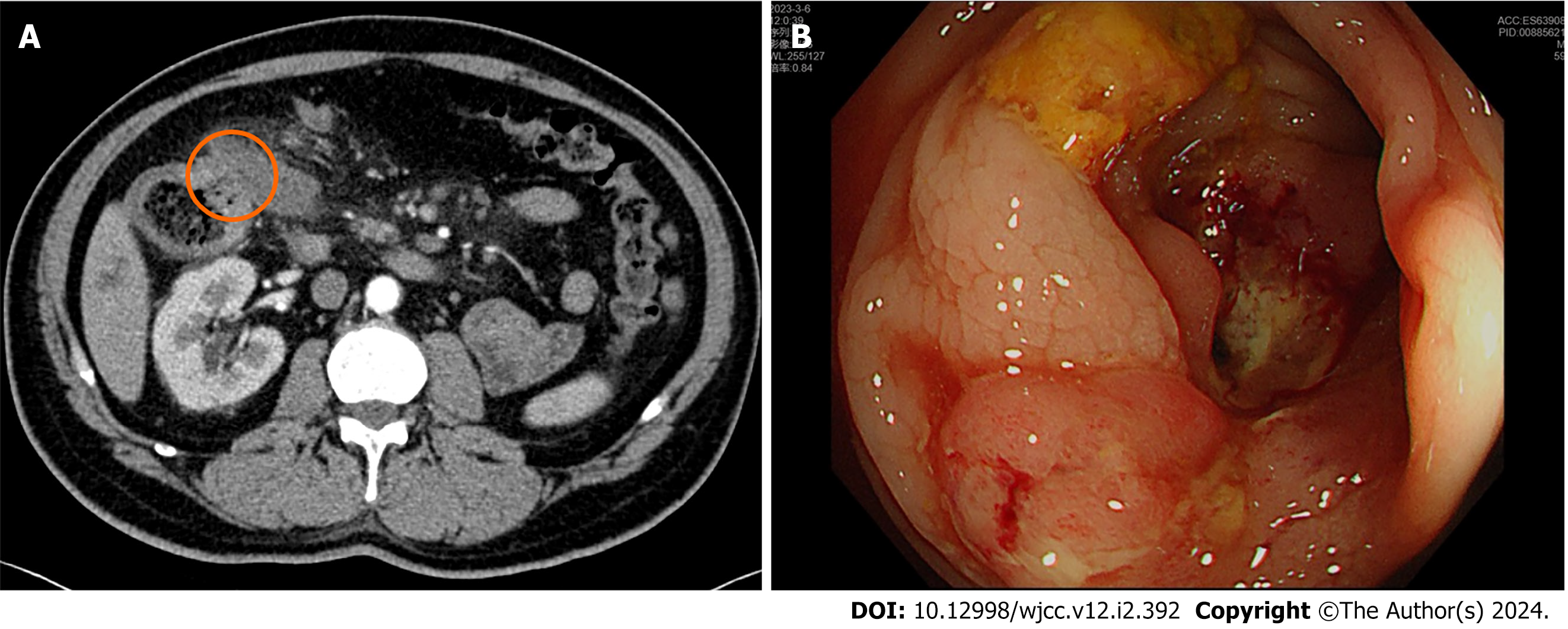
After six years, on February 28, 2023, the patient was readmitted to our hospital due to periumbilical pain over six days. A CT scan of the abdomen showed a tumor of the ascending colon. Colonoscopy examination, on the other hand, suggested a tumor in the descending colon (Figure 3). The pathological result of the colonoscopic biopsy specimen was adenocarcinoma of the descending colon (Figure 4). The contraindication for surgery was removed. On March 12, 2023, a subtotal colectomy and an ileosigmoidal anastomosis were performed under general anesthesia, and the operation was successful. The length of the colon removed was 65 cm. Three tumors were detected on the excised colon; one was 2 cm away from the distal margin and had a size of 3.5 cm × 2.5 cm, the other was adjacent to the ileocecal region and had a size of 2 cm × 2 cm, and the final tumor was 11 cm away from the proximal margin and had a size of 5.5 cm × 3.5 cm. All three tumors were recognized as adenocarcinoma based on the postoperative pathological findings (Figure 4). The final pathological tumor stage was pT3N0M0. The patient recovered smoothly after the operation and was discharged without any complications.
The patient’s final diagnosis revealed that he had three types of carcinoma, namely, renal pelvis cancer, bladder cancer, and colon cancer.
After conducting a thorough preoperative evaluation and finding no surgical contraindications, we performed three surgeries on the patient. However, after a discussion involving with the entire hospital’s multidisciplinary team, and after considering the fact that the patient had only one kidney and the renal impact of chemotherapy, chemotherapy was deemed temporarily unsuitable for this patient.
The patient was not provided with any adjuvant therapy and after an uneventful recovery, he was discharged without any complications. A follow-up one month later showed no evidence of tumor recurrence.
Although MPCs are a rare occurrence, it is crucial to consider and exclude the possibility of metastasis from another cancer[4,5]. To distinguish between MPCs and metastatic tumors, several essential points should be accounted for. These include identifying each cancer as malignant through a histologic evaluation, as well as ensuring that each cancer is both geographically separate and distinct. Finally, the possibility of metastasis must be eliminated[6,7]. Additionally, tumors should be considered as MPCs when the first primary tumor presents without relapse.
Regarding the occurrence of bladder metastasis after primary renal pelvis cancer resection, it has been found that this incidence ranges from 13% to 35.7%[8,9]. The differentiation between primary and metastatic bladder cancer can be a challenge, and there are two proposed mechanisms for the occurrence of these cancers[10,11]. These include the monoclonal hypothesis, where a single genetic tumor cell causes tumors to emerge in different areas of the urinary tract. Alternatively, the regional canceration hypothesis proposes that exposure to carcinogens leads to synchronous and metachronous occurrences of unrelated tumors in various parts of the urinary tract.
In our case report, the patient was found to have bladder cancer three years after undergoing radical nephrectomy. The cancer showed evidence of multifocal growth and local interstitial invasion. However, there were no findings indicating any metastasis of cancer cells in the peripheral lymph nodes. While there are reports that the postsurgical metastasis of bladder cancer from renal pelvis cancer usually occurs within two years, the thin walls of the renal pelvis and ureter, surrounded by abundant lymphatic drainage, make lymphatic infiltration in renal pelvis cancer a crucial factor in bladder metastasis. Based on the information presented in this case, the renal pelvis and bladder cancers were dependent on one another, constituting a case of metastasis.
The incidence of dual primary cancer concurrent colorectal with cancer has been found to be between 5% and 17%, with the most common site of onset being the rectum and right colon[12-15]. Double primary cancer patients with concomitant colorectal cancer have a higher incidence of microsatellite instability-high (MSI-H) when compared with single colorectal cancer[16]. In clinical practice, nearly 15% of colorectal cancers are caused by MSI resulting from mismatch repair (MMR) gene mutations. The MMR gene encodes four primary proteins, including Mut-S homolog 2 (MSH2), MSH6, Mut-L homolog 1 (MLH1), and postmeiotic segregation increased 2 (PMS2). If two or more of these proteins are not present, the cancer is MSI-H[17,18].
In our case report, colon cancer was discovered in a patient five years after radical surgery for bladder cancer. The colon cancer was classified as adenocarcinoma and was noted for its ulcerative growth accompanied by infiltration into the subserosa. No metastasis of cancer cells in the peri-intestinal lymph nodes was discovered. According to the diagnostic criteria for MPC, the colon cancer was a metachronous primary cancer. We determined the expression of MSH2, MSH6, MLH1, and PMS2 in carcinoma by immunohistochemical staining. The results were as follows: MSH2 (+), MSH6 (+), MLH1 (-), and PMS2 (-). The stable state of microsatellites can determine the prognosis of patients with MSI-H. Usually, these patients have a good prognosis. The MSI test can only be conducted through next generation sequencing and this patient has not had such testing, so the patient’s prognosis is not very clear.
The preoperative examination of the present patient revealed two tumors in the colon, and an additional tumor was discovered during the surgery. Thus, performing an adequate preoperative examination and a careful intraoperative exploration can prevent a missed diagnosis. Early detection of MPCs can greatly improve patient survival rates and quality of life.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gofrit O, Israel S-Editor: Wang JJ L-Editor: A P-Editor: Li X
| 1. | López ML, Lana A, Díaz S, Folgueras MV, Sánchez L, Comendador MA, Belyakova E, Rodríguez JM, Cueto A. Multiple primary cancer: an increasing health problem. Strategies for prevention in cancer survivors. Eur J Cancer Care (Engl). 2009;18:598-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Kim C, Chon H, Kang B, Kim K, Jeung HC, Chung H, Noh S, Rha S. Prediction of metachronous multiple primary cancers following the curative resection of gastric cancer. BMC Cancer. 2013;13:394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Sun LC, Tai YY, Liao SM, Lin TY, Shih YL, Chang SF, Huang CW, Chan HM, Huang CJ, Wang JY. Clinical characteristics of second primary cancer in colorectal cancer patients: the impact of colorectal cancer or other second cancer occurring first. World J Surg Oncol. 2014;12:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Feng Y, Zhong M, Zeng S, Xiao D, Liu Y. Metachronous triple primary neoplasms with primary prostate cancer, lung cancer, and colon cancer: A case report. Medicine (Baltimore). 2018;97:e11332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Jiang W, Mao Q, Wu X, Yu W, Chen D. Laparoscopic radical resection of gastric cancer and metachronous colon cancer-a case report. Transl Cancer Res. 2020;9:2053-2059. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Rovatti M, Gerosa E, Turi V, D'Abrosca F, De Cesare F. [Multiple primary malignant neoplasms]. Minerva Chir. 1995;50:949-958. [PubMed] |
| 7. | Kojima S, Sakamoto T, Nagai Y, Honda M, Ogawa F. Metachronous rectal metastasis from primary transverse colon cancer: a case report. Surg Case Rep. 2018;4:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Tan LB, Chang LL, Cheng KI, Huang CH, Kwan AL. Transitional cell carcinomas of the renal pelvis and the ureter: comparative demographic characteristics, pathological grade and stage and 5-year survival in a Taiwanese population. BJU Int. 2009;103:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Saika T, Nishiguchi J, Tsushima T, Nasu Y, Nagai A, Miyaji Y, Maki Y, Akaeda T, Saegusa M, Kumon H; Okayama Urogenital Cancer Collaborating Group (OUCCG). Comparative study of ureteral stripping versus open ureterectomy for nephroureterectomy in patients with transitional carcinoma of the renal pelvis. Urology. 2004;63:848-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Hafner C, Knuechel R, Stoehr R, Hartmann A. Clonality of multifocal urothelial carcinomas: 10 years of molecular genetic studies. Int J Cancer. 2002;101:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 135] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Takahashi T, Habuchi T, Kakehi Y, Mitsumori K, Akao T, Terachi T, Yoshida O. Clonal and chronological genetic analysis of multifocal cancers of the bladder and upper urinary tract. Cancer Res. 1998;58:5835-5841. [PubMed] |
| 12. | Ueno M, Muto T, Oya M, Ota H, Azekura K, Yamaguchi T. Multiple primary cancer: an experience at the Cancer Institute Hospital with special reference to colorectal cancer. Int J Clin Oncol. 2003;8:162-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 109] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Yamamoto S, Yoshimura K, Ri S, Fujita S, Akasu T, Moriya Y. The risk of multiple primary malignancies with colorectal carcinoma. Dis Colon Rectum. 2006;49:S30-S36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Kato T, Suzuki K, Muto Y, Sasaki J, Tsujinaka S, Kawamura YJ, Noda H, Horie H, Konishi F, Rikiyama T. Multiple primary malignancies involving primary sporadic colorectal cancer in Japan: incidence of gastric cancer with colorectal cancer patients may be higher than previously recognized. World J Surg Oncol. 2015;13:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Lee WS, Lee JN, Choi S, Jung M, Baek JH, Lee WK. Multiple primary malignancies involving colorectal cancer--clinical characteristics and prognosis with reference to surveillance. Langenbecks Arch Surg. 2010;395:359-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Li Q, Zhang B, Niu FN, Ye Q, Chen J, Fan XS. [Clinicopathological characteristics, MSI and K-ras gene mutations of double primary malignancies associated with colorectal cancer]. Zhonghua Yi Xue Za Zhi. 2020;100:301-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 17. | Picard E, Verschoor CP, Ma GW, Pawelec G. Relationships Between Immune Landscapes, Genetic Subtypes and Responses to Immunotherapy in Colorectal Cancer. Front Immunol. 2020;11:369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 346] [Article Influence: 69.2] [Reference Citation Analysis (0)] |
| 18. | Taieb J, Svrcek M, Cohen R, Basile D, Tougeron D, Phelip JM. Deficient mismatch repair/microsatellite unstable colorectal cancer: Diagnosis, prognosis and treatment. Eur J Cancer. 2022;175:136-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 144] [Article Influence: 48.0] [Reference Citation Analysis (0)] |