Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.4016
Revised: April 24, 2024
Accepted: May 9, 2024
Published online: July 6, 2024
Processing time: 110 Days and 7.9 Hours
Venous air embolism (VAE) is a potentially lethal condition, with a reported incidence rate of about 0.13%, and the true incidence may be higher since many VAE are asymptomatic. The current treatments for VAE include Durant's man
A 53-year-old female patient with VAE presented to the emergency clinic due to abdominal pain with fever for 1 d and unconsciousness for 2 h. One day ago, the patient suffered from abdominal pain, fever, and diarrhea. She suddenly became unconscious after going to the toilet during the intravenous infusion of ciprofloxacin 2 h ago, accompanied by nausea and vomiting, during which a small amount of gastric contents were discharged. She was immediately sent to a local hospital, where cranial and chest computed tomography showed bilateral pneumonia as well as accumulated air visible in the right ventricle and pul
ECMO may be an important treatment for patients with VAE in critical condition.
Core Tip: This report demonstrates that in cases of obstructive shock due to venous air embolism, veno-arterial extracorporeal membrane oxygenation (VA-ECMO) can be a lifesaving intervention. It rapidly restores hemodynamic stability, providing critical support to the patient's circulatory system. The prompt recognition of the condition, the decision to utilize VA-ECMO are all crucial in ensuring a favorable outcome. In summary, this case report underscores the value of VA-ECMO as a therapeutic option in the management of obstructive shock due to venous air embolism, providing a valuable addition to the clinical knowledge and treatment strategies for this rare but potentially fatal condition.
- Citation: Zhu GW, Li YM, Yue WH, Sun JX, Zhou X, Xu YX, Wang HB, Zhang QH. Veno-arterial extracorporeal membrane oxygenation for the treatment of obstructive shock caused by venous air embolism: A case report. World J Clin Cases 2024; 12(19): 4016-4021
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/4016.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.4016
Venous air embolism (VAE) occurs when air enters the veins and eventually reaches the right ventricle. It is mostly caused by iatrogenic events and, rarely, trauma, during which a positive pressure difference between the site of vein breakage and the right atrium causes air to enter the venous system. VAE has a reported incidence rate of about 0.13%, although the true incidence may be higher since many VAE are asymptomatic[1]. The clinical manifestations of VAE are related to the location, volume, and velocity of air entry and the disease mainly affects the cardiovascular, respiratory, and central nervous systems. The main symptoms include dyspnea, chest tightness, chest pain, arrhythmias, seizures, loss of consciousness, altered mental status, and hemiplegia. The treatment strategies for VAE include: preventing further entry of air into the circulatory system; increasing the central venous pressure by rehydration; and Durant's maneuver[2]. For critically ill patients, cardiotropic drugs and cardiopulmonary resuscitation can be applied[1]. Recently, a patient with obstructive shock caused by VAE was successfully salvaged in our center using veno-arterial extracorporeal membrane oxygenation (VA-ECMO). After two days of VA-ECMO treatment, the patient was successfully weaned off the extracorporeal membrane oxygenation (ECMO) and extubated. No sequela was observed during follow-up.
A 53-year-old woman presented to our hospital due to abdominal pain and fever for 1 d and unconscious for 2 h.
The patient experienced unexplained abdominal pain in the periumbilical region one day ago. She also had a fever, with a self-measured body temperature of 37.5 °C. Her diarrhea was featured by green watery stools occurring about 10 times within a 24-hour period. She had no chest pain, chest tightness, cough, sputum production, headache, or unconsciousness. She had been treated with intravenous infusion of ciprofloxacin and other drugs. She suddenly became unconscious after going to the toilet during the intravenous infusion of ciprofloxacin 2 h ago, accompanied by nausea and vomiting, during which a small amount of gastric contents were discharged. She was immediately sent to a local hospital, where cranial and chest computed tomography (CT) showed bilateral pneumonia as well as accumulated air visible in the right ventricle and pulmonary artery. She was then sent to our hospital for further management and was admitted due to air embolism and obstructive shock. Her diet and sleep quality were poor after disease onset, along with increased stool frequency (watery stool, about 10 times a day) and low urine output. There was no recent weight loss.
She had been in good health.
Her parents were healthy, and their marriage was not consanguineous. There was no family history of a similar disorder.
On physical examination, the vital signs were as follows: body temperature, 36.2 °C; blood pressure, 67/41mmHg; heart rate, 120 beats per min; respiratory rate, 23 breaths per min. Furthermore, the patient was unconscious [E2VTM3 on Glasgow coma scale (GCS)] and had a passive body position. Bilateral pupils were equal, round, and reactive to light. The thoracic cage was symmetric, and there was no tenderness on chest wall. The bilateral chest percussion sound was clear. Although the bilateral breath sounds were coarse, no moist or dry rales were heard on lung auscultation. The heart rate was 120 beats/min, along with regular rhythm. The heart sounds were dull and low-pitched. No obvious pathologic heart murmur was auscultated in all valves. Her abdomen was soft and flat. No gastrointestinal type and peristaltic wave and varicose veins on the abdominal wall were observed. The bowel sounds were normal. Also, the limb muscle-strength and muscle tone were normal, and no edema was observed in both lower limbs. The patient also had normal abdominal wall reflexes as well as normal biceps, triceps, knee tendon, and Achilles tendon reflexes. Both Babinski sign and meningeal irritation signs were negative.
Blood gas analysis showed type 1 respiratory failure and metabolic acidosis (Table 1).
| pH | pCO2 | pO2 | Lac | HCO3- | HCO3std | TCO2 | Beecf | BE(B) | SO2c |
| 7.28 | 46 mmHg | 53 mmHg | 5.4 mmol/L | 21.6 mmol/L | 20.4 mmol/L | 23 mmol/L | -5.1 | -5.3 | 82% |
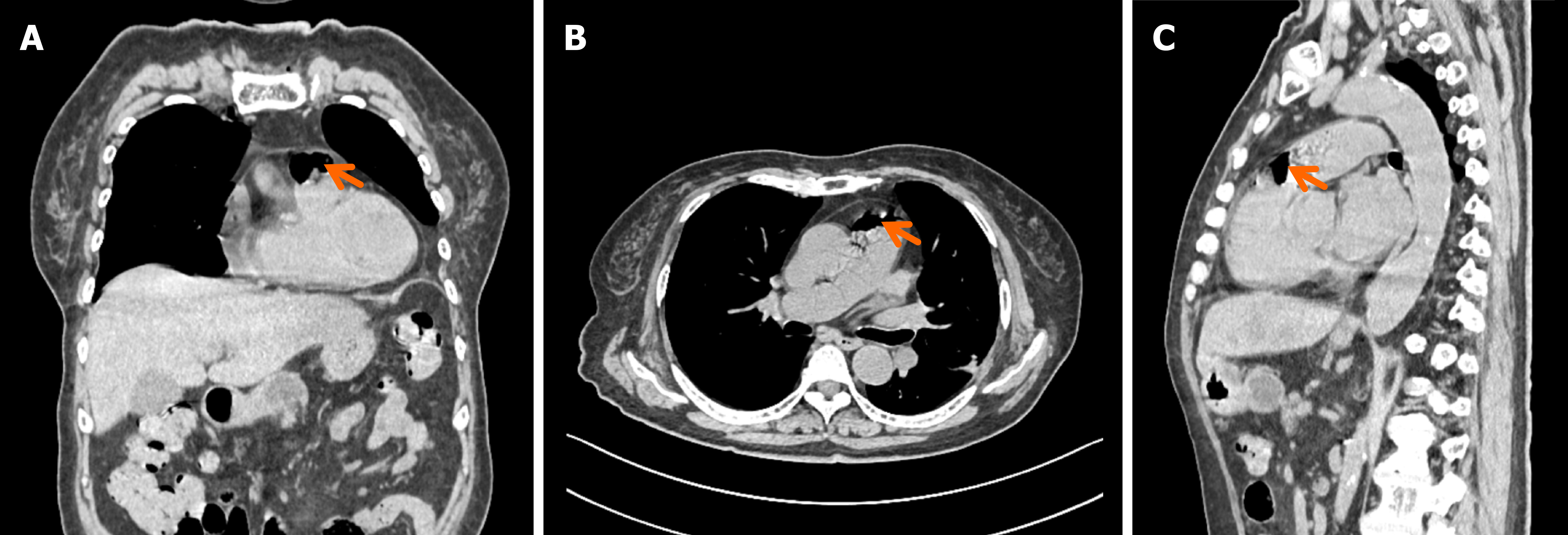
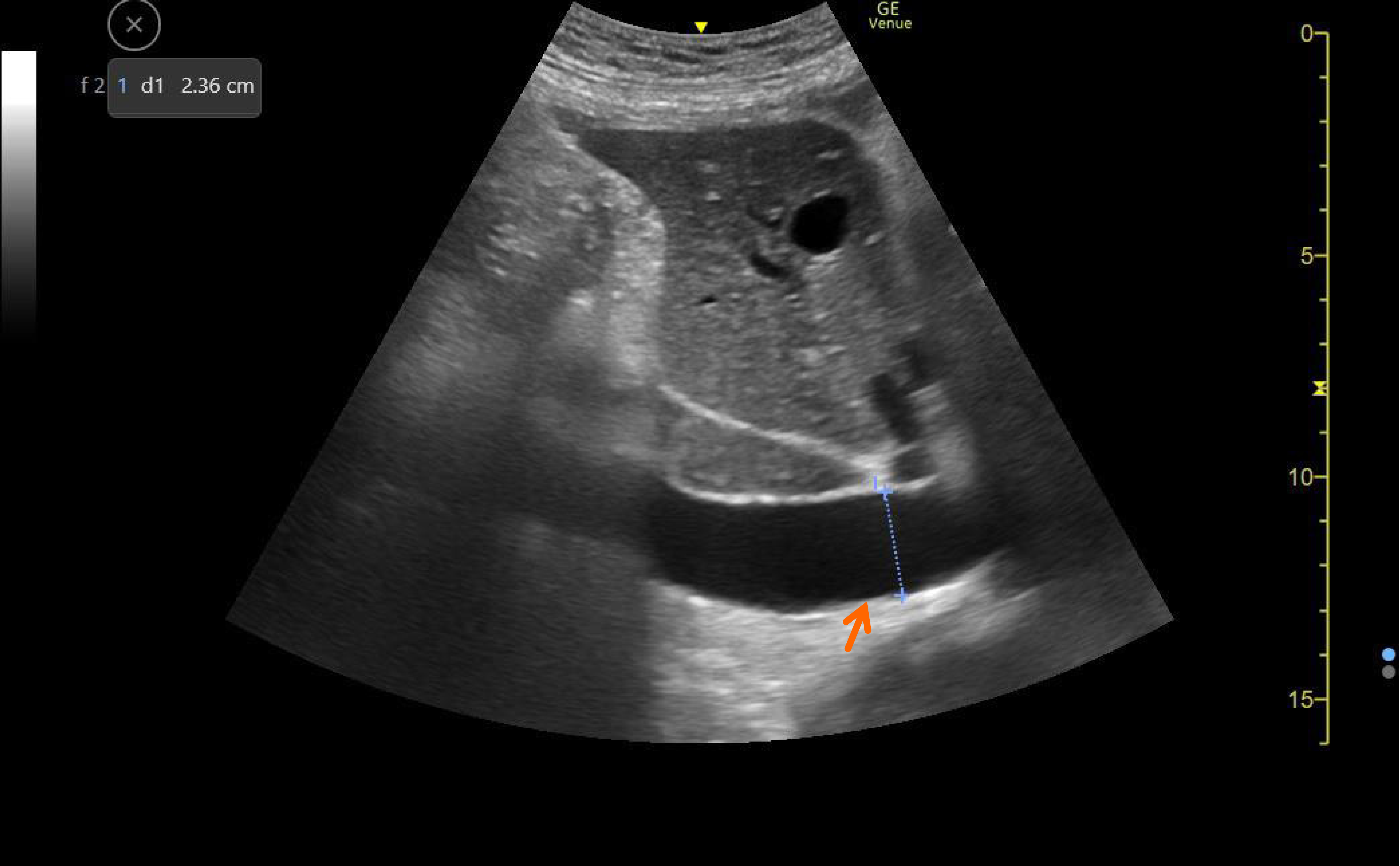
Cranial and chest CT showed bilateral pneumonia as well as accumulated air visible in the right ventricle and pulmonary artery; however, there was no obvious abnormality in the brain (Figure 1). Bedside ultrasound showed that the maximum diameter of the inferior vena cava was 2.36 cm and the respiratory variation was 16% (Figure 2).
Based on medical histories and physical examination and CT findings, the patient was diagnosed with VAE, obstructive shock, and diarrhea.
The patient was transferred to our department with a simple respirator connected via orotracheal intubation. The original infusion set had been replaced. Upon admission, endotracheal intubation and assisted ventilation were applied immediately. A pressure-regulated volume control mode was used, with a tidal volume of 400 mL, a frequency of 15 times/min, and an oxygen concentration of 100% (the patient had a height of 162 cm and a weight of 60 kg). An internal jugular vein access was established in internal jugular vein. Durant's maneuver was performed. No air was seen in the blood aspirated from deep veins. The blood pressure was low. Bedside ultrasound showed that the right heart was dilated, the maximum diameter of the inferior vena cava was 2.36 cm, and the respiratory variation was 16%. Norepinephrine (0.36 μg/kg.min) was immediately used as the vasopressor. In addition, 500mL of lactated Ringer's solution, 100 mL of 20% human albumin solution (for fluid resuscitation), and agents for improving gastrointestinal function were administered. However, the patient's condition did not improve significantly after 1 h. As the oxygenation index continued to drop despite the increased norepinephrine dosage (0.8 μg/kg.min), VA-ECMO (flow rate: 2.4 L/min; gas flow rate: 2.4 L/min; and oxygen concentration: 100%) was performed after communicating with the patient's family. No obvious bubbles were found using a bubble detector. The patient's condition gradually improved after 1 d of treatment, and his consciousness was recovered (GCS score: E4VTM6). The degraded ventilator support parameters were well tolerated, and blood gas analysis showed no obvious abnormality on pre-weaning exercise. The tracheal tube was removed, and the VA-ECMO blood flow and gas flow were reduced. The VA-ECMO was withdrawn 46.5 h after its initiation, and no obvious abnormality was observed on blood gas analysis after the withdrawal. Hyperbaric oxygen therapy was given subsequently. The patient was discharged after 6 days of hospitalization, with stable vital signs and without any neurological sequela.
It has been 6 months since the patient was discharged. She returned to work 1 month after discharge without any discomfort.
VAE is mostly iatrogenic but can also be caused by trauma in rare cases. It is mainly due to the positive pressure difference between the site of the venous vessel break and the right atrium, resulting in the entry of air into the veins. VAE is commonly seen in pressurized infusion, sitting/semi-sitting neurosurgery, laparoscopic surgery, and central venous catheterization and removal. The morbidity and mortality of VAE are related to the speed and volume of air in the venous circulation. If the air bolus is large (about 50 mL), there is a risk of right ventricular outflow tract obstruction (RVOTO), which can lead to circulatory failure. Early animal experiments have shown that venous air can damage pulmonary capillaries, leading to pulmonary edema, stimulating pulmonary capillaries to produce endothelin and platelet activation inhibitors, and increasing pulmonary artery pressure. Even a smaller VAE may result in severe RVOTO, leading to decreased cardiac output, hypotension, myocardial and cerebral ischemia, and even death[1].
No significant progress has been made in the treatment of VAE in the past decades, and currently available case reports mainly focus on its causes. The useful strategies include: Identifying the source of air entering the bloodstream and preventing further entry of air into the circulatory system; increasing the central venous pressure by rehydration; and use of Durant's maneuver[2], removal of air through venous catheters, and hyperbaric oxygen therapy. For critically ill patients, cardiotonic drugs and chest compressions are used[1]. The wider application of ECMO brings new option for critically ill VAE patients who are difficult to maintain homeostasis in the respiratory and circulation systems. However, only two articles have reported the use of ECMO for the treatment of air embolism: one was about VA-ECMO[3] and the other was about veno-venous extracorporeal membrane oxygenation (VV-ECMO)[4]. However, the use of ECMO to treat air embolism remains controversial because theoretically no air is allowed in the ECMO circuits as air can either cause centrifugal pump shutdown[5] or lead to severe air embolism symptoms if air enters the body (especially the left heart) via the ECMO circuits[6]. Notably, the advancement of ECMO manufacturing technology has enabled the artificial membrane lung of ECMO to expel a portion of air[7]. Actually, the use of ECMO in the treatment of air embolism needs to be further explored. First, the choice of ECMO mode (VV-ECMO or VA-ECMO) should be based on the vital signs and the volume of gas in the cardiovascular system. VV-ECMO can be considered in patients with stable vital signs as the membrane lung itself can remove bubbles and thus avoid severe complications caused by air bolus. If the volume of air embolism is less than 7.9 mL[7] but the vital signs are unstable and/or there is respiratory/cardiac arrest, VA-ECMO can be selected; however, the possibility of serious consequences (e.g., myocardial infarction, cerebral infarction, and distal limb infarction) caused by the entry of air into the left heart through the ECMO circuits must be taken into consideration. If the air embolism volume is greater than 7.9 mL, the combination of VV-ECMO with VA-ECMO can be considered, during which the air bubbles in the venous system were filtered out using VV-ECMO and then the cardiac function was supported by using VA-ECMO. In our current case, the volume of air embolism calculated on CT was less than 7.9 mL but the vital signs were extremely unstable, and thus the VA-ECMO was applied. Second, the rotational speed of ECMO is another concern. Literature review and our own air embolism experiments have shown that low rotational speed can reduce the formation of microbubbles in the return blood[8,9]. In the present case, the initial rotational speed was 2000 rpm, along with the close monitoring of flow volume and bubbles in the circuit. Third, air bubbles in the circuit should be removed. In our case, the Medtronic membrane lung was used as it can effectively remove a small amount of air bubbles. The circuit needs to be replaced if air in the circuit causes thrombosis. In our case, no air bubbles were found in the blood returned from the ECMO circuit. Fourth, special attention should be paid to the locations of the membrane lung and the centrifugal pump. Because the gas-port of the membrane lung is located on the upper side of the membrane lung, the air bubbles will be concentrated on the upper side of the membrane lung in a non-gravity-dependent manner. When ECMO was used to treat air embolism, we placed the membranous lungs at a level higher than the centrifugal pump to facilitate the expulsion of air bubbles[5].
ECMO may be used in the treatment of VAE, although further studies are required to demonstrate the ability of ECMO membrane lungs in clearing air bubbles in VAE patients. Numerous clinical studies will be necessary to determine the appropriate indications for ECMO.
| 1. | Marsh PL, Moore EE, Moore HB, Bunch CM, Aboukhaled M, Condon SM 2nd, Al-Fadhl MD, Thomas SJ, Larson JR, Bower CW, Miller CB, Pearson ML, Twilling CL, Reser DW, Kim GS, Troyer BM, Yeager D, Thomas SG, Srikureja DP, Patel SS, Añón SL, Thomas AV, Miller JB, Van Ryn DE, Pamulapati SV, Zimmerman D, Wells B, Martin PL, Seder CW, Aversa JG, Greene RB, March RJ, Kwaan HC, Fulkerson DH, Vande Lune SA, Mollnes TE, Nielsen EW, Storm BS, Walsh MM. Iatrogenic air embolism: pathoanatomy, thromboinflammation, endotheliopathy, and therapies. Front Immunol. 2023;14:1230049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 2. | DURANT TM, LONG J, OPPENHEIMER MJ. Pulmonary (venous) air embolism. Am Heart J. 1947;33:269-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 193] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Shin S, Nam B, Soh S, Koo BN. Percutaneous cardiopulmonary support to treat suspected venous air embolism with cardiac arrest during open eye surgery: a case report. Korean J Anesthesiol. 2014;67:350-353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Kuo CT, Yang Y, Tseng SH, Hsu MY, Wu NY, Wu YL, Tsai TP. Treat Venous Air Embolism Induced Acute Hypoxemic Respiratory Failure during Retinal Surgery by ECMO (V-V Mode). Acta Cardiol Sin. 2021;37:208-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Chan KM, Wan WTP, Ling L, So JMC, Wong CHL, Tam SBS. Management of Circuit Air in Extracorporeal Membrane Oxygenation: A Single Center Experience. ASAIO J. 2022;68:e39-e43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Muth CM, Shank ES. Gas embolism. N Engl J Med. 2000;342:476-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 602] [Cited by in RCA: 605] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 7. | Born F, Khaladj N, Pichlmaier M, Schramm R, Hagl C, Guenther SP. Potential impact of oxygenators with venous air trap on air embolism in veno-arterial Extracorporeal Life Support. Technol Health Care. 2017;25:111-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Born F, König F, Chen J, Günther S, Hagl C, Thierfelder N. Generation of microbubbles in extracorporeal life support and assessment of new elimination strategies. Artif Organs. 2020;44:268-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Ishida M, Takahashi S, Okamura H. Comparison of bubble removal performances of five membrane oxygenators with and without a pre-filter. Perfusion. 2023;38:530-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |