Published online Jan 16, 2024. doi: 10.12998/wjcc.v12.i2.361
Peer-review started: August 21, 2023
First decision: November 20, 2023
Revised: December 5, 2023
Accepted: December 26, 2023
Article in press: December 26, 2023
Published online: January 16, 2024
Processing time: 142 Days and 14.3 Hours
Low-grade appendiceal neoplasms (LAMN) are characterized by low incidence and atypical clinical presentations, often leading to misdiagnosis as acute or chronic appendicitis before surgery. The primary diagnostic tool for LAMN is abdominal computed tomography (CT) imaging. Surgical resection remains the cornerstone of LAMN management, necessitating en bloc tumor excision to mini
A 71-year-old male patient was admitted to our hospital with a pelvic space-occupying lesion detected 1 mo prior. Physical examination showed a soft abdo
LAMN is a rare disease that lacks specific clinical manifestations. Abdominal CT plays a crucial role in diagnosing LAMN, and laparoscopic surgery is a safe and effective diagnostic and therapeutic approach.
Core Tip: This study presents a case of asymptomatic low-grade appendiceal neoplasm (LAMN), highlighting the crucial role of abdominal computed tomography in its diagnosis. The early identification and treatment of LAMN are essential for mitigating the risk of pseudomyxoma peritonei and enhancing patient outcomes. Laparoscopic surgery is demonstrated to be a safe and effective diagnostic and therapeutic approach.
- Citation: Yao MQ, Jiang YP, Wang YY, Mou YP, Fan JX. Asymptomatic low-grade appendiceal mucinous neoplasm: A case report. World J Clin Cases 2024; 12(2): 361-366
- URL: https://www.wjgnet.com/2307-8960/full/v12/i2/361.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i2.361
Appendiceal mucinous neoplasm (AMN) is a rare disease detected in less than 0.3% of appendectomy specimens and accounts for approximately 1% of gastrointestinal tumors[1]. In 2016, the Peritoneal Surface Oncology Group International classified AMNs into low-grade appendiceal neoplasms (LAMN), high-grade appendiceal neoplasms, mucinous adenocarcinoma, and goblet cell carcinoid[2]. LAMN is the most common pathological AMN subtype. LAMN is defined as mucinous neoplasms with low-grade cytology and any of the following: loss of muscularis mucosae, submucosal fi
On April 15, 2023, a patient was admitted to our hospital because of a pelvic space-occupying lesion. The lesion was surgically resected on April 18, 2023, and postoperatively confirmed as LAMN. Here, we describe this case, along with a literature review.
A 71-year-old male patient was admitted to the hospital because of a pelvic space-occupying lesion detected 1 mo previously.
Examination revealed a cystic space-occupying lesion in the lower right abdomen. The patient had no fever, nausea/vomiting, abdominal pain, abdominal distension, hematemesis, or black stools.
The patient had a 10-year history of hypertension that was controlled with 80 mg/12.5 mg valsartan and hydro
He had a smoking history of approximately 20 cigarettes daily for 30 years and reported no alcohol consumption. There was no significant family medical history.
The patient was alert and oriented, and his mental status was unremarkable. There were no signs of enlarged or swollen superficial lymph nodes. Cardiac and pulmonary physical examination showed no apparent signs of abnormality. The patient’s abdomen was soft, without any tenderness or rebound, and there were no palpable masses. Physical exa
Laboratory tests following admission showed a white blood cell count of 6.0 × 109/L, red blood cell count of 4.78 × 1012/L, hemoglobin of 14.8 g/dL, platelet count of 234.0 × 109/L, and C-reactive protein concentration of 11.5 mg/L. The result of the fecal occult blood test was negative. Detection of tumor markers showed the following results: carcinoembryonic antigen, 10.83 ng/mL; CA72-4, 1.1 U/mL; and CA199, 5.1 kU/L.
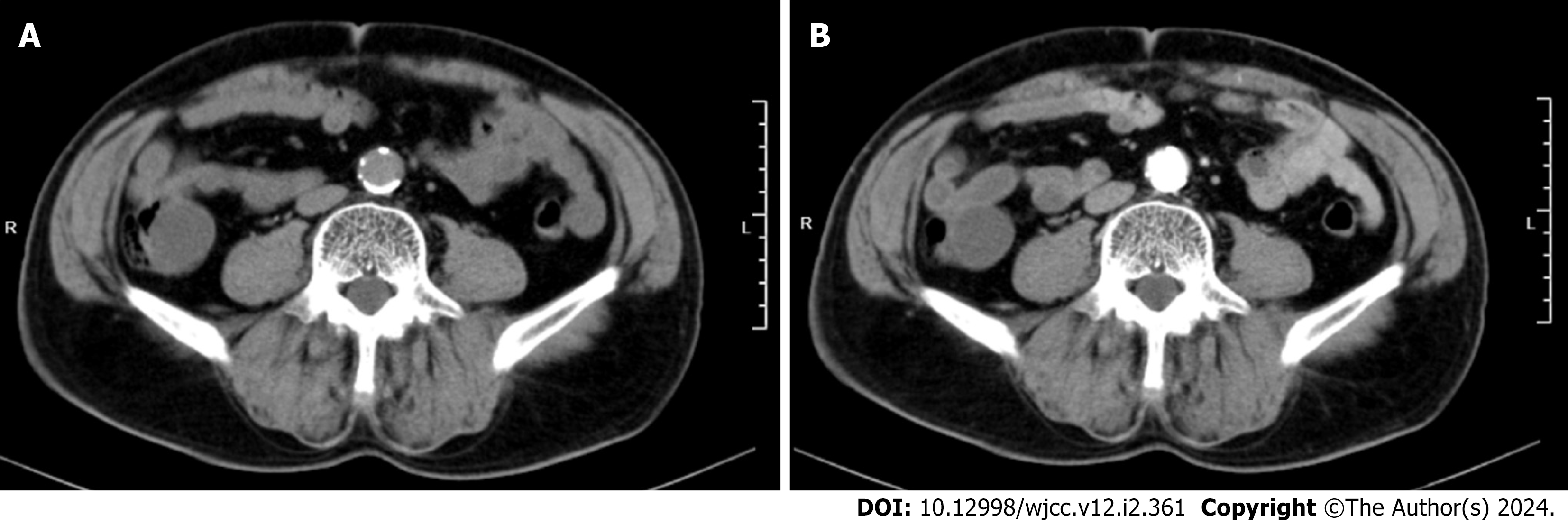
A raised mass with a smooth surface measuring 3.0 cm was observed in the cecum during enteroscopy (Figure 1). Abdominal contrast-enhanced computed tomography (CT) showed a markedly thickened and dilated appendix with visible cystic shadows. The appendix wall showed a slight enhancement following contrast enhancement (Figure 2).
The final diagnosis of LAMN was pathologically confirmed.
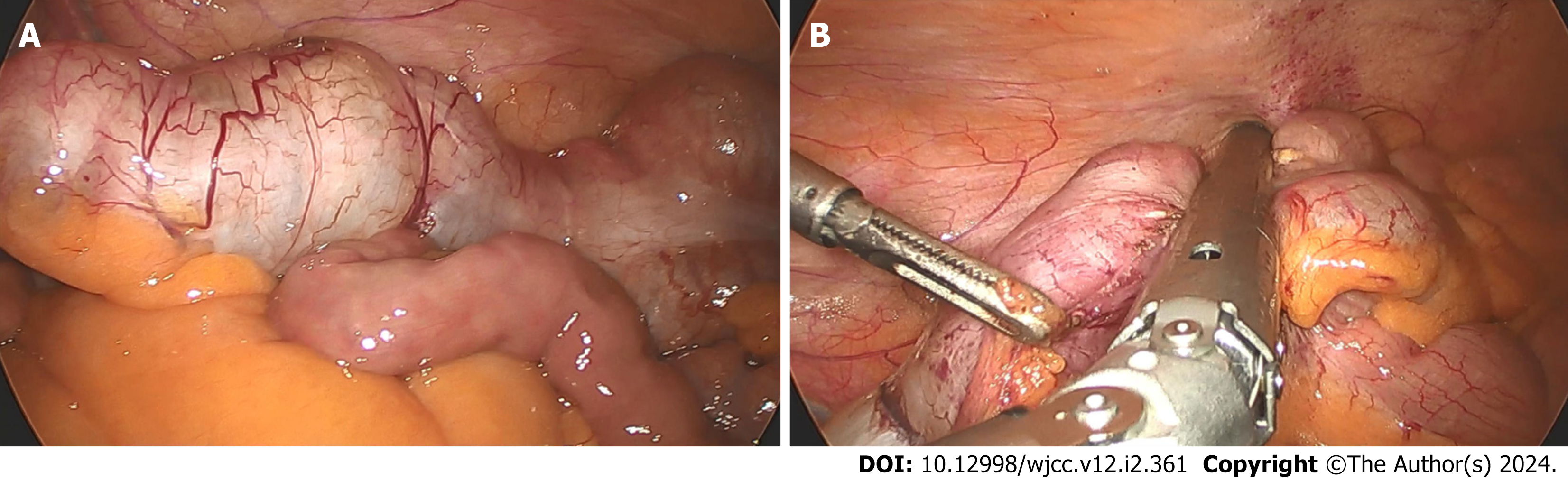
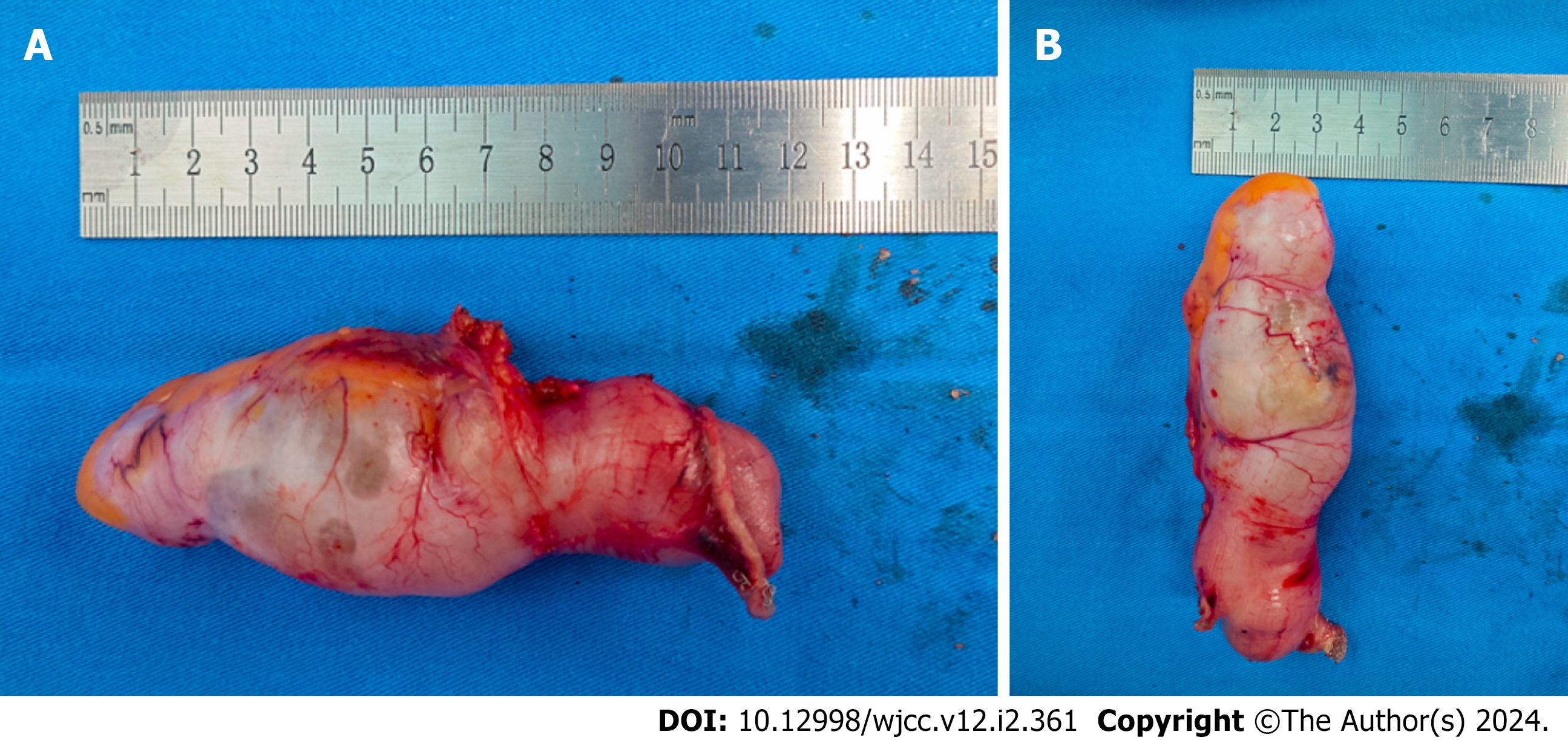
On the 3rd d of admission, laparoscopic surgery was performed and revealed a significantly dilated appendix (Figure 3A). A linear cutter/stapler was used to laparoscopically resect the appendix and portions of the cecum (Figure 3B). The appendix was 12 cm in length and 4 cm in width (Figure 4). Postoperative pathology confirmed that the tumor had in
The patient was discharged from our hospital on postoperative day 4 without experiencing any complications such as abdominal bleeding, intestinal obstruction, or incision infection. Routine blood tests, biochemical analyses, tumor marker assessments, and chest and abdominal CT scans were performed in an outpatient setting on November 20, 2023, revealing no evidence of recurrence.
Diagnosing LAMN is challenging because of its low incidence rate, atypical clinical features, lack of specific clinical symptoms, and absence of a specific tumor marker. The primary symptom of LAMN is pain in the lower right abdomen due to dilatation of the appendiceal lumen resulting from early-stage tumor growth. This may be mistaken for acute or chronic appendicitis before surgery[4]. Additional symptoms of LAMN include weight loss, nausea/vomiting, decreased appetite, and changes in bowel habits, which can lead to intestinal obstruction, intussusception, gastrointestinal he
Tumor rupture is the most serious and frequent complication of LAMN. It can cause the spread of tumor cells and mucinous ascites into the intraperitoneal cavity, which can result in pseudomyxoma peritonei (PMP)[7], a severe clinical syndrome with high morbidity and mortality. Therefore, early identification and treatment of LAMN is crucial in miti
Imaging is crucial for both LAMN diagnosis and treatment. AMNs are characterized by mucus accumulation and the "onion skin" sign on ultrasound[8]. LAMN is most commonly diagnosed through CT imaging, as it reveals two common features of LAMN: cystic dilation of the appendiceal lumen and irregular thickening of the appendiceal wall. Wall calcification may accompany the latter. Mucinous tissue typically does not reach the cecal lumen because of blockage in the appendiceal lumen. Colonoscopy may reveal a smooth elevated mass originating from the opening of the appendix, without any visible mucinous tumor tissue.
LAMN has the potential to become malignant, and rupture of the appendiceal wall can lead to PMP. Surgical resection is the primary treatment for LAMN, during which the tumor must be excised en bloc to minimize the risk of iatrogenic rupture. Ideally, LAMN lesions at different sites should be completely resected, ensuring negative surgical margins. Regional lymphadenectomy is not typically required[9]. For LAMNs found in the distal appendix, removal of the appen
LAMN is a rare disease that lacks specific clinical manifestations and is usually identified incidentally following appen
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wong Y, Taiwan S-Editor: Lin C L-Editor: Filipodia P-Editor: Xu ZH
| 1. | Ramaswamy V. Pathology of Mucinous Appendiceal Tumors and Pseudomyxoma Peritonei. Indian J Surg Oncol. 2016;7:258-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (2)] |
| 2. | Carr NJ, Cecil TD, Mohamed F, Sobin LH, Sugarbaker PH, González-Moreno S, Taflampas P, Chapman S, Moran BJ; Peritoneal Surface Oncology Group International. A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia: The Results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. Am J Surg Pathol. 2016;40:14-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 512] [Article Influence: 56.9] [Reference Citation Analysis (0)] |
| 3. | Al-Tarakji M, Ali SM, Shah AA, Petkar MA, Mirza S, Singh R, Zarour A. A Unique Case of Low-Grade Mucinous Neoplasm in Stump Appendectomy. Case Rep Surg. 2020;2020:8850403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Boshnaq M, Toeima M, Hamade A, Bagla N. Local Protocol for Management of Low-Grade Appendiceal Mucinous Neoplasm (LAMN). Indian J Surg Oncol. 2020;11:355-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Gonzalez HH, Herard K, Mijares MC. A Rare Case of Low-grade Appendiceal Mucinous Neoplasm: A Case Report. Cureus. 2019;11:e3980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Kwak HD, Ju JK. A prospective study of discrepancy between clinical and pathological diagnosis of appendiceal mucinous neoplasm. Ann Surg Treat Res. 2020;98:124-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Yamaguchi T, Murata K, Shiota T, Takeyama H, Noura S, Sakamoto K, Suto T, Takii Y, Nagasaki T, Takeda T, Fujii M, Kagawa Y, Mizushima T, Ohno Y, Yao T, Kishimoto M, Sugihara K; Study Group of Appendiceal Neoplasms in the JSCCR. Clinicopathological Characteristics of Low-Grade Appendiceal Mucinous Neoplasm. Dig Surg. 2021;38:222-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Xiao J, Li P, Liu W. Analysis of Clinical Characteristics of Low-Grade Appendiceal Mucinous Neoplasm (LAMN): A Retrospective Cohort Study of 51 LAMN Patients. J Invest Surg. 2021;34:721-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Wu YC, Wen L, Dou WD, Zhang JL, Wu T, Wang X. [Clinicopathological analysis and surgical strategy of primary appendiceal neoplasms]. Zhonghua Wei Chang Wai Ke Za Zhi. 2021;24:1065-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Qi XM, Sun P, Wan JY. Clinicopathologic analysis of low appendiceal mucinous neoplasm. Zhonghua Quanke Yishi Zazhi. 2016;15:871-874. |
| 11. | Han S, Li XW, Zhao PX, Guan TW, Li SY, Zhang DJ. Research progress on the diagnosis and treatment of low-grade appendiceal mucinous neoplasm. Zhonghua Jiepouyulinchuang Zazhi. 2019;24:512-515. |
| 12. | Chicago Consensus Working Group. The Chicago Consensus on Peritoneal Surface Malignancies: Management of Appendiceal Neoplasms. Ann Surg Oncol. 2020;27:1753-1760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 13. | Singh MK, Kumar MK, Singh R. Laparoscopic appendectomy for mucocele of the appendix. J Nat Sci Biol Med. 2014;5:204-206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |