Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.3956
Revised: April 25, 2024
Accepted: May 21, 2024
Published online: July 6, 2024
Processing time: 124 Days and 18.5 Hours
Intracranial arterial narrowing is a significant factor leading to brief episodes of reduced blood flow to the brain, known as transient ischemic attacks, or full-blown strokes. While atherosclerosis is commonly associated with intracranial arterial narrowing, it is frequently of a non-atherosclerotic nature in younger patients.
Here, we present the case of a young stroke patient with narrowing of the middle cerebral artery (MCA), characterized as non-atherosclerotic lesions, who exper
The use of drug-coated balloon angioplasty demonstrated favorable outcomes in repairing and reshaping the blood vessel wall in young patients. Therefore, it may be considered a promising treatment option for similar cases.
Core Tip: Drug-coated balloon angioplasty presents a technically viable solution that avoids the use of foreign materials within intracranial vessels and eliminates the necessity for prolonged dual antiplatelet therapy. Therefore, for young patients experiencing severe narrowing of intracranial arteries resulting in recurrent ischemic stroke episodes despite standard medical interventions, drug-coated balloon angioplasty may offer a favorable treatment alternative.
- Citation: Zhu PC, Shu LF, Dai QH, Tan HT, Wang JB, Wu T. Drug-coated balloon angioplasty for the treatment of intracranial arterial stenosis in a young stroke patient: A case report. World J Clin Cases 2024; 12(19): 3956-3960
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/3956.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.3956
Intracranial arterial narrowing stands as a significant contributor to transient ischemic attacks or strokes, often linked to atherosclerosis. Nonetheless, intracranial arterial narrowing in young patients commonly stems from non-atherosclerotic causes. Herein, we present a case of a young stroke patient with intracranial arterial narrowing who achieved positive treatment outcomes through drug-coated balloon angioplasty.
A 26-year-old male patient was admitted to the First Affiliated Hospital of Henan University of Traditional Chinese Medicine on November 28, 2020, complaining of "weakness in the left limbs for 2 wk, worsening for 1 d".
On November 27, 2020, the patient experienced a recurrence of left limb weakness and returned to our hospital. Neurological examination revealed grade IV muscle strength in the left upper limb, grade II muscle strength in the left lower limb, and increased muscle tone.
Prior to admission, on the evening of November 7, 2020, the patient experienced vomiting and black stools after alcohol consumption and sought medical attention at the First Affiliated Hospital of South China University, where he received symptomatic treatment. During hospitalization, on November 13, 2020, the patient suddenly experienced decreased mobility in the left limbs, with muscle strength of grade III in the left upper limb and grade II in the left lower limb, along with increased muscle tone. The patient received treatments aimed at improving neurological function, enhancing collateral circulation, and promoting limb recovery. After treatment, the patient's left limb function improved, with the left upper limb reaching grade V muscle strength and the left lower limb reaching grade IV muscle strength, and muscle tone returned to normal. He was discharged on November 21, 2020, and prescribed atorvastatin calcium 10 mg once daily and clopidogrel sulfate 75 mg once daily.
The patient denied any family history of cerebrovascular disease.
During the physical examination, the patient's vital signs were recorded as follows: Body temperature, 36.5℃; blood pressure, 150/100 mmHg; heart rate, 90 beats per minute; respiratory rate, 13 breaths per minute.
Prothrombin time 13.2 s, international normalized ratio 1.22, C-reactive protein 21.9 mg/L.
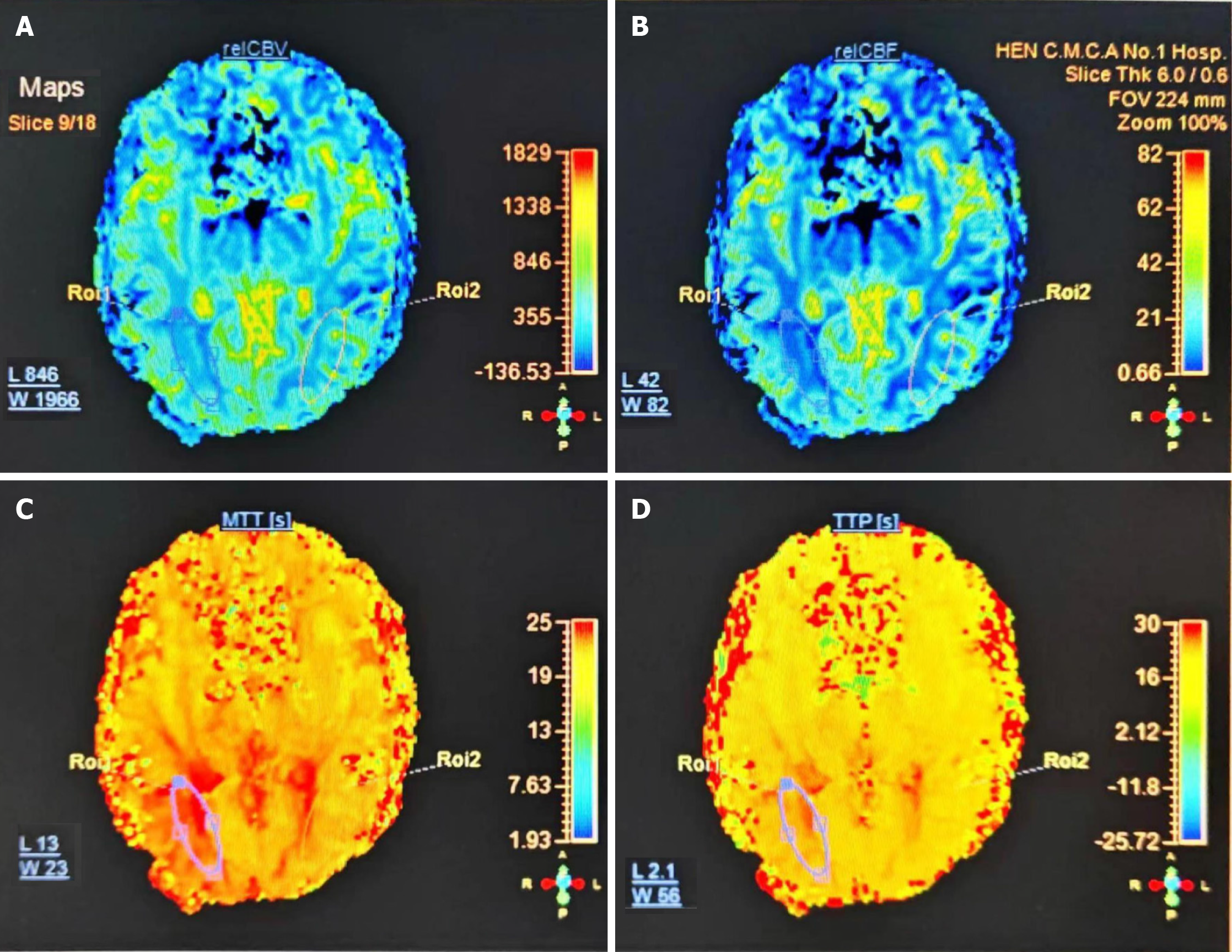
The transcranial Doppler ultrasound findings indicated the following: (1) Severe narrowing observed in the segment from the right internal carotid artery to the middle cerebral artery (MCA); and (2) Decreased flow velocity noted in the left anterior cerebral artery. Perfusion imaging depicted reduced cerebral blood flow and cerebral blood volume in the right temporal and parietal lobes when compared to the left hemisphere. Additionally, prolonged mean transit time and time to peak were observed, suggesting relative hypoperfusion on the right side (Figure 1).
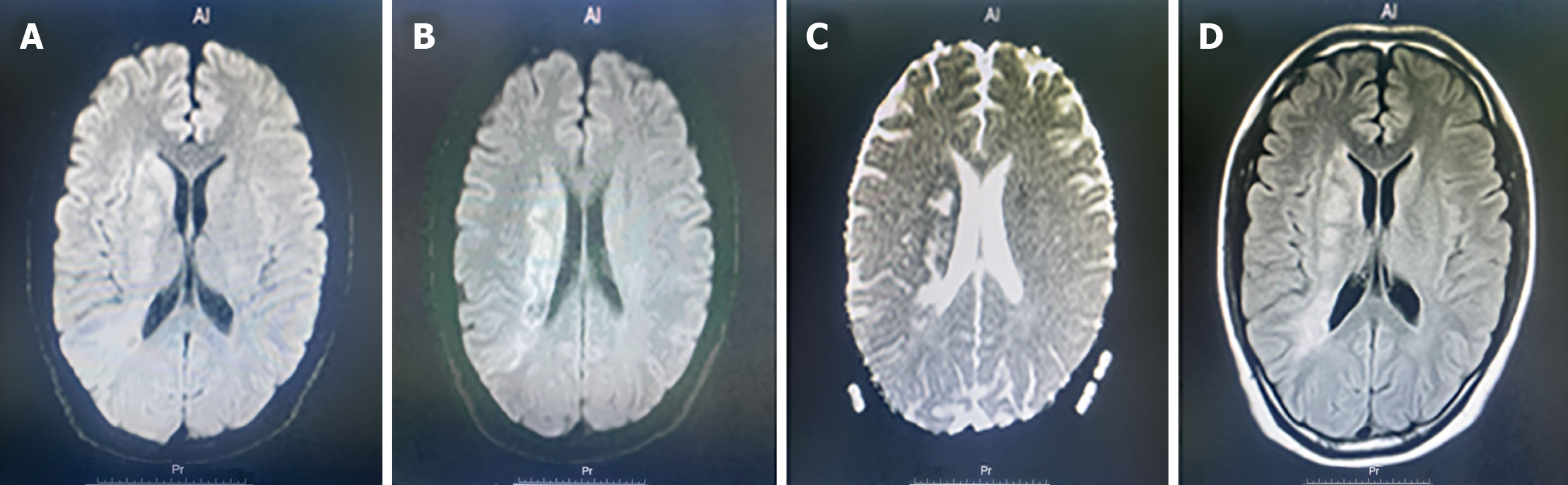
Diffusion-weighted imaging revealed that cerebral infarction existed in the right lateral ventricle, radiating crown and parietal lobe (Figure 2).
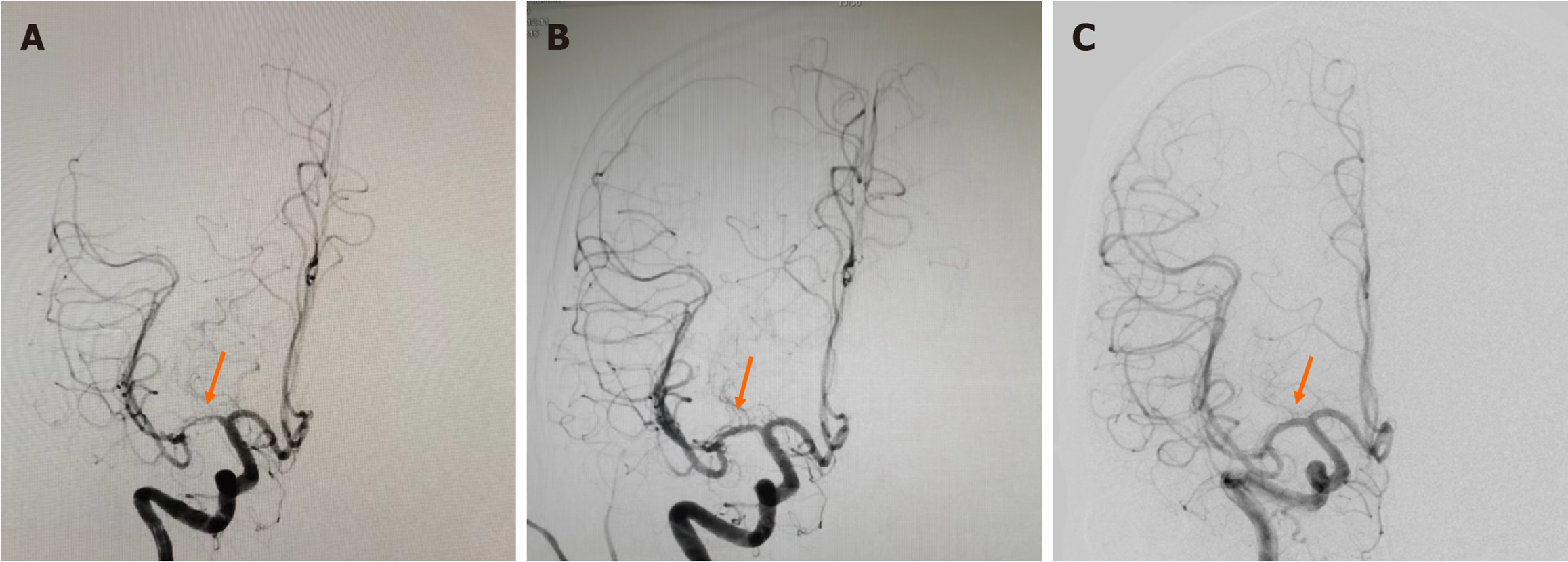
The final diagnosis was severe narrowing (approximately 80%) in the M1 segment of the right MCA (Figure 3A).
Despite receiving standard medical treatment, the patient experienced a recurrent ischemic stroke event associated with severe intracranial artery narrowing, along with evidence of reduced cerebral perfusion on the right side. Considering the patient's young age and absence of underlying atherosclerosis, alternative treatment options were explored. Therefore, drug-coated balloon angioplasty was selected as the treatment modality. A 6F arterial sheath was inserted into the right femoral artery, and a 6F guiding catheter was positioned in the C2 segment of the right internal carotid artery. Utilizing a micro-guidewire for guidance, the microcatheter was advanced through the stenotic M1 segment of the right MCA to the M3 segment. A 0.014-inch exchange wire was employed to navigate through the microcatheter, which was then left in the M3 segment. A drug-coated balloon catheter (YINYI) (2.0 mm × 15 mm) was deployed in the stenotic segment and gradually inflated to 8 atmospheres, leading to successful dilation and resolution of the stenosis. Subsequently, a drug-coated balloon catheter (SINOMED) (2.0 mm × 15 mm) was introduced into the stenotic segment and coated with paclitaxel for 1 min. Following this, angiography was performed, confirming the resolution of stenosis in the M1 segment of the right MCA. While the remaining branches exhibited satisfactory opacification, the vessel wall displayed irregularities (Figure 3B).
During hospitalization, the patient demonstrated improvement in left limb function, with the left upper limb reaching grade V muscle strength and the left lower limb achieving grade IV muscle strength, while muscle tone returned to normal. Subsequently, he was discharged on December 28, 2020. Follow-up digital subtraction angiography (DSA) conducted on June 25, 2021, revealed no significant stenosis in the right MCA, with a smooth vessel wall observed (Figure 3C). In a telephone follow-up on August 18, 2023, the patient reported no further ischemic stroke events related to right MCA stenosis in nearly three years.
Intracranial arterial narrowing represents a significant etiology of ischemic strokes, commonly associated with atherosclerosis. Nevertheless, in younger individuals, it is crucial to contemplate non-atherosclerotic origins such as arteritis and immune-related factors. In such cases, drug-coated balloon angioplasty emerges as a potentially appropriate therapeutic avenue[1,2]. Conversely, for elderly patients grappling with severe atherosclerotic intracranial arterial narrowing and experiencing recurrent events despite conventional medical management, stent placement may warrant consideration[3]. Considering the patient's youthfulness, minimal blood pressure elevation, and absence of atherosclerosis risk factors, the occurrence of ischemic stroke events related to right middle cerebral artery stenosis despite anti-platelet and intensive lipid-lowering therapy is noteworthy. Given the diagnosis of non-atherosclerotic vascular stenosis, drug balloon dilation therapy was chosen. Subsequent DSA angiography revealed alleviation of right MCA stenosis, albeit with irregular vessel wall morphology. The cerebral circulation blood flow improved (TICI3), and symptoms such as left limb numbness were relieved post-operation. A DSA reassessment six months post-operation demonstrated the absence of significant stenosis in the right MCA, with a smooth vessel wall and favorable vascular remodeling observed. Remarkably, without prior knowledge of the right middle cerebral artery's treatment with drug balloon dilation, it would have been challenging to detect, indicating the beneficial effects of drug balloons on vascular wall repair and remodeling in young patients[4].
Drug-coated balloon angioplasty represents a technically feasible approach that circumvents the retention of foreign materials within intracranial vessels and obviates the necessity for prolonged dual antiplatelet therapy[5,6]. Hence, for young patients grappling with severe intracranial artery stenosis and experiencing recurrent ischemic stroke events despite standard medical interventions, drug-coated balloon angioplasty may emerge as a favorable treatment option.
| 1. | Ekker MS, Boot EM, Singhal AB, Tan KS, Debette S, Tuladhar AM, de Leeuw FE. Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol. 2018;17:790-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 281] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 2. | George MG. Risk Factors for Ischemic Stroke in Younger Adults: A Focused Update. Stroke. 2020;51:729-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 126] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 3. | Mao LL, Ma AJ, Liu ZQ, Zhang J, Xu YF, Chen WY, Cao YJ. A retrospective study of individualized endovascular treatment for symptomatic intracranial atherosclerotic stenosis in patients with ischemic stroke/transient ischemic attack. Front Neurol. 2022;13:1057935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Zhang J, Zhang X, Zhang J, Song Y, Zheng M, Sun L, Meng Y, Zhao W, Yin H, Wang W, Han J. Drug-Coated Balloon Dilation Compared With Conventional Stenting Angioplasty for Intracranial Atherosclerotic Disease. Neurosurgery. 2020;87:992-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Han J, Zhang J, Zhang X, Zhang J, Song Y, Zhao W, Zheng M, Sun L, Wang W. Drug-coated balloons for the treatment of symptomatic intracranial atherosclerosis: initial experience and follow-up outcome. J Neurointerv Surg. 2019;11:569-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Zhang Y, Chu X, Meng Y, Zhang J, Sun L, Zhao W, Zheng M, Yin H, Wang W, Zhang J, Song Y, Han J. Drug-Coated Balloon-Oriented Angioplasty for Severe Symptomatic Atherosclerotic MCA Stenosis in Young Adults. Front Neurol. 2021;12:743851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |