Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.3971
Revised: April 30, 2024
Accepted: May 17, 2024
Published online: July 6, 2024
Processing time: 122 Days and 3 Hours
Pigmented villonodular synovitis (PVNS) is a benign proliferative disorder that affects the synovial joints, bursae, and tendon sheaths. To date, few studies have reported on the treatment of postoperative pain and edema in patients with PVNS. Herein, we present the case of a woman who developed pain and edema in the left lower limb 1 wk after synovectomy and arthroscopic partial meniscectomy and was unable to walk due to limited flexion and extension of the left knee.
A 32-year-old woman underwent synovectomy and arthroscopic partial meniscectomy successively and was treated with a combination of manual lymphatic drainage (MLD) and kinesio taping (KT) in our hospital to alleviate postoperative pain and edema. The following parameters were assessed at 2 wk post-treatment and 1 wk post-discharge follow up: suprapatellar circumference, infrapatellar circumference, visual analog scale score, knee range of motion, pittsburgh sleep quality index score, hamilton anxiety rating scale (HAMA) score, and hamilton depression rating scale (HAMD) score. After treatment, the postoperative pain and edema in the patient’s left knee were effectively relieved, resulting in improved sleep quality and remarkably attenuated HAMA and HAMD scores.
Combined MLD and KT may be an effective approach for relieving postoperative pain and edema in patients with PVNS.
Core Tip: We report the case of a 32-year-old woman who was diagnosed with pigmented villonodular synovitis (PVNS) and had undergone synovectomy and arthroscopic partial meniscectomy; however, her daily life activities were severely affected by pain and swelling after surgery. She was treated with a combination of manual lymphatic drainage (MLD) and kinesio taping (KT) to relieve postoperative pain and edema. After 2 wk, her pain and edema were markedly alleviated, and her knee flexion function gradually improved. This case indicates that the MLD and KT combination treatment may effectively relieve postoperative pain and edema in patients with PVNS.
- Citation: Qu YP, Jin W, Huang B, Shen J. Combination of manual lymphatic drainage and Kinesio taping for treating pigmented villonodular synovitis: A case report. World J Clin Cases 2024; 12(19): 3971-3977
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/3971.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.3971
Pigmented villonodular synovitis (PVNS) is a rare benign proliferative disorder that affects the synovial joints, tendon sheaths, and bursae[1]. PVNS mainly develops in the knees, followed by the hips and ankles. The incidence of PVNS in the United States is approximately 1.8 per million people[2]. Patients with PVNS primarily experience joint-related symptoms such as pain, swelling, and stiffness[3]. Synovectomy is currently the most appropriate treatment for patients with PVNS[4]. However, postoperative pain and edema have detrimental effects on patient rehabilitation and lead to delayed recovery. Recently, manual lymphatic drainage (MLD) and Kinesio taping (KT) have emerged as potential techniques for managing pain and edema management[5]. These techniques alleviate pain and edema by enhancing lymphatic and venous microcirculation and reducing lymphatic stasis in the intercellular space, thereby playing an important role in the treatment of musculoskeletal disorders[6-8]. To date, no study has specifically assessed the treatment of postoperative pain and edema in patients with PVNS. This report describes the case of a young woman who underwent synovectomy and arthroscopic partial meniscectomy. The patient was later treated with a combination of MLD and KT to relieve postoperative pain and edema.
A 32-year-old woman was admitted to our department with pain and swelling of the left lower limb 1 wk after synovectomy and arthroscopic partial meniscectomy, which resulted in an inability to walk due to limited flexion and extension of the left knee.
Five months prior, the patient experienced left knee pain after climbing a mountain that was not relieved with rest. The pain gradually increased with swelling of the left knee. Although the patient could walk independently, her gait was abnormal, and her daily life was affected. Subsequently, she received non-surgical treatment with a traditional Chinese medicine decoction and acupuncture at a local Chinese hospital for 3 months. However, there was no substantial improvement in swelling or pain. Finally, she went to a specialist orthopedic hospital for an magnetic resonance imaging (MRI) of the left knee. She was eventually diagnosed with PVNS and underwent arthroscopic partial meniscectomy and synovectomy. The patient experienced limitations in knee extension and flexion because of intense postoperative pain and swelling. She subsequently received 60 mg of etoricoxib (once/day) to alleviate postoperative pain. She was also administered 15 mg of rivaroxaban (once/day) to prevent blood clots. However, there was no apparent improvement in the patient’s condition, and she was transferred to the rehabilitation department 1 wk after surgery.
The patient had no history of undergoing other relevant therapies.
She was a nonsmoker and nondrinker, and had no family history of illness.
The vital signs were normal on admission. The surgical wound was closed, and swelling and edema were noted around the knee incision, including in the lower middle thigh, knee joint, and lower leg. A measuring tape was used to measure the circumference of the left lower limb, which was 1 cm larger at 15 cm above the left patella and 5 cm larger at 10 cm below the left patella. The patient experienced intense pain during continuous passive motion. The active range of motion (AROM) of the knee was measured using a goniometer, which revealed that the patient had knee flexion of 40° but could not achieve knee extension of 10°. Passive range of motion (PROM) of the knee indicated knee flexion of 80° and knee extension of 0°. Joints of the other limbs exhibited normal mobility. Left quadriceps muscle strength was grade 1 according to the manual muscle test. The patient could not perform a rapid straight leg raise because of pain in her left lower limb. Sensory testing of the left lower limb revealed normal outcomes. She was non-weight-bearing and had two axillary crutches. The patient was very anxious about the pain and functional decline.
Intraoperative pathological evaluation indicated the presence of PVNS. Immunohistochemical staining revealed the following results: Desmin (DES) (-), CD163 (+), H3F3A (-), Ki67 (+), P53 (-), P16 (-), and S100 (-).
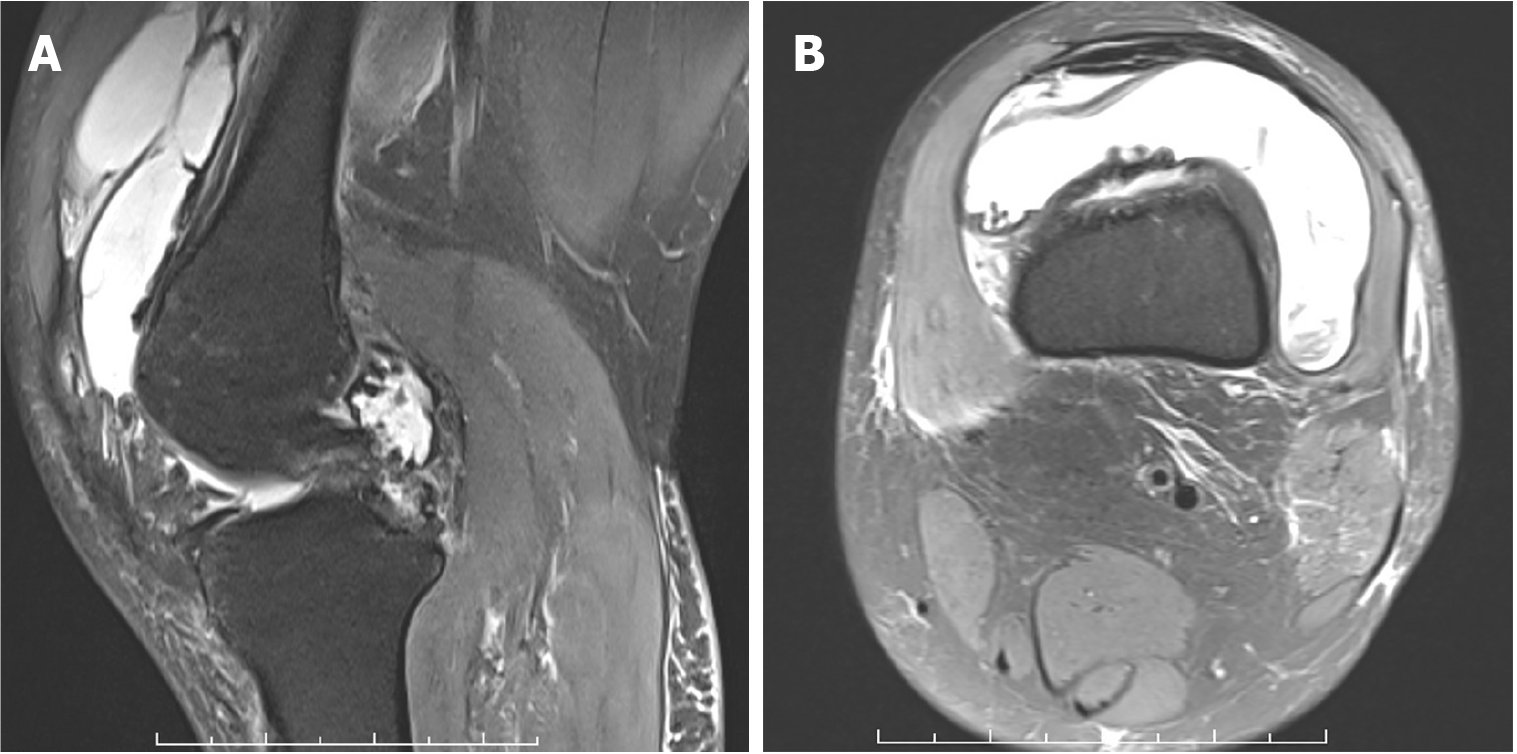
MRI of the left knee showed apparent joint effusion and noticeable synovial proliferation, consistent with the symptoms of PVNS (Figure 1). When the patient was transferred to our department, a B-wave ultrasound examination of the blood vessels in both lower limbs revealed no obvious abnormalities.
The patient was finally diagnosed with PVNS.
Although the orthopedic surgeon prescribed etoricoxib to control breakthrough pain, its therapeutic efficacy was unsatisfactory. The patient’s left lower limb remained swollen even 1 wk after surgery. After the patient was transferred to our rehabilitation department, a comprehensive rehabilitation protocol was implemented based on the primary dysfunction of pain and swelling along with restricted knee motion and comprised MLD, KT, and joint mobility training.
MLD and KT were performed by the same physical therapist. KT was administered for 24 h following MLD treatment. Subsequently, new MLD and KT sessions were conducted. In lymphatic taping, tape is used to alleviate swelling and edema. To tap the posterior part of the leg, the first strip of tape was attached to the medial popliteal fossa without tension, and 10%–20% tension was applied to the tail of the tape oriented toward the lateral malleolus, and the terminal tail had no tension. Similarly, another tape strip was attached to the lateral popliteal fossa without tension, crisscrossing the other strips and ending at the medial malleolus. The treatment session was conducted once daily for 2 consecutive weeks.
The MLD process was as follows: (1) Perform lymphatic massage in the inguinal region near the femoral artery and repeat this procedure three to five times; (2) Apply gentle pressure and use a shovel-shaped hand to massage from the knee joint toward the inguinal lymph nodes, moving in a distal-to-proximal direction on all four sides. this procedure 4 times; (3) Stimulate the popliteal lymph nodes delicately using circular motions with the thumb for approximately 2 min; (4) Use a hand shaped like a shovel to gently apply upward pressure and massage from the ankle to the popliteal fossa of the knee joint, covering both the front and back sides. Repeat this procedure four times; and (5) Place both thumbs closely together while gripping with all four fingers of one hand connected to those of the other hand; gradually and slightly push the hands upward toward the upper thigh area, avoiding any scar tissue, for approximately 2 min. The patient was underwent MLD twice daily.
The patient did not experience any complications or discomfort during the treatment session. After 14 d of rehabilitation, the patient was discharged and followed up for 1 wk. The patient showed a substantial improvement in pain intensity and edema in the left lower limb. This improvement further contributed to enhancing the knee joint mobility and quality of sleep of the patient and relieved her anxiety and depression.
The primary outcomes were knee pain, determined using the visual analog scale (VAS) score[9] and postoperative limb circumference to assess swelling. The secondary outcomes included knee ROM, subjective sleep quality assessed using the pittsburgh sleep quality index (PSQI) score[10], and anxiety and depression levels assessed using the hamilton anxiety rating scale (HAMA)[11] and hamilton depression rating scale (HAMD) scores[12], respectively. All measurements were performed before treatment, 2 wk after treatment, and 1 wk after discharge.
The VAS scores range from 0 to 10 points, with 0 and 10 points indicating no pain and unbearable pain, respectively. Pain intensity was classified as mild (score: 0–3), moderate (score: 4–6), and severe (score: 7–10). The VAS score decreased from 9 to 5 points 2 wk after treatment and further decreased to 3 points 1 wk after discharge (Table 1).
| Outcome measure | Pre-treatment | Post-treatment | Follow-up | |
| 2nd week | 1st week | |||
| VAS | 9 | 5 | 3 | |
| Lower limb circumference | ||||
| 15 cm above patella (cm) | 37 | 36 | 36 | |
| 10 cm under patellar (cm) | 34 | 29 | 30 | |
| AROM/PROM | ||||
| Felxion | 40°/80° | 90°/100° | 90°/105° | |
| Extension | -10°/0° | °0°/0° | 0°/0° | |
The circumference of the affected and postoperative limbs was measured 15 cm above and 10 cm below the edge of the patella. At 2 wk after treatment, the circumference of the left lower limb 10 cm below the patellar edge was reduced (from 34 to 29 cm), and no significant difference in circumference was noted at 1 wk after discharge (Table 1).
The ROM of the left knee was evaluated by using a protractor. Two weeks after treatment, the AROM of the left knee in flexion increased from 40° to 90°, and the PROM increased from 80° to 100°. Knee AROM during extension was normal. Furthermore, the AROM of the left knee in flexion reached 90° at 1 wk after discharge (Table 1).
The PSQI contains seven components: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction. The overall PSQI score ranges from 0 to 21 points, and a global score of 5 or more points indicates poor sleep quality; the higher the score, the worse the sleep quality. The scores for subjective sleep quality, sleep latency, sleep duration, sleep efficiency, and daytime dysfunction decreased after treatment, whereas the scores for sleep disturbance remained unaltered (Table 2).
| Outcome measure | Pre-treatment | Post-treatment | Follow-up |
| 2nd week | 1st week | ||
| PSQI | 17 | 6 | 4 |
| Subjective sleep quality | 3 | 0 | 0 |
| Sleep latency | 3 | 2 | 1 |
| Sleep duration | 3 | 0 | 0 |
| Sleep efficiency | 3 | 0 | 0 |
| Sleep disturbance | 2 | 2 | 1 |
| Use of sleep medications | 0 | 0 | 0 |
| Daytime dysfunction | 3 | 2 | 2 |
| HAMA | 45 | 25 | 21 |
| HAMD | 32 | 16 | 14 |
HAMA and HAMD scores were used to evaluate anxiety and depression symptoms, respectively, and scores greater than 7 indicated anxiety or depression. In our patient, the HAMA and HAMD scores were significantly reduced 2 wk after treatment and showed a further decrease at 1 wk follow-up (Table 2).
PVNS is a subtype of tenosynovial giant cell tumor that diffusely affects the soft tissue lining of joints and tendons[13]. PVNS are classified into two types: localized and diffuse. The diffuse type involves the entire synovial membrane and infiltrates adjacent structures; it is more aggressive and associated with a higher rate of recurrence than the localized type. Pain, swelling, and weakness are primary symptoms of PVNS. Additionally, the affected synovium of PVNS may invade and destroy the surrounding articular cartilage and bone. Surgical resection is the primary treatment for PVNS[14]. Pain, swelling, and reduced joint motion were the main postoperative complications. Poorly controlled acute postoperative pain and edema are associated with increased morbidity, functional decline, impaired quality of life, delayed recovery, and higher medical costs. Currently, there are several effective treatments for edema, including compression therapy, MLD, and KT[15].
Excessive fluid accumulation in intercellular spaces leads to edema. The lymphatic system regulates and compensates for interstitial fluid overflow by returning excess interstitial fluid into circulation. MLD is a massage technique designed to stimulate the lymphatic system[16]. Several studies have reported that MLD can effectively alleviate arm edema and pain in patients with breast cancer[17,18]. Furthermore, a previous study demonstrated that patients who received MLD treatment resumed their daily life activities earlier than those who underwent traditional therapies for managing edema[19]. Therefore, MLD may be a valuable treatment strategy, particularly for patients with primary and secondary lymphedema.
KT is a widely used rehabilitation modality for the prevention and treatment of musculoskeletal disorders[20]. It uses a latex-free porous cotton strip with elastic properties to ease pain and reduce discomfort caused by athletic injuries and other physical disorders. KT exerts several beneficial effects on muscle function, including reduced pain, decreased muscle fatigue, and increased ROM[21]. A previous study showed that KT can increase the subcutaneous space and subsequently improve blood circulation and lymphatic drainage[22]. Another study found that combination therapy with MLD and KT yielded more promising results in alleviating pain and edema than a single therapy[23].
To date, only a few studies have focused on the rehabilitation treatment needs of patients with PVNS. Only one study reported a comprehensive rehabilitation program for patients with PVNS; however, this study did not mention any specific approach for treating pain and edema[24]. In the present case, a young female patient underwent synovectomy for PVNS and experienced severe pain, swelling, and limited ROM of the knee postoperatively. The patient was treated with etoricoxib to relieve pain; however, the treatment efficacy was poor, and she continued to experience intense pain. Postoperative sleep disturbance has a multifactorial etiology that includes surgical inflammatory response, severity of surgical trauma, pain, anxiety, and environmental factors. To relieve pain and edema and improve sleep quality, our patient received a combination of MLD and KT. Based on the VAS, PSQI, HAMA, and HAMD scores, we observed that the MLD and KT combination treatment reduced postoperative pain and edema and improved sleep quality 2 wk after treatment in our rehabilitation department. Similar effects were observed during 1 wk follow-up period. Several researchers have proposed the “fast-track surgical approach, which has multiple benefits, including a shorter length of hospital stay, decreased hospitalization costs, and lower postoperative morbidity and mortality rates[25]. Effective control of pain and edema is a critical factor that should be considered when implementing treatment approaches for patients with PVNS. In the present case, MLD and KT, as low-cost, safe, and side-effect-free physiotherapy techniques, were found to relieve pain and edema in the early postoperative period. Thus, MLD and KT may play important roles in early orthopedic rehabilitation.
This study had some limitations. The proposed therapy was administered to only one patient with PVNS (a very small sample size); consequently, our findings cannot be generalized to all patients with PVNS. In addition, owing to the short-term follow-up period, the patient’s recovery status could not be reliably determined. Further research is required to overcome these limitations and validate our findings.
MLD and KT combination treatment may be an effective approach to relieve postoperative pain and edema in patients with PVNS.
| 1. | Chipman DE, Perkins CA, Lijesen E, Green DW. Pigmented villonodular synovitis/giant cell tumor in the knee. Curr Opin Pediatr. 2024;36:78-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 2. | Burton TM, Ye X, Parker ED, Bancroft T, Healey J. Burden of Illness Associated with Tenosynovial Giant Cell Tumors. Clin Ther. 2018;40:593-602.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Pinto AA, Krishnan R, Shekar KY, Amaravathi RS. A Novel Technique of Resecting Localized Pigmented Villonodular Synovitis of the Knee Joint. J Orthop Case Rep. 2023;13:18-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Schindler M, Puchner S, Reinhard J, Leiss F, Windhager R, Lass R. Recurrence-Free Survival after Synovectomy and Subsequent Radiosynoviorthesis in Patients with Synovitis of the Knee-A Retrospective Data Analysis. J Clin Med. 2024;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 5. | Guney-Deniz H, Kinikli GI, Aykar S, Sevinc C, Caglar O, Atilla B, Yuksel I. Manual lymphatic drainage and Kinesio taping applications reduce early-stage lower extremity edema and pain following total knee arthroplasty. Physiother Theory Pract. 2023;39:1582-1590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 6. | Ickert EC, Griswold D, Ross O, Dudash S, Duchon C, Learman K. Effects of kinesiotaping during early post-operative rehabilitation in individuals who underwent a total knee arthroplasty: A systematic review and meta-analysis of randomized control trials. Clin Rehabil. 2024;38:732-748. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Golkar M, Taheri A, Alam M, Asadi Y, Keyhan SO. The effects of Kinesio tapes on facial swelling following bimaxillary orthognathic surgery in the supraclavicular region. Maxillofac Plast Reconstr Surg. 2023;45:22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Provencher AM, Giguère-Lemieux É, Croteau É, Ruchat SM, Corbin-Berrigan LA. The use of manual lymphatic drainage on clinical presentation of musculoskeletal injuries: A systematic review. Complement Ther Clin Pract. 2021;45:101469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Cai Y, Deng Y, Ou L, Guo Y. Clinical trial of manual therapy in the treatment of chondromalacia patellae. Medicine (Baltimore). 2023;102:e33945. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Wang L, Wu YX, Lin YQ, Wang L, Zeng ZN, Xie XL, Chen QY, Wei SC. Reliability and validity of the Pittsburgh Sleep Quality Index among frontline COVID-19 health care workers using classical test theory and item response theory. J Clin Sleep Med. 2022;18:541-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 32] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 11. | Xu H, Kang B, Li Y, Xie J, Sun S, Zhong S, Gao C, Xu X, Zhao C, Qiu G, Xiao L. Using electroacupuncture to recover muscle strength in patients with knee osteoarthritis after total knee arthroplasty: a study protocol for a double-blinded, randomized, and placebo-controlled trial. Trials. 2020;21:705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Li H, George DM, Jaarsma RL, Mao X. Metabolic syndrome and components exacerbate osteoarthritis symptoms of pain, depression and reduced knee function. Ann Transl Med. 2016;4:133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 13. | Lingamfelter M, Novaczyk ZB, Cheng EY. Extensile Anterior and Posterior Knee Exposure for Complete Synovectomy of Diffuse Tenosynovial Giant Cell Tumor (Pigmented Villonodular Synovitis). JBJS Essent Surg Tech. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Bernthal NM, Ishmael CR, Burke ZDC. Management of Pigmented Villonodular Synovitis (PVNS): an Orthopedic Surgeon's Perspective. Curr Oncol Rep. 2020;22:63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Selcuk Yilmaz S, Ayhan FF. The Randomized Controlled Study of Low-Level Laser Therapy, Kinesio-Taping and Manual Lymphatic Drainage in Patients With Stage II Breast Cancer-Related Lymphedema. Eur J Breast Health. 2023;19:34-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 16. | Ramadan F. Manual lymphatic drainage: the evidence behind the efficacy. Br J Community Nurs. 2024;29:83-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Da Cuña-Carrera I, Soto-González M, Abalo-Núñez R, Lantarón-Caeiro EM. Is the Absence of Manual Lymphatic Drainage-Based Treatment in Lymphedema after Breast Cancer Harmful? A Randomized Crossover Study. J Clin Med. 2024;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 18. | Qiao J, Yang LN, Kong YH, Huang X, Li Y, Bai DQ. Effect of Manual Lymphatic Drainage on Breast Cancer-Related Postmastectomy Lymphedema: A Meta-analysis of Randomized Controlled Trials. Cancer Nurs. 2023;46:159-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Majewski-Schrage T, Snyder K. The Effectiveness of Manual Lymphatic Drainage in Patients With Orthopedic Injuries. J Sport Rehabil. 2016;25:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Tran L, Makram AM, Makram OM, Elfaituri MK, Morsy S, Ghozy S, Zayan AH, Nam NH, Zaki MMM, Allison EL, Hieu TH, Le Quang L, Hung DT, Huy NT. Efficacy of Kinesio Taping Compared to Other Treatment Modalities in Musculoskeletal Disorders: A Systematic Review and Meta-Analysis. Res Sports Med. 2023;31:416-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 21. | Llamas-Ramos I, Cortés-Rodríguez M, Llamas-Ramos R. Kinesiotape effectiveness in mechanical low back pain: A randomized clinical trial. Work. 2022;72:727-736. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Badino G, Veronese N, Cella A. Effectiveness of a kinesio-taping-based treatment in stage IV sacral pressure ulcers in older patients: a pilot study. J Wound Care. 2024;33:60-65. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Tornatore L, De Luca ML, Ciccarello M, Benedetti MG. Effects of combining manual lymphatic drainage and Kinesiotaping on pain, edema, and range of motion in patients with total knee replacement: a randomized clinical trial. Int J Rehabil Res. 2020;43:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Shekhani N, Neyman I. Rehabilitation outcome of a case of pigmented villonodular synovitis. J Pak Med Assoc. 1996;46:242-245. [PubMed] |
| 25. | Arienti C, Pollet J, Buraschi R, Piovanelli B, Villafañe JH, Galeri S, Negrini S. Fast-track rehabilitation after total knee arthroplasty reduces length of hospital stay: A prospective, case-control clinical trial. Turk J Phys Med Rehabil. 2020;66:398-404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |