Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.3950
Revised: April 23, 2024
Accepted: May 8, 2024
Published online: July 6, 2024
Processing time: 126 Days and 19.6 Hours
We report a case of eye-penetrating injury in which a massive silicone oil mig
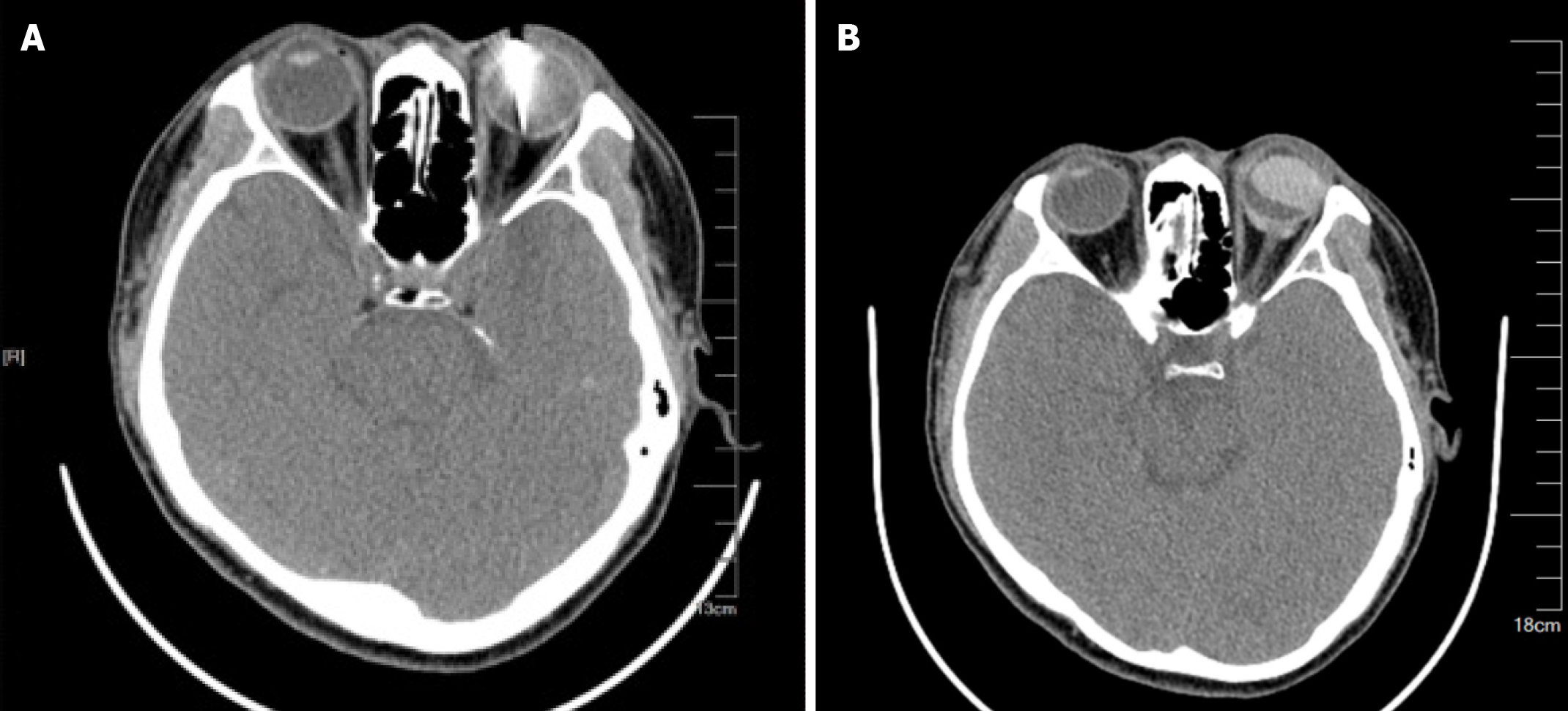
A 30-year-old male patient sought medical attention at Ganzhou People’s Hospital after experiencing pain and vision loss in his left eye due to a nail wound on December 9, 2023. Diagnosis of penetrating injury caused by magnetic foreign body retention in the left eye and hospitalization for treatment. On December 9, 2023, pars plana vitrectomy was performed on the left eye for intraocular foreign body removal, abnormal crystal extraction, retinal photocoagulation. Owing to the discovery of retinal detachment at the posterior pole during surgery, silicone oil was injected to fill the vitreous body, following which upper conjunctival bubble-like swelling was observed. Postoperative orbital computed tomography (CT) review indicated migration of silicone oil to the subconjunctival space and orbit through a self-permeable outlet. On December 18, 2023, the patient sought treatment at the First Affiliated Hospital of Nanchang University, China. The patient presented with a pronounced foreign body sensation following left eye surgery. On December 20, 2023, the foreign body was removed from the left eye frame and an intraocular examination was conducted. The posterior scleral tear had closed, leading to termination of the surgical procedure following supplementary laser treatment around the tear. The patient reported a significant reduction in ocular surface symptoms just one day after surgery. Furthermore, a notable decrease in the migration of silicone oil was observed in orbital CT scans.
The timing of silicone oil injection for an eye-penetrating injury should be carefully evaluated to avoid the possi
Core Tip: We report a case of ocular penetrating injury and significant migration of silicone oil into the subconjunctival space and orbit in a patient after vitrectomy. Subsequently, the foreign body was removed frame through surgical treatment. Ultimately, we believe the timing of silicone oil injection for an eye-penetrating injury should be carefully evaluated to avoid the possibility of silicone oil migration.
- Citation: Shu BL, Wu HY, Hu YX, Rao J, Wei B, Huang QY, Wu XR. Silicone oil migrating into the conjunctival space and orbit after surgery for an eye-penetrating injury: A case report. World J Clin Cases 2024; 12(19): 3950-3955
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/3950.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.3950
Silicone oil is commonly used for the surgical treatment of giant retinal tears and retinal detachment[1]. However, its use is associated with complications such as cataract formation, silicone oil keratopathy, emulsification with glaucoma, intraconjunctival oil inclusion cysts, subretinal oil accumulation, membrane reproliferation beneath the oil interface, and optic atrophy[2]. In a rare complication, silicone oil can migrate into the conjunctival space[3], orbit[4], or intracranial region[5]. Here, we present a case of silicone oil migration into the conjunctival space and orbit after treatment with vitreous implantation of silicone oil for an eye-penetrating injury.
Postoperative left eye redness and pain for 9 d.
The patient sought medical attention at Ganzhou People’s Hospital after experiencing pain and vision loss in his left eye due to a nail wound on December 9, 2023. Diagnosis of penetrating injury caused by magnetic foreign body retention in the left eye and hospitalization for treatment. On December 9, 2023, pars plana vitrectomy (PPV) was performed on the left eye for intraocular foreign body removal, abnormal crystal extraction, retinal photocoagulation. Owing to the discovery of retinal detachment at the posterior pole during surgery, silicone oil was injected to fill the vitreous body. Postoperative the patient presented with a pronounced foreign body sensation following left eye surgery. Orbital computed tomography (CT) review indicated migration of silicone oil to the subconjunctival space and orbit through a self-permeable outlet.
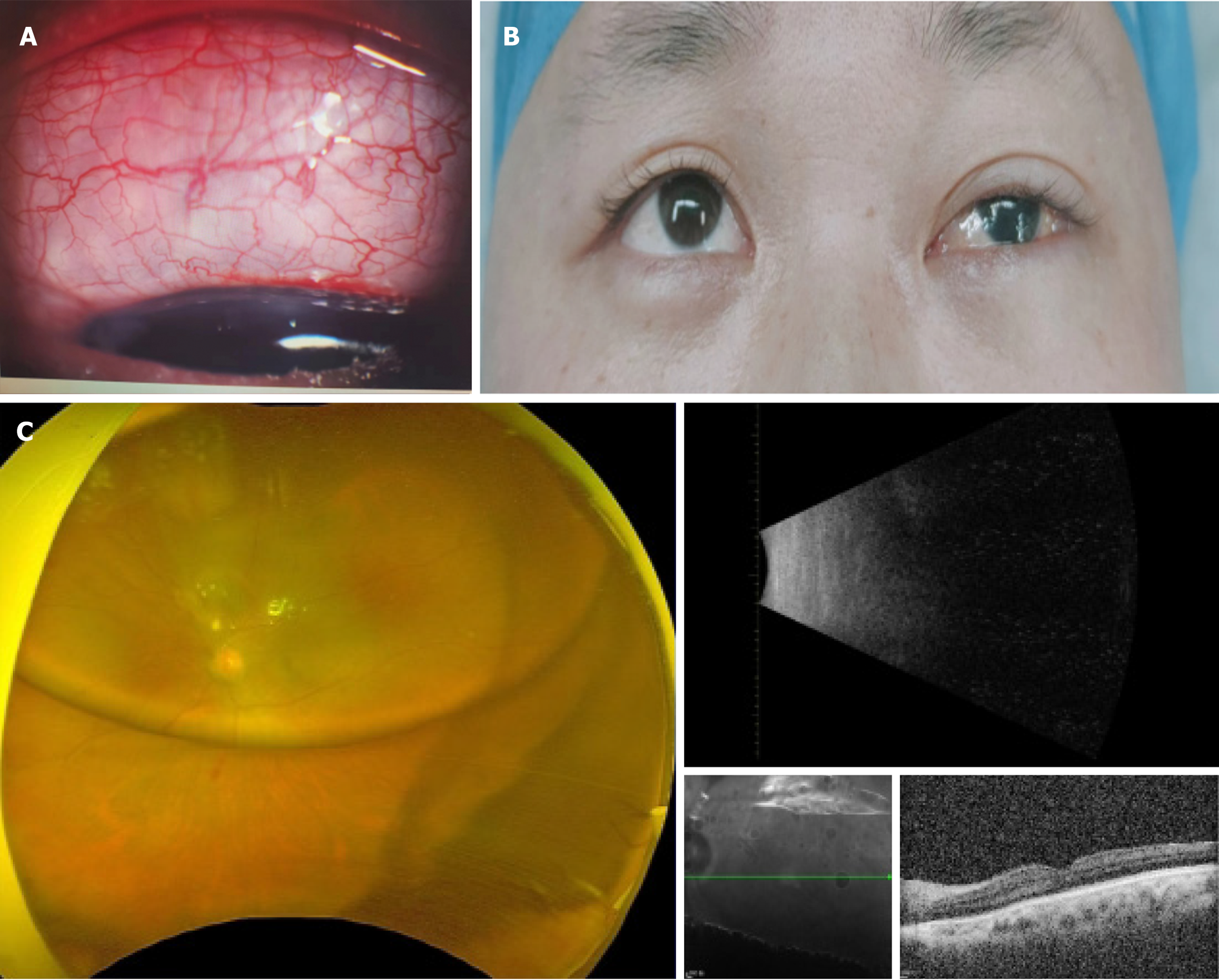
Previous physical fitness.
The patient had no history of family illness.
An ophthalmological examination revealed that the patient’s right eye had an uncorrected visual acuity of 0.2 and a corrected visual acuity of 1.0, while the left eye had a visual acuity of 0.08. The patient’s left eyelid was swollen, and conjunctival congestion together with a bubble-like swelling of the upper conjunctiva were present (Figure 1A and B). The corneal sutures at position seven were intact; however, extensive damage to the corneal epithelium was observed. The absence of the lens was confirmed; the vitreous cavity was observed to be filled with silicone oil; a flaky hemorrhage was noted in the upper retina; and laser spots were also noted surrounding the hemorrhage during a fundus examination (Figure 1C). Intraocular pressure in the left eye remained within the normal range.
No significant abnormalities were found in blood tests, routine urine tests and urinary sediment examination, routine fecal tests and occult blood test, blood biochemistry, immune indexes, and infection indexes.
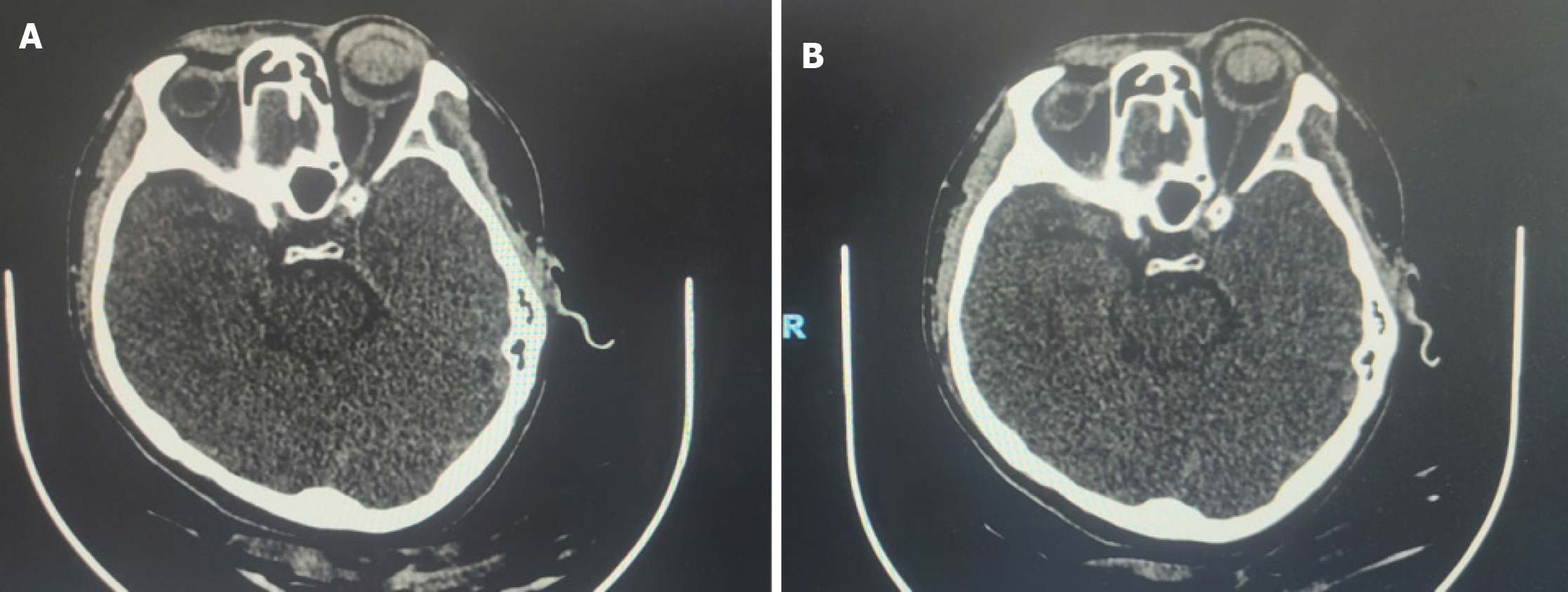
An orbital CT scan suggested the retention of a magnetic foreign body within the left eyeball (Figure 2A). Review of postoperative orbital CT imaging revealed migration of the silicone oil to the subconjunctival space and orbit through a self-permeable outlet (Figure 2B). A notable decrease in the migration of the silicone oil was thereafter observed in CT imaging of the orbit (Figure 3).
Silicone oil migration, aphakic, corneal epithelial defect.
On December 20, 2023, the foreign body was removed from the left eye frame, and an intraocular examination was conducted. The posterior scleral tear had closed, leading to termination of the surgical procedure after supplementary laser treatment around the tear.
The patient reported a significant reduction in ocular surface symptoms just one day after surgery. The duration of silicone oil filling is insufficient. To mitigate the risk of post-removal retinal detachment and wound proliferation, a three-month interval is planned for silicone oil removal.
In current conventional PPV surgery, a 25G transconjunctival sutureless vitrectomy technique is used. However, a slight leakage of silicone oil into the conjunctival space from the scleral puncture can occur[6]. Given the safety and stability of silicone oil, this minor migration does not typically cause discomfort to patients or require any specific treatment. However, if a significant amount of silicone oil migrates into the subconjunctival space, either because of a scleral puncture or other scleral rupture, patients can present with symptoms on the ocular surface. Although such migration is usually quickly discovered, the removal of migrated silicone oil can be challenging[3].
Migration into the orbit is an infrequent complication after intravitreal silicone oil implantation. However, this migration has no clear presenting clinical symptoms. Most patients are diagnosed with conditions such as mechanical ptosis or a hordeolum[4,7], possibly because of the increased load on the levator muscle caused by the accumulation of silicone oil. In most cases of silicone oil migration into the orbit, surgical intervention is required[8].
In the present case, the eye-penetrating injury played a crucial role in the silicone oil migration; however, other factors cannot be excluded as potential causes. Migration into the orbit can follow from a posterior scleral laceration in which wound closure is not performed or from high intraocular pressure post surgery leading to a reopening of the original lacerations. This silicone oil migration causes the eyeball to displace anteriorly and elevates the orbital pressure. CT imaging of the orbit will then reveal proptosis. In our patient, the silicone oil migration through the orbital septum into the subcutaneous and conjunctival spaces of the eyelid resulted in mechanical ptosis, accompanied by mild restriction of ocular motility. In terms of surgical method selection, removal of the migrated silicone oil was imperative, and preoperative knowledge indicated that the posterior scleral tear was located superior to the retina. Intraoperatively, the remaining silicone oil exerted sufficient pressure on the detached retina, and the posterior scleral tear was closed. To optimize the patient’s prognosis, the oil was retained.
The prognosis for visual acuity in patients with such eye injuries is often poor. Preoperatively, measures should be taken to reduce the risk of postoperative complications. In patients with eye-penetrating injuries who have posterior scleral lacerations that cannot be sutured, special attention should be paid to the possibility of silicone oil migration before silicone oil is injected. After the first stage of suturing the ruptured eyeball, waiting for the posterior scleral laceration to close before performing the second stage of silicone oil injection might be the preferable choice. On follow–up, close monitoring of postoperative changes in intraocular pressure and strengthening of the patient’s awareness of the potential for an intraocular pressure rise are necessary. If silicone oil migration is found, the migrated oil should be promptly removed, and the need for the intraocular silicone oil should be reevaluated. If remigration is a risk, the intraocular silicone oil should be removed as soon as possible. If a posterior scleral tear is closed, preserving the intraocular silicone oil can be an option for patients needing further treatment.
| 1. | Sharifi M, Ansari Astaneh MR. Migration of Silicone Oil into the Orbit and Eyelid as a Cyst. Case Rep Ophthalmol. 2020;11:217-221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Eller AW, Friberg TR, Mah F. Migration of silicone oil into the brain: a complication of intraocular silicone oil for retinal tamponade. Am J Ophthalmol. 2000;129:685-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 83] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Téllez J, Vela JI, Luna S, Delgado R. Massive Silicone Oil Migration into the Subconjunctival Space: A Leakage Mechanism Dilemma. Case Rep Ophthalmol. 2018;9:310-314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Ali Bautista S, Wladis EJ, Farber M, Falk NS, Phelps PO. Silicone oil migration into the orbit. Orbit. 2018;37:368-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Shimazaki R, Tsunogae M, Ueda M. Intraventricular Silicone Oil Migration Resembling Hemorrhagic Complication in a Patient with Ischemic Stroke Receiving Antithrombotic Therapy. J Stroke Cerebrovasc Dis. 2021;30:105527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Tibrewal S, Khurana R, Venkatesh R, Ganesh S. Subconjunctival silicone oil complicating strabismus surgery. GMS Ophthalmol Cases. 2019;9:Doc12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Lemaitre S, Vahdani K, Escalas P, Rose GE. Orbital Leakage of Intraocular Silicone Oil: Case Reports and Literature Review. Ophthalmic Plast Reconstr Surg. 2020;36:e75-e78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Lam SC, Chan AYY, Yuen HKL. Extraocular silicone oil migration to orbit and retrolaminar region: case report and systematic review. Graefes Arch Clin Exp Ophthalmol. 2020;258:2799-2807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |